اللهم يا معلّم موسى علّمني، ويا مفهم سليمان فهّمني، ويا مؤتي لقمان الحكمة وفصل الخطاب آتني الحكمة وفصل الخطاب اللهم اجعل ألستنا عامرة بذكرك، وقلوبنا بخشيتك، وأسرارنا بطاعتك، إنك على كل شيء قدير، حسبنا الله ونعم الوكيل
Updates through https://medatlax.com/Clinical/Level-11/EM/Emergency-Medicine within cs-ospe link - will be highlighted yellow
Collected from past batches 2015-2025; Lina Serhan, Maha Alasmari, Mayar Alhodaib, Mohammed AlMutairi, Khaled AlSaeed, Abdullah AlHamad, Yasser AlKhudairy, Amani Almalik, Sara Alramadhan, and Sadeem AlKharaan.
Emergency Medicine CS-OSPE
Table of Contents
Cases
- 1. Trauma & Acute Care
- 2. Toxicology
- 3. Cardiology
- 4. Respiratory
- 5. Gastroenterology & General Surgery
- 6. Endocrinology & Electrolytes
- 7. Neurology
OSPE
- Airway Management and Procedures
- Cardiovascular and ECG
- Trauma and Surgical Emergencies
- Radiology
- Pediatrics and Social
- Obstetrics and Gynecology
- Radiology and Imaging
Emergency Cases
1. Trauma & Acute Care
1.1. Trauma Approach & Surveys
Case Scenario: 22-year-old motorbike accident patient. Vitals: BP 80/60, HR 115, RR 19, SpO2 96%.
Q: What questions will you ask in the history? (SAMPLE)
- S: Symptoms (Nausea, vomiting, loss of consciousness, loss of vision, abnormal movements).
- A: Allergies.
- M: Medications.
- P: Past medical/surgical history (and Pregnancy if female).
- L: Last meal.
- E: Event / Environment (Mechanism of injury, e.g., airbag open, how many cars, speed, casualties, death, what did you hear?).
Q: What is the Primary Survey? (ABCDE) (MUST MENTION EVERYTHING HERE)
- A: Airway with C-spine immobilization (Intubation if patient is unconscious).
- B: Breathing
- C: Circulation and bleeding control
- D: Disability (GCS & Pupils)
- E: Exposure
- Adjuncts to Primary Survey: CXR, Pelvic X-ray, eFAST, Blood glucose level.
Q: What is the Secondary Survey?
- SAMPLE history
- Head-to-toe examination
- Adjuncts: X-ray (limbs), CT scan, blood tests, group & save, urine test.
1.2. eFAST (Extended Focused Assessment with Sonography in Trauma)
Q: What are the areas/views for eFAST?
- RUQ (Right Upper Quadrant / Hepatorenal)
- LUQ (Left Upper Quadrant / Splenorenal)
- Pelvic/Bladder (Suprapubic)
- Pericardial (Subxiphoid)
- Lung Scan
- (Note: FAST exam includes views 1–4; eFAST adds the Lung Scan).
Q: If eFAST is positive and the patient is hemodynamically unstable, what is the next step?
- Immediate Laparotomy (OR) (after surgery consultation).
1.3. Glasgow Coma Scale (GCS)
Q: What are the three components of GCS?
- Eye Opening (E)
- Verbal Response (V)
- Motor Response (M)
GCS Scoring Table:
| Score | Eye Opening (E) | Verbal Response (V) | Motor Response (M) |
|---|---|---|---|
| 6 | — | — | Normal / obeys command |
| 5 | — | Oriented & Converses | Localizes pain |
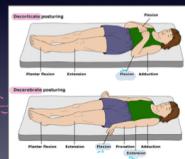
| 4 | Spontaneous | Confused | Withdraws to pain |
| 3 | To Speech | Inappropriate Words | Decorticate flexion |
| 2 | To Pain | Incomprehensible Sounds | Decerebrate extension |
| 1 | None | None | None |
Total Score = E + V + M (Range: 3–15)
Case Example:
- Scenario: Confused (4) + withdrawing from pain (4) + closed eyes (1) = 9.
1.4. Specific Trauma Injuries
Abdominal Trauma
- Q: What is the most common organ injured in blunt abdominal trauma?
- Spleen.
- Q: What are two clinical signs of retroperitoneal bleeding?
- Cullen’s Sign: Periumbilical ecchymosis.
- Grey-Turner’s Sign: Flank ecchymosis.
Head & Neck Trauma
- Q: What are signs of a basal skull fracture?
- Raccoon Eyes.
- Battle’s Sign.
- CSF Rhinorrhea.
- Bump.

Thoracic Trauma
- Q: Definition of Massive Hemothorax?
-
1500 ml of blood immediately after chest drain placement.
-
200 ml/hr of blood drained for 4 hours.
- CXR: Findings showing > 2/3 of available space in hemithorax.
-
Q: Initial treatment of Tension Pneumothorax?
- Immediate Treatment: Needle decompression (clinical diagnosis; do NOT wait for imaging as it will kill the patient).
- Needle Size/Site: 14G needle in the 2nd intercostal space (mid-clavicular line) or 5th intercostal space (mid-axillary line).
- Next step: Tube thoracostomy (Chest tube).
2. Toxicology
2.1. Paracetamol (Acetaminophen) Toxicity
Case Scenario: Young patient ingested 30 tablets (~11-15g) of Paracetamol.
Q: What investigations will you do?
- Serum Paracetamol Level, CBC, LFT, KFT (U&E), VBG, ECG, Co-ingestion screen, PT/INR/PTT.
Q: What is the toxic dose?
- Adults: Toxic Dose: 10 gram in total or 150 mg/kg
- Pediatrics: > 150 mg/kg
Q: What is the toxic metabolite?
- NAPQI.
Q: What is the antidote and its mechanism?
- Antidote: NAC (N-Acetylcysteine).
- Mechanism:
- Increases Glutathione stores/availability.
- Directly binds to NAPQI.
- Reduction of NAPQI back to acetaminophen.
Q: When should you measure the Paracetamol level?
- If ingestion < 4 hours ago: Wait and test at the 4-hour mark post-ingestion.
- If ingestion > 4 hours ago: Send level Immediately. Q: What are the indications for NAC?
- Serum level above the treatment line on the Nomogram.
- Serum level > 150 mcg/mL at 4 hours.
- Serum level > 10 mcg/mL with unknown ingestion time.
- Serum level results will not be back within 8 hours.
Q: Clinical Stages of Toxicity?
| STAGE | TIME COURSE | NAME | SYMPTOMS | SIGNS |
|---|---|---|---|---|
| 1 | 0 to 12 (up to 24 to 36) hours | Preinjury | Nausea, vomiting, anorexia, malaise | Elevated serum acetaminophen concentration |
| 2 | 8 to 36 hours | Liver injury | Nausea, vomiting, RUQ abdominal tenderness | Aminotransferase elevation (AST begins to rise 8 to 36 hours after ingestion) |
| 3 | 2 to 4 days | Maximum liver injury | Liver failure (encephalopathy, coagulopathy, hemorrhage, acidosis) | Hemorrhage, ARDS, sepsis/SIRS, multiorgan failure, cerebral edema |
| 4 | >4 days | Recovery | None | Complete hepatic histologic recovery |
Q: Role of Gastric Lavage?
- Rule: Not needed for Paracetamol.
- Reasoning: It is not a lethal drug and gastric lavage carries its own risks.
- Activated Charcoal 50g can be used within 1 hour of ingestion unless contraindicated. Q: Conditions causing decreased Glutathione stores?
- Chronic liver disease.
- Liver cirrhosis.
- Hepatitis.
- Infection.
- Diabetes.
- Pancreatitis.
- Parkinson’s disease.
- Malnutrition.
2.2. Aspirin (Salicylate) Toxicity
Q: What is the toxic dose?
- 150–300 mg/kg.
Q: What is the classic acid-base disturbance?
- Primary Respiratory Alkalosis.
- Followed by High Anion Gap Metabolic Acidosis.
- Respiratory Acidosis.
Q: What is the management?
- Antidote: Sodium Bicarbonate (for Urinary Alkalinization).
- Dialysis Indications: Coma, Hepatic failure, Pulmonary edema, Severe acid-base imbalance.
- Activated Charcoal: Useful if within 1 hour.
- IV Dextrose: If patient is hypoglycemic.
- Correct Hypokalemia (IV K+).
2.3. Iron Toxicity
Case Scenario: 7-year-old male ingested 30 tablets of iron.
Q: What are the clinical phases?
| Phase | Timeframe | Clinical Features | Mechanism of Toxicity |
|---|---|---|---|
| 1 | Gastrointestinal (≤6 hours) | • Vomiting • Diarrhea • Hematemesis • Hematochezia | Corrosive effect of iron on gastrointestinal mucosa |
| 2 | Latent (6-24 hours) | • Resolution of GI symptoms • Tachycardia • Acidosis • Depressed mental status | Ongoing cellular toxicity and organ damage |
| 3 | Systemic (12-24 hours) | • Return of GI symptoms • Metabolic acidosis • Leukocytosis • Coagulopathy • Renal failure • Lethargy or coma • Cardiovascular collapse | Iron distributes to tissues with worsening cellular toxicity |
| 4 | Hepatic (2-5 days) | • Fulminant liver failure • Coagulopathy | Rapid absorption from portal system with oxidative damage |
| 5 | Obstructive (3-6 weeks) | • Pyloric or bowel scarring • Obstruction | Healing of injured gastrointestinal mucosa |
Q: What is the preferred decontamination method?
- Whole Bowel Irrigation (WBI).
Q: What is the antidote?
- Deferoxamine.
Q: Indications for Antidote?
- Severe symptoms.
- High Anion Gap Metabolic Acidosis.
- Serum Iron > 500 mcg/dL.
- Significant number of pills visible on abdominal X-ray.
3. Cardiology
3.1. Ischemic Heart Disease (MI)
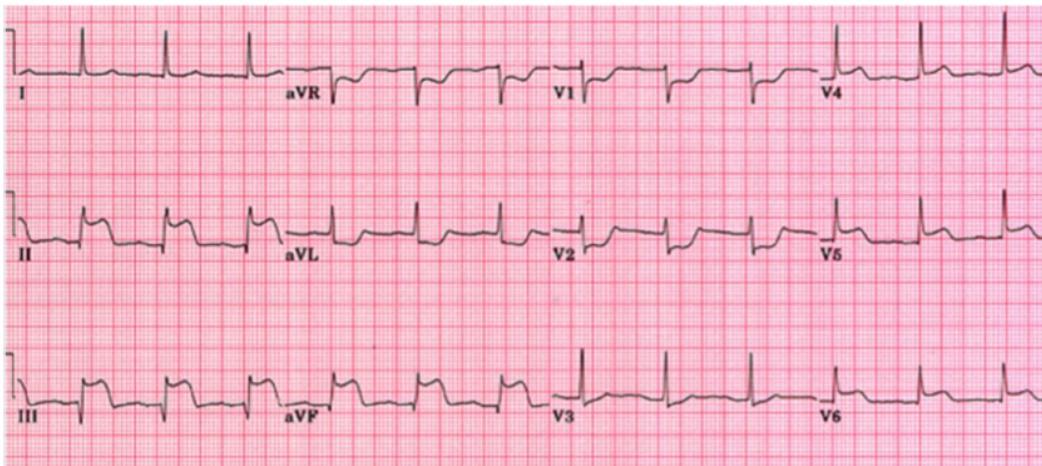
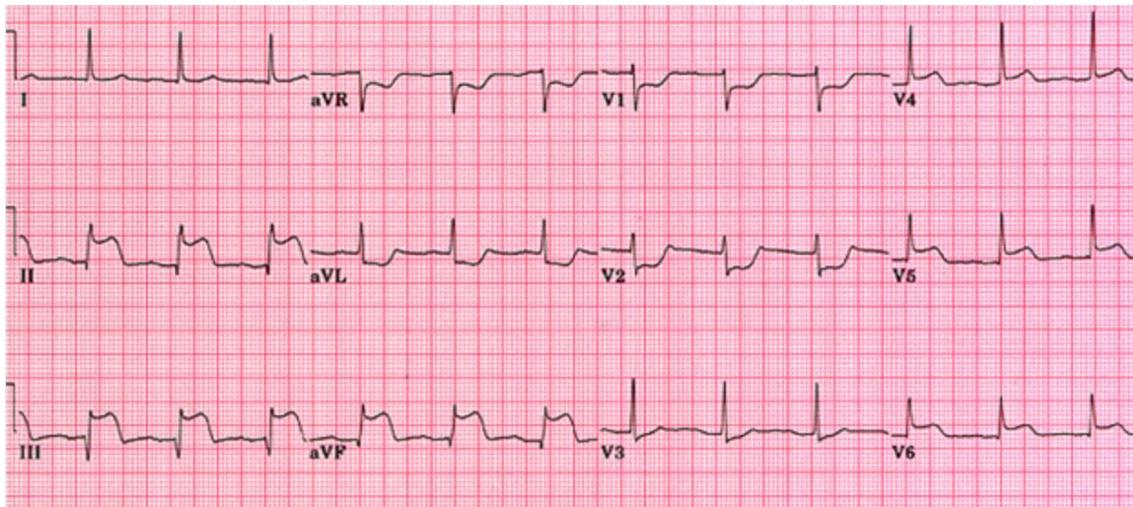
Case Scenario: 60-year-old male with DM/HTN, chest pain for 4 hours. ECG shows ST elevation in II, III, aVF.
Q: History Taking (Chest Pain - SOCRATES)
- S: Site
- O: Onset
- C: Character
- R: Radiation
- A: Associated symptoms (nausea, sweating, SOB)
- T: Timing/Duration
- E: Exacerbating/Relieving factors
- S: Severity
- Plus: Risk factors (Is HTN and DM controlled on medications?, Smoking history), Allergies, Medications.
Q: ECG Findings & Diagnosis?
- Findings: ST Elevation in II, III, aVF. ST depression in V1, V2 (reciprocal).
- Diagnosis: Inferior STEMI (possibly with Posterior extension).
Q: Investigations?
- ECG, Cardiac Biomarkers (Troponin), CXR, CBC, U&E, VBG, D-Dimer, BNP.
Q: Management?
- Immediate: MONA (Morphine (unless contraindicated), Oxygen (if sat <95%), Nitroglycerin, Aspirin 324mg - reduces mortality).
- Antiplatelets: Clopidogrel (Plavix) 300mg.
- Definitive: Cath Lab (PCI).
- Door to ECG time: < 10 min.
- Note: Nitroglycerin is contraindicated/used with caution in Hypotensive patients.
Q: Life-Threatening Causes of Chest Pain?
- Acute Coronary Syndrome (MI)
- Aortic Dissection
- Pulmonary Embolism
- Tension Pneumothorax
- Esophageal Rupture
- Cardiac Tamponade
- Pericarditis
3.2. Aortic Dissection
Case Scenario: 70-year-old male with sudden severe tearing abdominal and back pain. Exam: Hypotension, pulsatile abdominal mass, and BP difference between the arms.
Q: Diagnosis / Investigations?
- CXR: Wide mediastinum, deviated trachea, loss of aortic knob contour, double calcium sign, Pleural effusion, Left apical cap.
- Definitive: CT Angiogram (Aorta), Aortography.
- Bedside: TEE (Transesophageal Echocardiogram).
- Other Imaging: MRI.
Q: Ultrasound Findings?
- Intimal flap (linear structure).
- True and False lumen: Exhibit different hemodynamic characteristics and flow patterns on Doppler.
- Thrombus in false lumen.
- Pericardial effusion.
- Aortic regurgitation.
Q: Why is there a BP difference between the arms?
- Pathophysiology: Involvement of the subclavian artery or brachiocephalic trunk by the dissection flap reduces flow to one arm.
Q: Pharmacological goals in the ER?
- Goal: Anti-impulse therapy (decrease HR and shear force).
- 1st Line: IV Beta-blocker (e.g., Esmolol).
- 2nd Line: IV Vasodilator (e.g., Nitroprusside) — only after beta-blockade.
- Targets: HR 60–70 bpm and SBP 100–120 mmHg.
Q: Definitive Treatment?
- Emergent Surgical Repair (Open or EVAR).
3.3. Pulmonary Embolism (PE)
Case Scenario: Female on OCPs, SOB, hemoptysis, tachycardia.
Q: Investigations?
- Gold Standard: CT Pulmonary Angiogram (CTPA) (Spiral CT).
- Others: Pulmonary Angiography, D-Dimer (rule out in low risk), V/Q Scan (if renal failure/pregnancy), CXR, ECG.
Q: Management?
- Stable: Anticoagulation (Heparin/LMWH).
- Unstable (Hypotension/Arrest/Shock/Massive PE): Thrombolytics (tPA), Embolectomy (Catheter/Surgical), or IVC Filter.
4. Respiratory
4.1. Pneumonia
Case Scenario: 50 yrs female known case of DM on oral hypoglycemia ,complained for 2 days of fever , cough , SOB ,greenish sputum =38 ,RR=24 ,P=110, O2 sat =90 % , chest sound cripetation Rt lower zone with bronchial Breathing
Q: Diagnosis & Management?
- Dx: Community Acquired Pneumonia (CAP).
- Investigations: CBC, ESR, CRP, Chest X-ray, Blood Gas (VBG/ABG), Blood Culture, U&E, Random Blood Sugar.
- Tx: Oxygen, IV Fluids, Antibiotics (Broad spectrum).
- Complications: Septicemia with Septic Shock, Pleural Effusion, Pneumothorax, Respiratory Failure.
4.2. Shortness of Breath (History)
- History: Onset, trigger, associated symptoms (chest pain, fever), Past Medical Hx, Allergies, Social (Smoking/Animals).
- DDx: Asthma, COPD exacerbation, Pneumonia, PE, Pneumothorax, Heart Failure.
Q: Investigations?
- Spirometry, VBG/ABG, Chest X-ray, CBC, ECG.
Q: Management?
- Oxygen.
- Treat the underlying cause.
whats management sequence for asthma attacks?
5. Gastroenterology & General Surgery
5.1. Appendicitis / Acute Abdomen
Case Scenario: Young patient, periumbilical pain radiating to Right Iliac Fossa (RIF).
Q: Differential Diagnosis?
- General: Appendicitis, Mesenteric Ischemia.
- Female: Ectopic Pregnancy, Ovarian Torsion, Ruptured Ectopic.
- Male: Testicular Torsion.
Q: Investigations?
- Labs: CBC (Leukocytosis), CRP, Urinalysis, Beta-hCG (females), LFT, U&E, Serum Amylase/Lipase, Blood Glucose.
- Imaging/Others: Ultrasound (preferred in peds/female), CT Abdomen/Pelvis (gold standard), Abdominal X-Ray Erect, ECG (to rule out MI).
Q: What is the management?
- NPO.
- IV Fluids.
- Analgesia: The most important step; must prioritize pain control (e.g., Morphine).
- Antibiotics (Pre-operative).
- Examination (Reassessment).
- Disposition: Admission for General Surgery / Immediate Surgery Referral. Q: Life-Threatening/Common Causes of Epigastric Pain? (Mention at least 3)
- Inferior MI.
- Peptic Ulcer Disease (PUD).
- GERD.
- Pancreatitis.
- Lower lobar pneumonia.
- Sickle Cell Anemia (SCA) crisis.
Q: Life-Threatening Causes of Abdominal Pain (Elderly)?
- Ruptured AAA (Abdominal Aortic Aneurysm).
- Perforated Viscus (Peptic Ulcer).
- Bowel Obstruction.
- Inferior MI.
- Pancreatitis.
- Appendicitis.
5.2. Bowel Obstruction & Perforation
- Obstruction X-ray: Air-fluid levels, dilated loops.
- Perforation X-ray: Free air under the diaphragm.
6. Endocrinology & Electrolytes
6.1. Diabetic Ketoacidosis (DKA)
Case Scenario: Type 1 DM, missed insulin, Kussmaul breathing, dehydration. - Young male , c/o epigastric pain glucocheck was 25 mmol Labs: pH 7.25, PCO2 25, HCO3 10.
Q: Diagnostic Criteria?
- Hyperglycemia: > 250 mg/dL (Adults > 750 mg/dL, Pediatrics > 200 mg/dL).
- Acidosis: pH < 7.3, HCO3 < 15.
- Ketosis: Ketonemia or Ketonuria.
- Anion Gap: High (> 12).
Q: Anion Gap Calculation?
- Formula:
- Example Calculation: (High Anion Gap).
Q: Management Steps?
- IV Fluids (Bolus) - Critical first step.
- Potassium Correction (Correct K+ before giving insulin).
- IV Insulin (0.1 units/kg/hr).
- Dextrose (added when blood sugar drops).
- Treat precipitating cause (Infection, missed dose/meal, stress, puberty, insulin pump malfunction, substance abuse).
Case Scenario: Middle-aged patient with intermittent chest discomfort and weakness. Labs: Hyponatremia (Hypovolemic hypotonic subtype), Hypokalemia. ECG: ST depression, Flat T wave, U wave.
Q: Management sequence for Hyponatremia?
- If Na continuously drops (e.g., 105) and patient starts seizing/confused: 3% Hypertonic Saline (100 mL bolus).
- General Correction: Isotonic saline + Potassium replacement (volume resuscitation first).
6.2. Hyperkalemia
Case Scenario: Renal failure patient, missed dialysis for 3 weeks, general fatigue. Labs: K+ 7, Na+ 142.
Q: ECG Changes?
- Tall Peaked T waves (Hyperacute T waves).
- Prolonged PR interval, Loss of P wave.
- Wide QRS, ST elevation (pseudoinfarction pattern).
Q: Management Hierarchy? First Line
- Salbutamol nebulization / ventolin: Shifts K into the cells. Effect appears within 20-30 minutes.
Second Line
- Insulin and Glucose /Dextrose infusion: Shifts K into cells. Effect appears within 10-20 minutes.
Third Line
- Furosemide: Excretes K through renal tubules. Effect appears within 60-120 minutes.
- Calcium Gluconate (or Calcium Chloride - 3x more potent): Given in moderate to severe hyperkalemia to stabilize cardiac conduction. Z (ECG CHANGES GIVE IMMEDIATLY)
- Calcium Resonium (Kayexalate): Antagonizes K effect. Effect appears within 60-120 minutes. Z (PROTECT HEART AND ORGANS AGAINST K EFFECT)
Finally Excretion: Hemodialysis (Definitive).
Q: Causes of Hyperkalemia?
- Increase intake.
- Decrease excretion (e.g., Renal failure, missed dialysis, Adrenal insufficiency/Addison’s disease).
- Increase intracellular shift (e.g., Burn, Rhabdomyolysis, Dehydration).
- Medications (Beta Blockers, ACE Inhibitors).
- Lab Error.
Q: What is the normal level of potassium?
- 3.5 – 5.5 mmol/L.
6.3. Hypokalemia
Case Scenario: …
Q: What is the diagnosis?
- Definition: Serum potassium < 3.5 mEq/L (or < 3.4 mmol/L in pediatrics).
Q: What are the ECG changes of hypokalemia?
- T wave inversion, ST depression, and prominent U waves.
- Other changes: Prolonged PR/heart block, atrial fibrillation, ventricular fibrillation, and Torsades de pointes.
Q: Causes of hypokalemia?
- Decreased intake: Malnutrition.
- GI losses: Vomiting, diarrhea.
- Renal losses: Diuretics, RTA, hyperaldosteronism.
- Transcellular shifts: Alkalosis, insulin, beta-agonists (albuterol).
Q: What is the treatment? Very Important: Ensure intact urine output prior to administration of intravenous potassium. Close cardiac monitoring is critical. Z
- Oral: 40 to 60 mEq KCl every 2 to 4 hours (for stable patients > 3.0 mEq/L).
- IV: 10 to 20 mEq/hr (for severe < 2.5 mEq/L or symptomatic patients).
- Note: Ensure intact urine output and monitor rhythm; replace Magnesium concurrently.
7. Neurology
7.1. Headache & Meningitis
Q: History Taking (Headache)?
- SOCRATES.
- Associated Symptoms: Neck pain, Photophobia, Phonophobia, Nausea/Vomiting, Blurred vision, Nasal Congestion, Altered mental status.
Q: Investigations (Headache)?
- CT scan, CBC, Electrolytes, CRP, ESR, Tonometry.
Q: Treatment of Cluster Headache?
- 100% Oxygen.
- Sumatriptan.
Q: Serious Causes of Headache?
- Subarachnoid Hemorrhage (SAH).
- Meningitis.
- Tumor / Mass Effect.
- Giant Cell Arteritis.
- Stroke.
- Brain Aneurysm.
- Sinusitis.
- Increased ICP.
Q: Headache Examination?
- Full Neurologic Assessment, Babinski sign, Kernig and Brudzinski’s sign, Gait testing, Cranial nerves, Fundoscopy (Papilledema).
Q: Differential Diagnosis (Headache/Fever)?
- Meningitis.
- Encephalitis.
- Brain Abscess.
- Sinusitis.
- Migraine.
- Cluster Headache.
Q: Meningitis Investigations & Management?
- Priority Sequence: CT Head → LP → IV Antibiotics.
- CT Head: Must be done before LP if signs of increased ICP (Papilledema, focal deficit) to avoid herniation. ✓ Papilloedema ✓ focal neurological deficit ✓ abnormal conscious state if you suspect pt has high ICP do CT or MRI before LP to avoid Herniation
- Lumbar Puncture (LP):
- Bacterial Findings: High Protein, Low Glucose, High WBC (> 500, 90% PMN), Turbid appearance, Gram Stain.
- Treatment: IV Antibiotics.
7.2. Lumbar Puncture (LP)
Q: Indications?
- Meningitis, Encephalitis.
- Subarachnoid Hemorrhage (SAH).
- Benign Intracranial Hypertension.
- Multiple Sclerosis (MS).
- Seizure (Brain seizure).
Q: Complications?
- Post-LP Headache.
- Infection.
- Bleeding (Hematoma / Epidural Hematoma).
- Brain Herniation (if ICP is high).
- Nerve root puncture.
- Worsening of meningitis.
7.3. Subarachnoid Hemorrhage (SAH)
Q: Diagnosis?
- CT Brain (Non-contrast).
- LP (if CT is negative but suspicion remains high).
7.4. Seizure
Case Scenario: 20-year-old male brought to ER by family because he is seizing.
Q: What will you ask in history?
- Description of the event: Onset (abrupt vs. gradual), duration, and nature of movements (stiffening, jerking, automatisms).
- Associated features: Tongue biting, urinary/fecal incontinence, fall/injury.
- Post-ictal state: Confusion, headache, muscle pain, or deep sleep (todd’s paralysis).
- Provoking factors: Missed medications (compliance), sleep deprivation, fever/infection, head trauma, substance abuse/alcohol.
- Background: Family history of epilepsy, past medical history (previous seizures), and current medications (antiepileptics).
Q: What investigations will you ask for?
- Bedside: Random Blood Glucose (exclude hypoglycemia).
- Labs: CBC, Electrolytes (Na, Ca, Mg), Renal/Liver function, Toxicology screen (if suspected overdose).
- Imaging: CT Brain (Non-contrast) to rule out acute hemorrhage, tumor, or trauma in the ER. MRI is preferred for long-term structural evaluation.
- Neurophysiology: EEG (gold standard for diagnosis and classification, though may be normal interictally).
Q: How will you treat this patient?
- Safety First: Position the patient (recovery position), protect the head, and do NOT put anything in the mouth.
- Acute Management (Stop the Seizure):
- First-line: Benzodiazepines (e.g., IV Lorazepam, IV Diazepam, or IM Midazolam) to abort the attack.
- Prevention of Recurrence:
- Load with anti-epileptic drugs (AEDs) such as Phenytoin (Epanutin), Valproate, or Levetiracetam.
- Status Epilepticus: If seizure lasts >5 mins (or two seizures without regaining consciousness), follow the status epilepticus protocol (Airway management, IV/IO access, and tiered drug therapy).
revise diagnosis and management of types of shock, asthma, meningitis, pneuomothorax, tdm2
unstable pelvis? Answer :pelvic binder
Airway Management and Procedures
Head Tilt-Chin Lift Maneuver
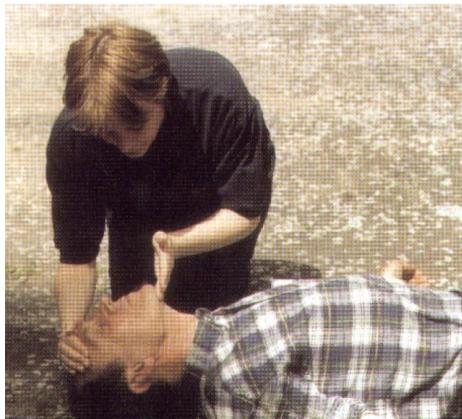

- Name of Maneuver: Head tilt-chin lift maneuver.
- Aim/Purpose: To open the airway in non-traumatic or unconscious patients.
- Indication: Unconscious patient with no suspicion of C-spine injury.
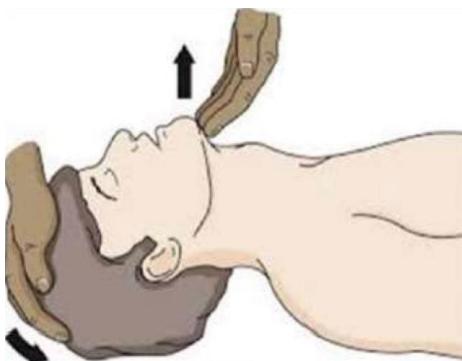
Jaw Thrust Maneuver

- Name of Maneuver: Jaw thrust maneuver.
- Indication: Used to open the airway in patients with suspected trauma (e.g., C-spine injury) or where the mechanism of injury is unknown.
- Advantage: Minimizes movement of the cervical spine while opening the airway.
Oropharyngeal Airway (OPA)


- Name of Equipment: Oropharyngeal airway (Guedel airway).
- Indications:
- To maintain the airway in unconscious patients.
- Used as a bite block for unresponsive patients.
- Helps prevent the tongue from obstructing the airway.
- Sizing: Measure from the corner of the mouth to the angle of the mandible.
- Complications/Risks:
- Too small: The tongue may still obstruct the airway.
- Too large/deep: May injure the airway or push the epiglottis over the glottic opening.
- Insertion Methods:
- Direct: Using a tongue depressor to move the tongue out of the way.
- Indirect: Inserting the airway upside down and rotating it 180° into position (adults only).
- Contraindications: Conscious or semi-conscious patients with an intact gag reflex (can induce vomiting and aspiration).
- Pediatric Note: Never use the indirect (rotation) method in children, as it may damage the soft and hard palate.
Nasopharyngeal Airway (NPA)


- Name of Equipment: Nasopharyngeal airway (Nasal trumpet).
- Indications: To maintain an airway in conscious or semi-conscious patients who may still have a gag reflex.
- Sizing: Measure from the nostril to the tragus or pinna of the ear.
- Insertion: Use lubricant before insertion.
- Contraindications:
- Maxillofacial fractures.
- Basal skull fractures (due to the risk of intracranial entry).
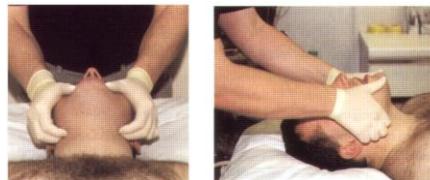
Bag-Valve-Mask (BVM) Ventilation




- Name of Equipment: Bag-Valve-Mask (BVM).
- Purpose: To ventilate a patient who is not breathing or is breathing inadequately.
- Components: Mask (apex and base), self-inflating bag, oxygen reservoir.
- Technique:
- C-E Clamp Method: Use the thumb and index finger to form a ‘C’ to seal the mask, while the other fingers form an ‘E’ to lift the mandible.
- Ensure a tight seal to prevent leaks.
- Risks: Excessive volume or pressure can increase gastric pressure, inducing vomiting and aspiration.
- Efficiency: Can provide up to 90-100% FiO2 when connected to a high-flow oxygen source.
Laryngeal Mask Airway (LMA)



- Name of Equipment: Laryngeal Mask Airway (LMA).
- Indications:
- Management of a difficult airway.
- Failure of BVM ventilation.
- Temporary airway during anesthesia or prehospital care.
- Contraindications:
- Airway obstruction.
- Inability to open the mouth.
- Pharyngeal pathology or thoracic injury.
- Key Notes:
- Not a definitive airway (does not prevent aspiration).
- Temporary and easier to insert than an endotracheal tube.
- Useful in obese or short-necked patients where vocal cords are hard to visualize.
Endotracheal Tube (ETT) and Intubation
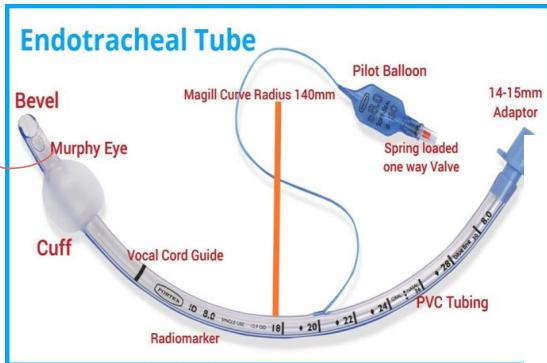
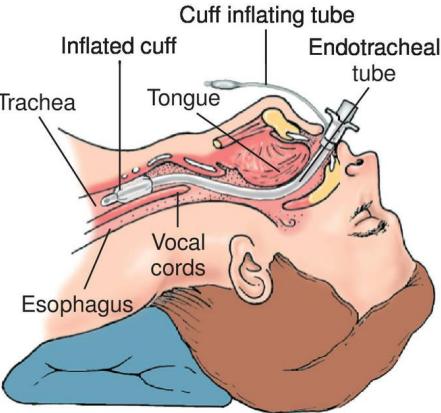

- Name of Equipment: Endotracheal Tube (ETT).
- Purpose: To maintain a definitive airway, provide maximum oxygenation/ventilation, and prevent aspiration.
- Indications:
- GCS (unable to protect airway).
- Comatose patients or cardiac arrest.
- Respiratory failure.
- Sizing:
- Female: 7.0 - 7.5 mm.
- Male: 7.5 - 8.0 mm.
- Note: If a stylet is used, it shouldn’t pass the Murphy eye.
- Confirmation of Placement:
- Primary (Clinical):
- Chest rise.
- Seeing the tube pass through the vocal cords.
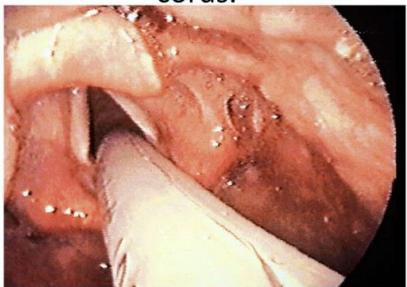
 - Chest rise.
- Bilateral breath sounds (5-point auscultation: epigastrium first, then left/right bases and axillae).
- Chest rise.
- Bilateral breath sounds (5-point auscultation: epigastrium first, then left/right bases and axillae). - CO2 fog inside the tube.
- Secondary (Equipment):
- Capnography/ETCO2 detector (Gold standard).
- Pulse oximetry.
- ABG.
- Chest X-ray (to verify tip position above the carina).
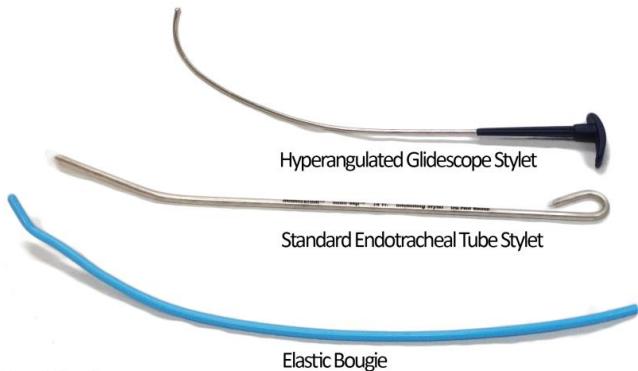
Intubation Adjuncts (Laryngoscopes & Stylets)
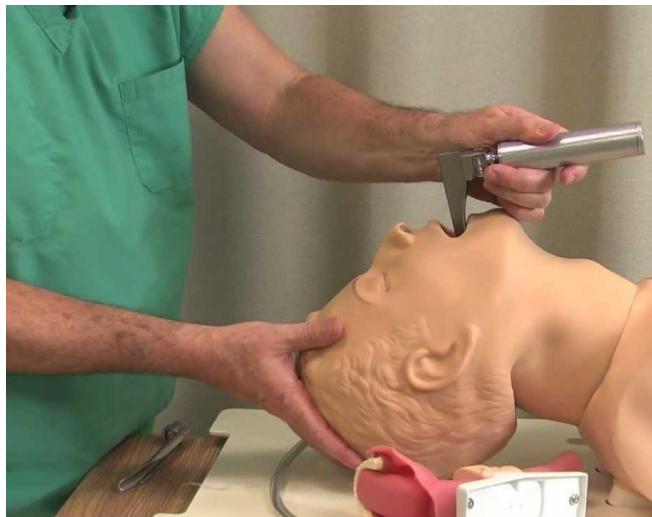




- Laryngoscope: Used to visualize the glottis during intubation.
- Curved (Macintosh) blade: Standard for adults.
- Straight (Miller) blade: Preferred for pediatrics or difficult adult cases.
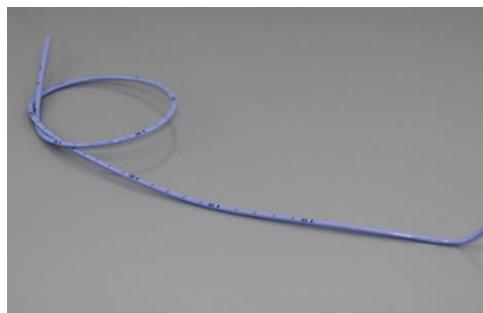
- Elastic Gum Tube (Bougie):
- Indication: Used for difficult airway management (when only the epiglottis is visible).
- Technique: Inserted blindly into the trachea; the user feels for tracheal rings or resistance at the carina. The ETT is then railroaded over it.
- Video Laryngoscope (Glidescope): Uses a camera to assist in visualizing a difficult airway.
Colorimetric ETCO2 Detector



- Name of Device: Colorimetric End-Tidal CO2 (ETCO2) detector.
- Purpose: Used to confirm correct endotracheal tube placement.
- Interpretation:
- Yellow/Gold: Success (CO2 detected, tube is in the trachea).
- Purple/Blue: Failure (No CO2 detected, tube likely in the esophagus).
- Grey: Indicates low ventilation; repeat the cycle.
- Exceptions (False Readings):
- False Positive: Yellow color despite esophageal placement (e.g., patient recently consumed carbonated beverages).
- False Negative: Purple color despite correct tracheal placement (e.g., in low-perfusion states like cardiac arrest).
Quantitative Waveform Capnography

- Purpose: Continuous monitoring of ETT placement and CPR quality.
- Clinical Use:
- Confirms ETT placement.
- CPR Quality: If ETCO2 is mmHg, chest compressions are likely inadequate.
- ROSC: A sudden, significant increase in ETCO2 indicates Return of Spontaneous Circulation.
- Failure to achieve ETCO2 mmHg after 20 minutes of CPR may be considered as a factor in ending resuscitative efforts.
Cardiovascular and ECG
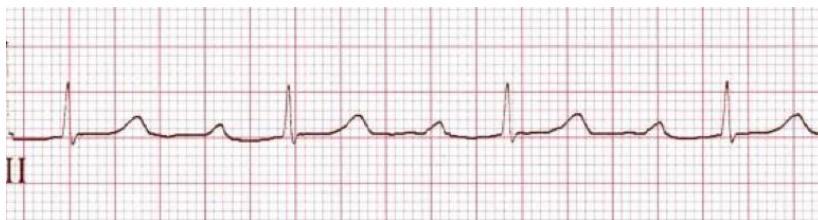
Normal Sinus Rhythm
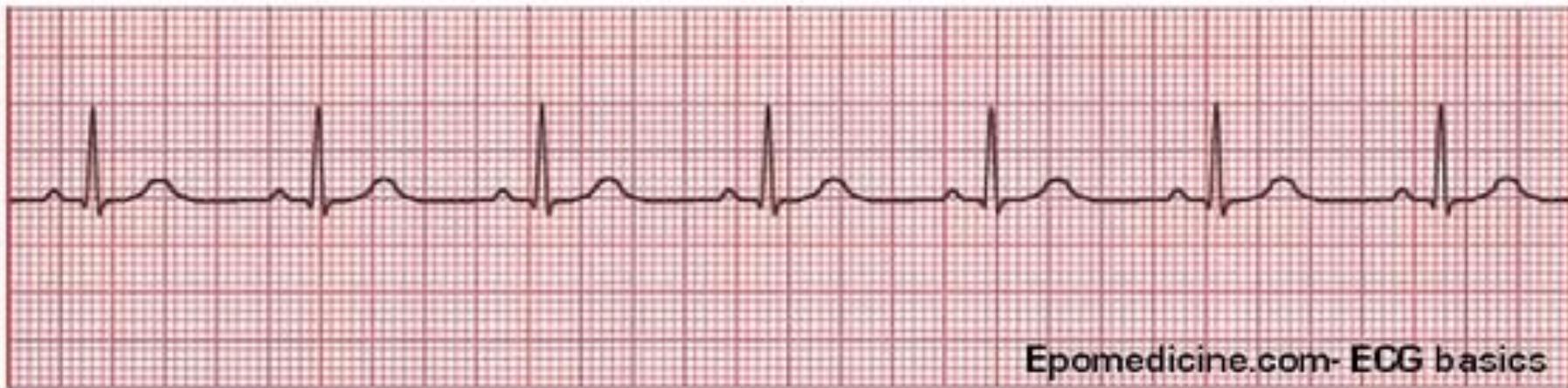
- Rate: 60–100 bpm.
- Rhythm: Regular.
- P Waves: Upright and uniform, one before every QRS.
- PR Interval: Normal (0.12–0.20 sec).
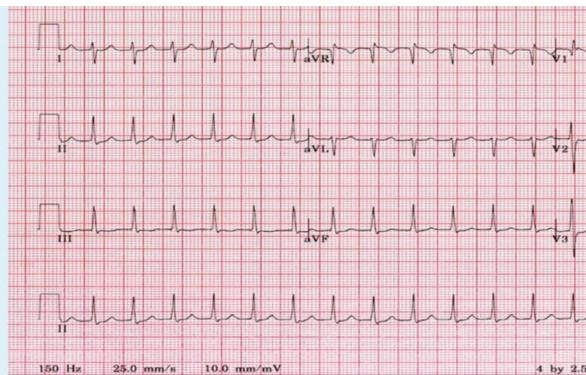
Atrial Fibrillation (AFib)
- Diagnosis: Atrial Fibrillation.
- ECG Findings:
- Irregularly irregular rhythm.
- No P waves (replaced by fibrillatory waves).
- Narrow QRS complexes.
- Treatment:
- Stable: Medications (Beta-blockers or Calcium Channel Blockers for rate control).
- Unstable: Synchronized cardioversion.
- PEA/Pulseless: CPR and Epinephrine.
Atrial Flutter

- Diagnosis: Atrial Flutter.
- ECG Findings: “Sawtooth” appearance of F-waves.
- Management: Check for pulse and stability; management similar to AFib.
Multifocal Atrial Tachycardia (MAT)
- Diagnosis: Multifocal Atrial Tachycardia.
- Treatment: Treat the underlying cause (e.g., hypoxia/COPD).
Supraventricular Tachycardia (SVT)
- Diagnosis: Supraventricular Tachycardia.
- ECG Findings:
- Regular rhythm, narrow QRS.
- Tachycardia (often bpm).
- P waves often not visible.
- Treatment: if + pulse check stability
- Stable: Vagal maneuvers (e.g., Valsalva), Adenosine (6mg, then 12mg).
- Unstable (e.g., BP 70/60, pulse 130): Synchronized cardioversion.
- Note: If no pulse, follow the PEA/Asystole protocol.
Ludwig’s Angina

- First Management Steps:
- Secure the Airway.
- Start Broad-spectrum IV Antibiotics.
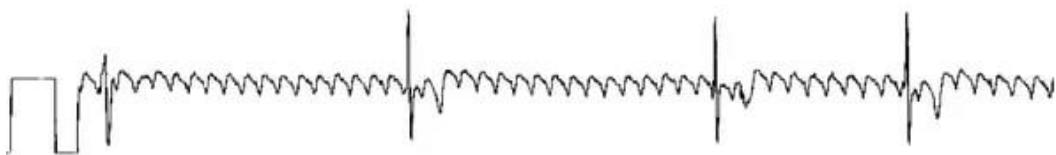
Ventricular Tachycardia (VT)
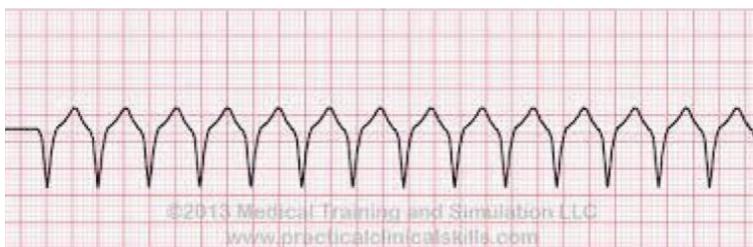
- Diagnosis: Ventricular Tachycardia.
- ECG Findings: Wide, monomorphic QRS complexes; usually regular.
- Management:
- First Step: Check for Pulse.
- Pulseless: Immediate CPR and Defibrillation (Unsynchronized).
- Pulse + Stable: IV Antiarrhythmics (Amiodarone, Procainamide, or Sotalol).
- Pulse + Unstable: Defibrillation/Cardioversion.
Ventricular Fibrillation (VF)
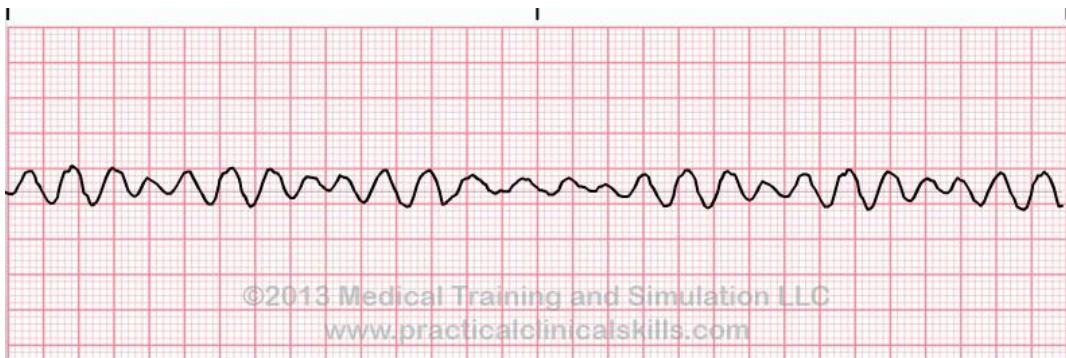
- Diagnosis: Ventricular Fibrillation.
- ECG Findings: Disorganized, chaotic electrical activity; no discernible waves.
- Management: if stable Stable: medications (antiarrhythmia as IV procainamide, IV amiodarone, IV sotalol). if unstable Immediate CPR and Defibrillation. Administer Epinephrine and Amiodarone/Lidocaine as per ACLS.
Torsades de Pointes
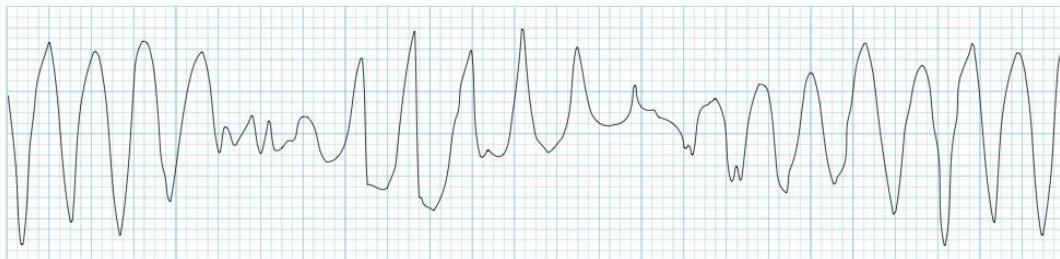
- Diagnosis: Torsades de Pointes.
- ECG Findings: “Twisting of the points”; polymorphic ventricular tachycardia.
- Risk Factors/Causes:
- Hypomagnesemia (most common).
- Hypokalemia, Hypocalcemia.
- QT-prolonging drugs.
- Treatment: IV Magnesium Sulfate. + Treat the underlying electrolyte imbalance.
Heart Blocks (Atrioventricular Blocks)
| Type | PR Interval | R-R Rhythm |
|---|---|---|
| 1st Degree | Fixed, prolonged () | Regular |
| 2nd Degree Mobitz I | Progressive prolongation until a QRS is dropped | Irregular |
| 2nd Degree Mobitz II | Fixed PR interval, but some QRS complexes are dropped | Irregular |
| 3rd Degree (Complete) | Variable (P waves and QRS are independent) | Regular |
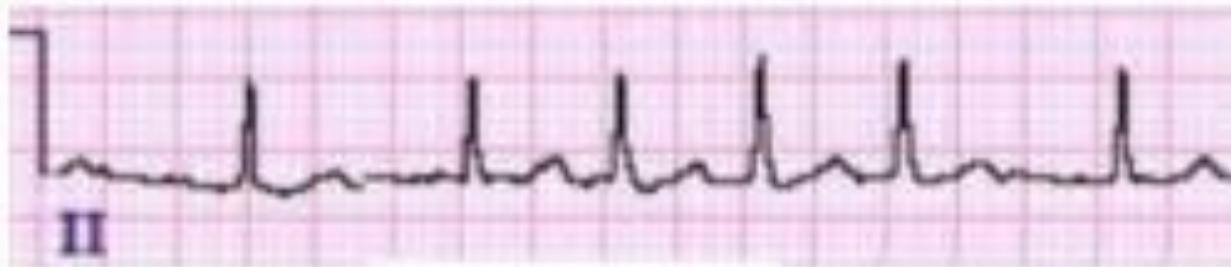
1st Degree AV Block

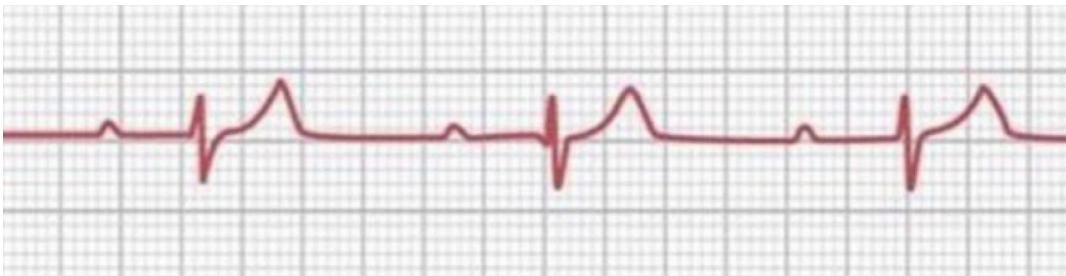
- Describe the abnormality in this ECG?
- Regular RR, fixed prolonged PR interval.
- Management: For asymptomatic patients, discharge and refer to outpatient cardiology.
2nd Degree AV Block (Mobitz I / Wenckebach)
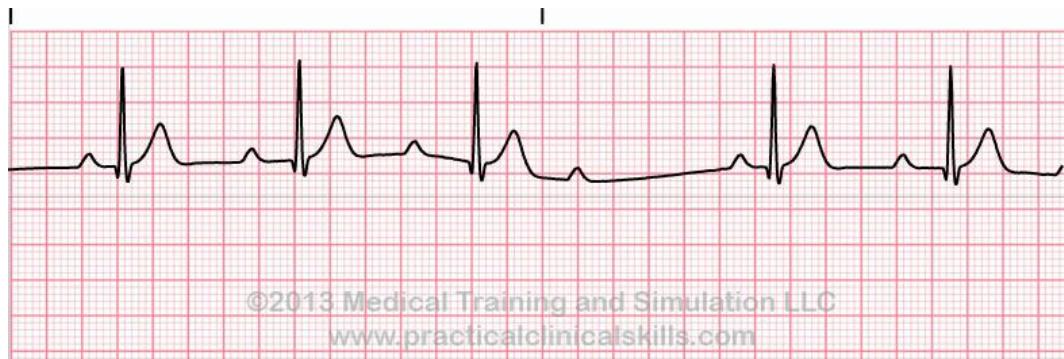
- Irregular RR, variable PR interval.
2nd Degree AV Block (Mobitz II)

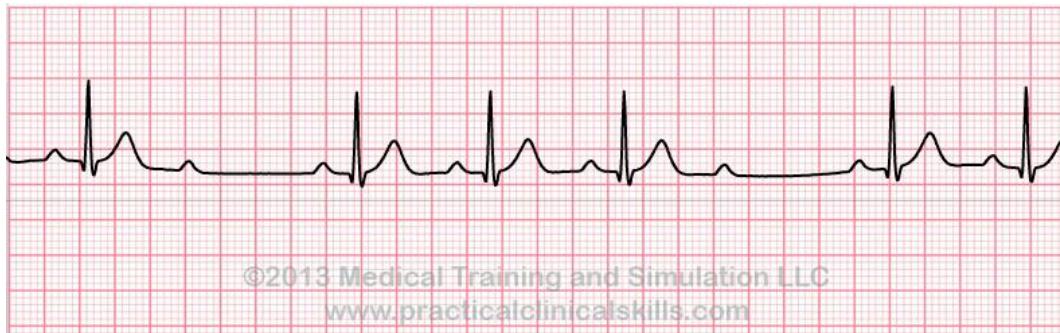
- Irregular RR, fixed PR interval.
- Management: Usually requires a pacemaker.
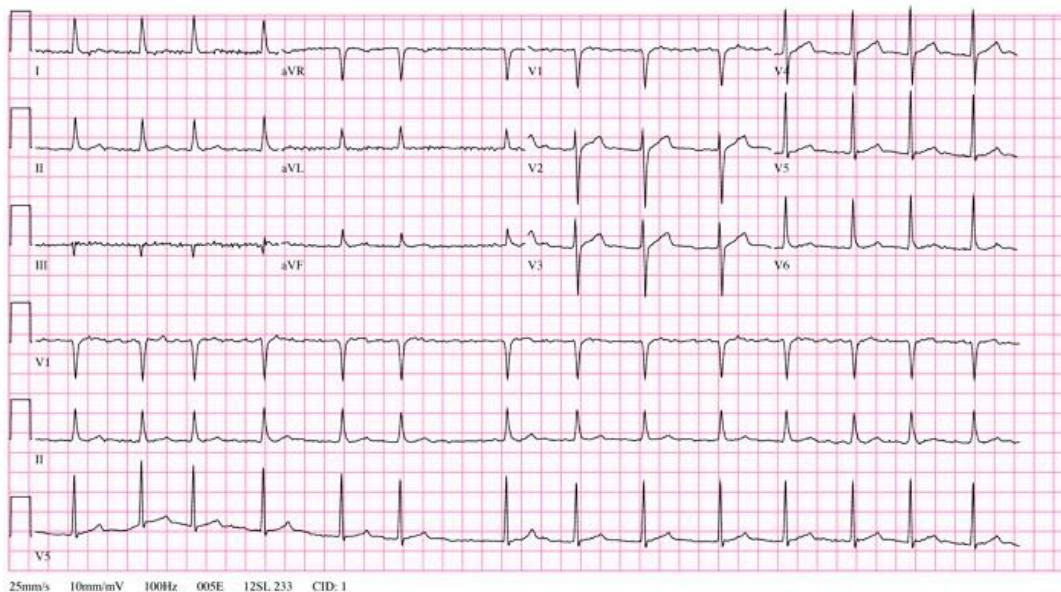
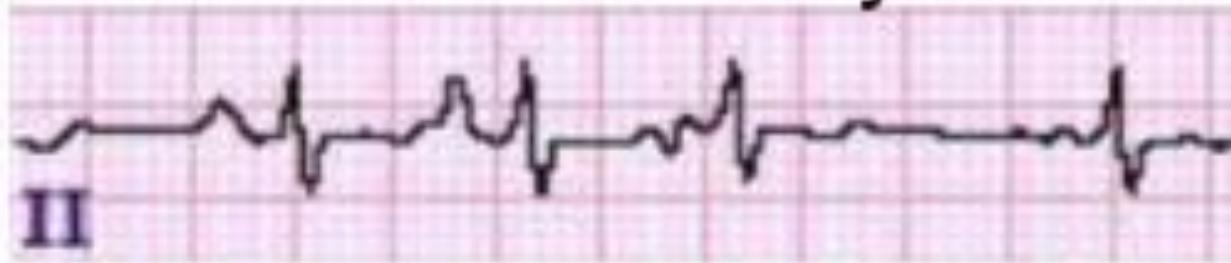
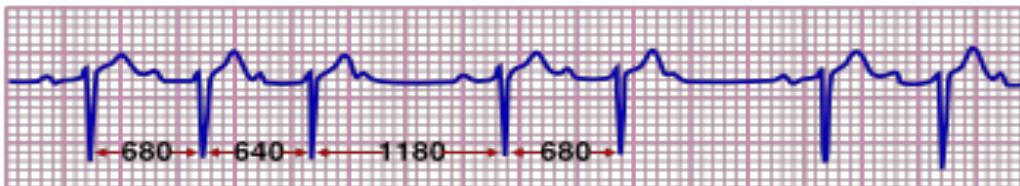
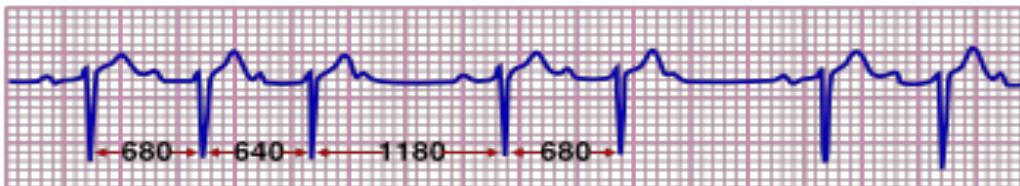
3rd Degree (Complete) AV Block
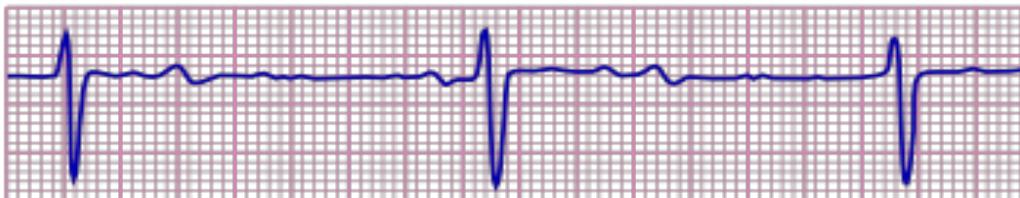
-
What is the diagnosis?
- 3rd degree heart block.
-
Describe the ECG abnormality?
- Regular RR, variable prolong PR interval.
-
Management: Pacemaker (indicated even if asymptomatic).
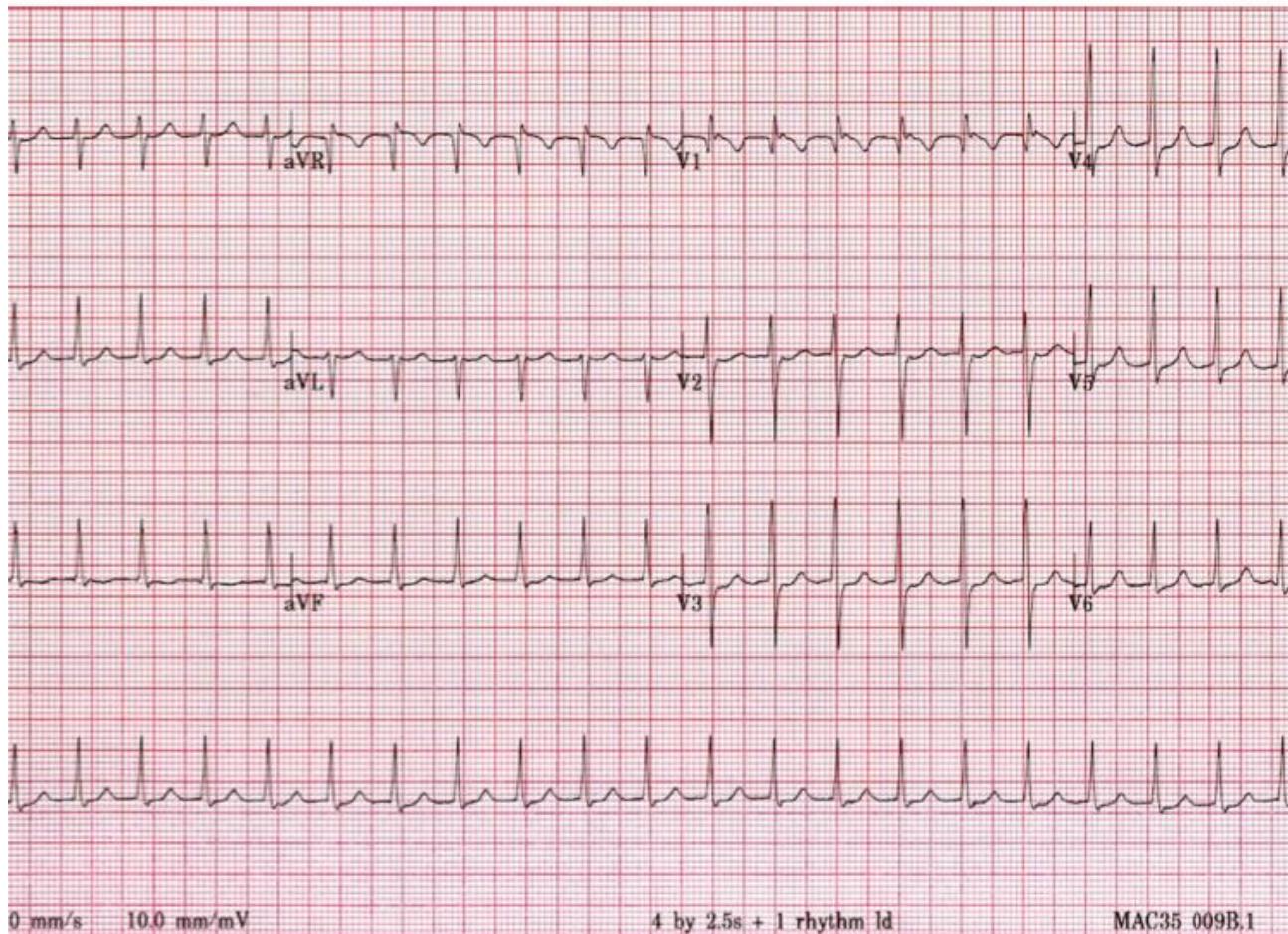
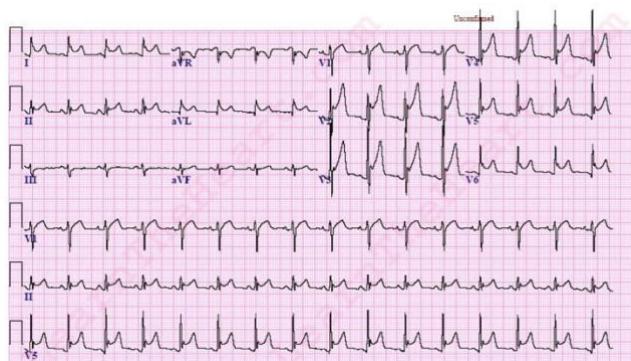
Acute Coronary Syndrome (ACS)
- STEMI: ST elevation in contiguous leads + positive troponin + chest pain.
- NSTEMI: No ST elevation (may have ST depression/T-wave inversion) + positive troponin + chest pain.
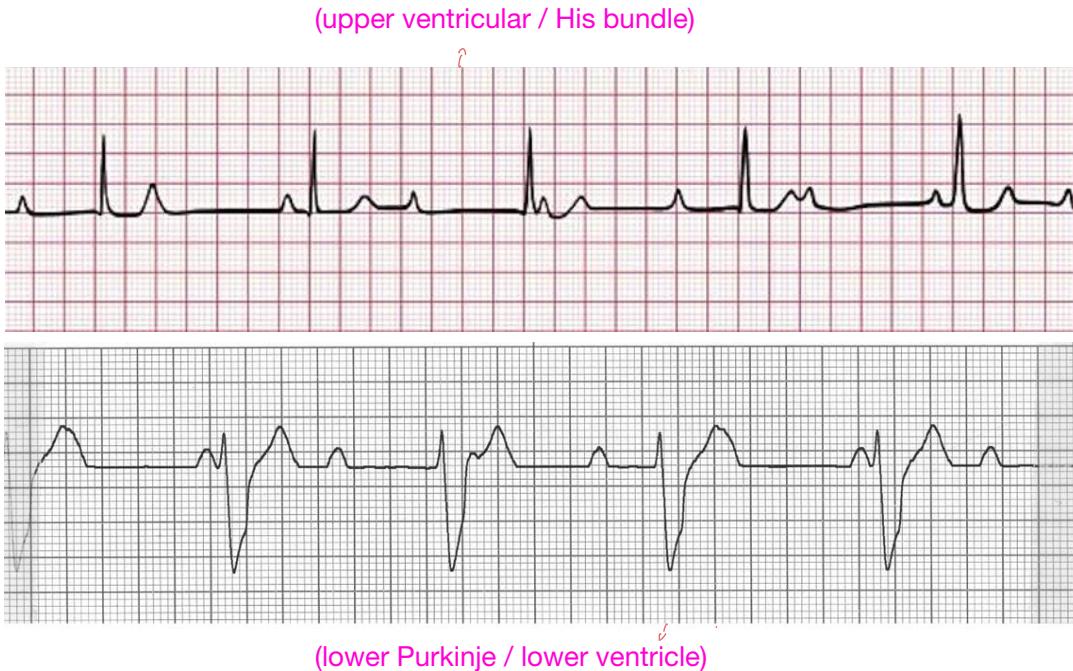
- Unstable Angina: Normal ECG and troponin, but clinical chest pain (at rest, increasing severity, or new-onset).
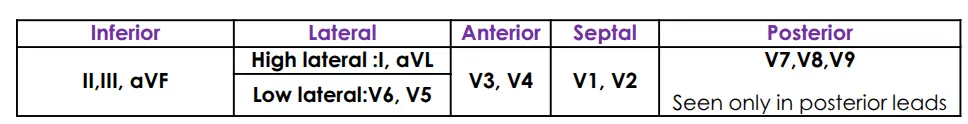
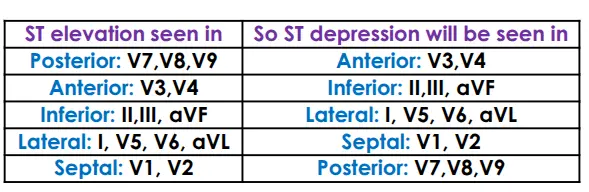
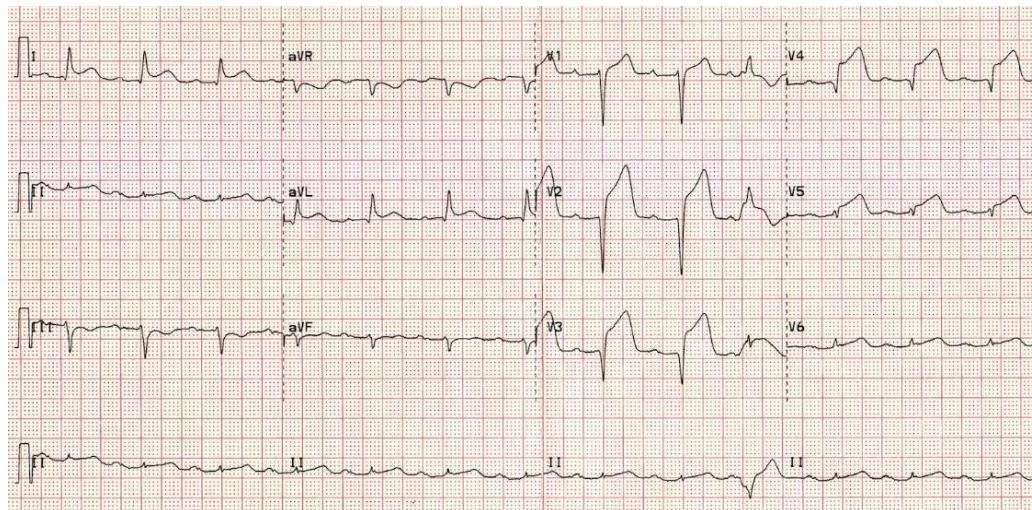
Inferior Myocardial Infarction (MI)
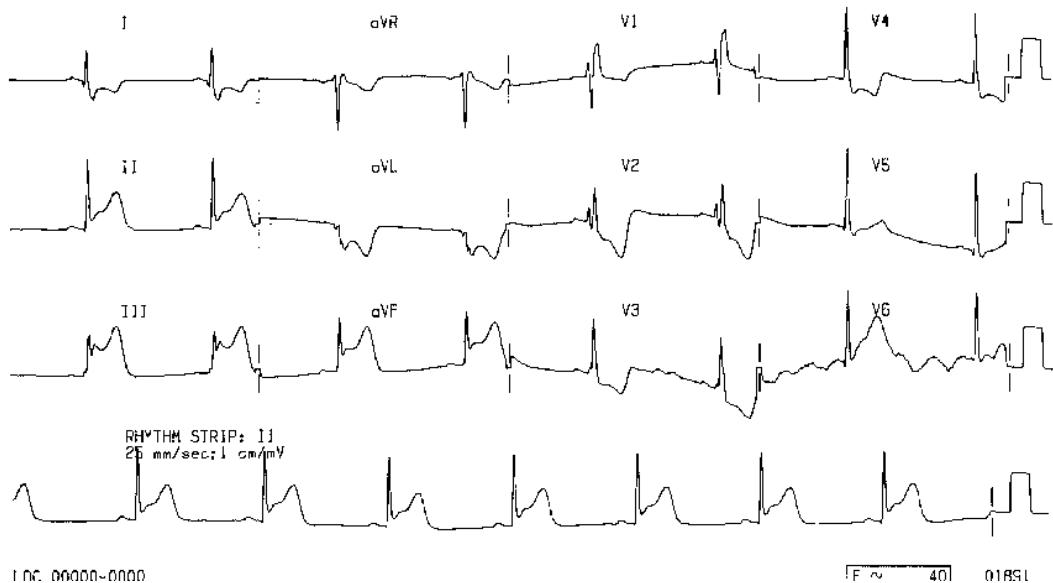
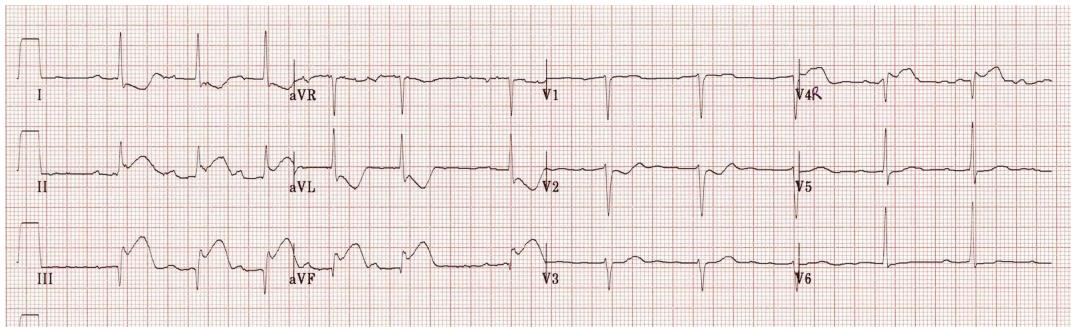
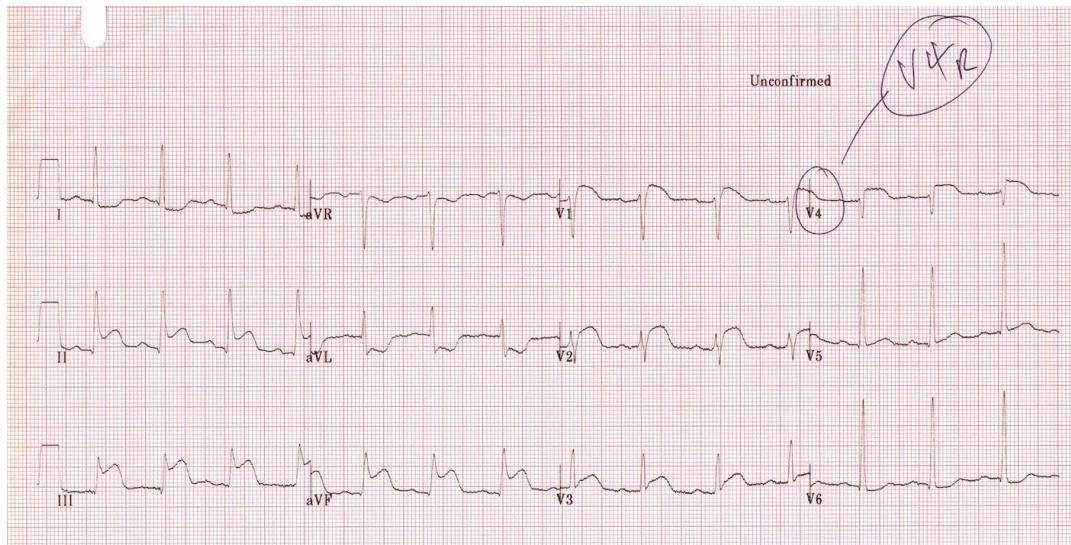
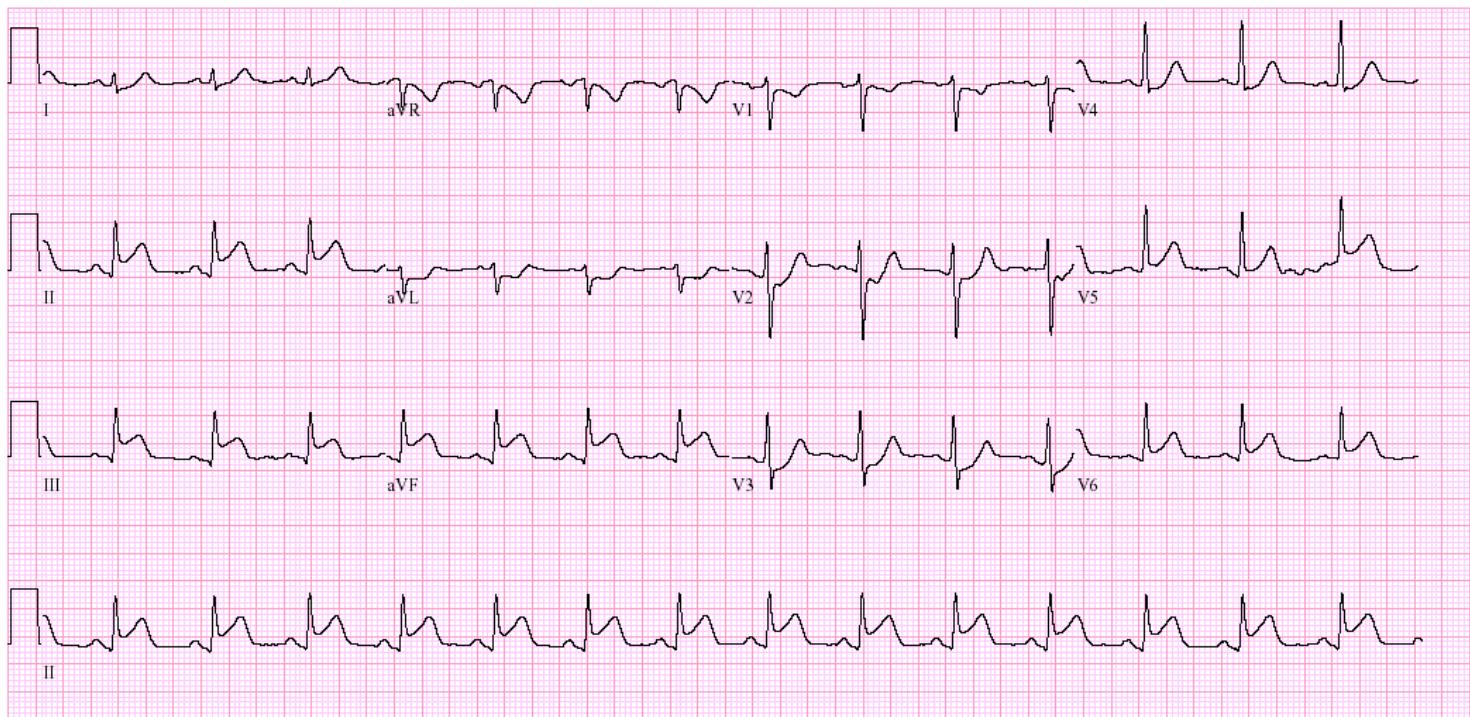
- ECG Findings: ST elevation in leads II, III, and aVF.
- Reciprocal Changes: ST depression in lead aVL. - V1, V2, V3, V4 +R and T wave so maybe ischemia of posterior MI. - ask for right and posterior
- Next Steps:
- Order a Right-Sided ECG (V4R) to exclude Right Ventricular Infarction.
- Order a Posterior ECG (V7-V9) if reciprocal changes are seen in V1-V3.
- Check cardiac enzymes (Troponin).
- Contraindications (in RV Infarction): Avoid Nitroglycerin and Morphine (can lead to severe hypotension).
if you see RT inferior infarction changes don’t give nitroglycerin patient or alveloid V4 elevation + inferior = RT inferior infarction= no morphine no nitroglycerine it will lead to complicate PCI
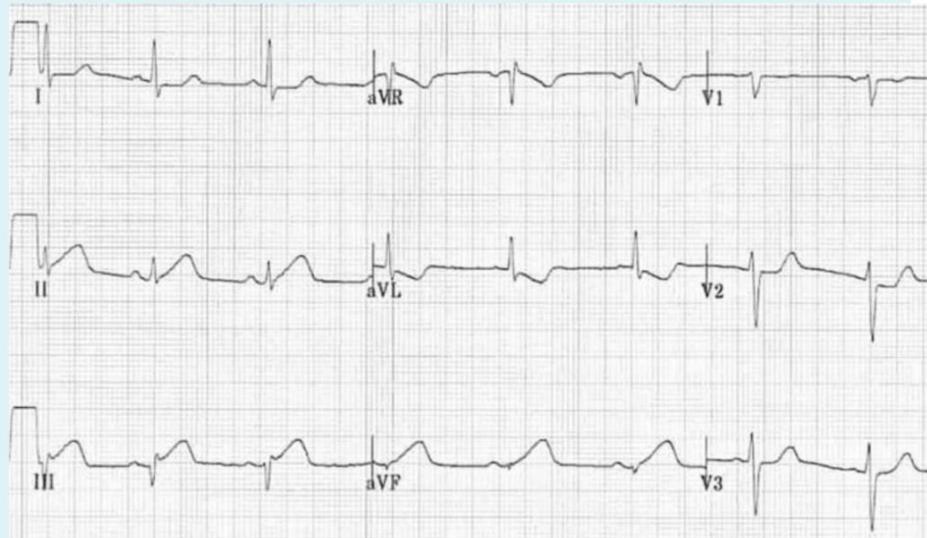
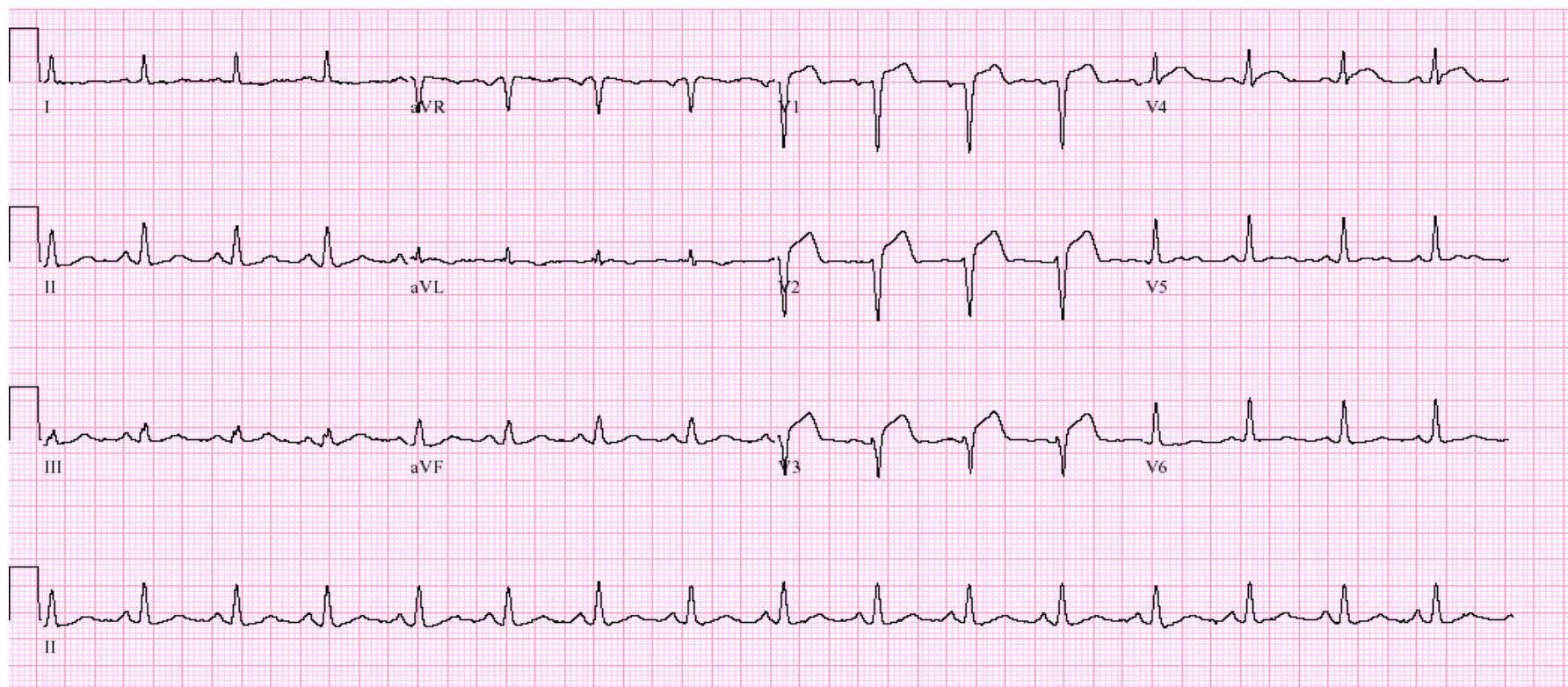
Posterior Myocardial Infarction
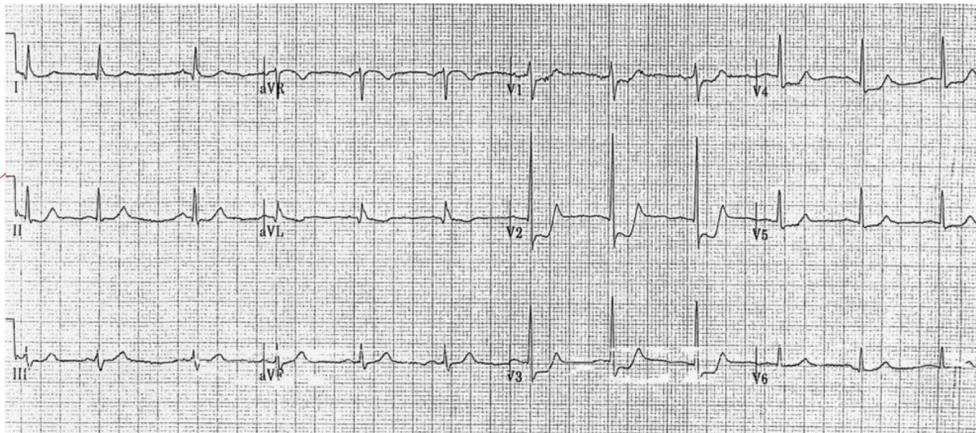
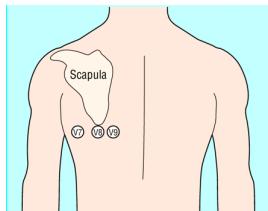
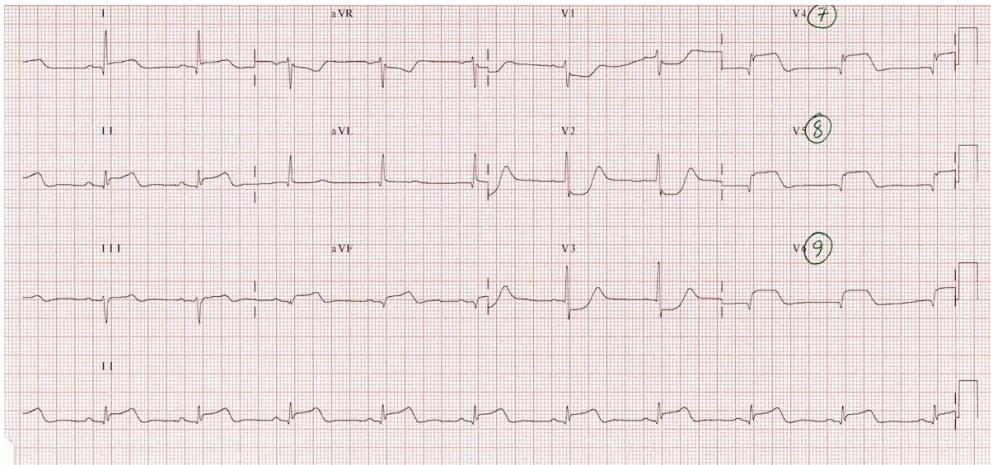
- ECG Findings: ST depression and tall R waves in V1, V2, and V3.
- Confirmation: Perform a 15-lead ECG i.e. + posterior (including V7, V8, V9).
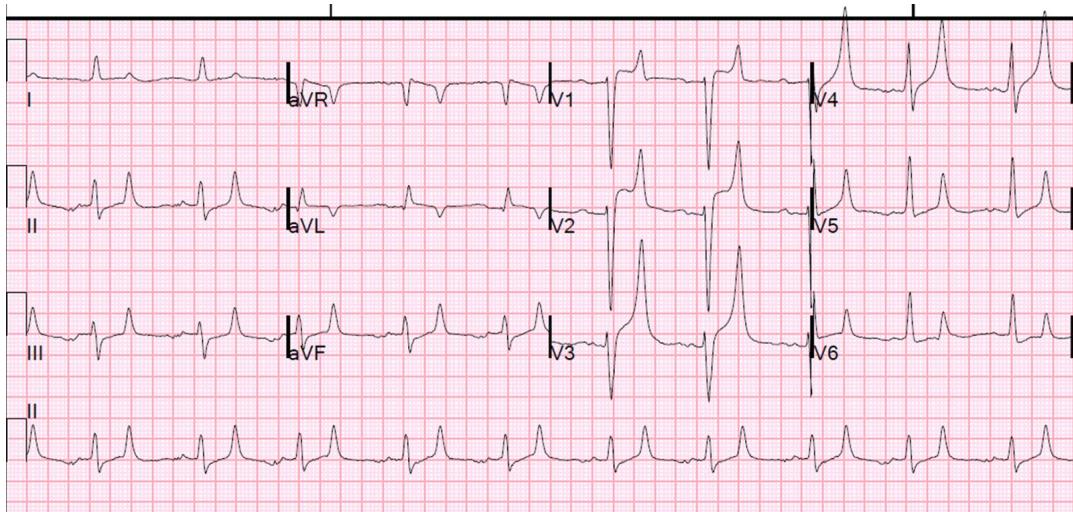
Anterior / Anteroseptal MI

- ECG Findings: ST elevation in leads V1, V2, V3, and V4.
- Management: MONA (Morphine, Oxygen if , Nitroglycerin, Aspirin), immediate Cath Lab/PCI.
Hyperacute T-waves / Hyperkalemia
- ECG Finding: Peaked (Hyperacute) T-waves.
- Differential Diagnosis:
- Hyperkalemia.
- Early STEMI (Hyperacute MI).
- Next Investigations: Cardiac biomarkers (Troponin) and serum Potassium level.
- Hyperkalemia Management:
- Protect Heart: Calcium Gluconate or Calcium Chloride.
- Shift K+: Insulin + Dextrose, Beta-2 agonists.
- Remove K+: Dialysis, Diuretics.
Asystole

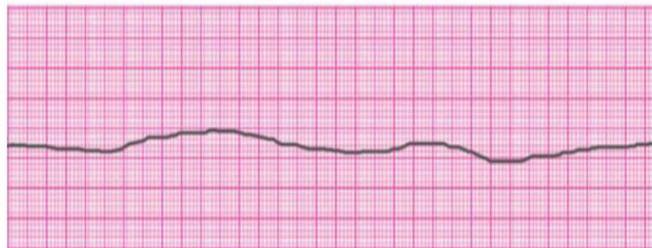
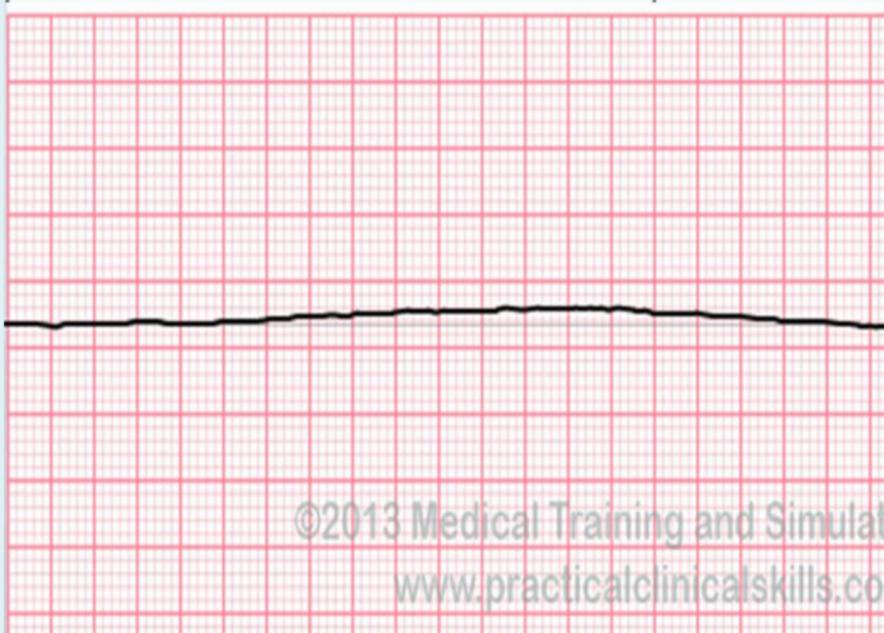
- Diagnosis: Asystole.
- Flat Line Protocol (Confirmation):
- Check the connection between the patient and the machine.
- Verify the rhythm in more than one lead (standard: check at least 2 leads).
- Increase the ECG gain/size on the monitor to exclude fine Ventricular Fibrillation.
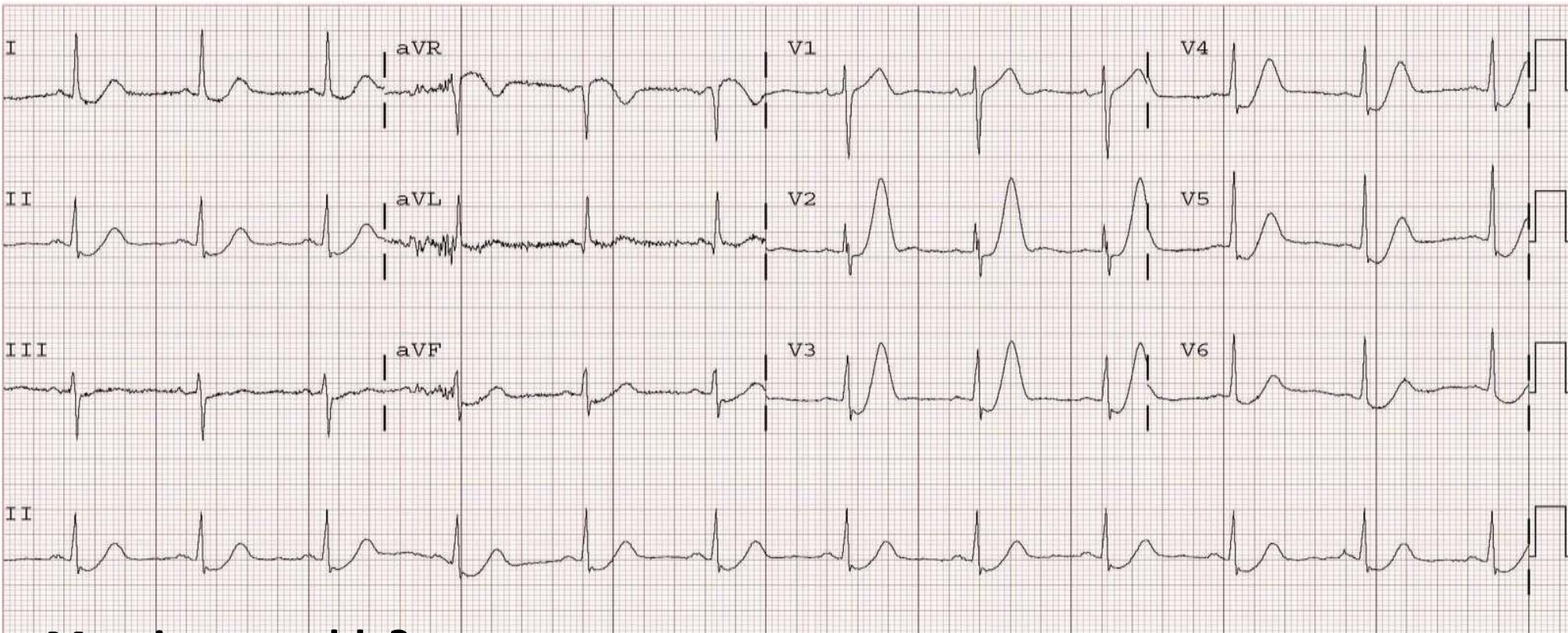
Pericarditis
- Clinical Case: Patient with chest pain and recent URTI.
- ECG Findings: Diffuse ST elevation (concave/upward) and PR segment depression.
- Diagnosis: Pericarditis.
Trauma and Surgical Emergencies
Nasal Septal Hematoma
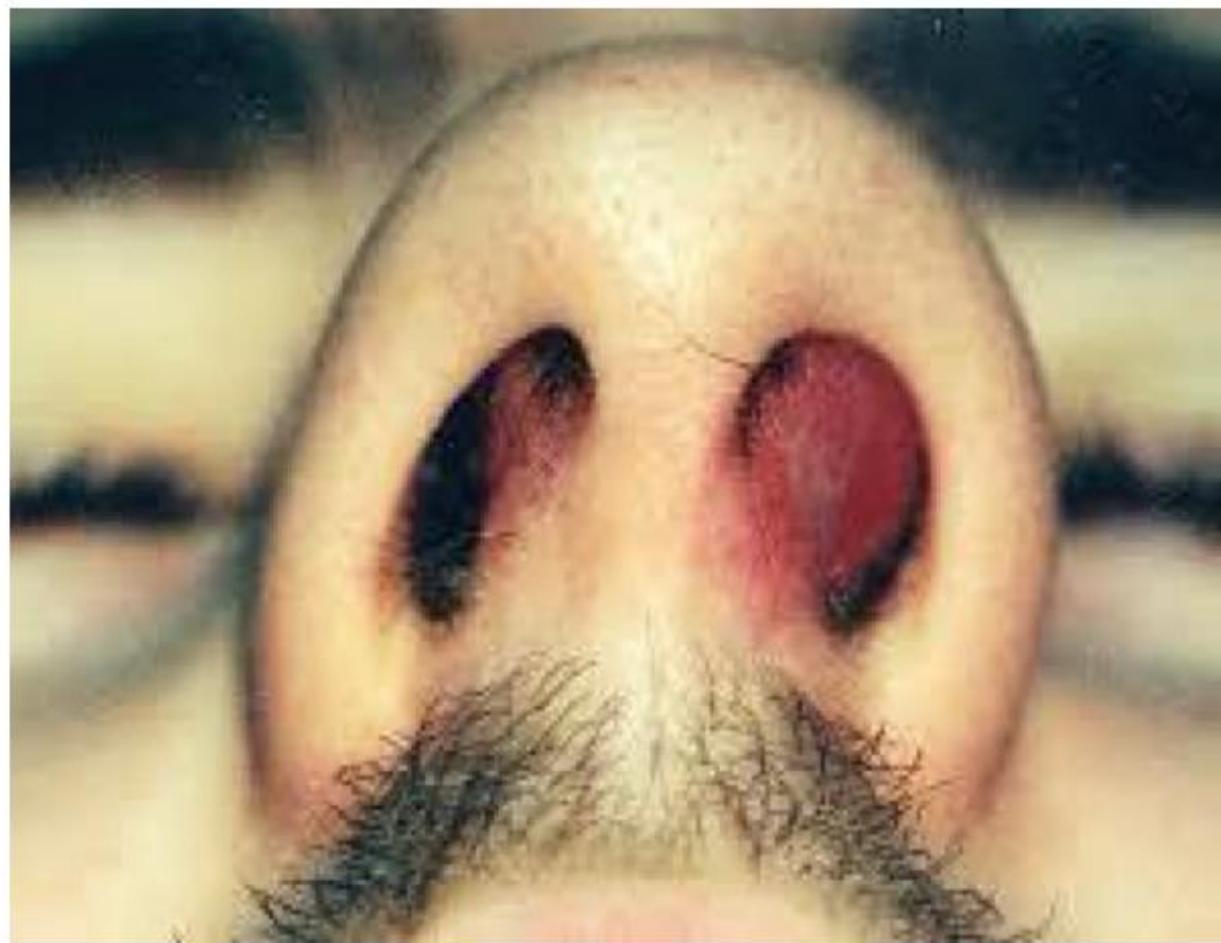
- Diagnosis: Nasal Septal Hematoma.
- Pathology: Usually due to nasal trauma.
- Management:
- Urgent Incision and Drainage (I&D).
- Nasal packing to prevent re-accumulation.
- Antibiotics.
- ENT consultation.
- Complications: If left untreated, can lead to saddle nose deformity or septal necrosis/perforation.
Auricular Hematoma
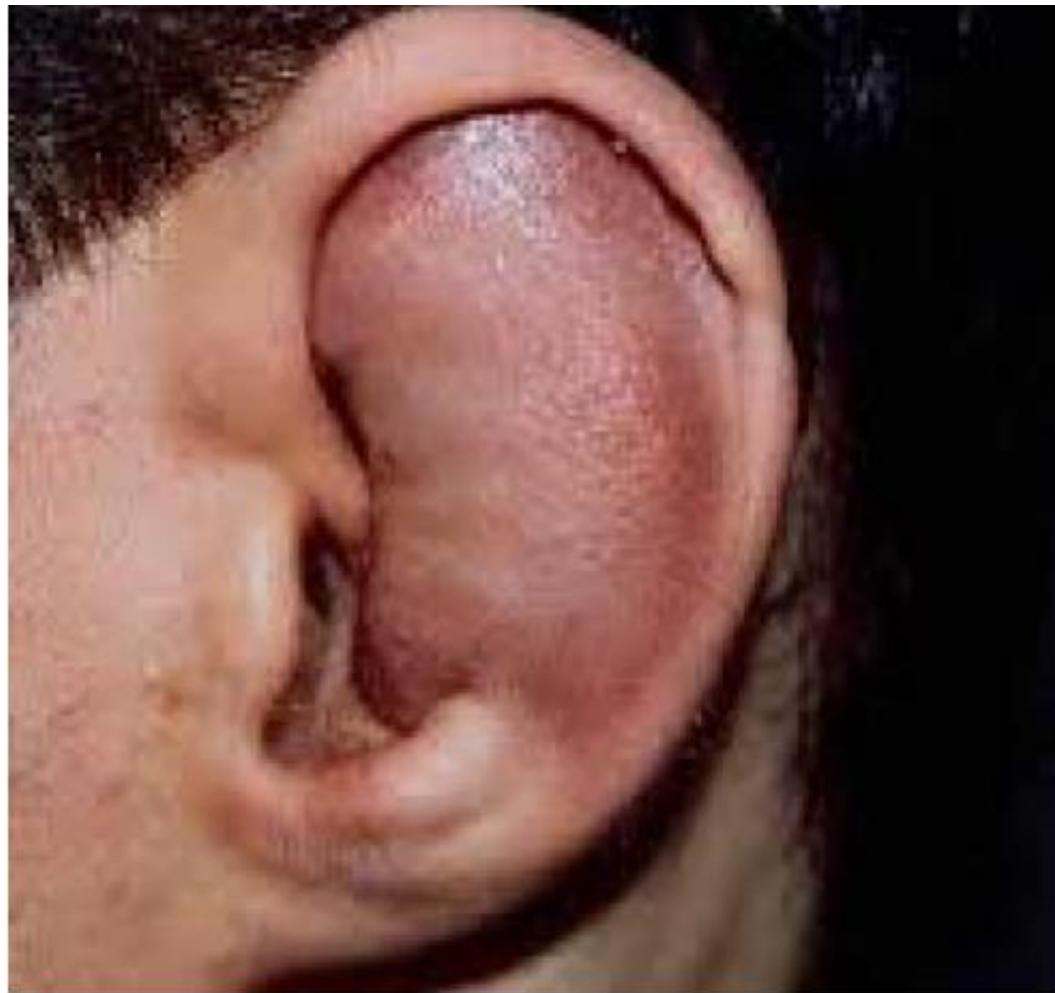
- Diagnosis: Auricular Hematoma.
- Management:
- Evacuation of the hematoma.
- Compression dressing and Cold/Ice packs.
- Complications: Can lead to cauliflower ear due to cartilage necrosis if not treated promptly.
Cauliflower Ear

- Description: Chronic deformity of the ear due to untreated auricular hematoma.
- Pathology: Necrosis of the ear cartilage.
Peritonsillar Abscess (Quinsy)
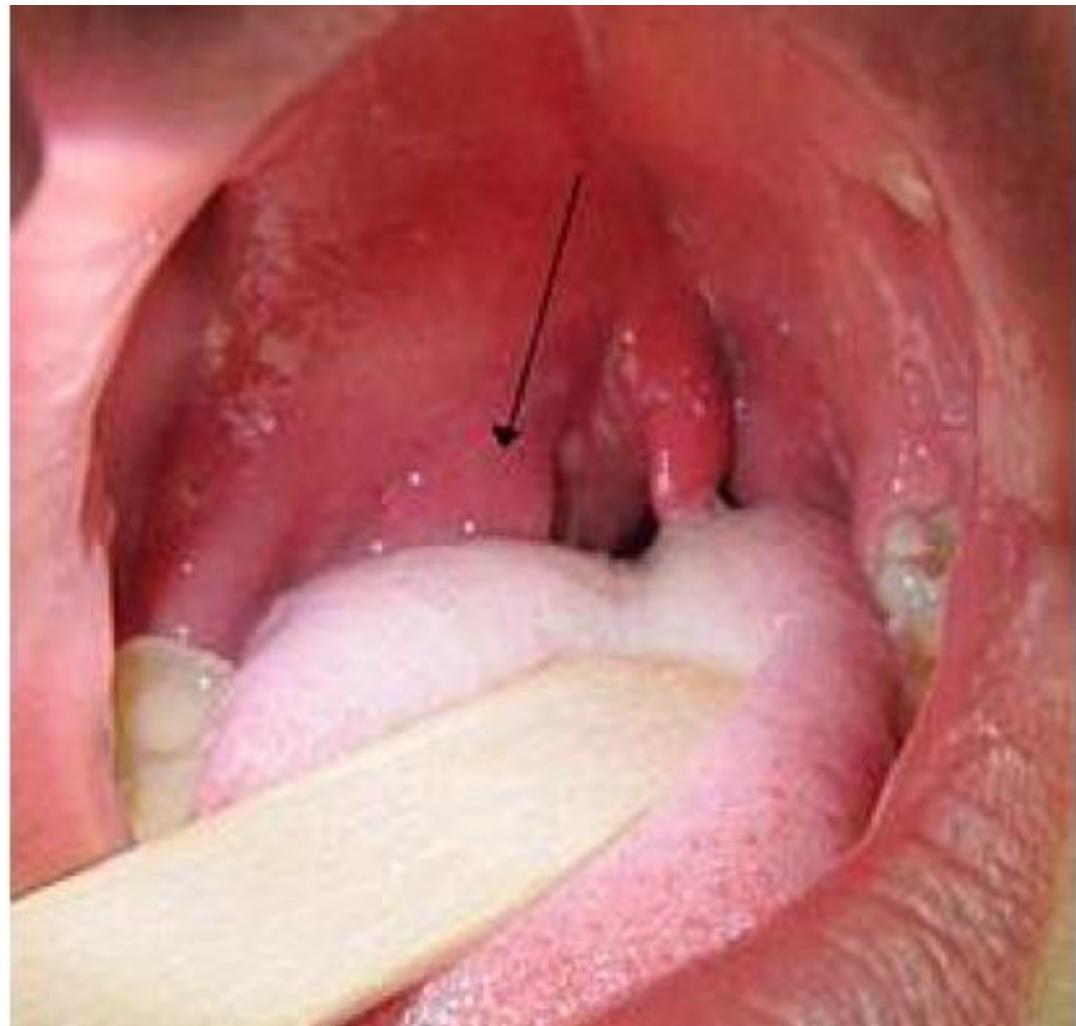
- Diagnosis: Peritonsillar Abscess.
- Clinical Presentation: History of tonsillitis not improving with antibiotics; “hot potato” voice, uvular deviation.
- Management: Incision and Drainage (I&D).
Hyphema

- Diagnosis: Hyphema (Blood in the anterior chamber of the eye).
- Causes:
- Trauma (most common).
- Sickle cell anemia.
- Bleeding disorders.
- Management: Ophthalmologist consultation; usually resolves spontaneously but may require bed rest and eye protection.
Orbital Blowout Fracture

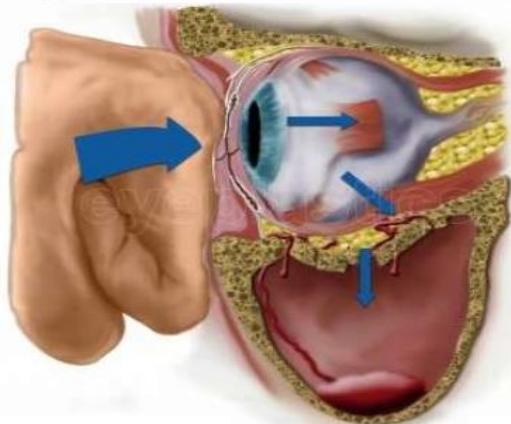
- Diagnosis: Orbital Blowout Fracture (Fracture of the orbital floor).
- Clinical Signs:
- Periocular redness/bruising.
- Inability to move the eye upwards (diplopia on upward gaze).
- Pathology: Entrapment of the inferior rectus muscle.
- Mechanism: Blunt force to the eyeball increases intraorbital pressure, causing a fracture at the weakest point (orbital floor).
Facial Nerve Palsy (7th Nerve)
- Diagnosis: Facial Nerve Palsy (Bell’s Palsy if idiopathic).
- Classification:
- Lower Motor Neuron (LMN): Affects the entire half of the face (including the forehead).
- Upper Motor Neuron (UMN): Affects only the lower quadrant of the face (spares the forehead/upper 1/4); may indicate a tumor or stroke.
- Assessment of Severity: Ask the patient to raise their eyebrows.
- LMN: No wrinkles on the affected side.
- UMN: Wrinkles are present (forehead muscles are spared).
- Other tests: Blow cheeks, smile.
Fournier Gangrene

- Diagnosis: Fournier Gangrene.
- Risk Factors: Immunocompromised states (Diabetes Mellitus, HIV, Cancer, immunosuppressive therapy).
- Treatment:
- Urgent surgical debridement (excision of gangrenous tissue).
- IV Broad-spectrum antibiotics.
Venomous Snake Bite


- Diagnosis: Snake Bite.
- Treatment: Antivenom.
- Management:
- Immobilize the extremity below the level of the heart.
- Draw a circle around the bite site to monitor for spreading.
- Contraindications: Do NOT use a tourniquet, and do NOT perform incision and suction.
Pneumoperitoneum (Air Under Diaphragm)
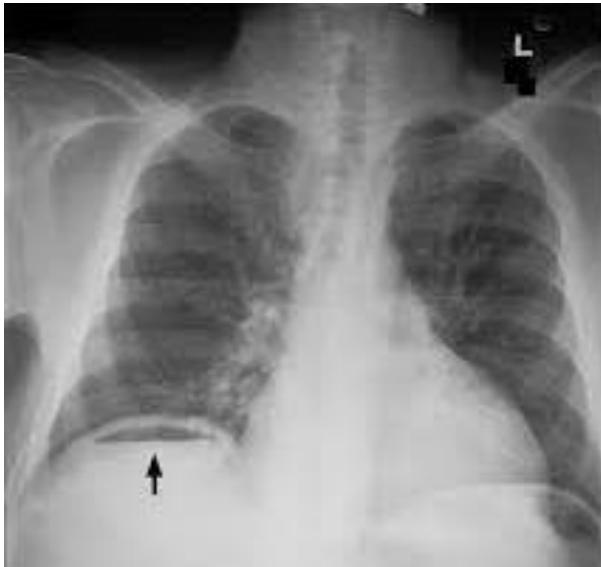

- Sign: Air under the diaphragm (Pneumoperitoneum).
- Diagnosis: Perforated viscus (e.g., perforated peptic ulcer).
- Clinical Presentation: Sudden abdominal pain, board-like rigidity.
- Management: Surgical emergency; requires immediate OR.
Small Intestinal Obstruction

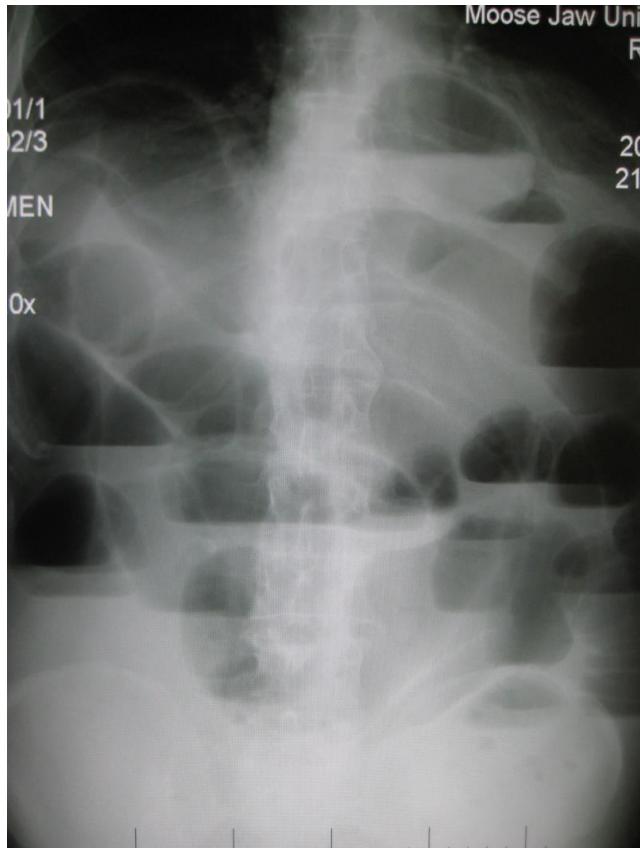
- Diagnosis: Small Intestinal Obstruction.
- X-ray Findings: Multiple air-fluid levels on erect abdominal X-ray; distended bowel loops.
- Clinical Presentation:
- Abdominal distention.
- Constipation and vomiting.
- Decreased/hypoactive bowel sounds.
Volvulus

- Diagnosis: Volvulus (Sigmoid or Cecal).
- Cause: Malrotation or twisting of the bowel.
- Risk Factors:
- Chronic constipation.
- Abdominal adhesions.
- Hirschsprung’s disease.
- Common in elderly or bedridden patients.
- Management: Surgical emergency.
Acute Mastoiditis

- Diagnosis: Acute Mastoiditis.
- Presentation: Often follows Otitis Media; post-auricular tenderness and redness.
Mediastinal Calcification

- Diagnosis: Mediastinal calcification with obstruction.
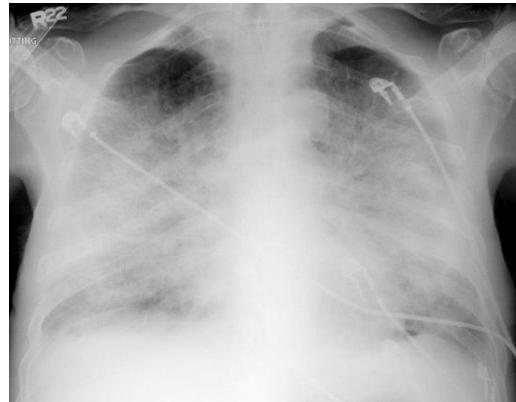
Pneumothorax

- Diagnosis: Right-sided Pneumothorax.
- Tension Pneumothorax (Clinical Diagnosis):
- Tracheal deviation to the opposite side.
- Hyperresonance on percussion.
- Congested neck veins, hemodynamic instability.
- Treatment of Tension Pneumothorax: Urgent needle decompression followed by chest tube insertion.
Pulmonary Edema

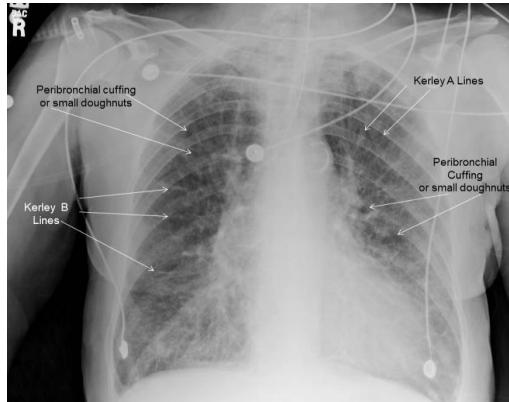
- Diagnosis: Pulmonary Edema.
- Radiological Signs:
- Cephalization (early).
- Kerley B lines, peribronchial cuffing.
- Bat wing or butterfly appearance (late/severe).
- Cardiomegaly.
- Differential Diagnosis: Pneumonia, ARDS.
- Management:
- Position: Sitting up.
- Respiratory support (CPAP or BiPAP).
- Diuretics (Furosemide), Vasodilators (Nitroglycerin).
Lung Abscess

- Diagnosis: Lung Abscess.
- Findings:
- Cavitation with an air-fluid level and surrounding consolidation.
- May show a curvy line (associated with unresolved Pneumonia, e.g., Klebsiella).
- Management: IV Antibiotics, potentially drainage (I&D).
Gallstones (Cholelithiasis)

- Diagnosis: Gallstones.
- Modality: Ultrasound showing echogenic focus in the gallbladder.
Sutures and Skin Closure
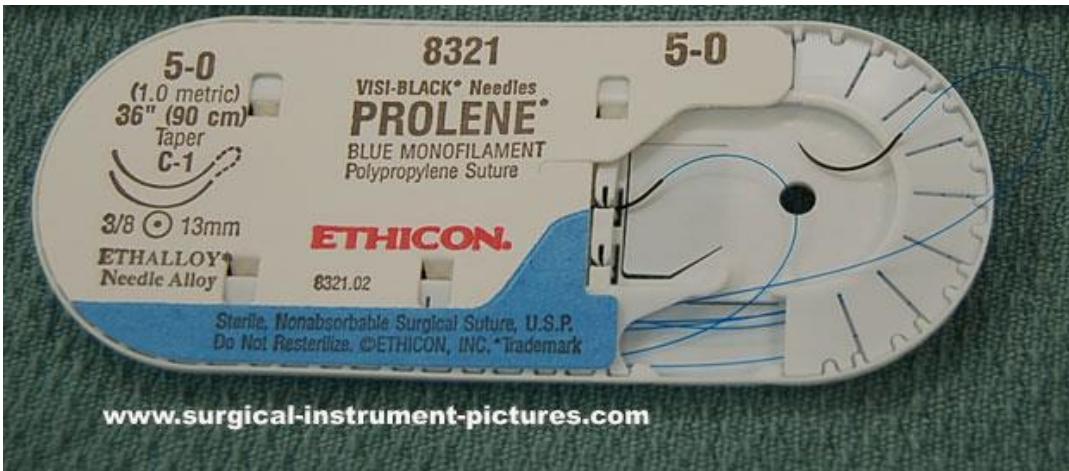

- Prolene monofilament Suture: (First image)
- Non-absorbable monofilament; used for skin closure (e.g., jaw lacerations).
- Sizing: Higher gauge number = smaller suture (e.g., 5.0-6.0 is smaller than 2.0-3.0). Use smaller sizes (5.0-6.0) for face/cosmetic areas, larger (2.0-3.0) for areas needing strong support.
- Absorbable Sutures: Used for mucous membranes (e.g., inside the mouth), internal structures, and pediatrics.
- Skin Adhesive (Dermabond): Sterile liquid glue for wound closure; no removal needed. (second image)
Lumbar Puncture
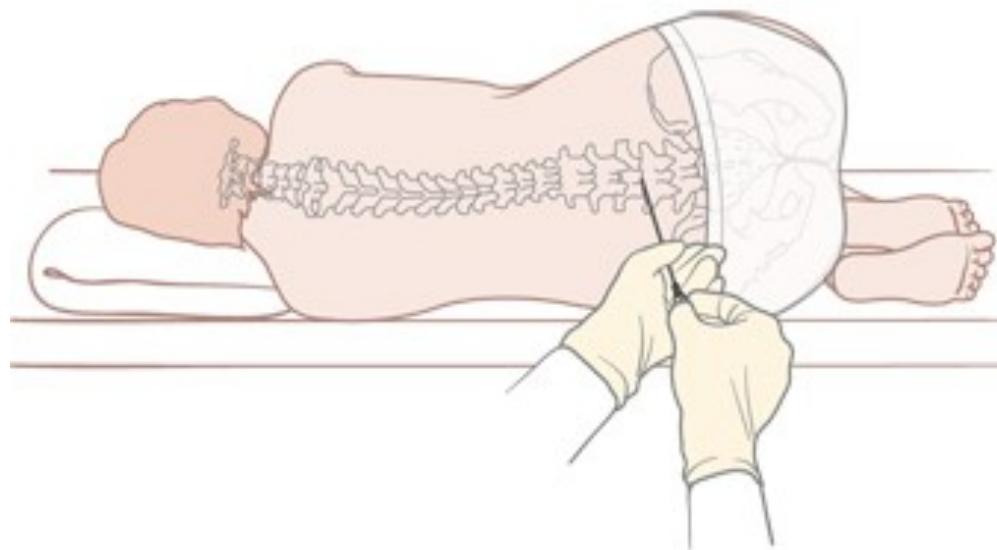
- Indications:
- Confirm meningitis.
- Evaluate for intracranial hemorrhage.
- Investigate CNS disorders or malignancies.
Radiology
Scaphoid Fracture






- Diagnosis: Scaphoid Fracture.
- Clinical Sign: Tenderness in the anatomical snuffbox.
- Management: Thumb spica splint/cast. If X-ray is normal but tenderness is present, treat as a fracture and repeat X-ray in 10-14 days or order a CT/MRI.
Monteggia Fracture


- Diagnosis: Monteggia Fracture.
- Pathology: Fracture of the proximal third of the ulna with dislocation of the radial head.
- Management: Analgesia, neurovascular assessment, and orthopedic referral (usually requires ORIF).
Posterior Hip Dislocation



- Diagnosis: Posterior Hip Dislocation.
- Limb Position: The affected limb is shortened, adducted, and internally rotated.
- Radiological Sign: The femoral head is seen above the acetabulum.
- Management: Emergency reduction under sedation/anesthesia by orthopedics.
Occult Elbow Fracture (Fat Pad Sign)


- Sign: Positive posterior fat pad sign (always abnormal) or an enlarged anterior fat pad (sail sign).
- Diagnosis: Occult fracture of the elbow (e.g., supracondylar fracture in children or radial head fracture in adults).
- Management: Splinting and orthopedic follow-up; CT may be needed for confirmation.
Elbow/Shoulder Dislocation

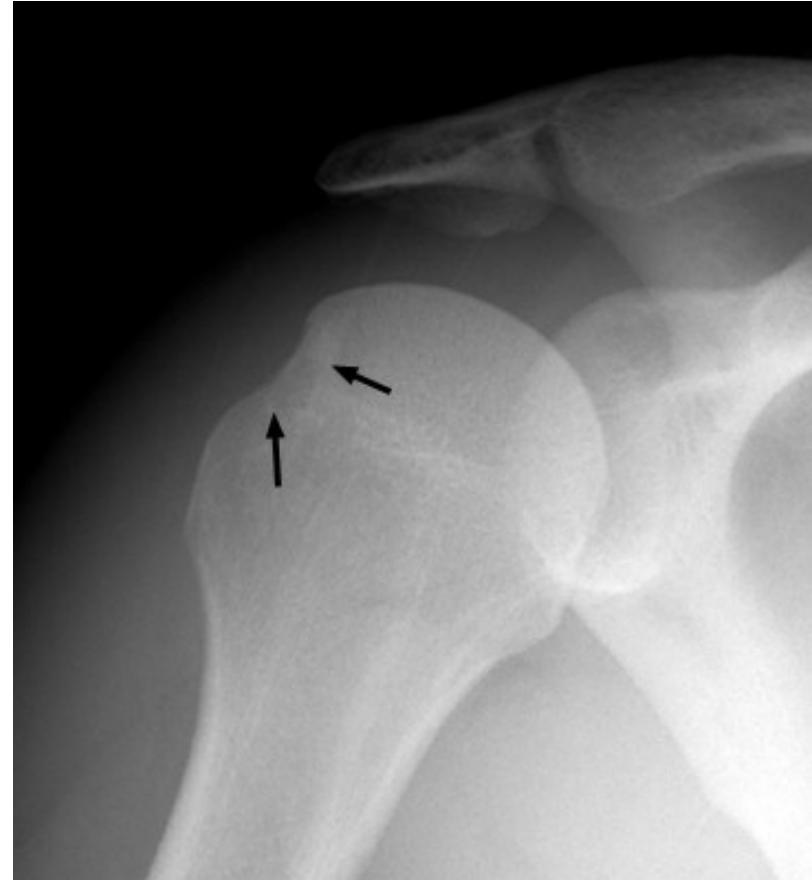

- Elbow Dislocation: Check for median/ulnar nerve or brachial artery injury. (1st image)
- Shoulder Dislocation Signs:
- Hill-Sachs Deformity: Compression fracture of the posterior humeral head. - recurrent anterior shoulder dislocation. (2nd image)
- Bankart Lesion: an anterior dislocation of shoulder - Injury to the anterior glenoid labrum. (3rd)
Finger Splint
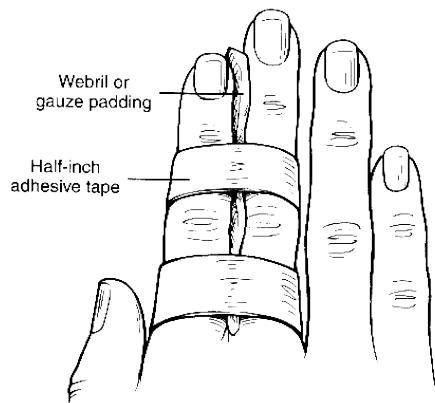
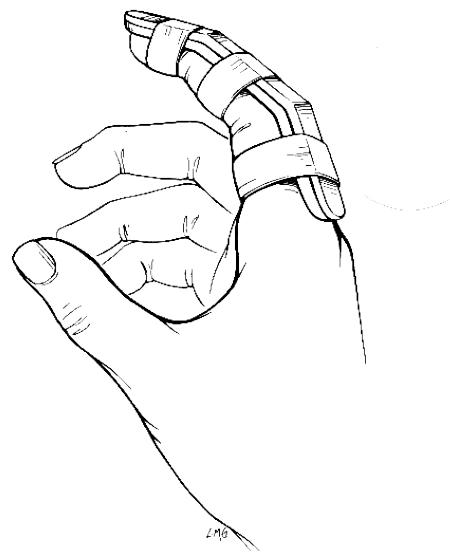
- Use: Immobilization for phalangeal fractures or dislocations.
Pediatrics and Social
Child Abuse



- Suspicion Factors:
- Multiple bruises in different stages of healing (different colors).
- Injuries in soft tissues or unusual areas (not over bony prominences).
- Specific patterns: loop marks (belt/cord), fist or pinch marks, cigarette burns.
- Spiral fractures in non-walking children.
- History inconsistent with the injury.
- Management:
- Manage as a trauma patient.
- MANDATORY reporting to social workers and child protection teams.
- Admission for safety if necessary.
Measles

- Diagnosis: Measles (Rubeola).
- Complications: Otitis Media (most common), Pneumonia (most common cause of death), Encephalitis, SSPE (Subacute Sclerosing Panencephalitis - late).
Burns

- Diagnosis: Superficial Partial Thickness Burn (Second Degree).
- Features: Erythema, blistering, pain, shedding of skin.
Obstetrics and Gynecology
Molar Pregnancy (Complete Mole)
- Diagnosis: Complete Molar Pregnancy.
- Ultrasound Finding: Snowstorm appearance.
- Clinical Presentation:
- Vaginal bleeding in early pregnancy.
- Excessive vomiting (Hyperemesis Gravidarum).
- Hypertension/Preeclampsia before 20 weeks.
- Fundal height greater than gestational age.
- Differential Diagnosis for Early Bleeding: Molar pregnancy, Ectopic pregnancy, Abortion.
Radiology and Imaging
C-Spine X-ray
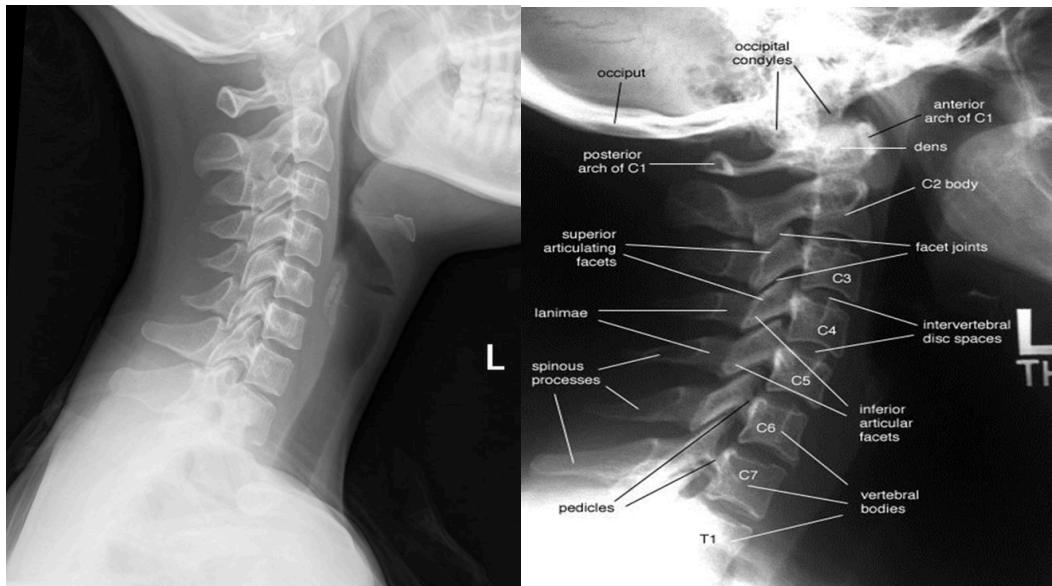
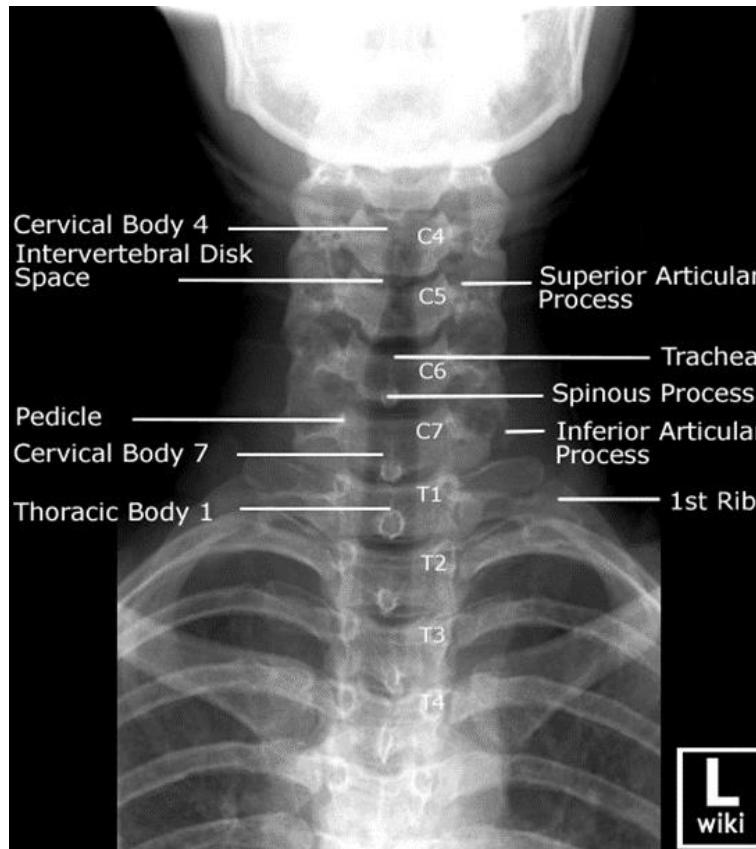
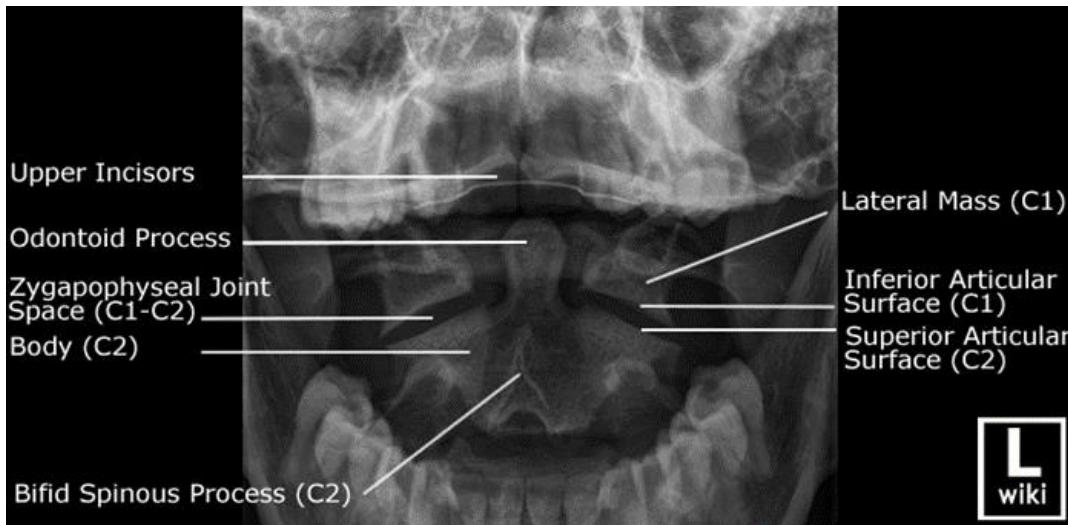

- Views:
- Lateral View: Must show C1 down to the C7-T1 junction.
- AP View.
- Odontoid (Open Mouth) View: Used to visualize C1 and C2 (especially the dens).
- Pathology:
- Odontoid Fracture (C2): Seen on the open mouth view.
- C2 Fracture (Hangman’s fracture) can be seen on the lateral view.
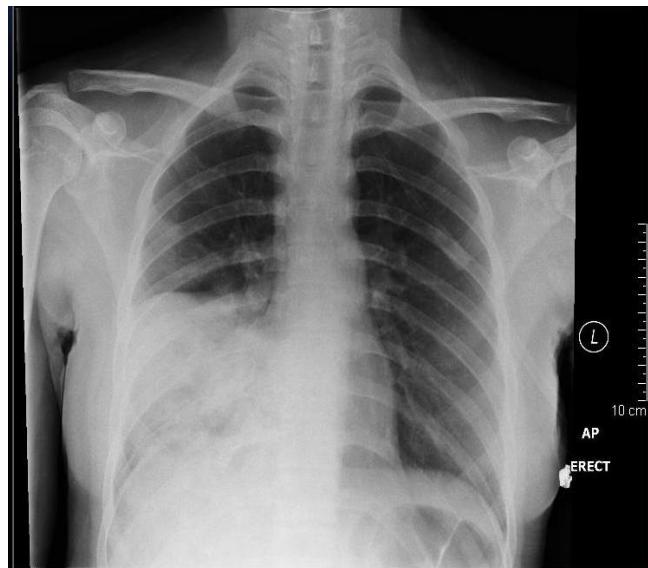
Chest X-ray: Pneumonia


- Finding: Right lower lobe consolidation.
- Diagnosis: Pneumonia.
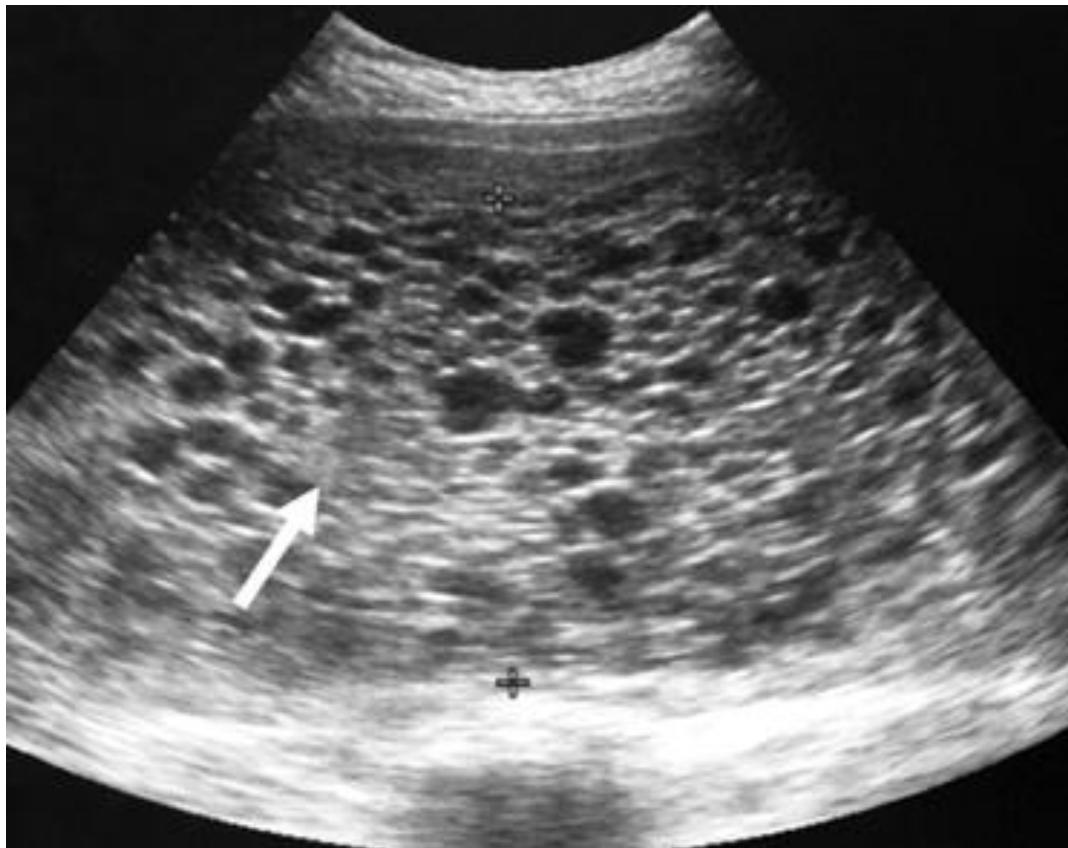
FAST / eFAST Ultrasound
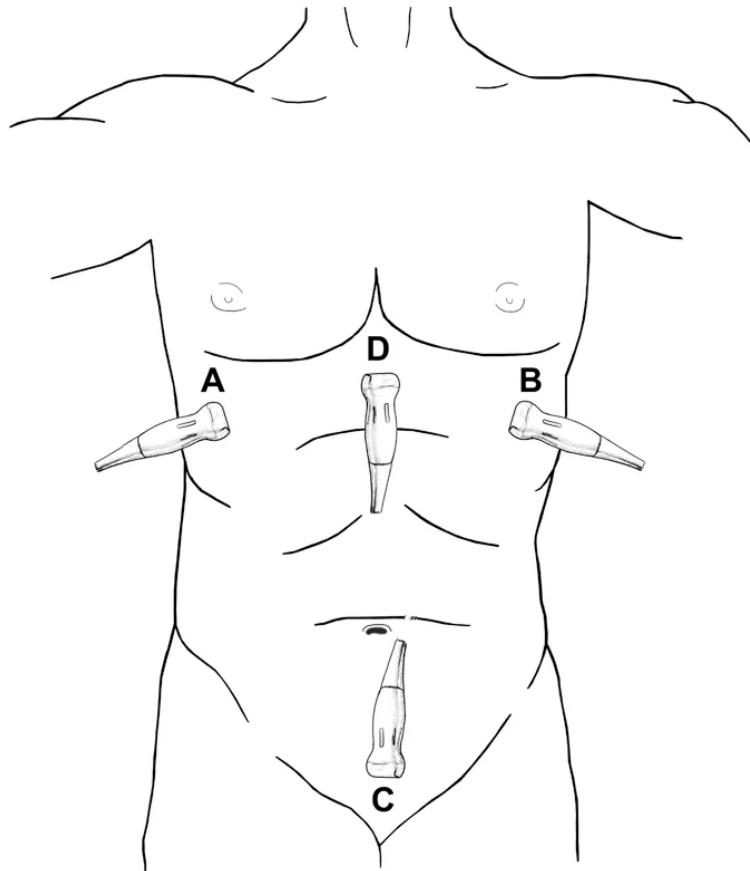
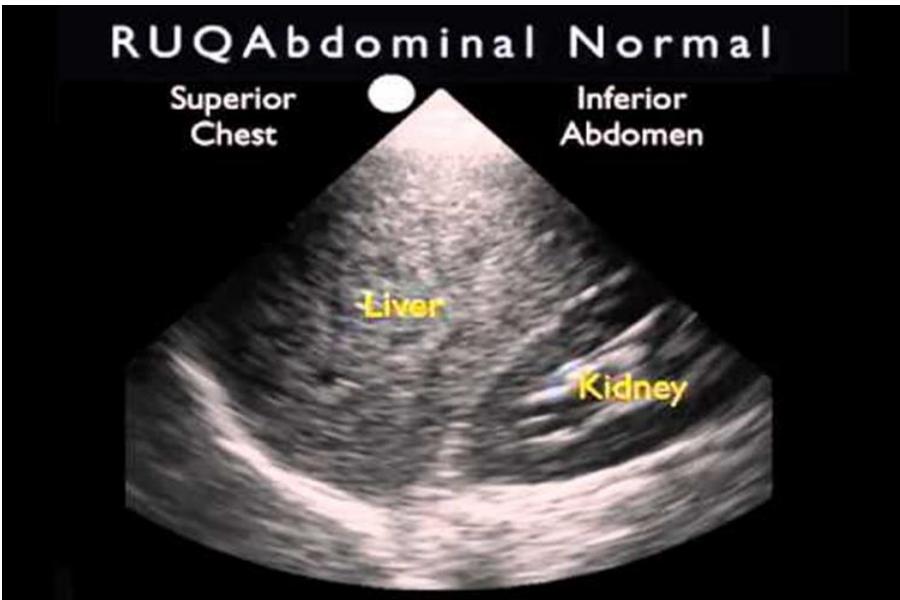
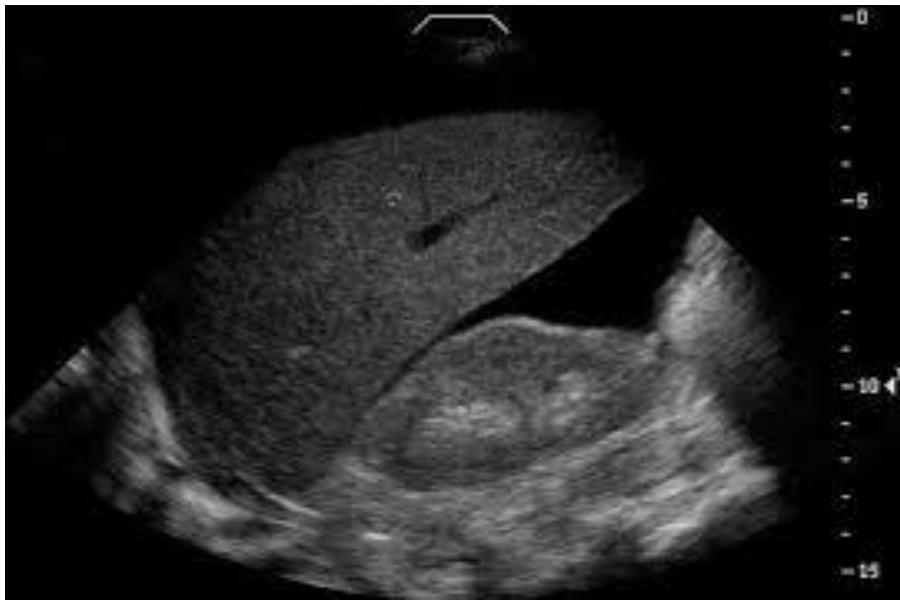

- Modality: Focused Assessment with Sonography in Trauma (FAST).
- Standard 4 Views:
- RUQ (Morison’s Pouch): Hepatorenal recess.
- LUQ: Splenorenal recess.
- Pelvic (Pouch of Douglas): Suprapubic window.
- Pericardial: Subxiphoid window.
- eFAST: Includes the pleura to check for pneumothorax/hemothorax.
- Positive Finding: Anechoic (black) fluid collection indicating blood in a trauma patient.
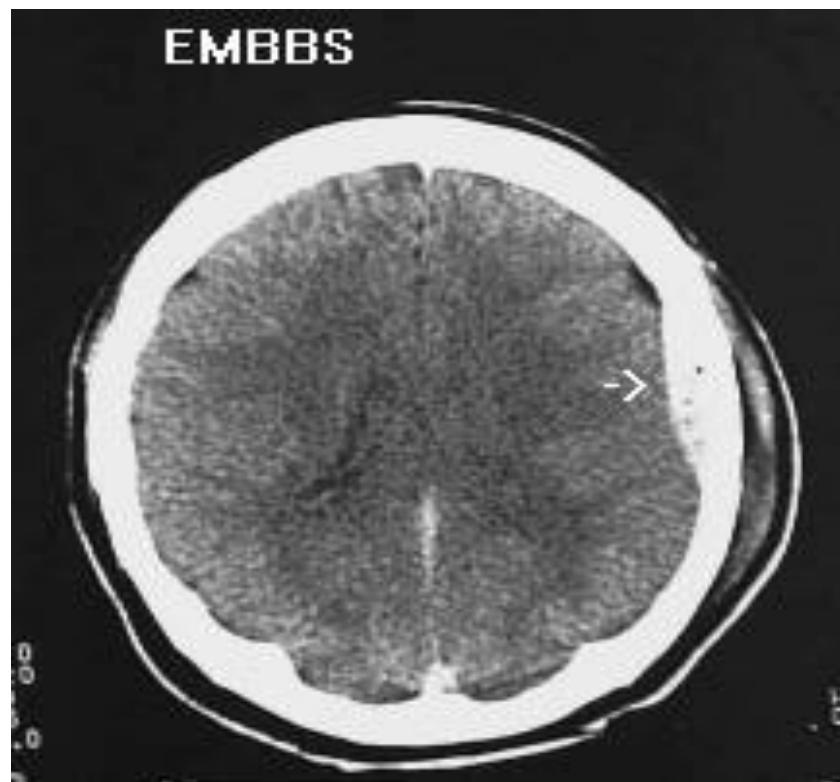
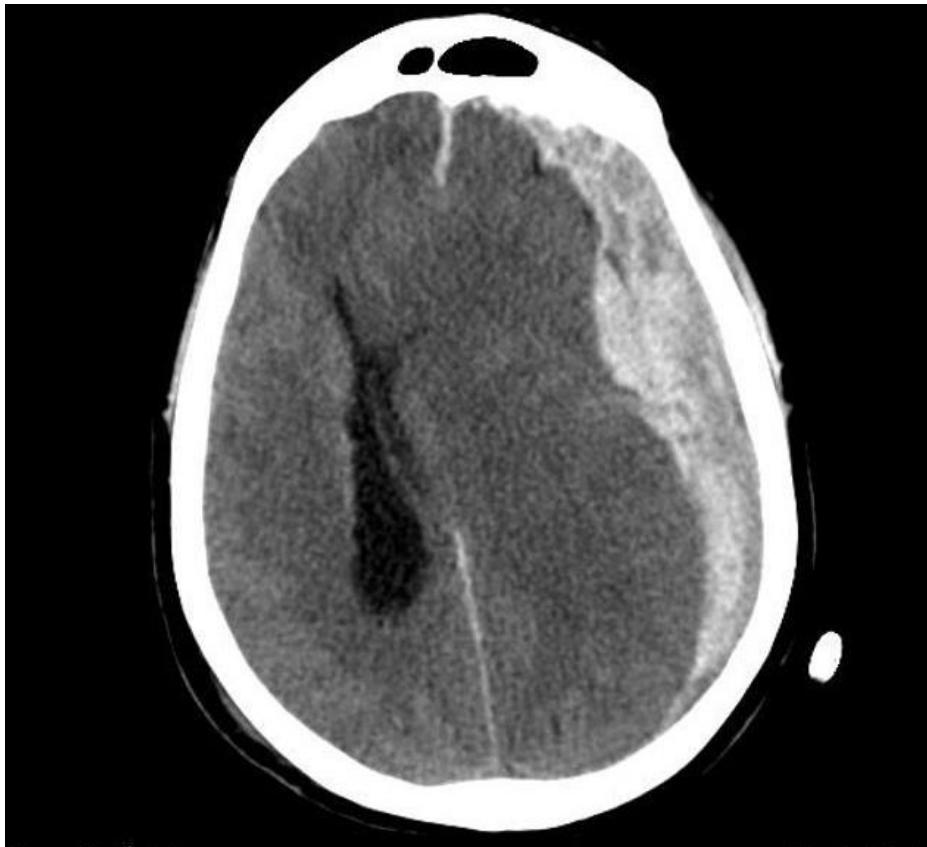
Brain CT Scan
Epidural Hematoma

- Diagnosis: Epidural Hematoma.
- CT Finding: Biconvex (Lens-shaped) hyperdensity; does not cross suture lines.
- Pathology: Usually arterial bleed (Middle Meningeal Artery).
- Note: May show midline shift.
Subdural Hematoma

- Diagnosis: Subdural Hematoma.
- CT Finding: Crescent (Sickle-shaped) hyperdensity; can cross suture lines.
- Pathology: Bleeding from bridging veins.
- Note: Higher density indicates acute bleeding.
Intracerebral Hemorrhage


- Diagnosis: Intracerebral Hemorrhage.
- CT Finding: Hyperdensity within the brain parenchyma.
Ischemic Stroke

- Clinical Case: Face drop, weakness.
- Management: Perform CT to rule out hemorrhage before giving thrombolytics. - if hemorrhagic to OR STAT