Mini ACLS
DR SATTAM ALENEZI
Today your first day in clinical session at emergency department , the nurse in observation unit calling you to come to assess 55 years old lady who is looks critical .
The patient is unconscious , not breathing .
Introduction to Cardiac Arrest
Adult Cardiac Arrest Statistics
- Despite important advances in prevention, cardiac arrest remains a substantial public health problem and a leading cause of death in many parts of the world.
- Cardiac arrest occurs both in and out of the hospital.
- In the US and Canada, approximately 350,000 people/year (approximately half of them in-hospital) suffer a cardiac arrest and receive attempted resuscitation.
Cardiopulmonary Resuscitation (CPR) Fundamentals
- Definition: Emergency lifesaving procedure performed when the heart stops beating.
- Importance: Immediate CPR can double or triple the chances of survival after cardiac arrest.
- Function: Keeping blood flow active – even partially – extends the opportunity for a successful resuscitation once trained medical staff arrive on site.
- Chain of Survival: CPR is a critical step in the AHA’s Chain of Survival.
Despite recent gains, less than 40% of adults receive layperson-initiated CPR, and fewer than 12% have an AED applied before EMS arrival.
Case Presentation
Today your first day in clinical session at emergency department, the nurse in observation unit calling you to come to assess 55 years old lady who is looks critical.
- The patient is unconscious, not breathing.
What should I do?

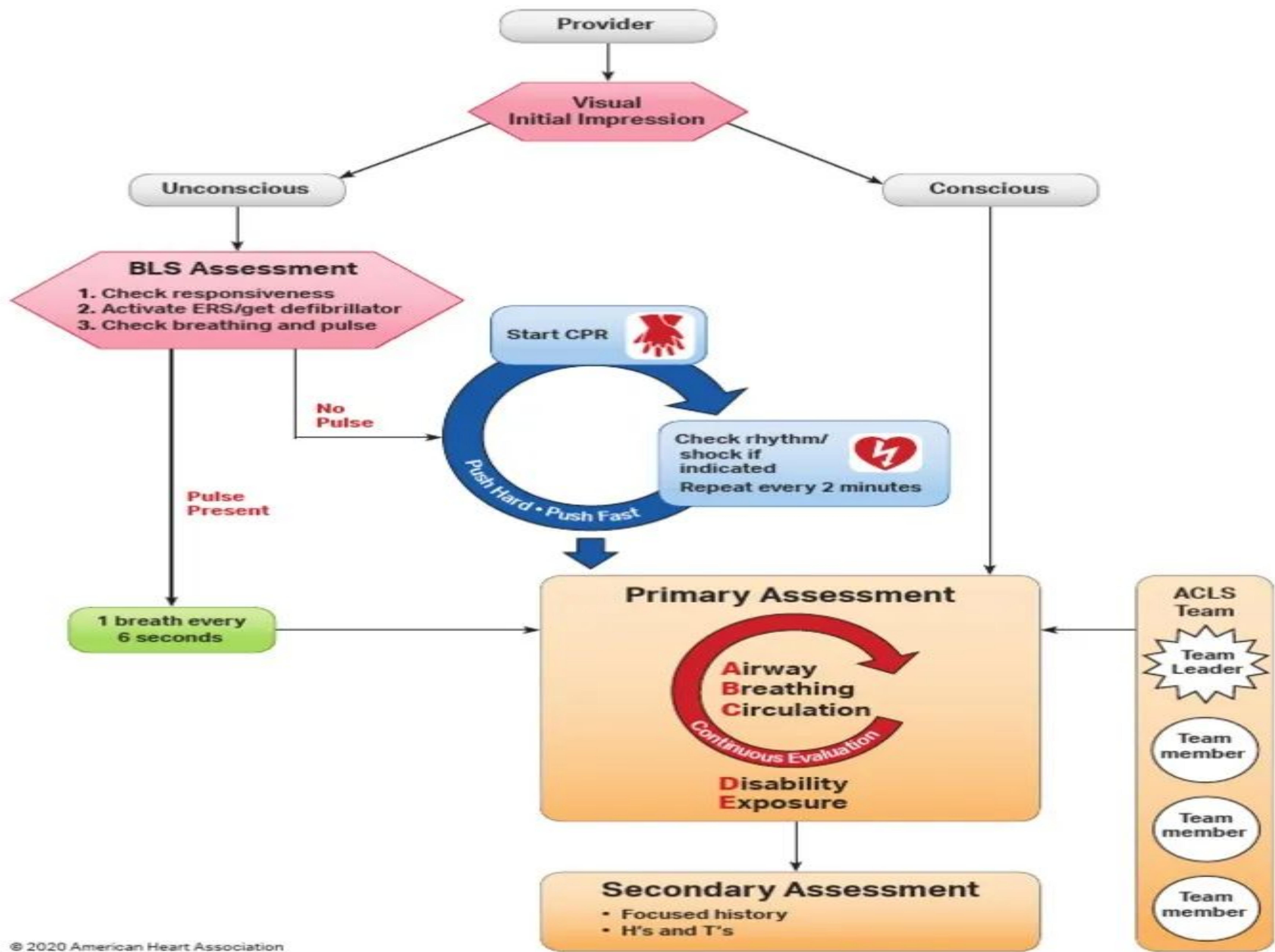
Systematic Approach to Cardiac Arrest
Initial Impression
- (Provider visually checks while approaching patient)
Patient Assessment Pathways
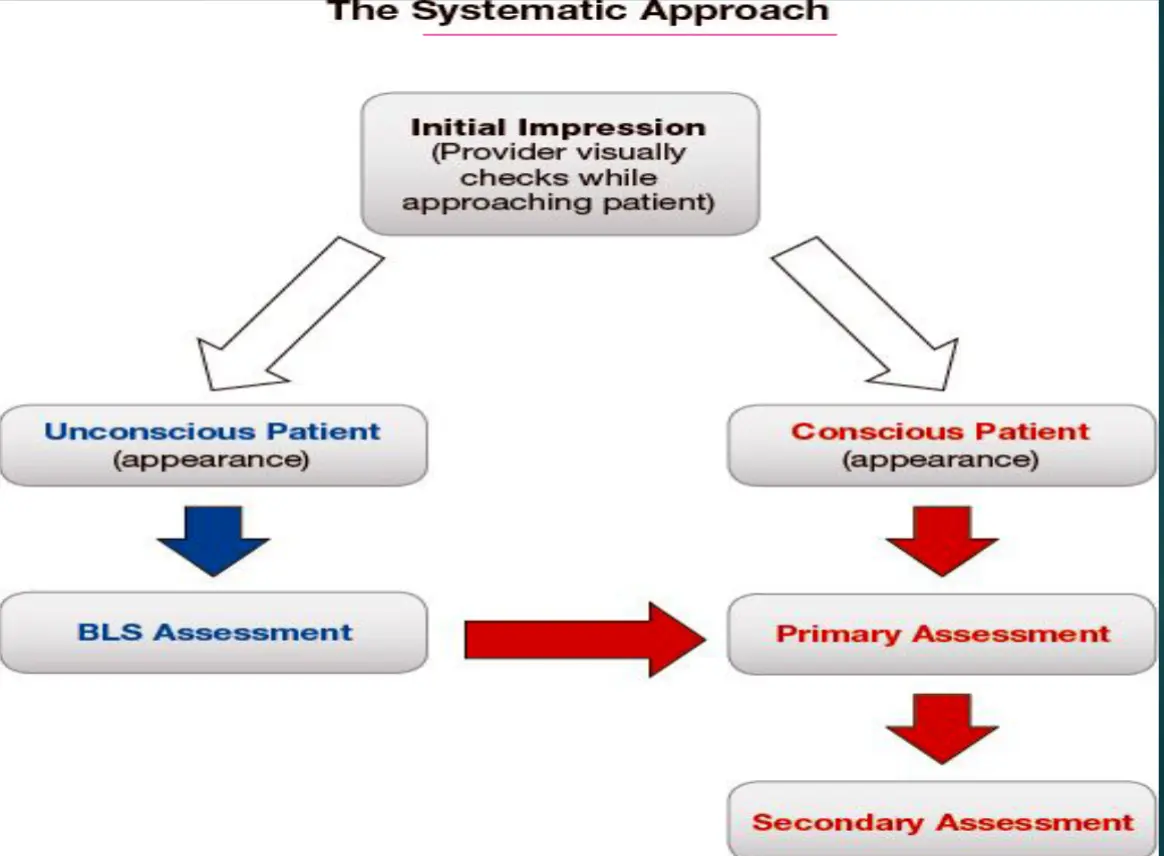
Unconscious Patient
- (appearance)
BLS Assessment
Conscious Patient
- (appearance)
Primary Assessment
Secondary Assessment
Expanded Systematic Approach Algorithm

Basic Life Support (BLS)
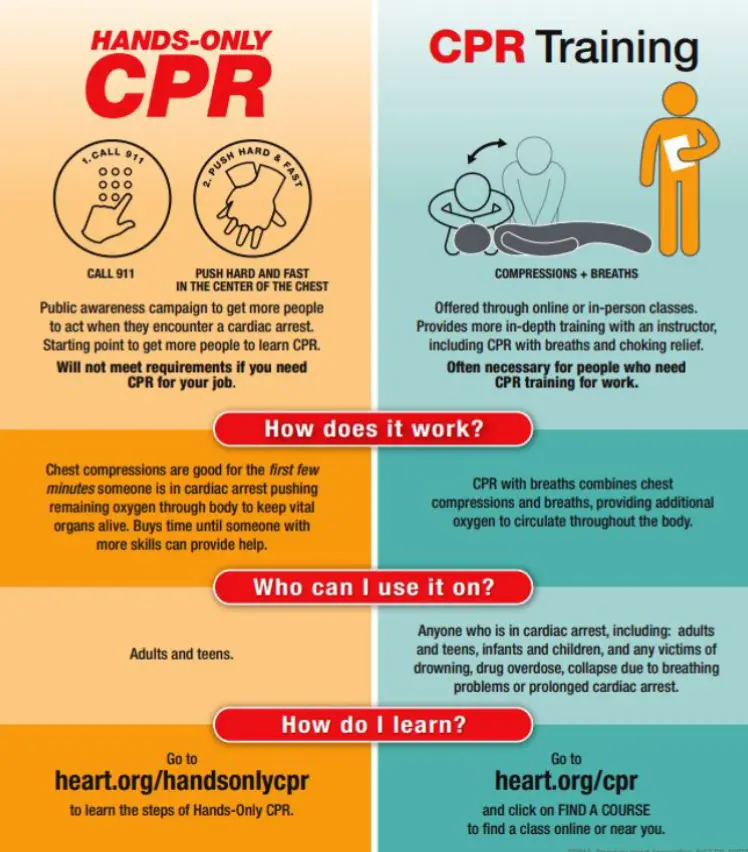
For the general public or bystanders who witness an adult suddenly collapse: compression-only CPR, or Hands-Only CPR. Hands-Only CPR is CPR without mouth-to-mouth breaths. It is recommended for use by people who see a teen or adult suddenly collapse in an out-of-hospital setting (such as at home, at work, or in a park).
Complete CPR Protocol
2 Steps to Save a Life
- Hands-Only CPR consists of two easy steps:
- 1. Call 911 \ 997 (or send someone to do that)
- 2. Push hard and fast in the center of the chest.
- Ischemic Heart Disease is the leading cause of death in the world
- 1 in 3 deaths in the U.S. is cardiovascular
- Most victims will die without immediate and appropriate intervention
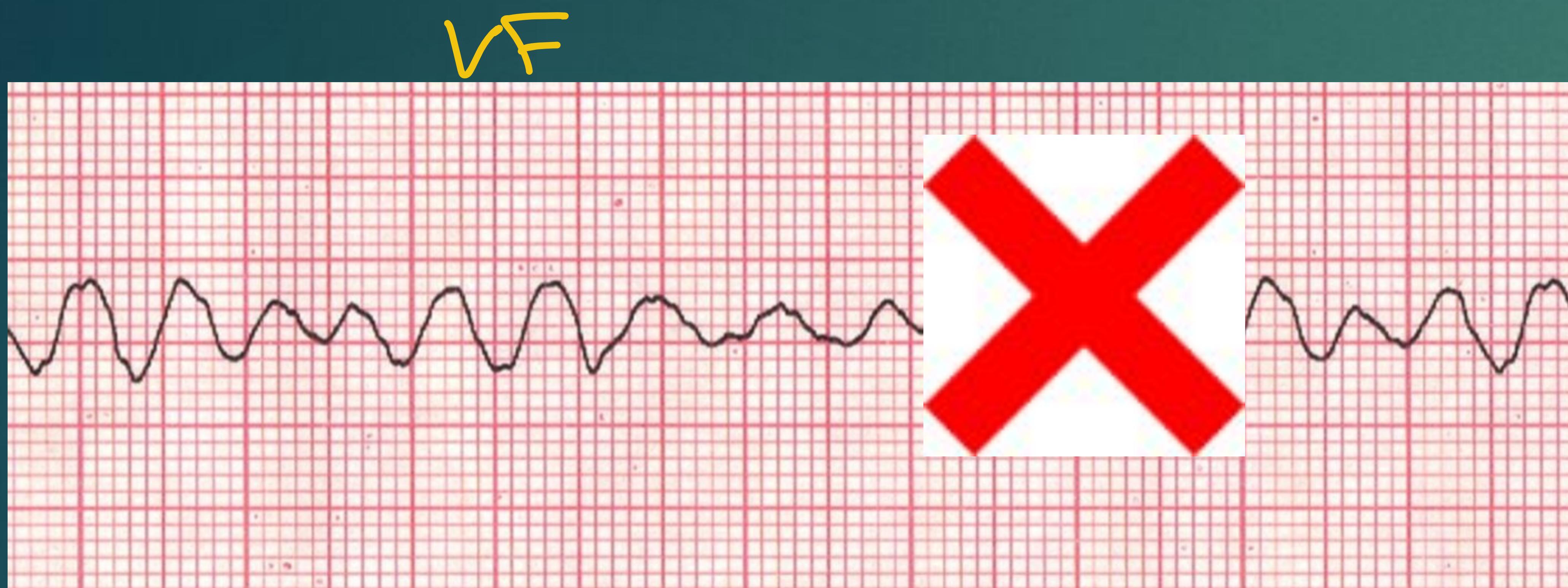
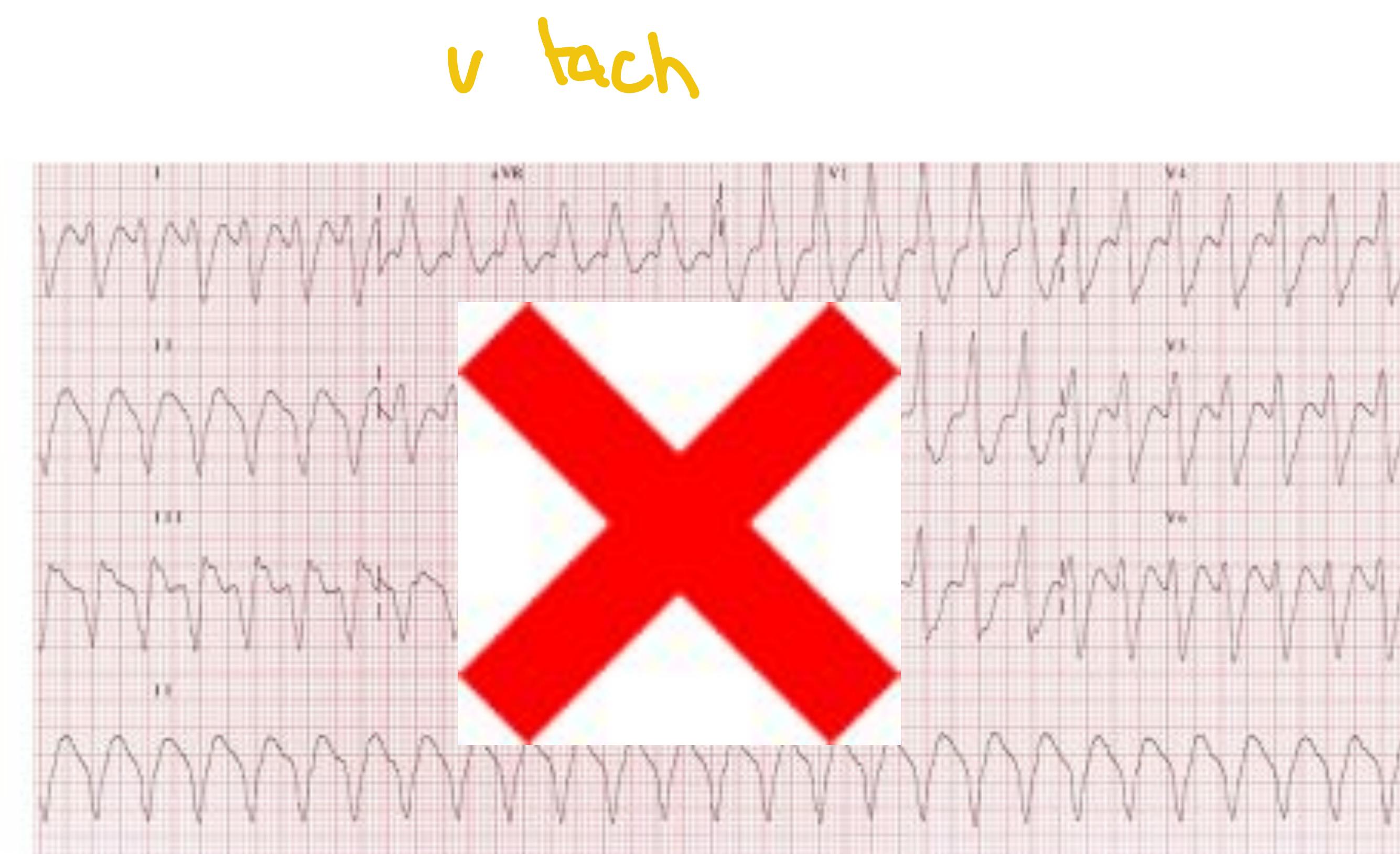
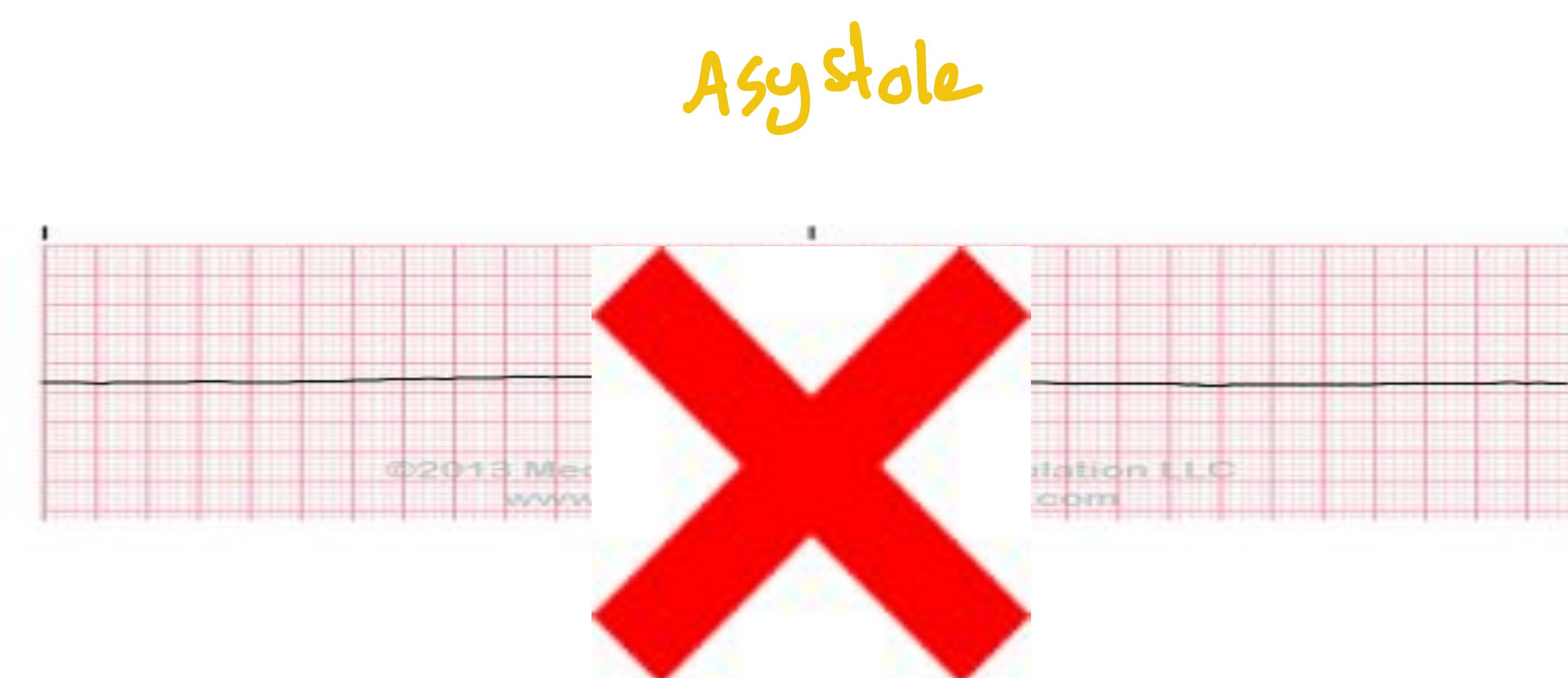
Cardiac Rhythm Prognosis
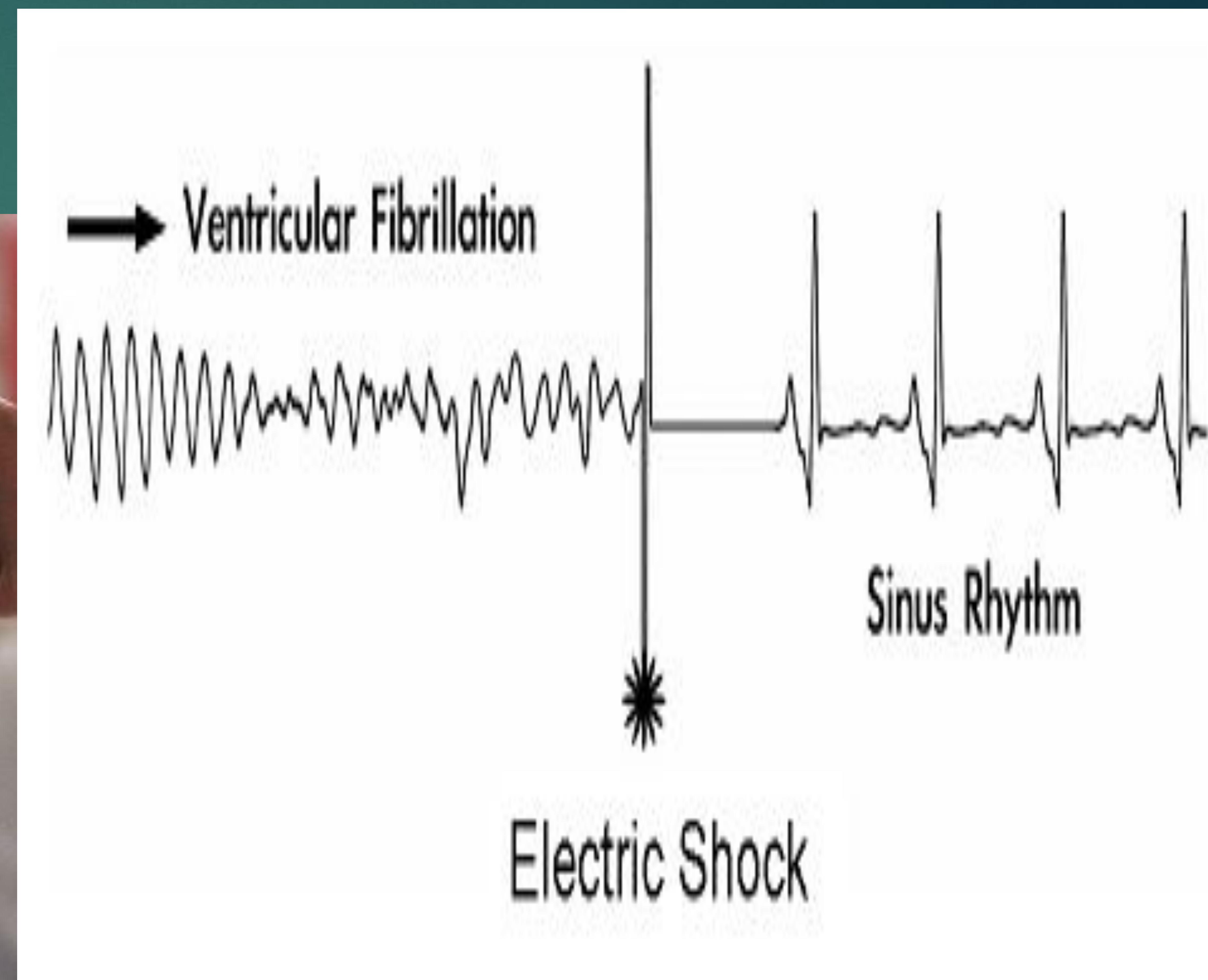
Cardiac arrest victims who present with ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) have a substantially better outcome compared with those who present with asystole or pulseless electric activity.
Ventricular Tachycardia (V Tach)
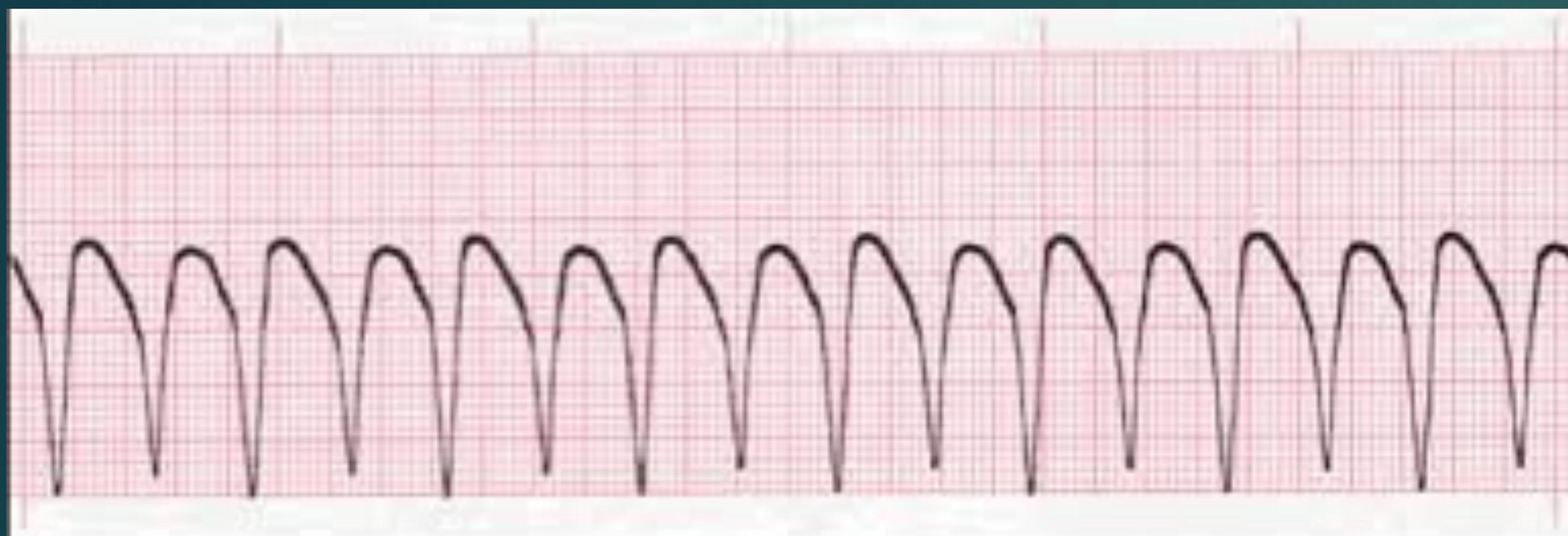
Which one has better prognosis?

Ventricular Fibrillation (VF)
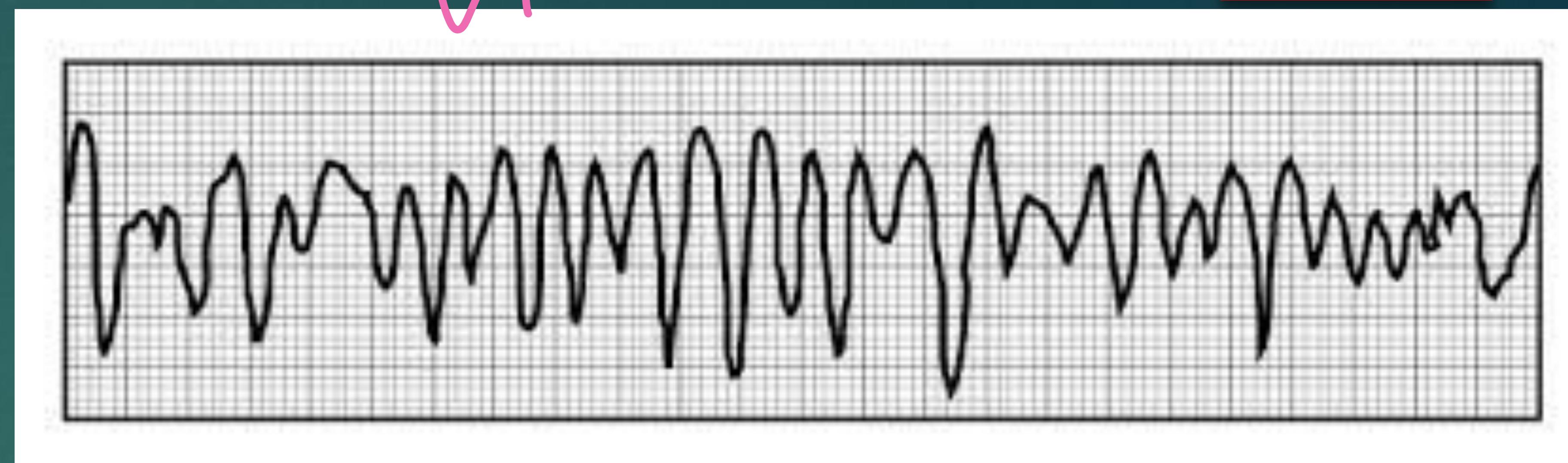
Asystole

Chain of Survival
Key Principles in Resuscitation
- Successful resuscitation following cardiac arrest requires an integrated set of coordinated actions represented by the links in the Chain of Survival.
Signs Needing Rapid Response Team Activation
- Hypotension
- ↓ O₂ saturation
- Tachycardia
- Tachypnea
- Respiratory coming down
If Arrested → Call emergency team

AHA Chains of Survival
In-Hospital Cardiac Arrest (IHCA)

- Early Recognition and Prevention
- Activation of Emergency Response
- High-Quality CPR
- Defibrillation
- Post-Cardiac Arrest Care
- Recovery
Out-of-Hospital Cardiac Arrest (OHCA)

- Activation of Emergency Response
- High-Quality CPR
- Defibrillation
- Advanced Resuscitation
- Post-Cardiac Arrest Care
- Recovery
If PIT Sabation allows me, I will try to Push the pit to cardiac center, but if not it’s enough to reach nearest general hospital
Adult Basic Life Support Algorithm for Healthcare Providers
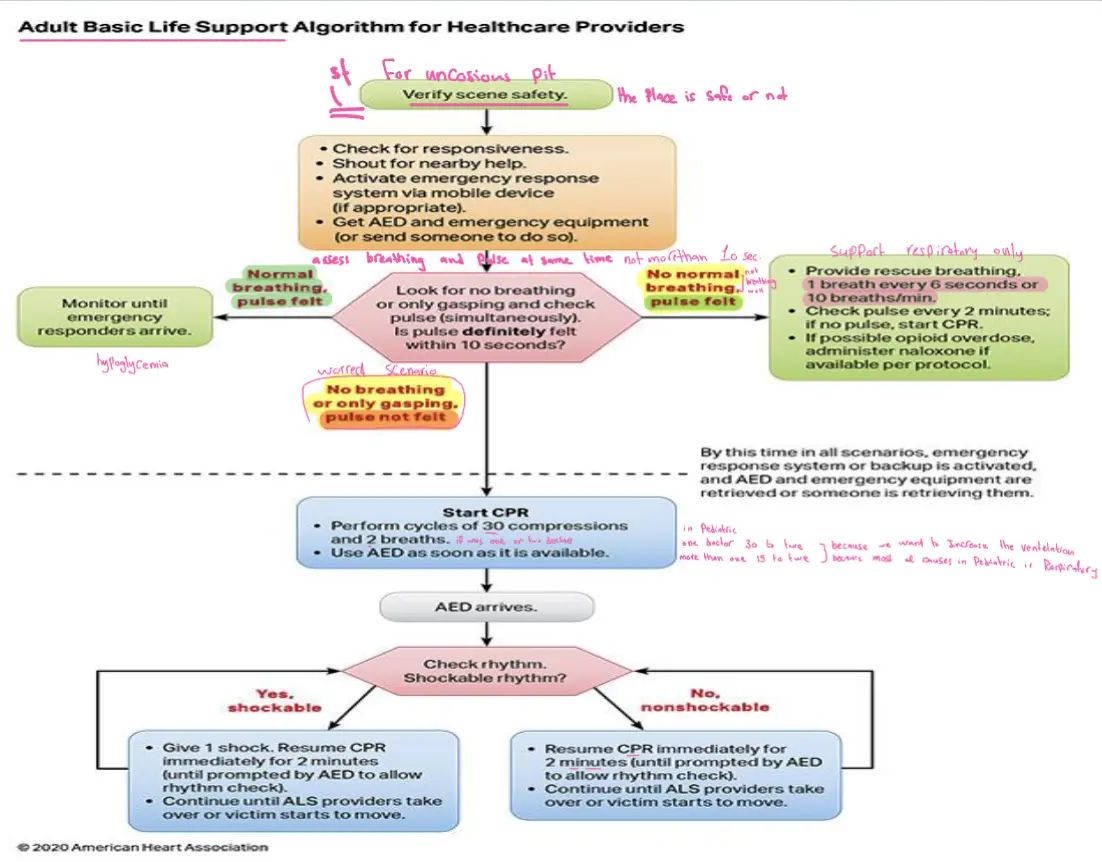
Initial Assessment
Assess Safety
- ► Witnessed or unwitnessed an unconscious victim
- ► Look for any danger, look out for blood spills, sharps, electric wire, unsteady beds, trolleys.
- ► Wear Personal Protective Equipment if available
- ► Make sure the victim and any bystanders are safe
Check for Responsiveness

If the patient is unconscious with abnormal or absent breathing, it is reasonable for dispatcher to assume that the patient is in cardiac arrest.

Call for help (Dial emergency number, call for ambulance and bring AED).
Check for Breathing and Pulse
- At least 5, but no more than 10 seconds.
- Check pulse and breathing at same time. (carotid don’t go with pharyngeal)
- If both absent, start CPR with chest compression.
- If pulse present, start rescue breathing at 1 breath every 6 seconds.
- (check pulse about every 2 minutes).


Patient Assessment Pathways
Look for no breathing or only gasping and check pulse (simultaneously). Is pulse definitely felt within 10 seconds? (assess breathing and pulse at same time not more than 10 sec.)
Normal Breathing, Pulse Felt
- Monitor until emergency responders arrive. (hypoglycemia)
No Normal Breathing, Pulse Felt
- Support respiratory only
- Provide rescue breathing, 1 breath every 6 seconds or 10 breaths/min.
- Check pulse every 2 minutes; if no pulse, start CPR.
- If possible opioid overdose, administer naloxone if available per protocol.
No Breathing or Only Gasping, Pulse Not Felt (Worst Scenario)
- By this time in all scenarios, emergency response system or backup is activated, and AED and emergency equipment are retrieved or someone is retrieving them.
- Start CPR
- Perform cycles of 30 compressions and 2 breaths. (if was one or two doctors)
- Use AED as soon as it is available.
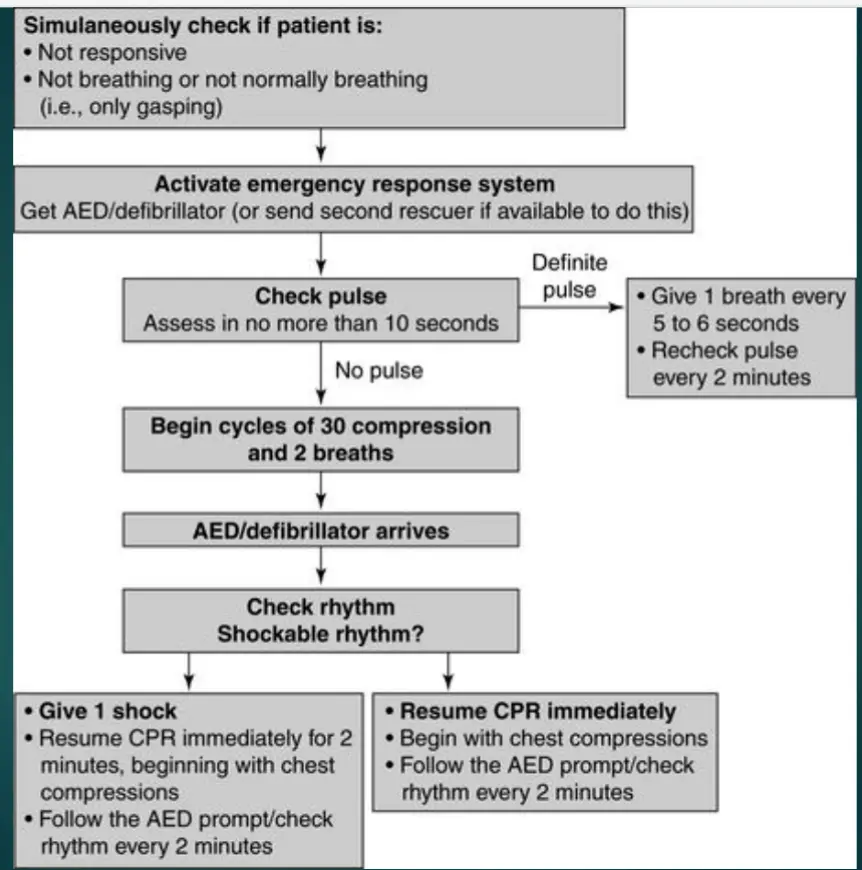
AED Protocol
AED arrives. Check rhythm. Shockable rhythm?
Yes, Shockable
- Give 1 shock. Resume CPR immediately for 2 minutes (until prompted by AED to allow rhythm check).
- Continue until ALS providers take over or victim starts to move.
No, Non-shockable
- Resume CPR immediately for 2 minutes (until prompted by AED to allow rhythm check).
- Continue until ALS providers take over or victim starts to move.
C-A-B Approach
With no Pulse Pit → any other Pit we go with ABC
-
The recommended sequence for a single rescuer has been confirmed: the single rescuer is to initiate chest compressions before giving rescue breaths (C-A-B rather than A-B-C) to reduce delay to first compression.
-
The single rescuer should begin CPR with 30 chest compressions followed by 2 breaths.
Chest Compressions
-
Look for normal breathing in not more than 10 seconds.
-
Start Chest Compressions (Cardiopulmonary Resuscitation (CPR)) if the victim not breathing.
Put my hands 2 Fingers above xiphoid process


Compression Technique
- Start high quality chest compressions. “Push hard, push fast”
- Middle chest, depth 5 to 6 cm, rate 100 – 120 compression per min, full recoil. (more than that will cause rib fracture for the chest)
- After 30 compressions, proceed with 2 ventilations (Each breath over 1 second, just enough to see chest rise).
- Ratio compressions to ventilation 30:2 in 1 cycle
- Check pulse at Carotid Artery after complete 5 cycle, continue CPR if no pulse is present.
Defibrillation
- Attach AED as available without interrupting compressing
- Follow AED promptly, manual defibrillator “Shock” if VF/VT rhythm recognized.
- Shockable rhythm: Give 1 shock, resume CPR immediately for 2 minutes.
- Non Shockable rhythm: Resume CPR immediately for 2 minutes.
- Check rhythm every 2 minutes.


Primary and Secondary Assessment
Primary Assessment Components
Airway
- Is the airway patent?
- Is an advanced airway indicated?
- Is proper placement of airway device confirmed?
- Is tube secured and placement reconfirmed frequently?
Breathing
- Are ventilation and oxygenation adequate?
- Are quantitative waveform capnography and oxyhemoglobin saturation monitored?
Circulation
- Are chest compressions effective?
- What is the cardiac rhythm?
- Is defibrillation or cardioversion indicated?
- Has IV/IO access been established?
- Is ROSC present?
- Is the patient with a pulse unstable?
- Are medications needed for rhythm or blood pressure?
- Does the patient need volume (fluid) for resuscitation?
Disability
- Check for neurologic function GS
- Quickly assess for responsiveness, levels of consciousness, and pupil dilation
- AVPU: Alert, Voice, Painful, Unresponsive
Exposure
- Remove clothing to perform a physical examination, looking for obvious signs of trauma, bleeding, burns, unusual markings, or medical alert bracelets
Secondary Assessment
SAMPLE History
- Signs and symptoms
- Allergies
- Medications (including the last dose taken)
- Past medical history (especially relating to the current illness)
- Last meal consumed
- Events
H’s and T’s (Reversible Causes)
| H’s | T’s |
|---|---|
| Hypovolemia | Tension pneumothorax |
| Hypoxia | Tamponade (cardiac) |
| Hydrogen ion (acidosis) | Toxins |
| Hypo-/hyperkalemia | Thrombosis (pulmonary) |
| Hypothermia | Thrombosis (coronary) |
Airway Management
Airway Techniques
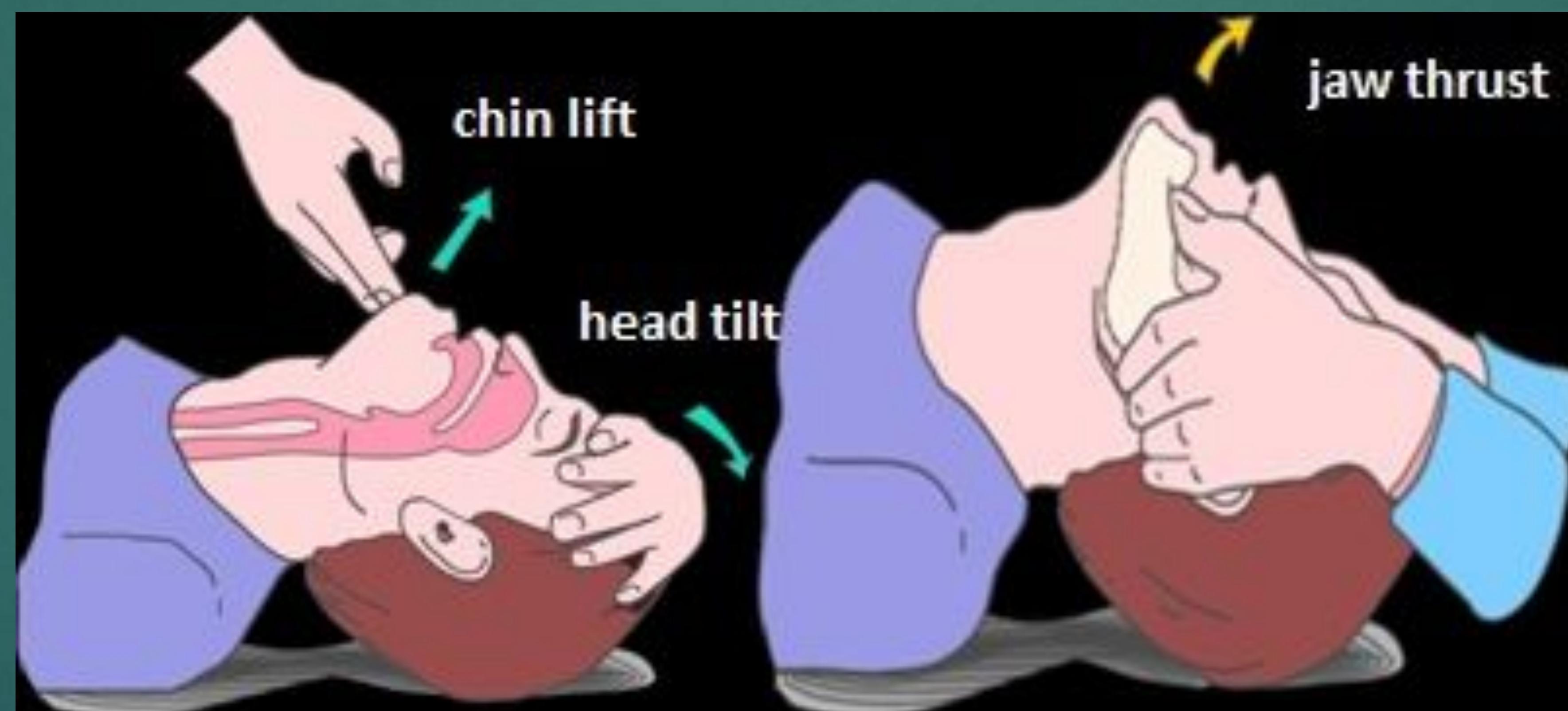
The Airway
- Open the airway using “Head tilt chin lift” technique or “Jaw Thrust” if cervical spine injury is suspected
- This lifts the tongue off the back of the throat, opening up the airway
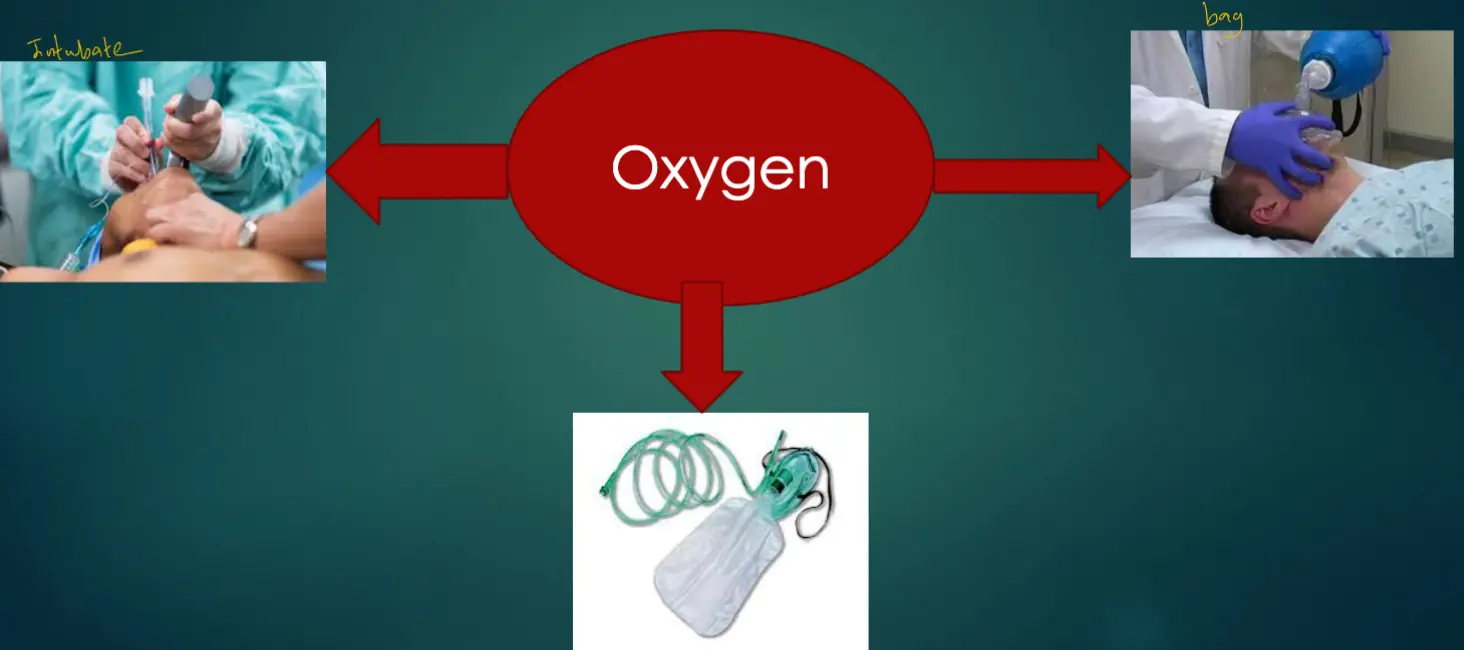
Breathing Support
Breathing Equipment
Oxygen → Intubate → Bag
Detailed BLS Algorithm
Age-Specific Considerations
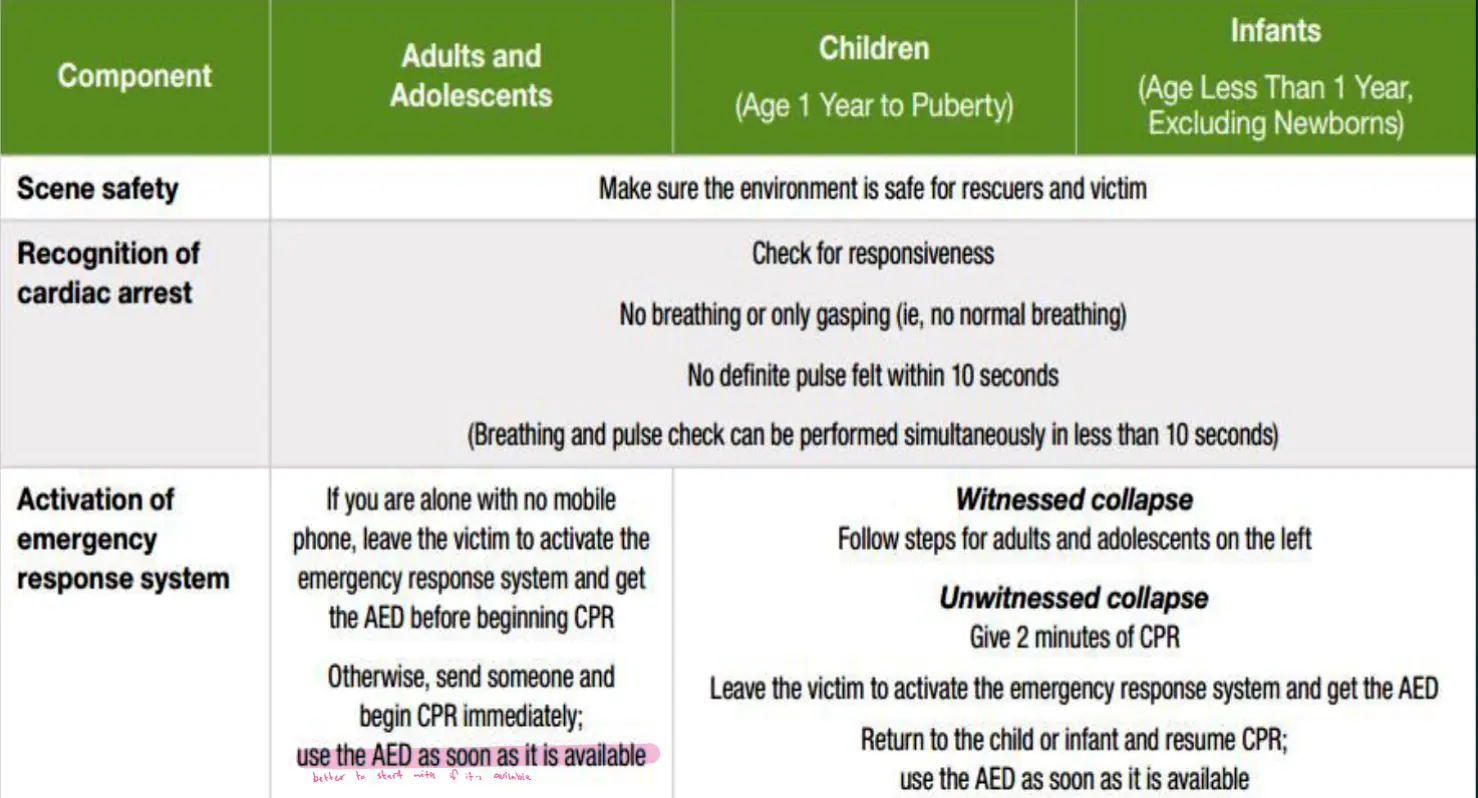
Algorithm Step-by-Step
Initial Assessment
Not too fast; Not too hard
100-120/min • 5-6cm deep
CPR Quality Guidelines
Rescuer Performance Standards
Rescuers Should
- Perform chest compressions at a rate of 100-120/min.
- Compress to a depth of at least 2 inches (5 cm) but not more than 2.4 inches (6 cm)
- Allow full recoil after each compression
- Minimize pauses in compressions
- Ventilate adequately (2 breaths after 30 compressions, each breath delivered over 1 second, each causing chest rise)
Rescuers Should Not
- Compress at a rate slower than 100/min or faster than 120/min.
- Compress to a depth of less than 2 inches (5 cm) or greater than 2.4 inches (6 cm).
- Lean on the chest between compressions.
- Interrupt compressions for greater than 10 seconds.
- Provide excessive ventilation (ie, too many breaths or breaths with excessive force)
Shock First vs CPR First
- For witnessed adult cardiac arrest when an AED is immediately available, it is reasonable that the defibrillator be used as soon as possible.
For adults with unmonitored cardiac arrest or for whom an AED is not immediately available, it is reasonable that CPR be initiated while the defibrillator equipment is being retrieved and applied and that defibrillation, if indicated, be attempted as soon as the device is ready for use.
Advanced Cardiac Life Support (ACLS)
ACLS Fundamentals
“The foundation of successful ACLS is good BLS”
- ACLS guidelines first published 1974 by AHA, most recent update 2015
- A series of interventions for urgent treatment of cardiac arrest, stroke, and life threatening medical emergencies
- Several algorithms for VF/Pulseless VT, Bradycardia, Suspected Stroke
- An essential part of using the algorithm correctly is to search for and correct potentially reversible causes of arrest
- Performing high quality CPR, identifying arrhythmias and understanding the pharmacology behind key drugs are central to ACLS.
Adult Cardiac Arrest Algorithm
No Pulse
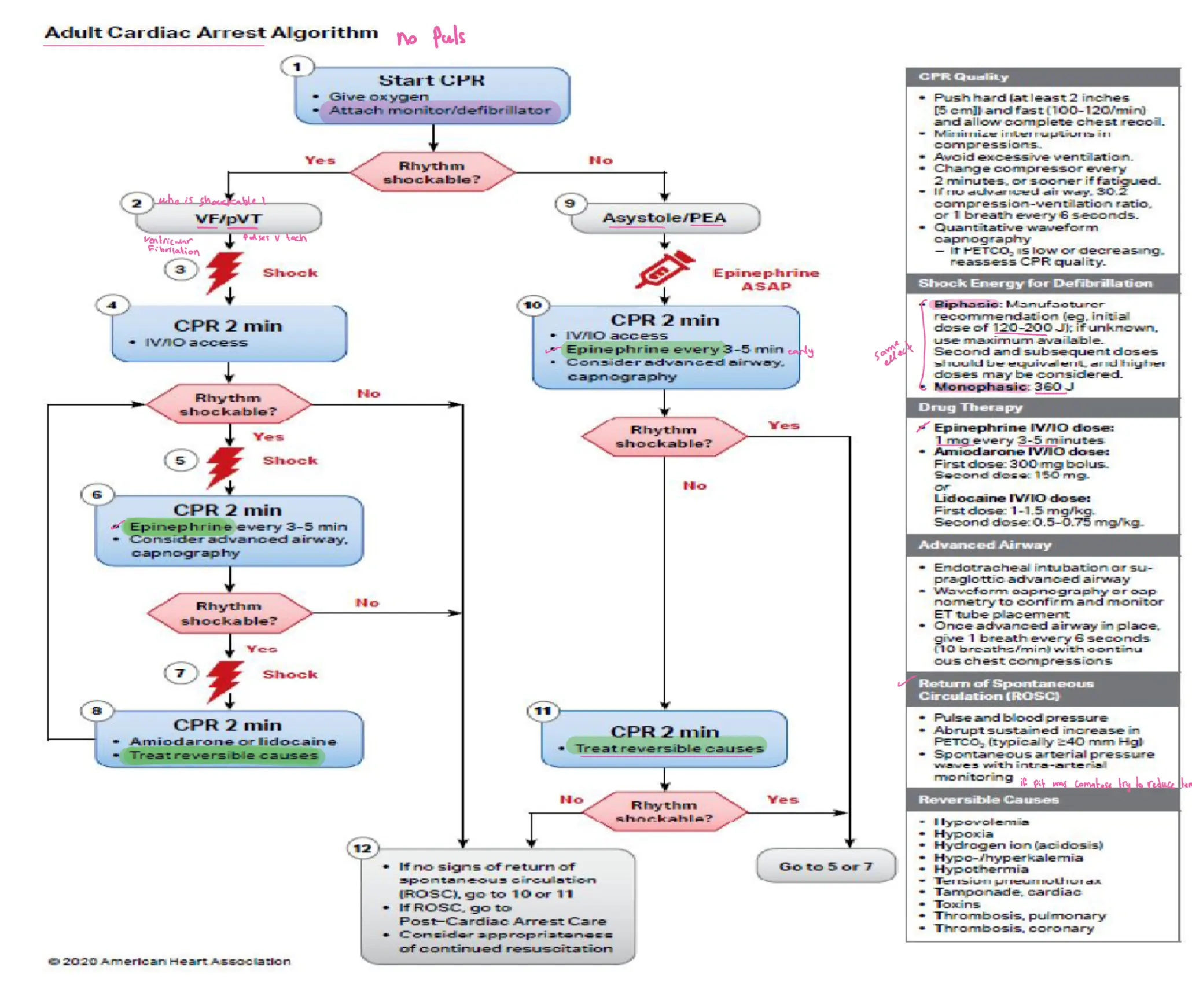
Cardiac Rhythm Recognition and Management
Ventricular Fibrillation (VF)
Ventricular fibrillation → go for shock
Characteristics: bizarre shape
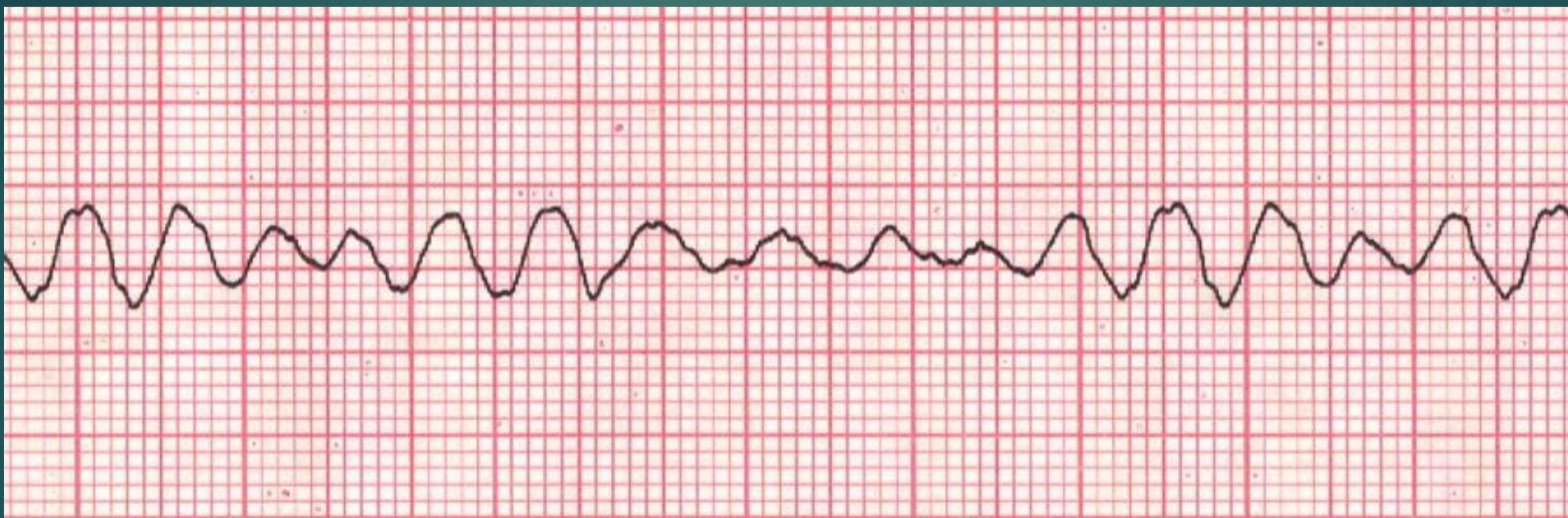
Ventricular Tachycardia
No Pulse → Shock
Pulse → Not shockable
Characteristics: wide QRS → from ventricle
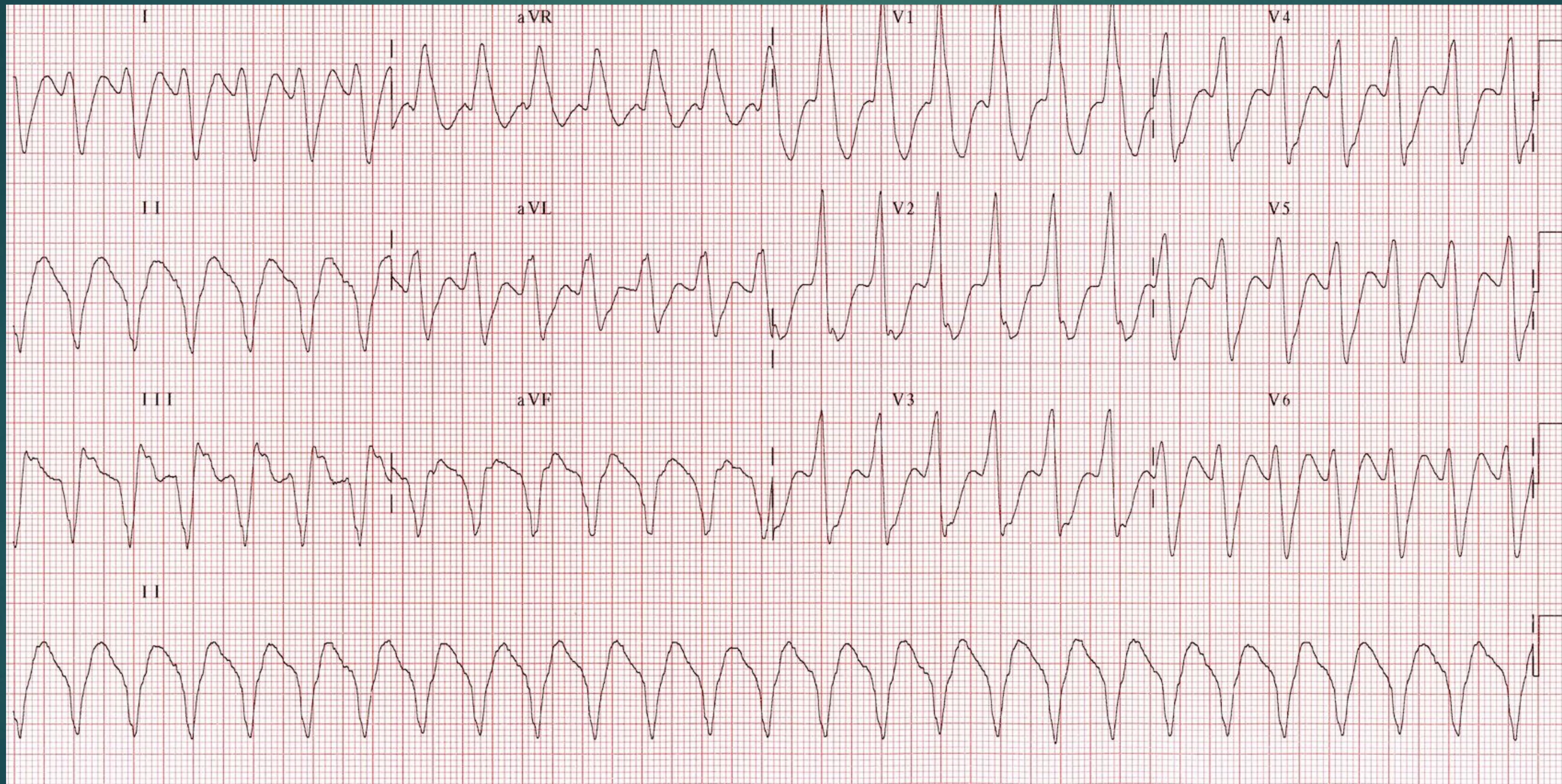
Asystole
Flat line protocol:
- Check the connection between pit and machine
- Check the other leads 1 and 3
- Increase the size of ECG
- Epinephrine
- CPR
→ in lead 2

Pulseless Electrical Activity (PEA)
Epinephrine • CPR
There is activity in monitoring, but no pulse. All cases except these 3:
- VF
- VT
- Asystole
Detailed Reversible Causes (H’s and T’s)
Hypoxia
- Pulmonary embolism
- CO Poisoning
- Exacerbation of Asthma or COPD
- Lung trauma
Hypovolemia
- Bleeding
- Rupture embolism
- Rupture ectopic pregnancy
Hydrogen Ion (Acidosis)
- DKA
- ARF
Hypokalemia
- Vomiting
- Dehydration
Hyperkalemia
- ARF
- Treated by Calcium to protect heart
- Insulin - Glucose
- β agonist
- Dialysis
Hypothermia
- Exposure to cold weather
- Endocrine causes
Thrombosis (Pulmonary)
Thrombosis (Coronary)
Tamponade
- Fluid in Pericardiac
- No space for heart contraction
- Pericardiac Centesis
Tension Pneumothorax
- Critically diagnosed
- Needle decompression followed by tube
Toxins
- Anti-dote
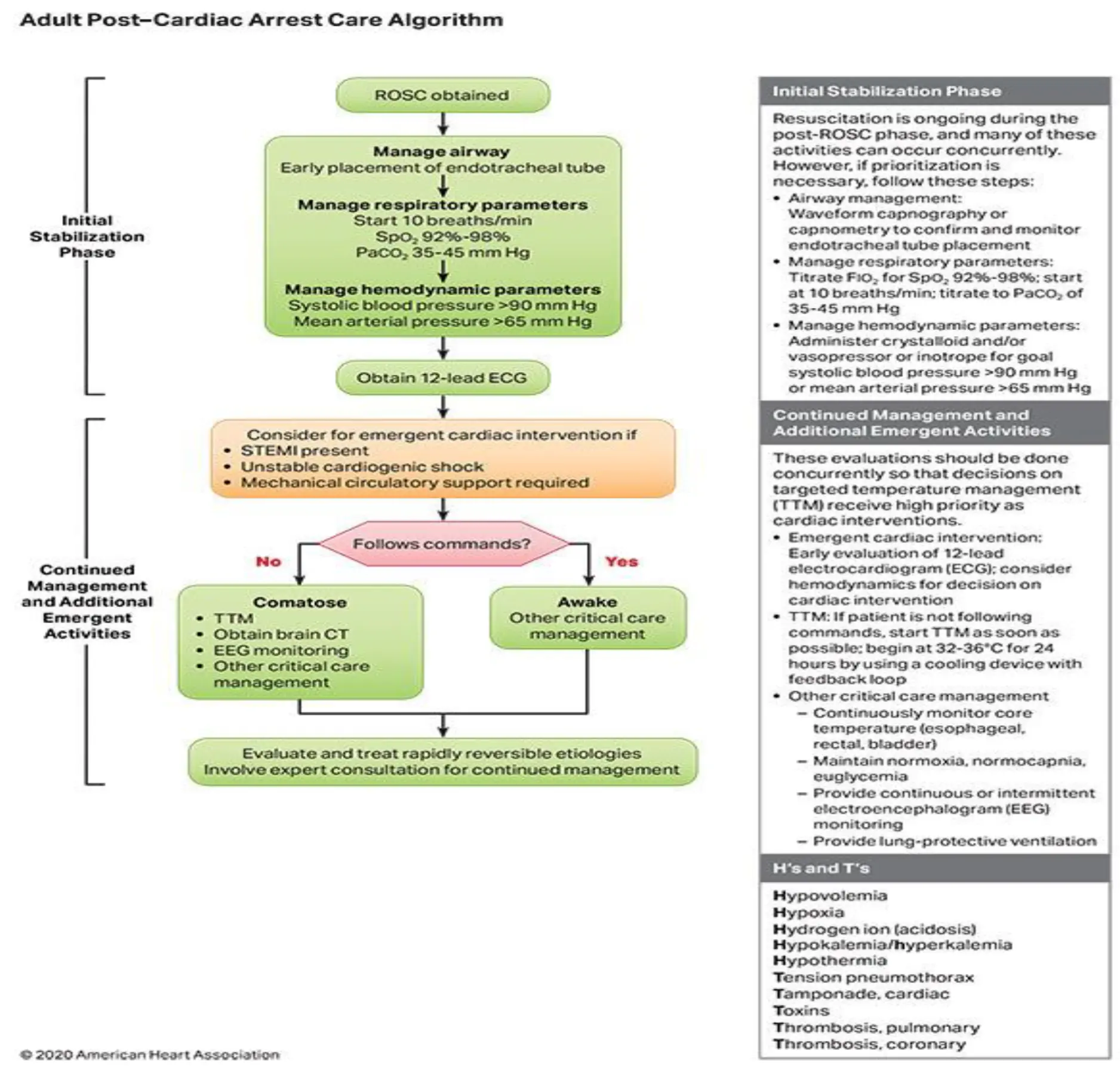
Comprehensive Adult Cardiac Arrest Protocol
Bradycardia Management
Bradycardia Types
There are 2 types:
Absolute
- HR < 60
Relative
- Normal number but it’s abnormal for the condition.
- Example: Child with trauma he has hypotension but Pulse is 70 [normal but according to case he should be tachy]
Adult Bradycardia Algorithm
Tachycardia Management
Tachycardia Overview

TACHYCARDIA IS DEFINED AS A HEART RATE ABOVE 100 BEATS PER MINUTE, BUT SYMPTOMATIC TACHYCARDIA GENERALLY INVOLVES RATES OVER 150 BEATS PER MINUTE, UNLESS UNDERLYING VENTRICULAR DYSFUNCTION EXISTS
Adult Tachycardia With a Pulse Algorithm
Narrow-Complex Tachycardia
Differential Diagnosis:
- Sinus tachycardia (with stress)
- Supraventricular tachycardia
- Atrial fibrillation
- Atrial flutter
- Multifocal atrial tachycardia
Sinus Tachycardia
Treat the cause.
- Pain
- Fever
- Stress
- Caffeine
- Anemia
Characteristics: P wave follow by narrow Complex

Supraventricular Tachycardia (SVT)
No Pulse - PEA
- Epinephrine
- CPR
With Pulse
- Check stability.
- If stable:
- Vagal maneuver
- Adenosine
- Beta or calcium channel blocker (if I give it for unstable pt he will has bad prognosis he may arrest)
- If stable:
- Cardioversion if unstable
Characteristics: No P wave • Regular • Narrow Complex • HR > 140

Atrial Fibrillation
- Check stability. Unstable → Cardioversion Stable → β-Blocker - CCB
- Control rate
- Control rhythm
Characteristics: Irregular
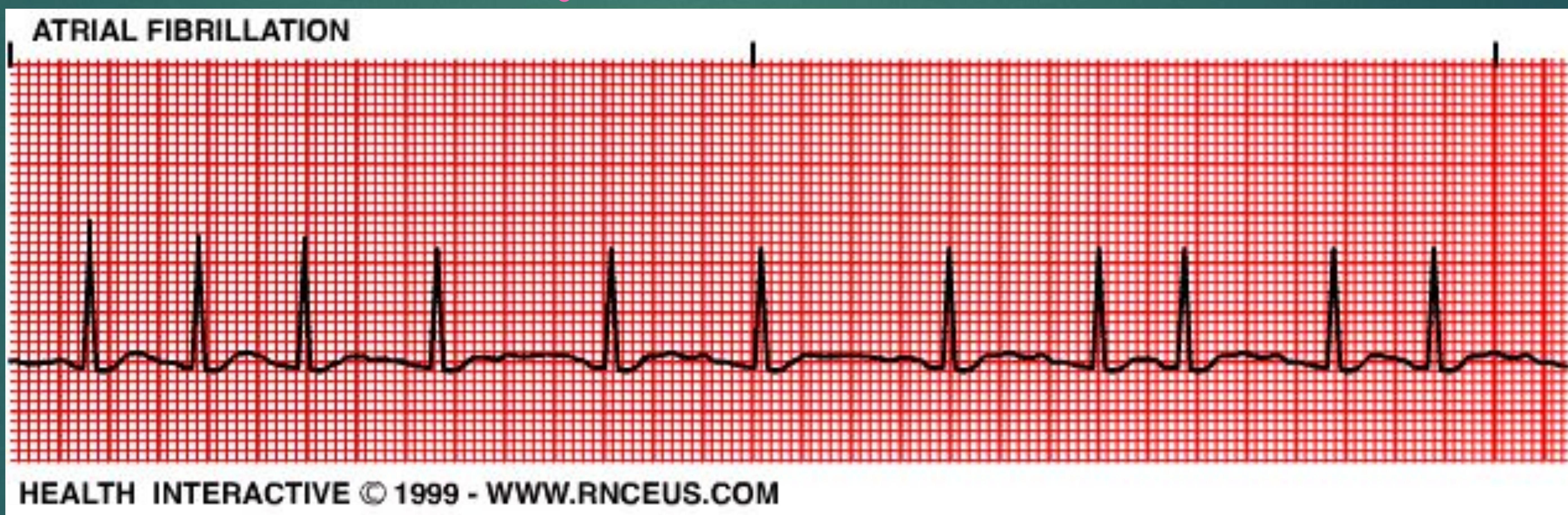
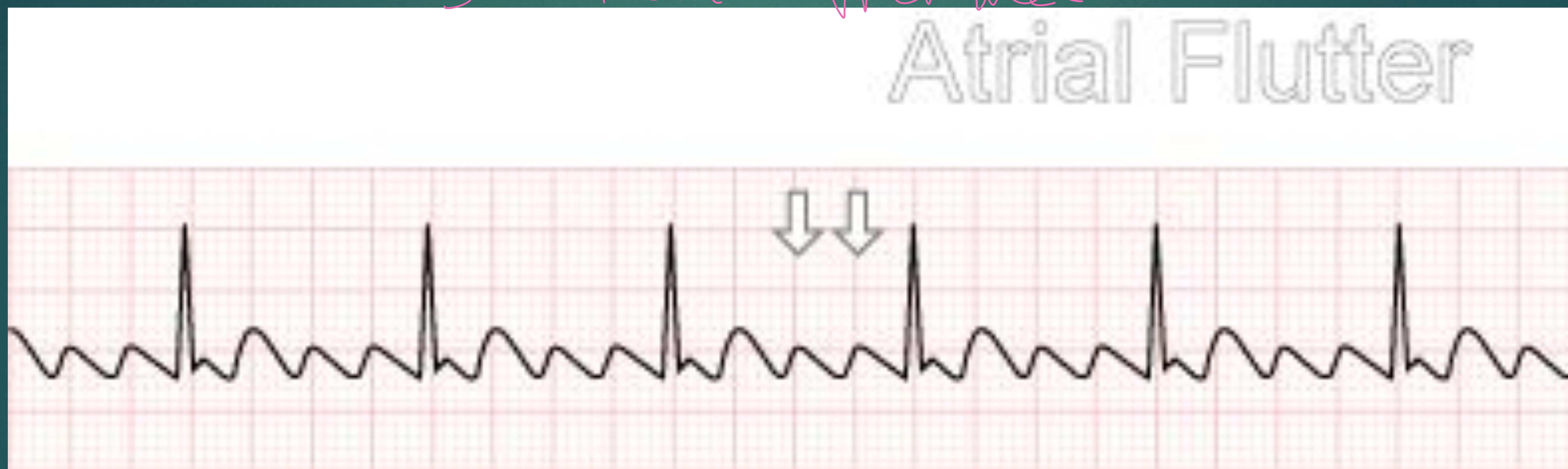
Atrial Flutter
- Same as Atrial Fibrillation.
Characteristics: Saw tooth appearance
Treat the cause mainly hypoxia.
Multifocal Atrial Tachycardia (MAT)
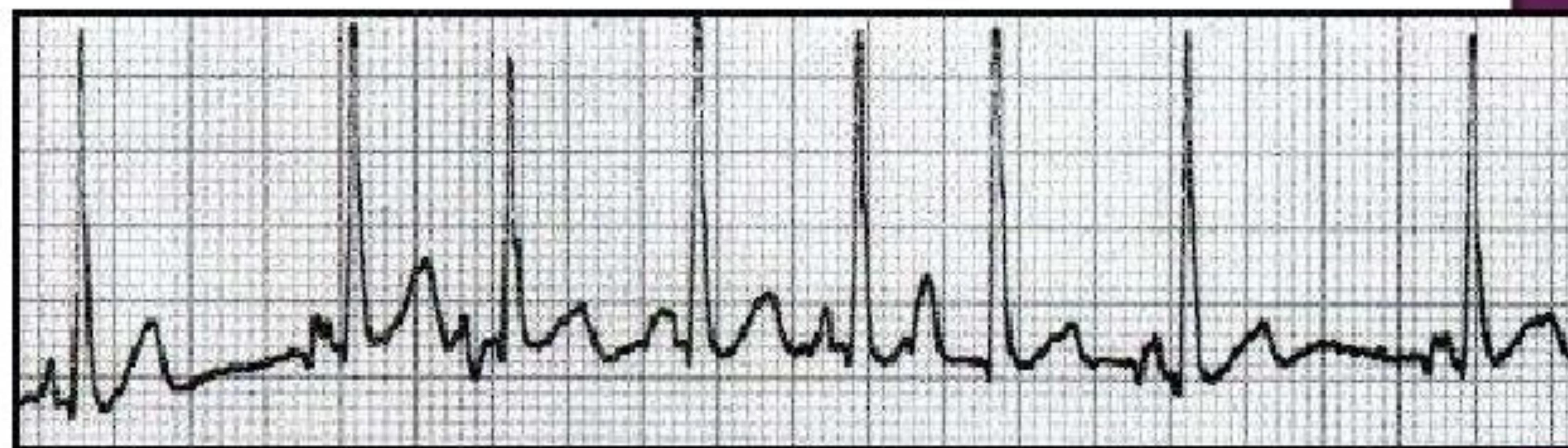
ECG Characteristics:
- Discrete P waves with at least 3 different morphologies
- Absence of one dominant atrial pacemaker
- Atrial rate > 100 bpm
- The PP, PR, and RR intervals all vary
→ usually with hypoxia • Asthma - COPD • So treat the hypoxia • no place for other medication
Wide-Complex Tachycardia
Wide-Complex Tachycardia Overview
Characteristics: > 3 small squares
- Most dangerous
- Ventricular tachycardia
- SVT with aberrancy → left bundle or Right bundle
- SVT with WPW syndrome (accessory pathway)
- AF with aberrancy (already has left or Right bundle branch then he develop AF)
- AF with WPW (accessory pathway between Atrial and ventricle WPW syndrome)
SVT with Aberrancy
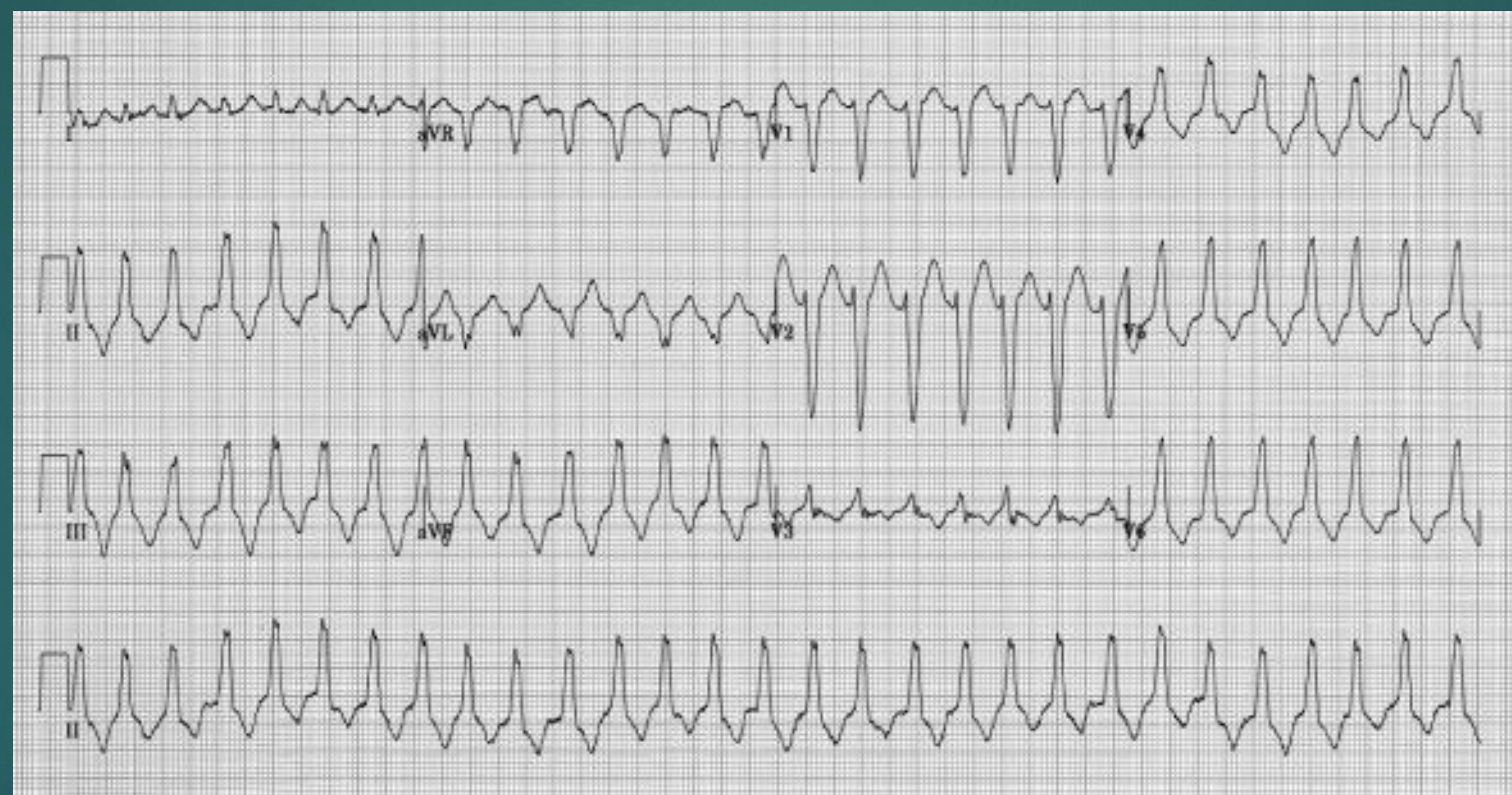
SVT with WPW
Delta wave
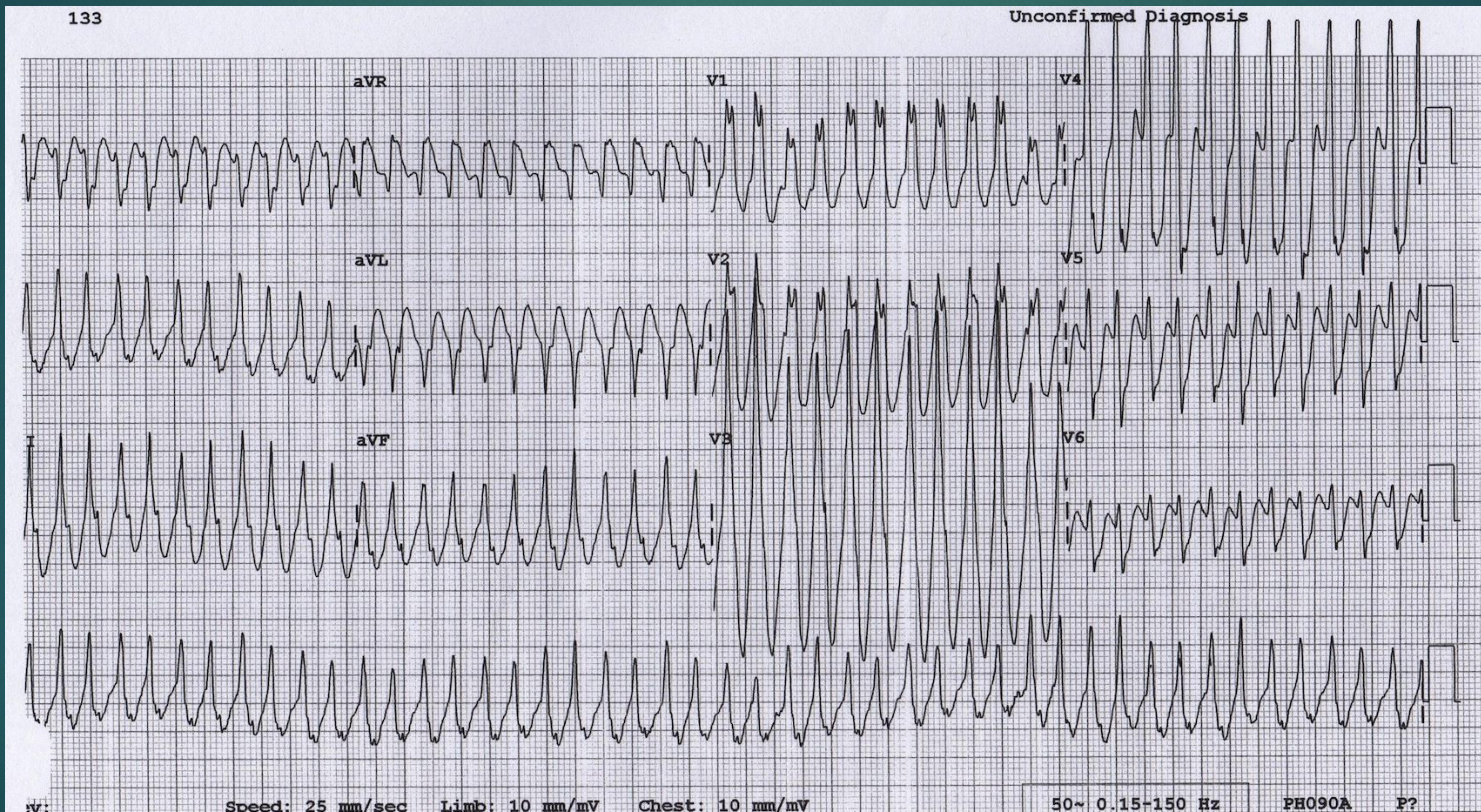
ECG parameters visible on the tracing:
- Speed: 25 mm/sec
- Limb: 10 mm/mV
- Chest: 10 mm/mV
- Frequency filter: 50~ 0.15-150 Hz
- Machine identifier: PH090A
- Marker: P?
AF with WPW
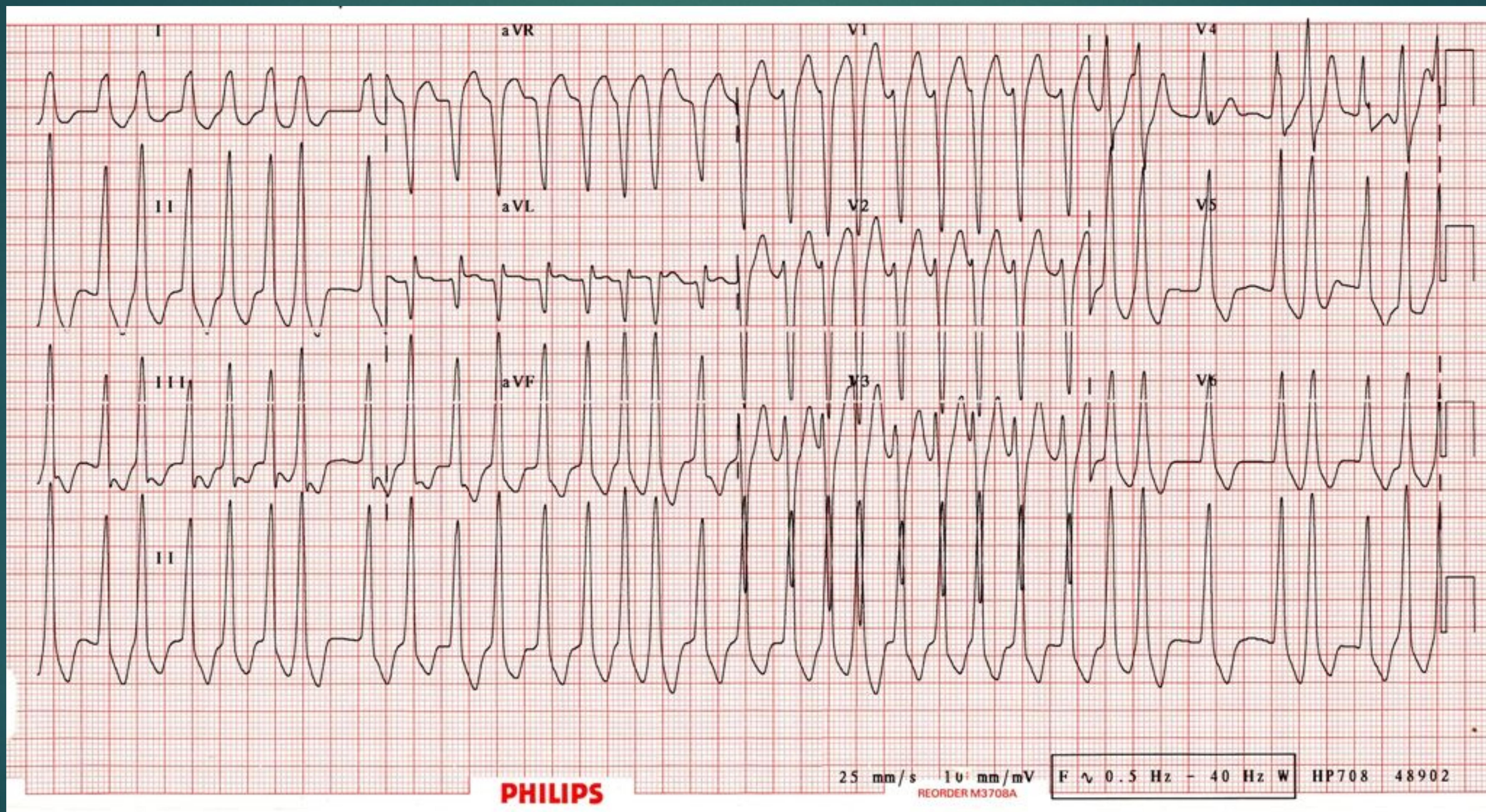
- Check stability.
- Safe to treat as VT.
Consider the worst and be in safe side
Pulse
- No: CPR, defibrillation
- Yes: Stability
- Stable: medication
- Unstable: Cardioversion
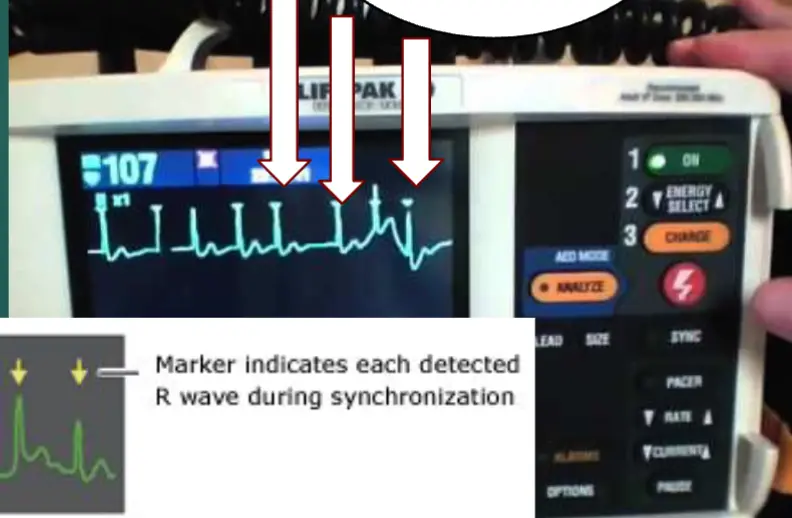
Two mode in one machine “Life bag”
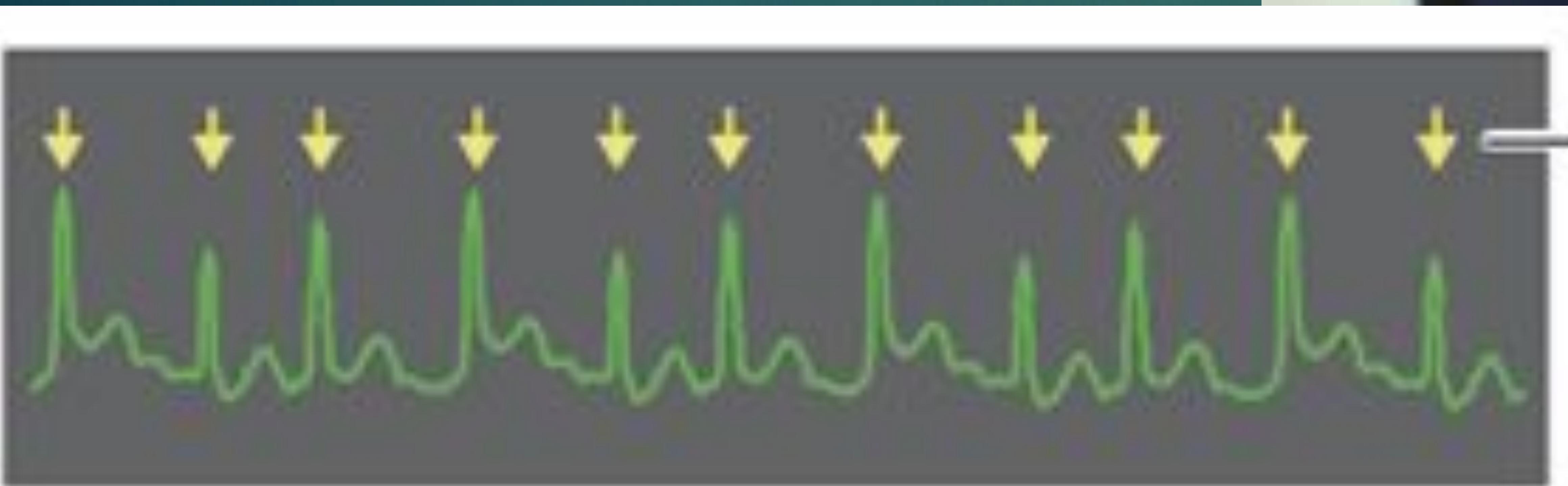
Cardioversion vs Defibrillation
Comparison Table
| Use in | All tachycardia except VF and pulseless VT | VF and pulseless VT - Shockable |
|---|---|---|
| Synchronize | Synchronize | Asynchronous |
| Sedation | Need sedation and analgesia | No need. Patient Arrested |
| Energy | Low energy shock | High energy shock highest |
| Shock will deliver | delivers shock with peak of QRS ( Synchronize ). ARP absolute refractory period | delivers as soon as shock button is pushed ( asynchronous ). RRP relative refractory period |
| Screen of monitor | Dots in monitor | No dots. |
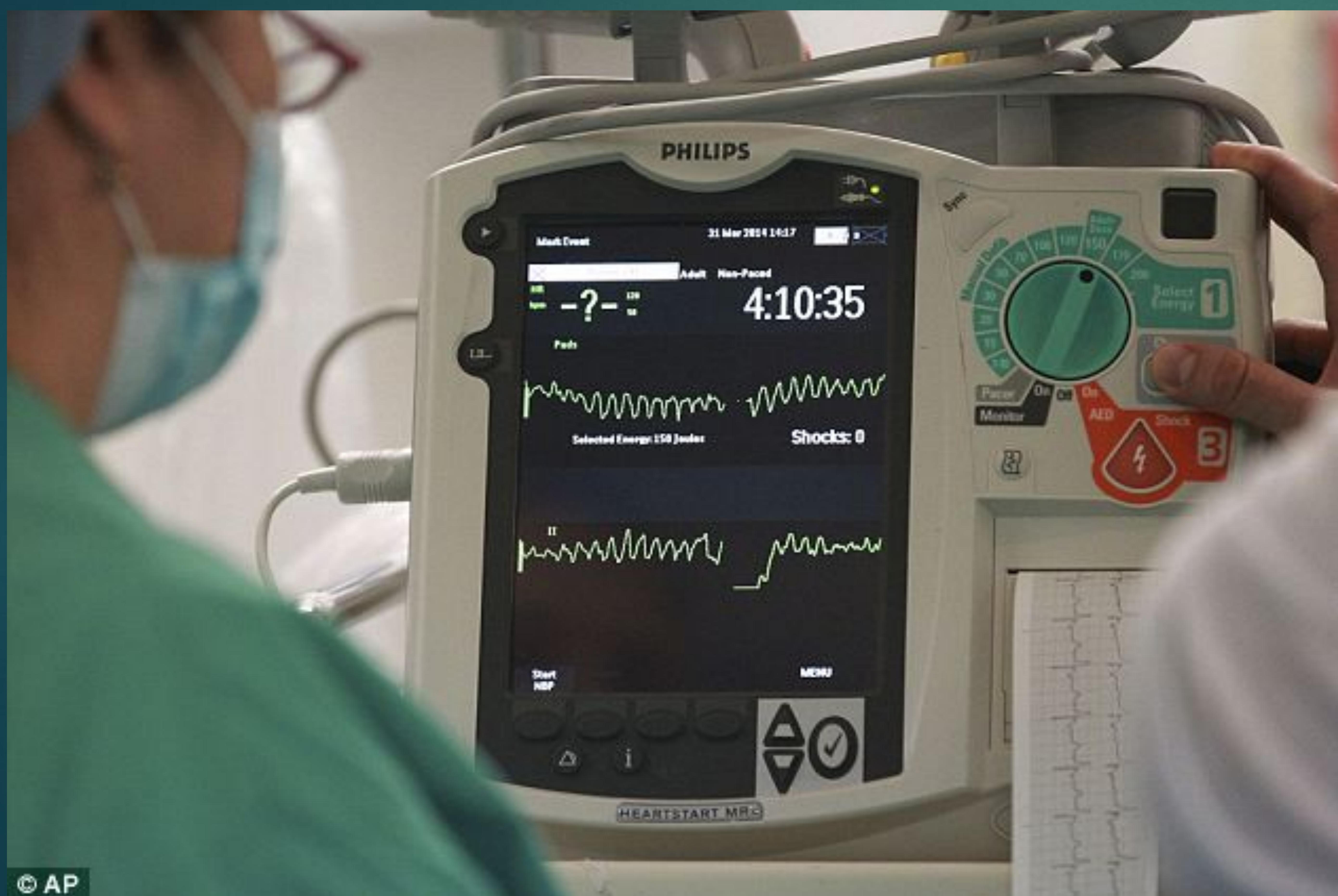
| cc images |
Cardioversion Details
You can see dots in the monitor
Marker indicates each detected R wave during synchronization
Defibrillation
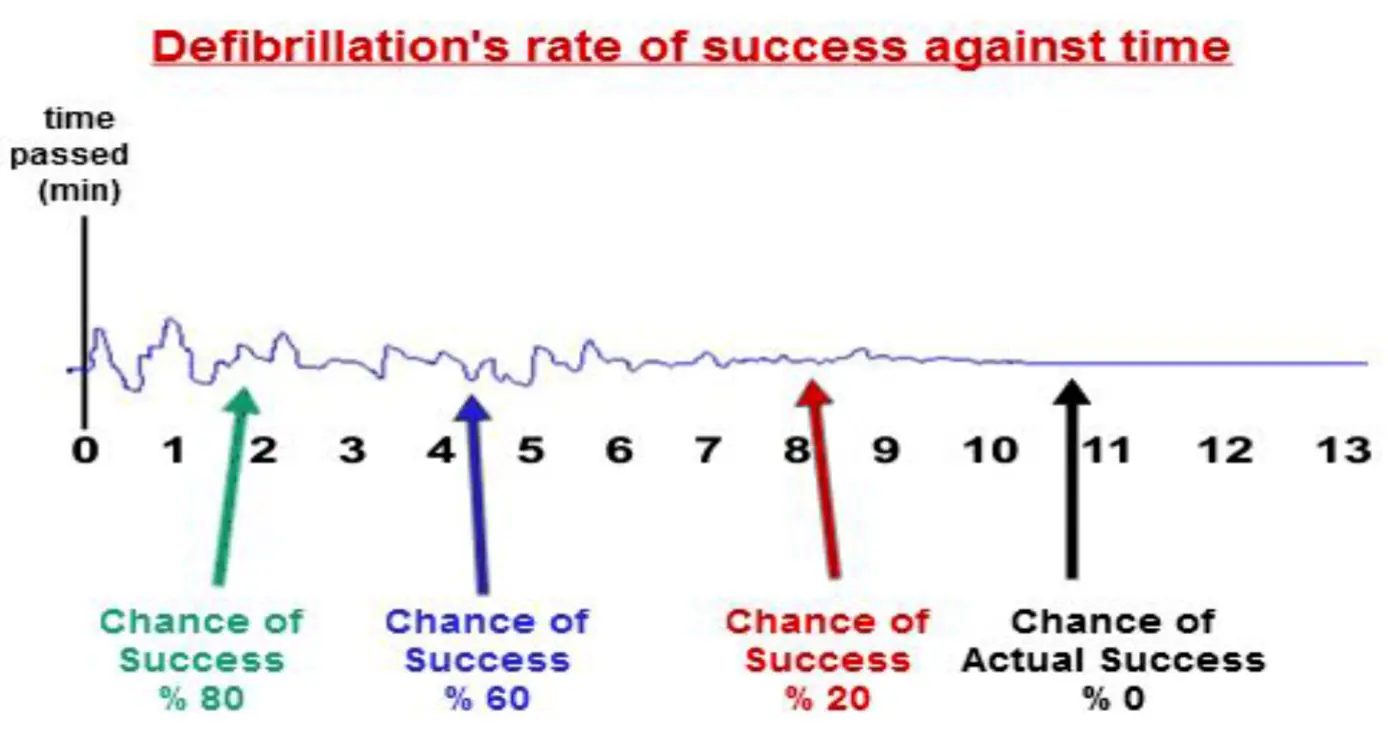
Defibrillation Success Rate
Defibrillation’s Rate of Success Against Time