Airway practice
- open the airway
- Maneuvers (to open the airway)
- JT (Jaw thrust)
- HT/CL (Head tilt / Chin lift)
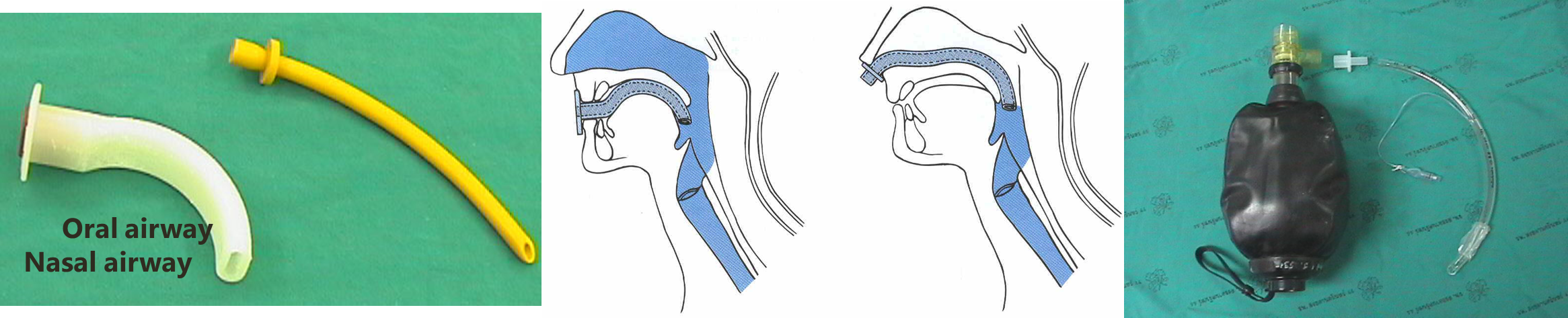
- Airway adjuncts (to maintain airway)
- OPA (oropharyngeal airway)
- Contraindicated in conscious/semiconscious patients as it triggers gagging.
- Use: To keep the airway open for a long time in an unconscious patient.
- NPA (nasopharyngeal airway)
- Used in conscious/semiconscious patients.
- Contraindicated in maxillary/basal skull fracture.
- Could be used in both nostrils.
- OPA (oropharyngeal airway)
- Maneuvers (to open the airway)
Now the airway is patent, so we need O2 to pass. Assess for spontaneous effort or help him by ventilation.
Aspiration is the enemy.
- Fluid instead of air in the alveoli.
- A cuffed tube in the trachea is the definitive prevention.
Breathing (oxygenation + ventilation)
- BMV (bag mask valve) ventilation more leak
- supraglottic airway (LMA) less leak
- definitive airway (ETT) → should have cuffed in trachea that Prevent aspiration because all air go to trachea direct I have full control.
In Anesthesia
Timeline: NPO → ① Sedation → ② BMV → ③ Paralytics → ETT
In ER
- Example: emergency C-section
- (RSI): rapid sequence induction
Timeline: Spontaneous breathing → ① Sedation + paralytic → ② ETT
Note: No BMV because the patient is not prepped, so they have a full stomach & BMV may cause aspiration.
Indications for intubation in ER
- Airway
- obstruction
- protection
- Breathing (O2/CO2) ex. hypoxemia (COPD)
- Anticipated course…
Intubation as prevention in semi normal seizure - Burn - transfer pt through helicopter
Q: Is it crash?
(need Immediate Intubation)
- Yes → Crash algorithm (dead or dying)
- without using medication
- ex. cardiac arrest
- No ↓
Q: Is it difficult?
- Yes → Difficult algorithm
- if not succeeded we can use one dose of paralytic (sedation)
- call seniors + more advanced devices
sever facial trauma - huge neck tumor - I’m not able to see vocal cord
- No ↓
RSI Algorithm (Intubation in Patient who have full stomach)
| v
can’t O₂
oxygenate at any time
→ failed airway ↓ should do surgical airway (cricothyrotomy)
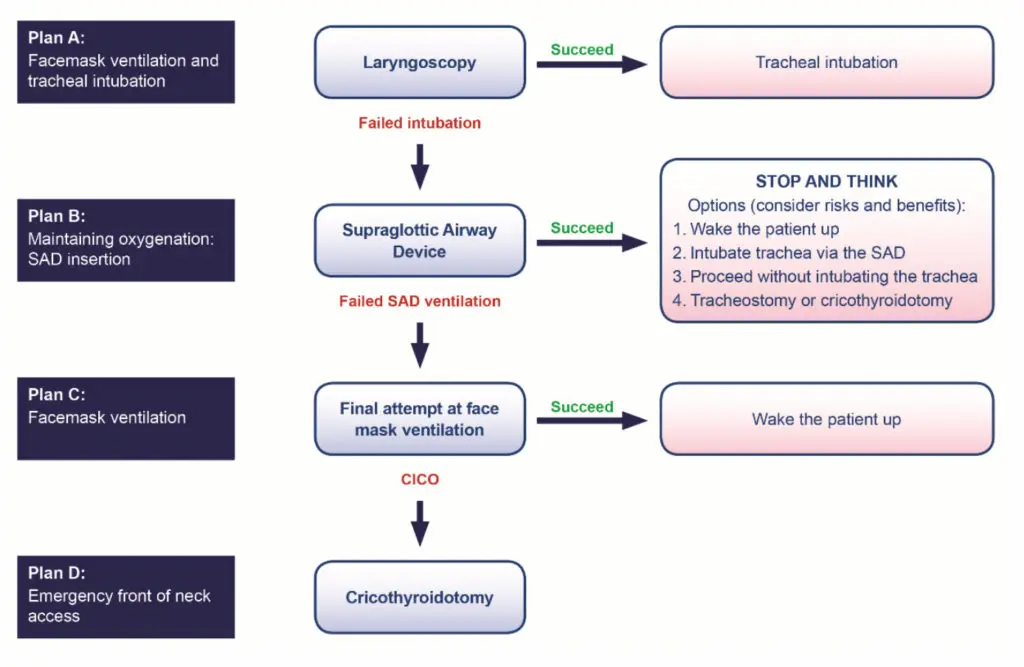
Difficult, failed, RSI
Procedure
https://www.youtube.com/watch?v=cF2PZ5NpcLA https://www.youtube.com/watch?v=I7o6WB1oMU0
Air way assessment Z
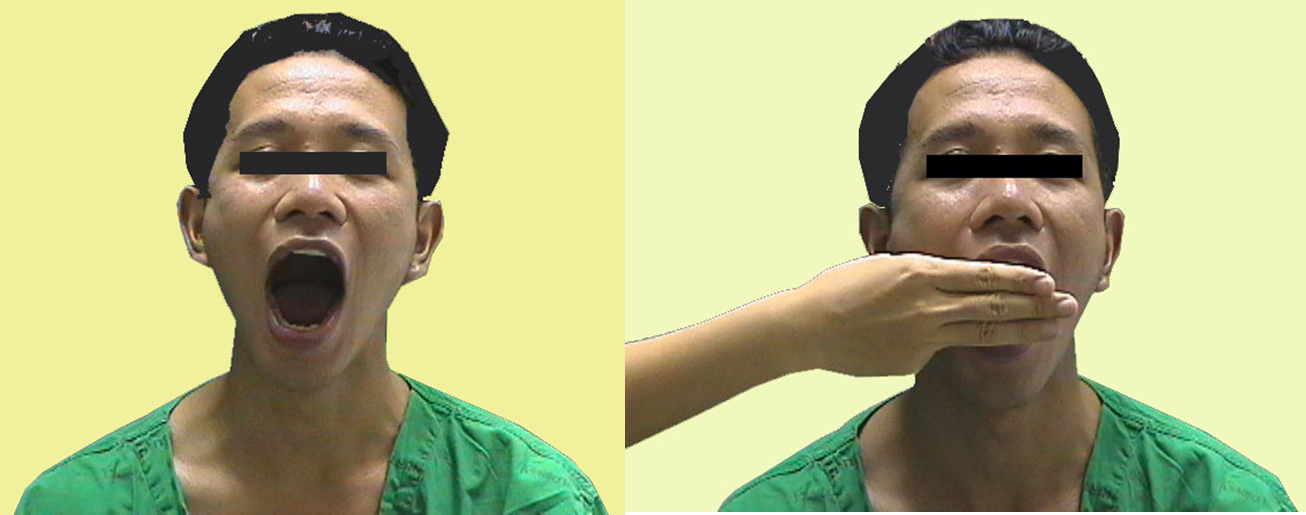
- Mallampati classification This test is performed with the patient in the sitting position, head in a neutral position, the mouth wide open and the tongue protruding to its maximum
- Class I: Visualization of the soft palate, uvula, anterior and the posterior pillars.
- Class II: Visualization of the soft palate and uvula.
- Class III: Visualization of soft palate and base of uvula.
- Class IV: Only hard palate is visible. Soft palate is not visible at all
Class III, IV difficult to intubate

- Interincisor gab: Normal >4.5 cm (3 fingers)
3) Thyromental distance (TMD) :
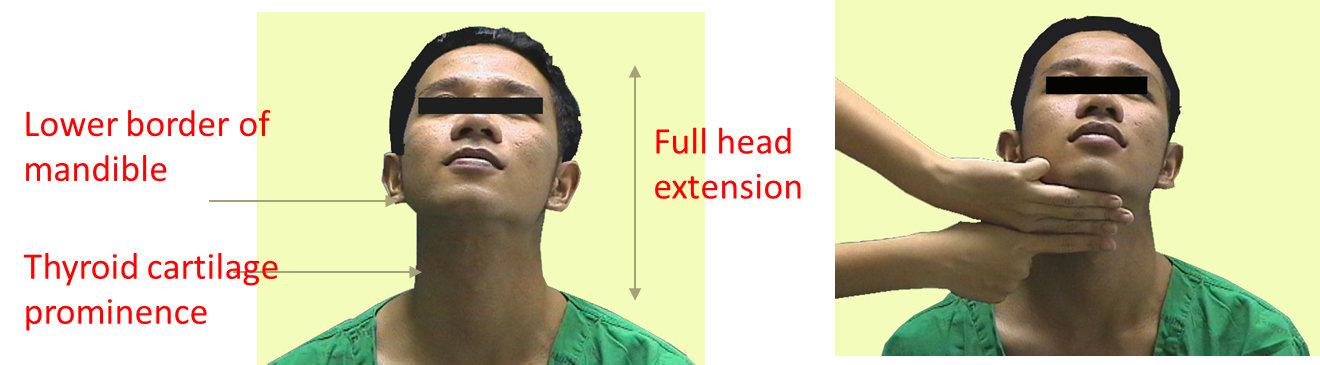
4) Flexion and extension of neck
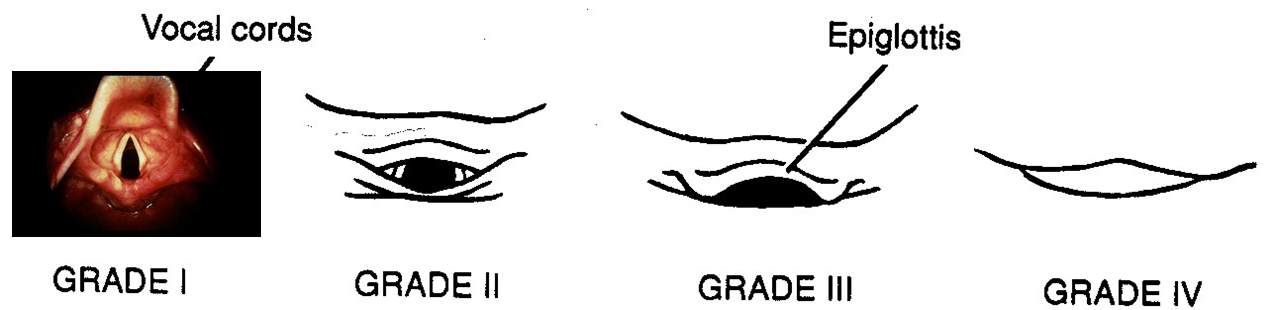
- Laryngoscopic view
6) Movement of temperomandibular joint (TMJ)

Preparing the procedure…
Essentials that must be present to ensure a safe intubation!.. They can be remembered by the mnemonic SALT
-
Suction. This is extremely important. Often patients will have secretions in the pharynx, making visualization of the vocal cords difficult.
-
Airway. the oral airway is a device that lifts the tongue off the posterior pharynx, often making it easier to mask ventilate a patient. Also a source of O2 with a delivery mechanism (ambu-bag and mask) must be available.
-
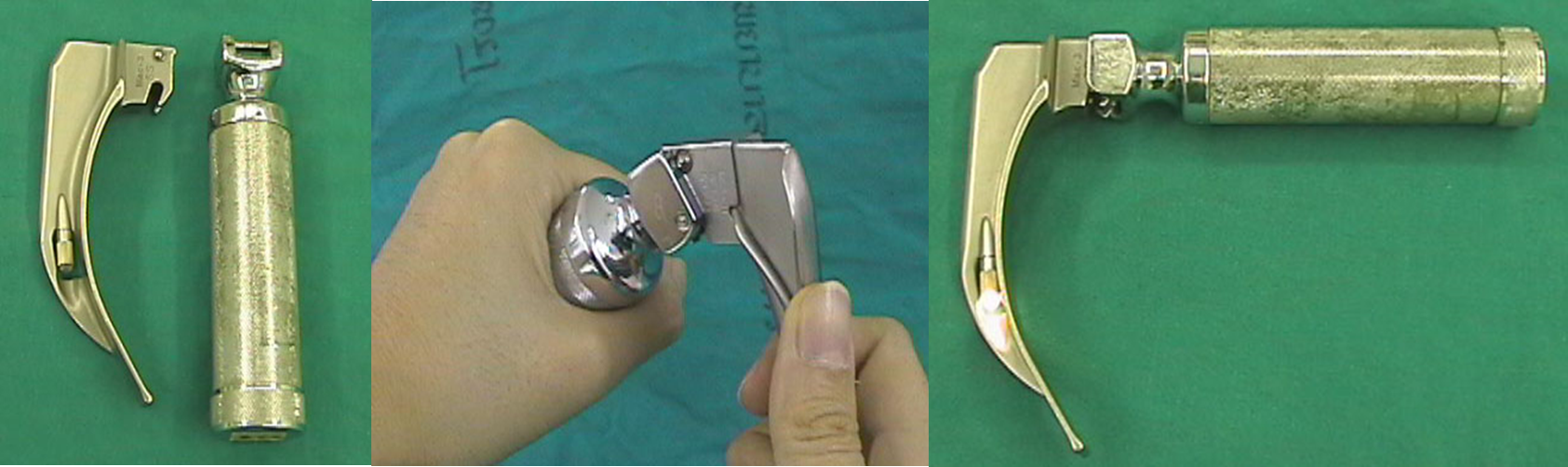
Laryngoscope. This is vital to placing an endotracheal tube.
-
Tube. Endotracheal tubes come in many sizes. In the average women adult, a size 7.0 or 8.0 endotracheal tube and 7.5 to 8.5 mm in men
Instruments used…
- Self-refilling bag-valve combination (eg, Ambu bag), tubing, and oxygen source.
- Plaster or tube holder .
- Introducer (stylets or Magill forceps).
- Laryngoscope
- Suction apparatus
- Syringe, 10-mL, to inflate the cuff.
- Mucosal anesthetics (eg, 2% lidocaine)
- Water-soluble sterile lubricant.
- Gloves.
- Pulse oximeter
- Stethoscope

Oropharyngeal or nasopharyngeal airway
Laryngoscope : handle and blade
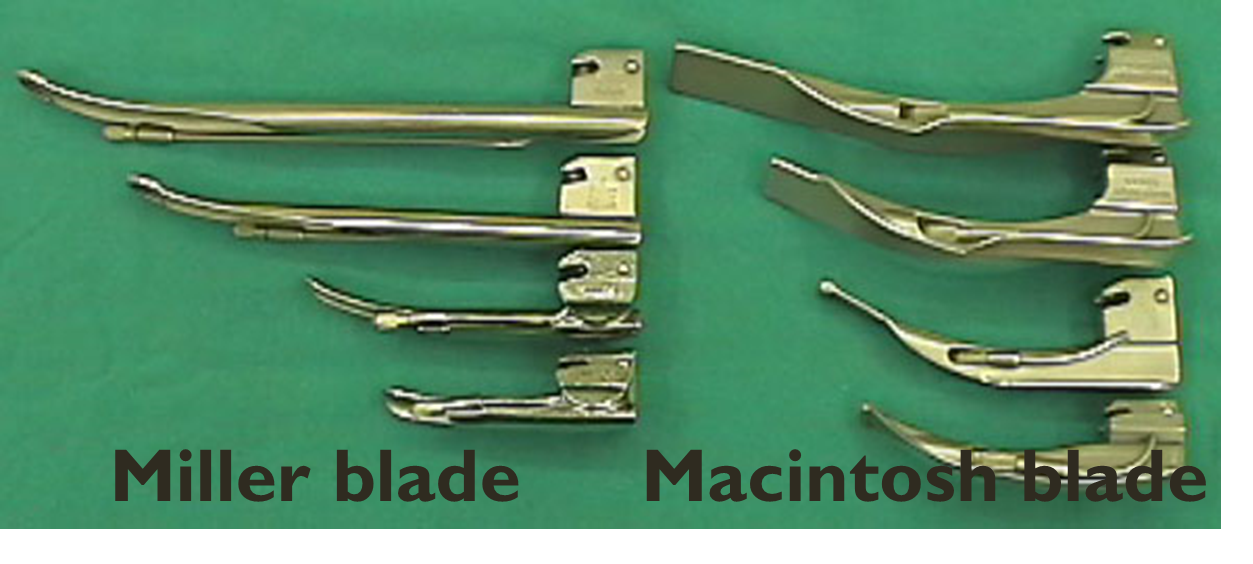
LARYNGOSCOPIC BLADE
- Macintosh (curved) and Miller (straight) blade
- Adult : Macintosh blade (No 3 and No 4),
- Children : Miller blade (No 2 and No 3)
Video Laryngoscopy (Glidescope)

2) Endotracheal tube
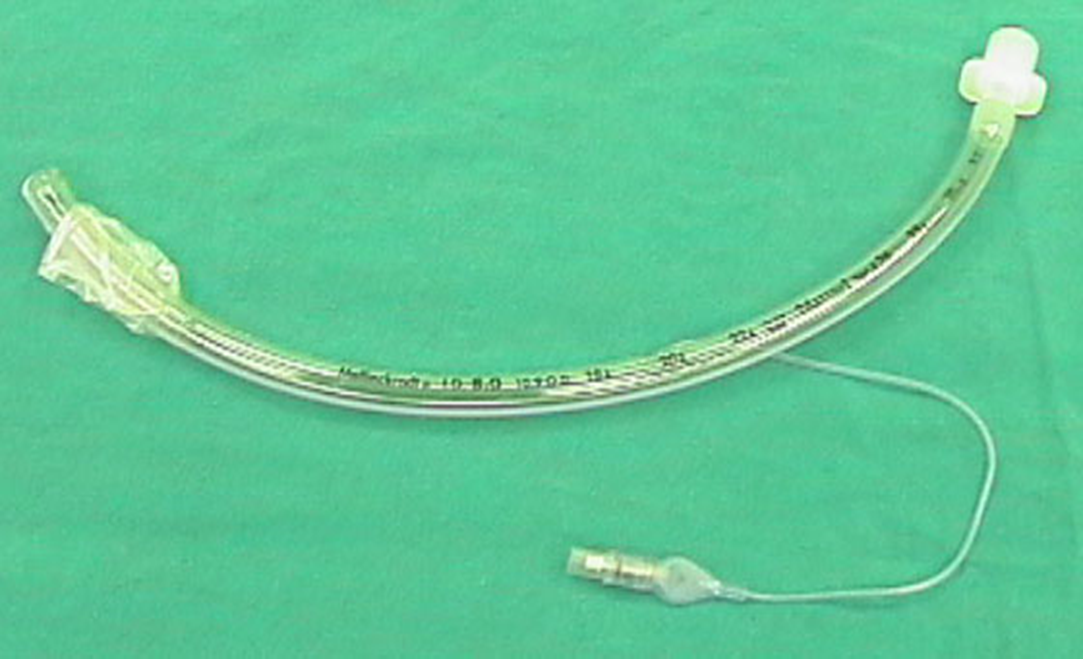
Depth of endotracheal tube :
Midtrachea or below vocal cord ~ 3-4 cms ,
- Adult: Male = 23 cms ,
- Female = 21 cms
- Children: endotracheal tube = (Age/2) + 12 (cm)
The goal is to place the tip of the ETT 2 to 4 cm from the carina (to avoid endobronchial intubation) and the proximal edge of the cuff at least 3 cm below the vocal cords (to avoid vocal cord damage and inadvertent extubaion).
Technique:
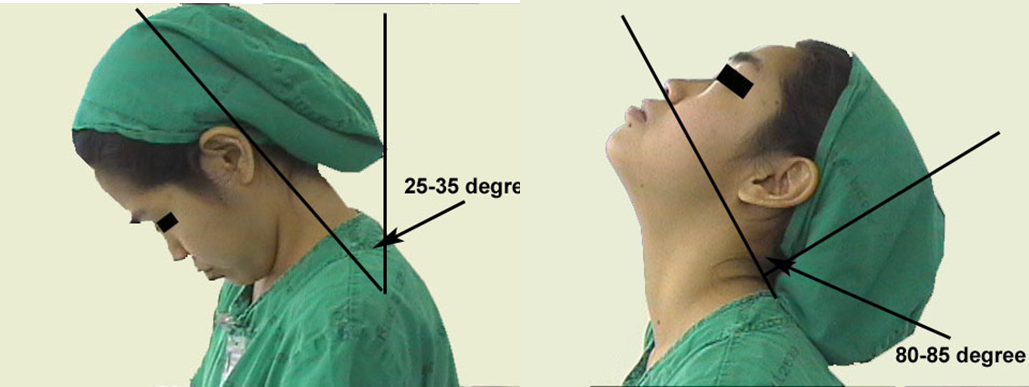
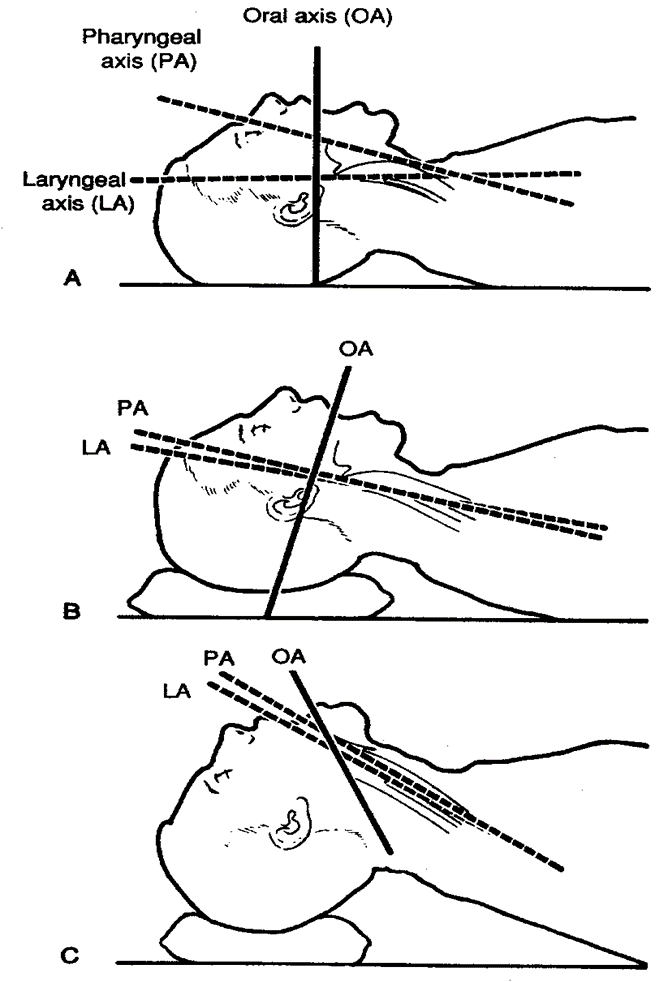
Sniffing position
- Flexion at lower cervical spine
- Extension at atlanto-occipital joint
- Make sure that all materials are assembled and close at hand
- Make sure that the balloon inflates
- Check the laryngoscope and blade for proper fit, and make sure that the light works
- Anesthetize the mucosa of the oropharynx, and upper airway with lidocaine 2%, if time permits and the patient is awake.
- Hyperventilate the patient with 100% oxygen for 1 minute prior to intubation attempt
- Place the patient in the sniffing position.
- Open the patient’s mouth with the right hand,.
- Grasp the laryngoscope in the left hand
- Spread the patient’s lips, and insert the blade between the teeth, being careful not to break a tooth.
- Pass the blade to the right of the tongue, and advance the blade into the hypopharynx, pushing the tongue to the left.
- Lift the laryngoscope upward and forward, without changing the angle of the blade, to expose the vocal cords.
- Take the endotracheal tube in the right hand and starts inserting it through the mouth opening.
- The tube is inserted through the cords to the point that the cuff rests just below the cords (between 21-23 mark on the tube)
- Holding the tube firmly in place, quickly remove the laryngoscope
- Remove the stylet from the endotracheal tube (if used)
- Finally, the cuff is inflated with 5-10 ml of air
- Ventilate the patient
- Observing the chest rise and fall with each ventilation
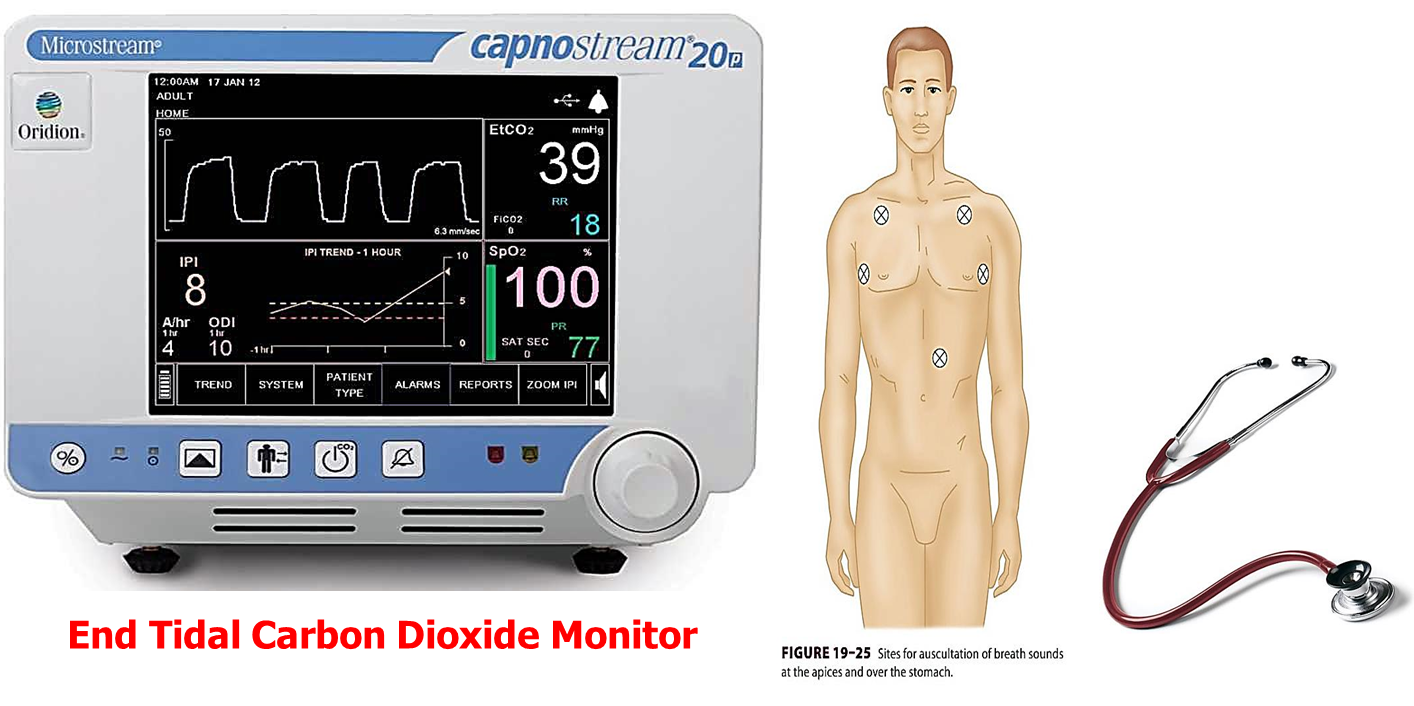
- Listens for breathing sounds to ensure correct placement of the tube (in stomach and chest)
- If no breath sounds and there is bubble sound in stomach (it is in stomach) remove the tube and ventilate the patient and start all over again
- If the tube is advanced too far, it will get into the right bronchus and only the right lung is ventilated. If this occurs deflate the cuff with draw 2-3 cm and re-inflate the cuff and listen again
- Attach the tube to the patient and to the ventilating apparatus

Confirmation of Tube Placement
-
Direct visualization of endotracheal tube
-
Auscultation: breath sounds audible over both lung fields
-
Condensation: consistently visible in the tube during exhalation
-
CO2 detection: gold standard of successful endotracheal intubation
-
Imaging CXR: The distal tip of the endotracheal or tracheal tube should be 2–6 cm above the carina Trained practitioners only: Ultrasound may be used to confirm tube position.

CC
1- Flex head slightly
2- mandible pitch forward and downward
3- Measure Oropharyngeal from mandible for correct size and insert
4- nasopharyngeal airway measure to ear and exclude polyps
5- use ampu bag, ensure correct placement with 1c, 5 second interval, press on margins with both hands
Snap macintosh, Check light potency testing with your hand
endotracheal size 8 male, 7 female
size of macintosh 4 for adults
must be on edge of bed
Prepare
- must be on edge of bed
- height of bed reach to thoracic
- Macintosh held at left hand always
- Ensure height of tube from incisor of teeth to ear? (21 female, male) - should reach t4 best
- go in center, follow with curve of tongue, reaching vericula?? pull (not with wrist. pull up with shoulder), then you’ll see vocal cord
- Gel with sylet and tube - apply stylet to eye merphis
- after insertion ensure securement
Confirmation
straight, remove tongue, go to the end to the esophagus, then pull up, pull up, pull up from shoulder to enter below epiglottis, when you see vocal cord insert
AMA - non definitive airway, may case aspiration
Large laryngeal mask airway used for diffucult airway.
suck air to become spoon shaped - then put index on front, push tongue away, place gel at posterior of AMA not anterior, push the tongue, index pin point. - it has to be center with good entry. - if you are in, push your index finger all way down until there’s resistance, then inflate the balooon. - comes up and seals airway, then use ampu bag for 25 minutes