Uterine Contractions
Uterine contractions are quantified as the number of contractions present in a 10-minute window, averaged over a 30-minute period
Normal: five contractions or less in 10 minutes, averaged over a 30-minute window Tachysystole: more than five contractions in 10 minutes, averaged over a 30-minute window

Tachysystole

Electronic Fetal Monitoring Definitions
Baseline
Normal FHR baseline: 110–160 beats per minute Z
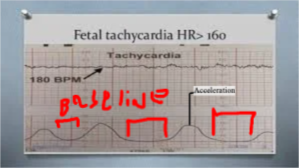
- Tachycardia: FHR baseline is greater than 160 beats per minute for >10 min
- Bradycardia: FHR baseline is less than 110 beats per minute for >10 minute
Fetal Tachycardia HR> 160
Bradycardia

Baseline Bradycardia
| Birthing-Person Causes | Fetal Causes |
|---|---|
| Supine positioning | Prolonged cord occlusion/cord prolapse |
| Hypotension | Fetal hypoxia |
| Connective tissue disease (eg, lupus) | Cardiac conduction or anatomic defects |
| Hypothermia | Post dates >42 0/7 weeks |
| Hypoglycemia | |
| Excessive vagal stimulation (eg, pushing in second stage) | |
| Tachysystole > SC |
Baseline Tachycardia
- Baseline >160 bpm for >10 minutes
| Birthing-Person Causes | Fetal Causes |
|---|---|
| Fever/infection/chorioamnionitis | Anemia |
| Dehydration | Fetal cardiac abnormalities |
| Hyperthyroidism | Tachyarrhythmias (supraventricular tachycardia) |
| Anemia | Chronic fetal hypoxia |
| Birthing person anxiety | Severe prematurity |
| Cocaine, amphetamines | Prolonged fetal activity |
| Parasympatholytic or beta-sympathomimetic drugs (terbutaline) | Vibroacoustic stimulation |
Causes of Decreased Variability Z
| Birthing-Person Causes | Fetal Causes |
|---|---|
| Fever | Fetal sleep cycles (20- to 40-minute duration) ⇒ scalp scrap then baby will awake if more than 50 min is pathology |
| Central nervous system (CNS) depressants (ie, opioids, benzodiazepines, magnesium sulfate) | Prematurity |
| General anesthesia | Cardiac anomalies |
| Alcohol | Fetal tachycardia |
| Corticosteroids | Hypoxia/acidosis |
| Anticholinergics/parasympatholycis | CNS anomalies |
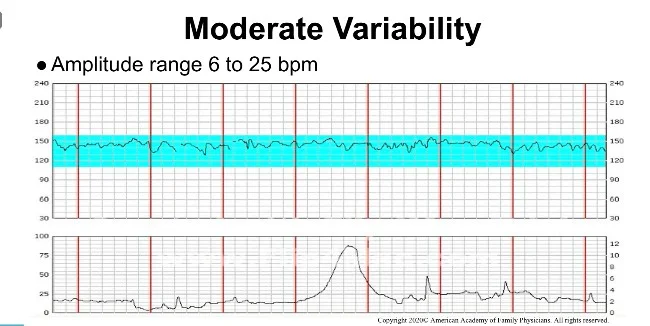
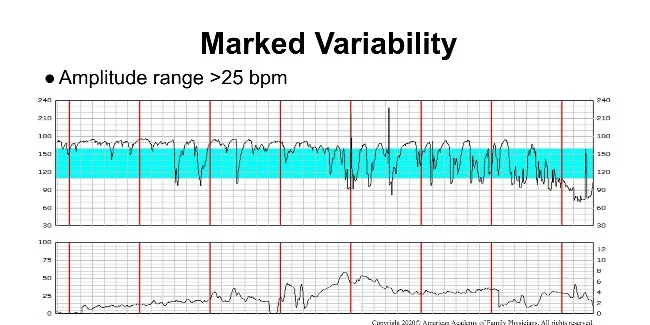
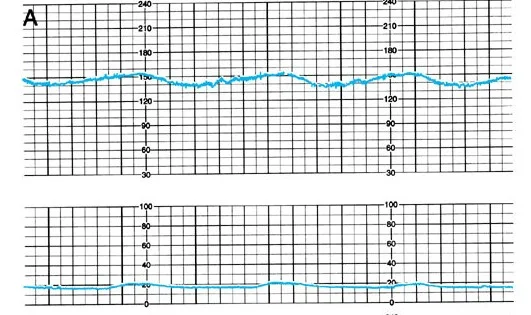
Baseline Variability
Minor Fluctuations in the baseline FHR that are irregular in amplitude and frequency
It is assessed by estimating the difference in bpm between the highest peak and lowest trough of fluctuation in one minute segment of trace
- Moderate variability amplitude range 5–25 beats per minute
- Minimal variability less than 5bpm
- Marked variability more than 25bpm
- Absent
Moderate Variability
- Amplitude range 6 to 25 bpm
Marked Variability
- Amplitude range >25 bpm
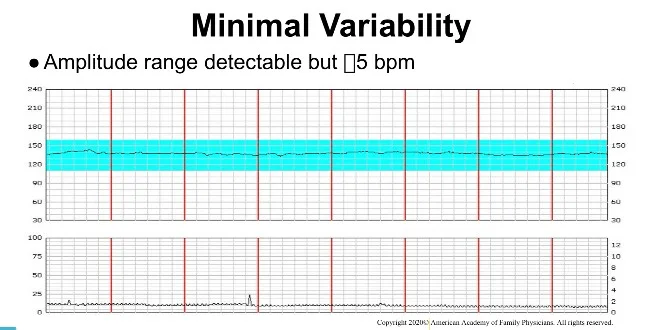
Minimal Variability
- Amplitude range detectable but ≤5 bpm
Acceleration Z
Abrupt increase in the FHR
At 32 weeks of gestation and beyond, an acceleration has a peak of 15 beats per minute or more above baseline, with a duration of 15 seconds or more
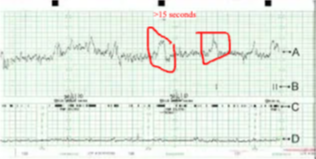
if no acceleration = non reactive but normal
Non-Reactive NST
Decelerations
Transient slowing of FHR below the baseline level of more than 15 bpm and lasting for 15 sec or more
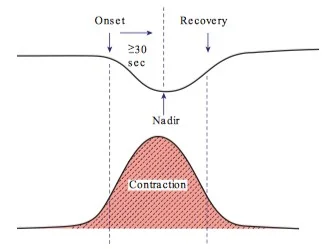
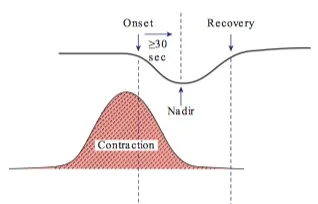
Early Deceleration (Head Compression) - during labor
- Visually apparent usually symmetrical
- Gradual decrease and return of the FHR associated with a uterine contraction
- A gradual FHR decrease is defined as from the onset to the FHR nadir of 30 seconds or more
Late Deceleration
Visually apparent usually symmetrical gradual decrease with return to baseline Onset to nadir >30 second The onset, nadir, and recovery of the deceleration occur after the beginning, peak, and ending of the contraction, respectively - starts after ending of contraction
- Due to uteroplacental insufficiency
- Common in patients with PIH, DM, IUGR or other form of placental insufficiency
- Reduces Baseline variability together with Late Decelerations or Variable Decelerations is associated with increased risk of CP
Variable Deceleration
May happen with or after contraction
- Vary in duration, intensity and relation to uterine contractions
- Visually apparent abrupt decrease in FHR
- Onset to nadir <30 second
- Decrease in FHR is 15 bpm or more lasting for 15 second but less than 2 minute
- Caused by cord compression
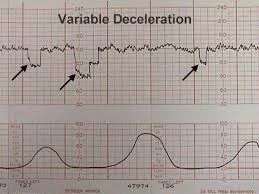
W shape is variable # if no contraction its variable
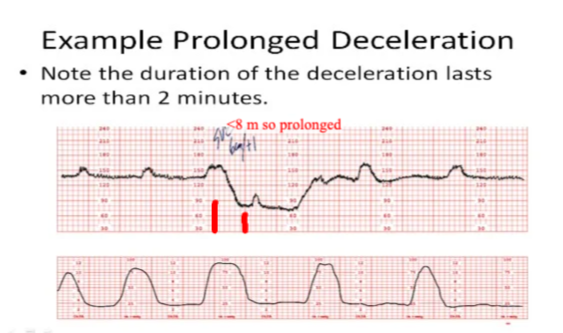
Prolonged Deceleration
Any deceleration 15 bpm or more below the baseline that lasts 2 minute or more but less than 10 minute - if more bradycardia
Sinusoidal Pattern
Visually apparent, smooth, wave-like above and below FHR baseline with a cycle frequency of 3–5 per minute when persists for 20 minutes or more. (Role out narcotic induced)
Causes: fetal anaemia (Rh isoimmunisation, fetal haemorrhage)
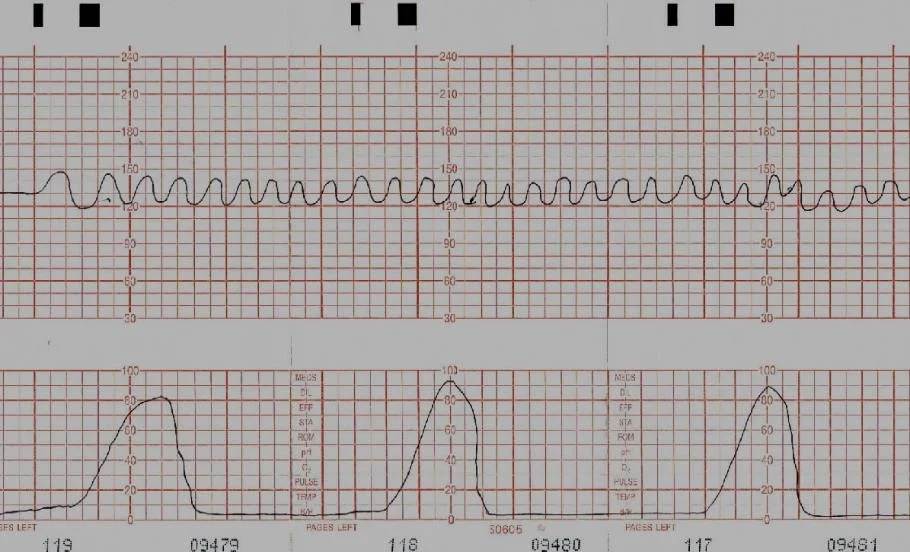
Fetal Heart Rate Monitoring Strip