Rhogam Dosing (Anti-D)
,### Prevention of Isoimmunization
- Estimation of maternal fetal blood can be done using the Kleihauer-Betke test.
- The standard dose of anti-D is 0.3 mg Z, which will eradicate 15 ml of fetal red blood cells (RBC) or 30 mls of fetal whole blood. Z
- Schedule for injection:
| Trimester/Procedure | Dose |
|---|---|
| Antepartum bleeding 1st trimester | 50 μg RhIgG |
| Antepartum bleeding 2nd & 3rd | 300 μg RhIgG |
| Prophylaxis GA 28-32 weeks | 300 μg RhIgG |
| Delivery | <72 hr - 300 μg RhIgG |
7M & 78h from birth doses
Kleihauer-Betke Test
Detection of Fetomaternal Hemorrhage
-
Used for detecting Fetomaternal or Transplacental Hemorrhage.
-
The test is dependent on the fact that adult hemoglobin is more readily eluted through the cell membrane in the presence of acid than is fetal hemoglobin (HbF).
Procedure
-
The maternal blood is fixed on a slide with ethanol (80%) and treated with a citrate phosphate buffer to remove the adult hemoglobin.
-
After staining with hematoxylin and eosin, the fetal cells can readily be distinguished from the empty maternal cells.
The green marks are pointing to fetal HGB.

Screening for Rh Isoimmunization
Initial Steps
-
Identify mother’s blood group in the first ANC visit.
-
If Rh-negative patients → check father → If Rh neg, the fetus will be Rh neg → safe.
-
If the father is Rh positive, his Rh genotype and ABO status should be determined.
-
If the father is:
- Homozygous for the D antigen → every fetus will be Rh positive.
- Heterozygous → only half of his children will be positive.
Follow-Up for Rh-Negative Pregnancies
Monitoring and Testing
-
If it is not possible to test the antigen status and zygosity of the father, it must be assumed that he is antigen positive.
-
MATERNAL Rh-ANTIBODY TITER Anti-D antibody titers.
-
Serial Ab titer gives + serial USS and + past ob Hx → guides management.
Follow-Up Methods
Cut‑off titer level: < 1:16 Z
- If the titer is < 1:16, repeat the test every 2–4 weeks. - insignificant
- When the titer rises to ≥ 1:16, a detailed assessment is warranted. - significant - maternal RH testing if exceeds - if parental negative ⇒ routine, positive ⇒ Amniocentesis for RHD antigen
Factors influencing the timing and method of invasive testing
- Current clinical status of the fetus
- Gestational age
- Patient’s obstetric history
Note (ACOG): the titer reflects how many times maternal blood can be diluted while still detecting anti‑D antibodies.
Clinical tip: Titers are generally not useful for monitoring a patient with a history of a previous fetus affected by hemolytic disease.
Non-Invasive and Invasive Techniques
Non-invasive Invasive
- Ultrasonography 1. Amniocentesis
- Doppler velocimetry of MCA 2. Fetal blood sampling
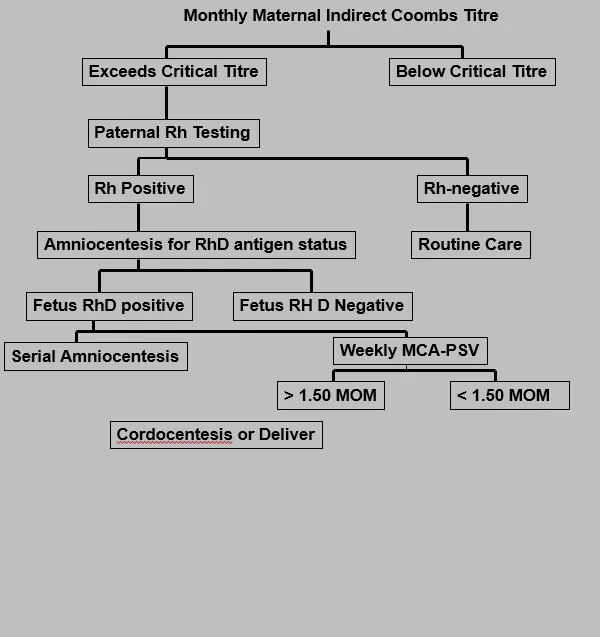
Monthly Maternal Indirect Coombs Titre
Management Based on Titre Levels
- Exceeds Critical Titre
- Paternal Rh Testing
- If Rh Positive
- Amniocentesis for RhD antigen status
- Fetus RhD positive
- Serial Amniocentesis
- Fetus RH D Negative
- Weekly MCA-PSV
-
1.50 MOM
- < 1.50 MOM - Cordocentesis or Deliver
-
- Weekly MCA-PSV
- Fetus RhD positive
- Amniocentesis for RhD antigen status
- If Rh-negative
- Routine Care
- If Rh Positive
- Paternal Rh Testing
- Below Critical Titre
- repeat 2-4 wks
Ultrasonography
Role in Monitoring Fetal Condition
-
To Establish The Correct Gestational Age.
-
In Guiding Invasive Procedures And Monitoring Fetal Growth And Well-being.
-
Ultrasonographic Parameters To determine Fetal Anemia: * Placental Thickness. * Umbilical Vein Diameter (increased). * Hepatic Size. * Splenic Size. * Polyhydramnios. * Fetal Hydrops (e.g., Ascites, Pleural Effusions, Skin Edema). * Blood velocity (increased).

Doppler Velocimetry of Middle Cerebral Artery (MCA)
Predicting Fetal Anemia
-
Anemic fetus preserves oxygen delivery to the brain by increasing cerebral flow (sparing effect).
-
For predicting fetal anemia.
-
Predict the timing of intrauterine fetal transfusion.
Invasive Techniques for Diagnosis
Indications and Procedures
-
Critical anti-D titer: A titer associated with a significant risk for fetal hydrops (Anti-d titer value between 8 and 32).
-
Previous seriously affected fetus or infant.
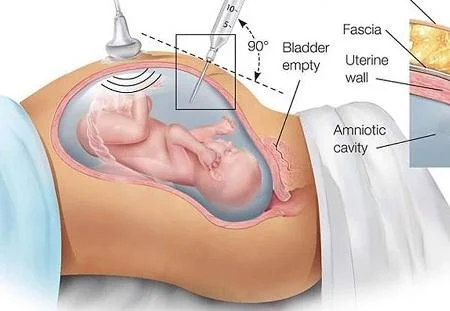
Amniocentesis
Procedure and Interpretation
- Bilirubin in amniotic fluid decreases with advanced gestation.
- It derives from fetal pulmonary and tracheal effluents.
- Its level rises in correlation with fetal hemolysis.
Determination of Amniotic Fluid Bilirubin
- By the analysis of the change in optical density of amniotic fluid at 450 nm on the spectral absorption curve (delta od450).
- Procedures are undertaken at 10–15 days intervals until delivery data are plotted on a normative curve based upon gestational age.
Amniocentesis Procedure
Key Elements
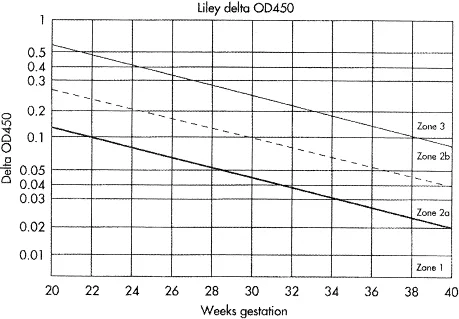
Queenan Curve for Delta-OD 450 Values
Assessing Risk of Intrauterine Death
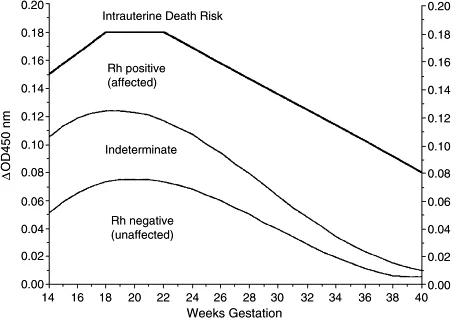
Interpretation Of Amniotic Fluid Bilirubin
Clinical Implications
-
A falling curve: is reassuring (An unaffected or Rh D-negative fetus).
-
A plateauing or rising curve: suggests active hemolysis (require close monitoring & may require fetal blood sampling &/or early delivery).
-
A curve that reaches to or beyond the 80th percentile of zone II on the Liley graph or enters the “intrauterine transfusion” zone of the Queenan curve necessitates investigation by fetal blood sampling.
Fetal Blood Sampling
Gold Standard for Detection of Fetal Anemia
-
Is the gold standard for detection of fetal anemia.
-
Reserved for cases with:
- With an increased MCA-PSV.
- Increased ∆OD 450.
-
Complications:
- Total Risk of Fetal Loss Rate 2.7%.
- Bleeding from the puncture site in 23% to 53% of cases.
- Bradycardia in 3.1% to 12%.
- Fetal-maternal hemorrhage: occur in 65.5% if the placenta is anterior and 16.6% if the placenta is posterior.
- Infection and abruptio placenta (rare).