Introduction
Definition and Cause
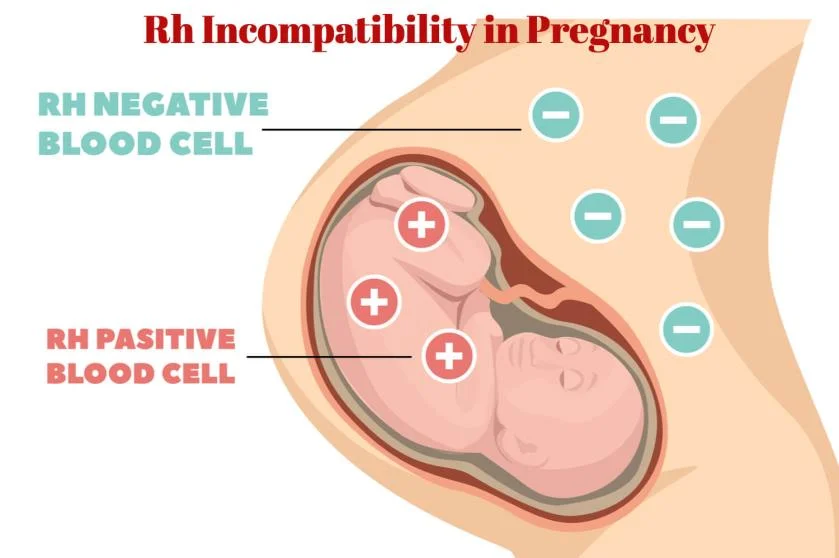
- Rhesus (Rh) isoimmunization is an immunologic disorder that occurs in a pregnant, Rh-negative patient carrying an Rh-positive fetus.
- The immunologic system is stimulated to produce antibodies to the Rh antigen, which then cross the placenta and destroy fetal red blood cells.
Pathophysiology
Rh Complex and Isoimmunization
- The Rh complex is made up of a number of antigens, including C, D, E, c, e, and other variants.
- More than 90% of cases of Rh isoimmunization are due to antibodies to D antigens.
- Rh negative: RBCs lack D antigen on the surface; an individual with Rh negative has no D antigen.
- Rh positive: RBCs surface has D antigen.
- When Rh-negative patients are exposed to the Rh antigen, they may become sensitized.
Mechanism of Sensitization
Theories and Process
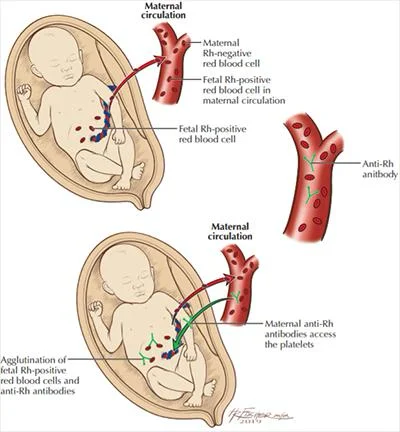
- Two mechanisms theories are proposed for sensitization:
- Undetected placental leak of fetal red blood cells into the maternal circulation during pregnancy. (most likely)
- Rh-negative woman may have been sensitized from birth by receiving enough Rh-positive cells from her mother.
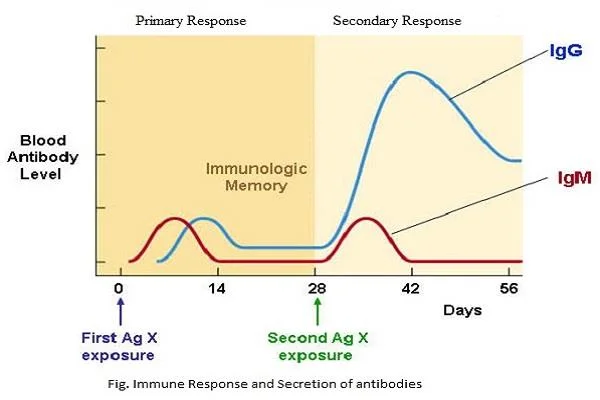
Two exposures to the Rh antigen are required to produce any significant sensitization, unless the first exposure is massive.
- 1st exposure → primary sensitization
- 2nd Exposure → Anamnestic response leading to the rapid production of immunoglobulins.
Types of Immunoglobulins
Response to Rh Antigen
-
The initial response to exposure to Rh antigen is the production of immunoglobulin M (IgM) antibodies for a short period.
-
Followed by the production of IgG antibodies that are capable of crossing the placenta and lasts for a lifetime.
The Effect on Fetus
Hemolysis and Its Consequences
- Antibodies will coat the fetal red blood cells and cause Hemolysis.
- →Mild: fetus can compensate by increasing erythropoiesis.
- →Severe: profound anemia, resulting in hydrops fetalis
What are the products resulting from hemolysis?
Note: High bilirubin levels can damage the central nervous system and lead to neonatal kernicterus.
Development of Rh System in Fetus
Timing and Implications
-
Establishment of the fetal circulation occurs at 4 weeks.
-
The presence of the Rh D antigen has been demonstrated as early as 38 days after conception.
-
The risk is low in the first 8 weeks, but it rises significantly by 12 weeks.
Risk Factors for Isoimmunization
Events Leading to Sensitization
-
Immunizations occur at the time of: A. 1st Trimester: Abortions, Ectopic (less likely at GA of 8 weeks)
B. 2nd half of pregnancy: transplacental hemorrhage (e.g., second-third trimester vaginal bleeding, invasive procedures, abdominal trauma, or after external cephalic version)
C. Peripartum: Delivery, cesarean, manual removal of placenta.
Incidence of Sensitization
Risk Based on Pregnancy Conditions
- The overall risk of immunization for the second full-term Rh-positive fetus in:
- ABO-compatible pregnancy → 1 in 6 pregnancies (16.5%)
- ABO-incompatible → 2%
| Previous Encounter | Risk Incidence for Immunization |
|---|---|
| Spontaneous Abortion | 3.5% |
| Induced Abortion | 5.5% |
| Ectopic | 1% |
The protection is due to the destruction of the ABO-incompatible cells in the maternal circulation and the removal of the red blood cells by the liver.
Natural History of RH Isoimmunization and Hemolytic Disease
Outcomes Without Treatment
-
Less than 20% of Rh D incompatible pregnancies actually lead to maternal isoimmunization.
-
25-30% of the offspring will have some degree of hemolytic anemia and hyperbilirubinemia.
-
20-25% will be hydropic and die either in utero or in the neonatal period.
-
Cases of hemolysis in the newborn that do not result in fetal hydrops still can lead to kernicterus.