CHRONIC SPECIFIC INFECTION
Chronic from the start Caused by specific bacteria i.e. TB or Brucella. Affects any age More common in the immunocompromised (AIDS, chronic renal failure, substance abuser)
Musculoskeletal Tuberculosis
Epidemiology
- Caused by Mycobacterium tuberculosis
- Vertebral body
- Large joints
- Multiple lesions in 1/3 of patient
Common Sites
Targets:
- Spine (50%)
- Thoracic (50%)
- Lumbar (25%)
- Cervical (25%)
- Pelvis
- Hip
- Knee
- Ankle and shoulder
Presentation
Symptoms and Signs
History
- Constitutional symptoms:
- Fever
- Weight loss
- Night sweats
- Anorexia
- Pain
- Stiffness
- Deformity
Physical Examination
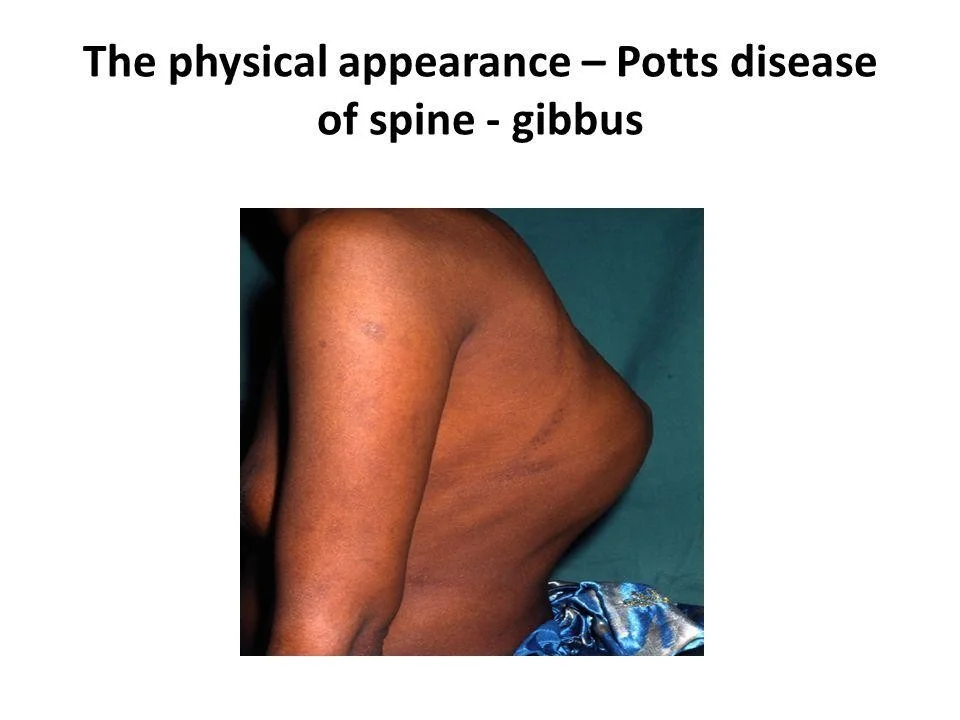
Spine:
- Deformity (gibbus, kyphosis)
- Muscle spasm
- Neurological compromise (motor > sensory)
Joints:
- Swelling
- Stiffness
- Loss of function
Diagnosis
Diagnostic Approaches
Blood Work
- Lymphocytosis
- Anemia
- Elevated ESR
- PCR
- Brucella titer

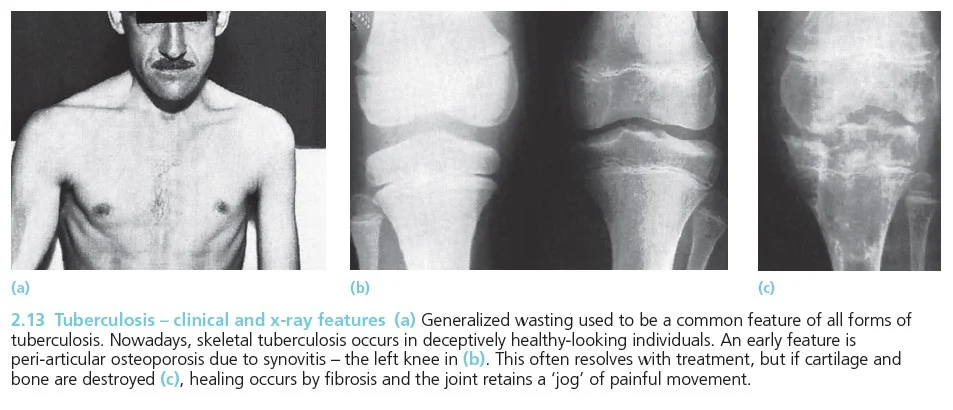
Plain X-rays
- Joints: usually monoarticular
- Peri-articular osteopenia
- Subchondral and peripheral erosions affecting both sides of the joint
- Loss of joint space

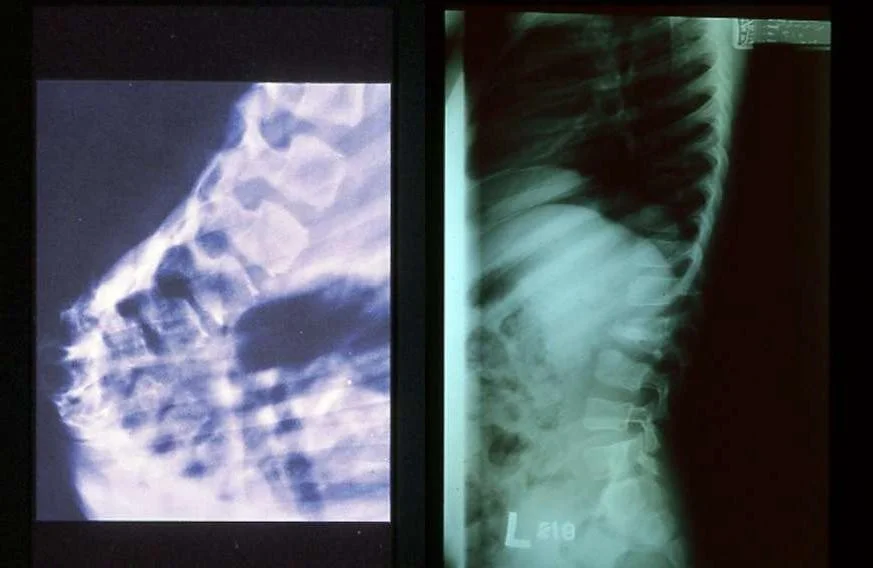
Radiology in Spinal TB (Pott’s Disease)
Characteristics
Spinal T.B (Pott’s Disease):
-
Secondary to hematogenous spread
-
Affect two or more adjacent vertebrae
-
Skip levels
-
Primarily does not affect the disc but eventually the disc is affected
-
Affects most commonly the anterior part of the vertebral endplates
-
Causing erosion and destruction and finally anterior wedging of the vertebrae
-
Infection spreads to adjacent level under the longitudinal ligaments and hematologically
-
The disc herniates into the weakened and destructed body and narrowing of the disc height follows
-
Eventually a kyphotic deformity occurs
-
Para vertebral abscess is common and may be distant as well
- Cervical > retropharyngeal abscess
- Lumbar > psoas abscess
-
Compression of the spinal cord is more likely to occur at the thoracic level
-
Neurological deficits occur due to the compression secondary to the deformity or compression from the abscess
-
Paraplegia may occur
- Reversible if treated early
- Mostly treated non-surgically


 psoas abcess
psoas abcess



Computerized Tomography:
- Further delineate bony destruction and sequestrum Magnetic Resonance Imaging with Contrast:
- Soft tissue mass, abscess
- Nerve root, cord status
- Distant abscess
- Non-enhanced cold abscess with enhanced peripheral ring




Special Tests
- Mantoux skin test
Biopsy/Aspiration
Spine:
- CT guided needle biopsy
Joints:
- Synovial aspiration
- Should get bone/soft tissue
- Send for aerobic/non-aerobic bacteria, fungal, AFB, enriched culture media
- Takes up to 4-6 weeks
Treatment of Musculoskeletal Tuberculosis
Medical and Surgical Approaches
Medical Treatment
- Mainstay of treatment is combination anti-microbial agents
- Usually 3-4 medications needed: Isoniazid, Rifampin, Ethambutol, Pyrazinamide are commonly chosen
- Modify according to culture results
- Given for prolonged period of time (6 months up-to 18 months)
Surgical Indications
- Tissue biopsy to confirm diagnosis
- Abscess drainage if resistant to conservative treatment
- Joint lavage and removal of foreign bodies
- Marked and progressive neurological deficit not responding to medical treatment requiring decompression
- Spinal instability requiring stabilization