SEPTIC ARTHRITIS
Introduction
Overview
- May affect any age and any joint
Pediatric:
- Younger than 2 years of age
- Hip joint
- Risk factors: Prematurity, Cesarean section
Adult:
-
80 years
- Knee joint
- Risk factors: Diabetes, Rheumatoid arthritis, Cirrhosis, HIV, History of crystal arthropathy, Endocarditis or recent bacteremia, IV drug user, Recent joint surgery
Pathophysiology
Mechanisms
- Hematogenous route
- Dissemination from osteomyelitis
- Spread from an adjacent soft tissue infection
- Diagnostic or therapeutic measures
- Penetrating damage by puncture or cutting
- Direct inoculation from trauma or surgery
- Contiguous spread from adjacent osteomyelitis
- In joints where metaphysis is intracapsular (Hip, shoulder, Elbow and Ankle)
Consequences
- Acute synovitis with purulent joint effusion
- Articular cartilage attacked by bacterial toxin and cellular enzymes
- Cartilage injury occur by 8 hours
- Nutritious synovial fluid replaced by pus
- Complete destruction of the articular cartilage
- With healing: Adhesions, fibrosis, and bony ankylosis


Microbiology
Common Pathogens
- Most common pathogen is staphylococcus aureus (accounts for >50% of cases)

Clinical Presentation
Symptoms by Age
Neonate
- May not show fever
- Irritability, refuses to feed
- Rapid pulse
- Pseudo-paralysis
- Locally: warmth, tenderness, resistance to movement
Children
- Acute pain in single large joint (Hip joint most affected)
- Looking ill, in pain with high grade fever
- Joint held in resting position
- In superficial joints: Redness, hotness, tenderness, Swelling, effusion and fluctuation
- Extremely painful to move joint (does not allow passive movement)
- Vaccination history must be obtained
Adult
- Often superficial joints: Knee (most common), ankle, wrist
- Clinical picture: similar to children




Radiology
Diagnostic Tools
X-ray
- AP and frog-leg lateral pelvic x-rays Findings:
- May be normal, especially in early stages of disease
- Early: Widening of the joint space, subluxation, or dislocation
- In infants → lateral subluxation of the proximal femur
- Later: narrowed joint space
- May see bone involvement with associated osteomyelitis

Ultrasound
- May be helpful to identify effusion
- Used to guide aspiration
MRI
- Difficult to obtain emergently
- Identifies a joint effusion and adjacent osseous involvement
Laboratory Tests
Diagnostic Parameters
- WBC, Differential (neutrophils)
- ESR, CRP
- Blood culture: positive in 50% of proven cases
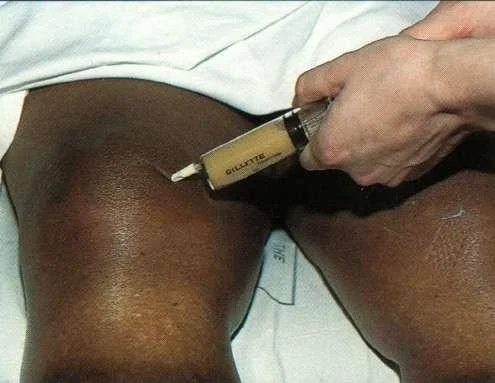
Joint Aspiration
Diagnostic - Indicated whenever there is high suspicion
Joint fluid studies should include:
- Cell count with differential
- Gram stain, Culture, and sensitivities
- Glucose and protein levels
- Crystal analysis
- Alpha defensin
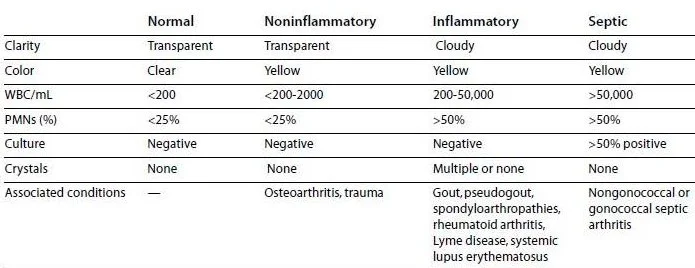
| Normal | Noninflammatory | Inflammatory | Septic | |
|---|---|---|---|---|
| Clarity | Transparent | Transparent | Cloudy | Cloudy |
| Color | Clear | Yellow | Yellow | Yellow |
| WBC/mL | <200 | <200-2000 | 200-50,000 | >50,000 |
| PMNs (%) | <25% | <25% | >50% | >50% |
| Culture | Negative | Negative | Negative | >50% positive |
| Crystals | None | None | Multiple or none | None |
| Associated conditions | — | Osteoarthritis, trauma | Gout, pseudogout, spondyloarthropathies, rheumatoid arthritis, Lyme disease, systemic lupus erythematosus | Nongonococcal or gonococcal septic arthritis |

Differential Diagnosis
- Transient synovitis
- Acute osteomyelitis: nearby metaphysis
- Trauma: acute hemarthrosis
- Hemophilia: hemarthrosis
- Rheumatic fever
- Gouty arthritis - adults
Transient Synovitis
Characteristics
- Benign Hip pain due to inflammation of the synovium of the hip
- Aged 4-8 years old & male-to-female ratio is 2:1
- Risk factors: Trauma, Bacterial or viral infection (poststreptococcal toxic synovitis), Allergic reaction
- Natural history of disease: Improvements in 24-48 hours; Complete resolution of symptoms will usually occur in <1 week
Treatment
- Self-limited after 2-7 days
- Bed rest
- Non-steroidal Anti-Inflammatory Drugs (NSAIDS):
- Ibuprofen: 2 days
- 80% of all patients has resolution by 7 days
Septic Arthritis vs Transient Synovitis
Comparison
| Transient Synovitis | Septic Arthritis | Category |
|---|---|---|
| < 38.5 | > 38.5 | Fever |
| Yes | No | Weight bearing |
| < 12,000 | > 12,000 | WBC |
| < 2 | > 2 | ESR |
Kocher Criteria for Septic Arthritis
(3 out of 4 = 93% chance of septic arthritis)
-
Temperature > 101.3° (38.5° c) is the best predictor of septic arthritis followed by CRP of >2.0 (mg/dl)
-
When in doubt: Aspiration of joint
- If turbulent, or pus: open drainage
- If clear: conservative
Treatment of Septic Arthritis
Emergency Measures
Septic Arthritis is One of Orthopedic Emergencies:
- Admission, General supportive measures, splint (NPO & IVF)
- Joint Aspiration
- Emergency arthrotomy and washout, broad spectrum IV antibiotics and splintage
- Initiate empiric therapy based on patient age and or risk factors
- Transition to organism-specific antibiotic therapy based once obtain culture sensitivities
- Treatment can be monitored by following serum WBC, ESR, and CRP levels during treatment
lyme disesase could be enough in cases of septic arthritis
Antibiotic Therapy
- Be sure antibiotic treatment will not delay the surgery
- I.V. for 3 weeks, followed by oral for 2-3 weeks
- Flucloxacillin for Gram positive
- If in doubt: third generation cephalosporin (neonates)
Complications of Septic Arthritis
Potential Outcomes
- Dislocation: by tense effusion and over-stretching of capsule
- Epiphyseal destruction: In neonates → Unstable pseudoarthrosis
- Osteoarthrosis: In partial cartilage destruction
- Ankylosis: In massive cartilage destruction
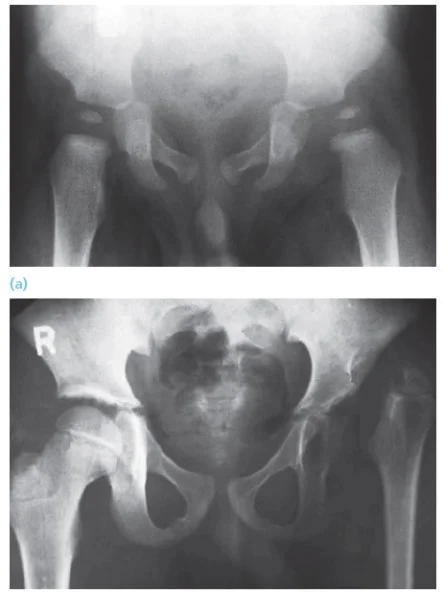

Case: septic arthritis, hip 14y old boy Presented with pain in R hip after history of a fall with abrasions few days before Had fever, limitation of R hip motion WBC: 13,000, ESR 23mm/1 hour Initial x-ray: not significant
Initial x-ray

X-ray 8 days later

X-ray taken on follow-up after surgical irrigation and debridement – too late!
