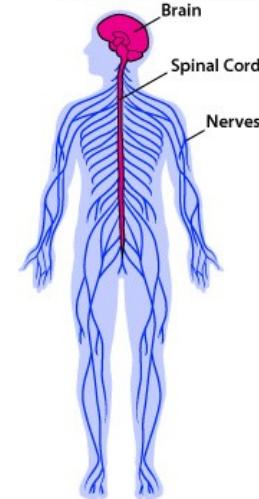
Central Nervous System (CNS)
- Components: Brain & spinal cord
- Protection: Protected by bones and blood-brain barrier
Peripheral Nervous System (PNS)
- Components: Nerves & ganglia outside CNS
- Characteristics:
- Not protected by bones and blood-brain-barrier
- Exposed to toxins and mechanical injuries
- Capacity to regenerate - re-grow if cut (unlike CNS)
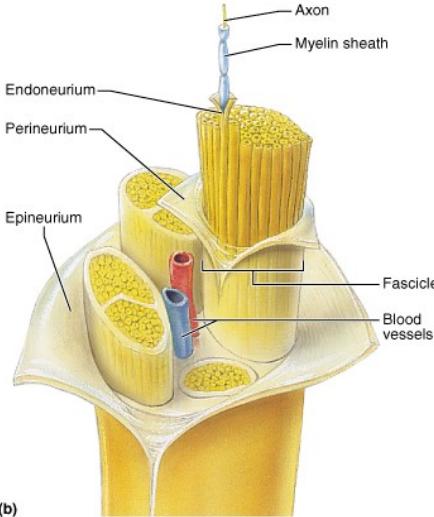
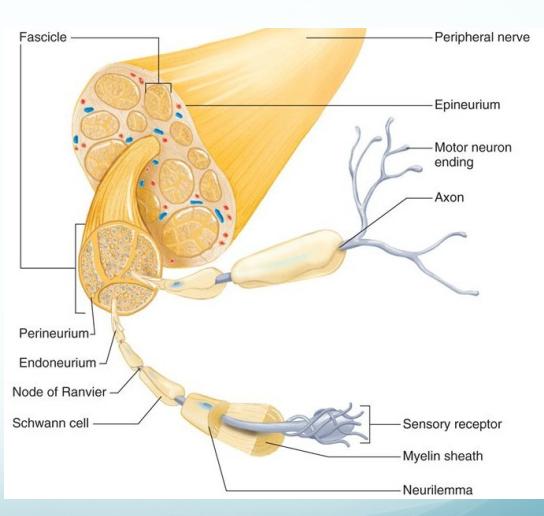
Nerve Structure
Connective Tissue Layers
- Epineurium: Outermost connective tissue layer
- Perineurium: Middle connective tissue layer surrounding fascicles
- Endoneurium: Innermost connective tissue layer surrounding individual nerve fibers
Copyright © 2001 Benjamin Cummings, an imprint of Addison Wesley Longman, Inc.
Nerve Fiber Components
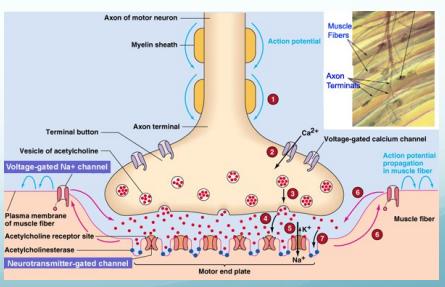
- Motor axons: Transmit motor signals
- Sensory axons: Transmit sensory signals
- Myelin coating:
- Lipoprotein layer produced by Schwann cells
- Facilitates rapid nerve conduction
Classification of Nerve Injuries
Types of Injury
- Neuropathies: Degenerative nerve disorders
- Ischemia: Reduced blood supply to nerve tissue
- Mechanical Injury:
- Compression: Prolonged pressure on nerve
- Traction: Stretching or pulling forces
- Laceration/Cut: Sharp or penetrating injuries
- Burn: Thermal or chemical damage
Extent of Damage
- Transient Injury:
- Recoverable loss of function
- Usually temporary conduction block
- Complete Injury:
- Irreversible structural damage
- Complete or permanent loss of function
Pathophysiology of Nerve Injury
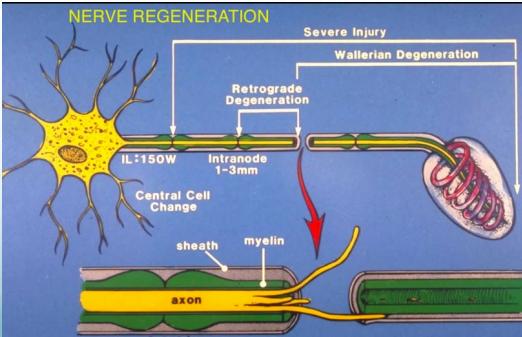
Degeneration Process
When a peripheral nerve is cut:
- Distal axon segments undergo Wallerian degeneration (cell death)
- Wallerian degeneration: Progressive destruction of distal axon segments
- Retrograde degeneration extends to the first Node of Ranvier
- Proximal axon segments undergo regeneration (attempt regrowth)
- Regeneration rate: Approximately 1mm/day
Regeneration Challenges
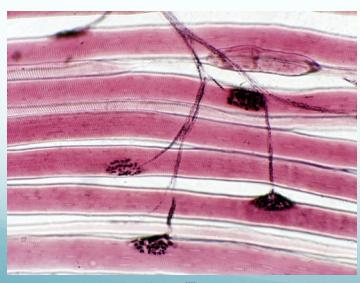
If muscles remain paralyzed for extended periods:
- Muscle atrophy and degeneration of motor end plates
- Joint stiffness and contracture development
- Clinical implication: Need to maintain muscle readiness and joint flexibility through physical therapy
Sources: stevegallik.org | houseofmind.tumblr.com
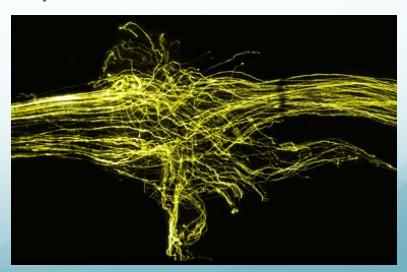
Complications of Regeneration
- Misdirected axonal growth in mixed nerves
- Motor-to-sensory and sensory-to-motor inappropriate connections
- Axonal loss during regeneration process
- Some axons fail to reach target destinations
- Time-dependent challenges:
- Motor end plate degeneration in denervated muscles
- Joint stiffness from prolonged immobilization
Seddon Classification of Mechanical Nerve Injuries
Overview
| Type | Severity | Structural Damage | Recovery Potential |
|---|---|---|---|
| Neuropraxia | Mild | Conduction block without structural damage | Excellent (days-weeks) |
| Axonotmesis | Moderate | Axonal damage with intact connective tissue | Good (weeks-months) |
| Neurotmesis | Severe | Complete transection of nerve | Poor (requires surgery) |
| Z | |||
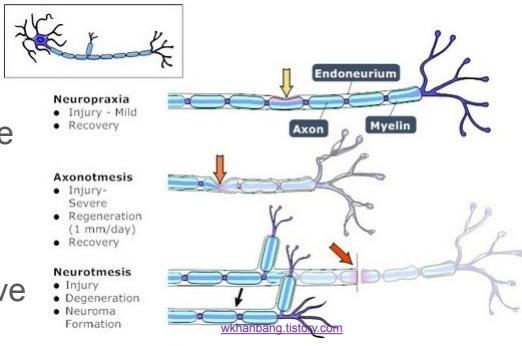 |
Neuropraxia (First Degree)
Pathophysiology:
- Result of blunt trauma or overstretching without structural damage
- Transient localized physiological conduction block
- No anatomical disruption of nerve fibers
- No distal Wallerian degeneration occurs
Clinical Features:
- Presents primarily as motor paralysis
- Some residual sensory or autonomic function typically preserved
- Nerve conduction studies: Show conduction block at injury level
Prognosis and Management:
- Complete recovery typically occurs within days to weeks
- Usually diagnosed by exclusion of more severe injuries
- Conservative management with observation
Axonotmesis (Second Degree)
Pathophysiology:
- Result of more severe blunt injury, traction, or overstretch
- Axonal damage within intact connective tissue framework
- Endoneural tubes remain intact and provide pathway for regeneration
- Distal Wallerian degeneration occurs distal to injury
Clinical Features:
- Significant motor and sensory deficits
- More complete functional loss than neuropraxia
Prognosis and Management:
- Expected spontaneous recovery
- Recovery may take weeks to months
- May leave residual deficits due to imperfect regeneration
- Physical therapy to maintain joint mobility and muscle readiness
Neurotmesis (Third Degree)
Pathophysiology:
- Complete transection of nerve:
- All nerve components severed (axons, myelin, endoneurium, perineurium, epineurium)
- Neuroma formation at injury site
- Disorganized mass of regenerating axons, Schwann cells, and fibroblasts
Clinical Features:
- Complete loss of motor and sensory function
- Permanent functional deficit without intervention
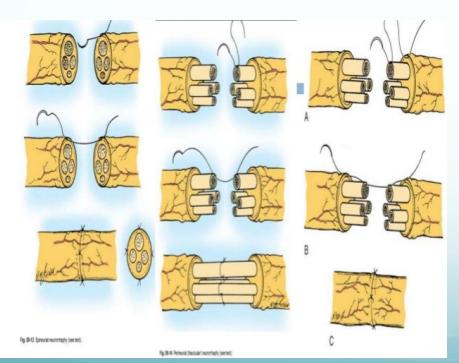
Prognosis and Management:
- Function never returns to normal without surgical intervention
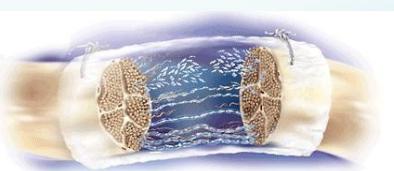
- Surgical repair required:
- Epineural repair: Suturing of outer nerve sheath
- Endoneural repair: Microscopic repair of individual fascicles
- Cable grafting: Using donor nerve (commonly sural nerve) for gaps
- Tube scaffolds: Synthetic conduits for nerve regeneration

Source: w.axogeninc.com
Clinical Assessment of Nerve Injuries
Comprehensive Evaluation
Medical History
- Thorough history collection:
- Symptoms indicating nerve dysfunction
- Mechanism and timing of injury
- Progression of symptoms
- Associated medical conditions
Physical Examination
- Systematic neurological examination:
- Motor function assessment (strength testing)
- Sensory examination (light touch, pinprick, temperature)
- Reflex testing
- Special tests for specific nerve injuries
Diagnostic Investigations
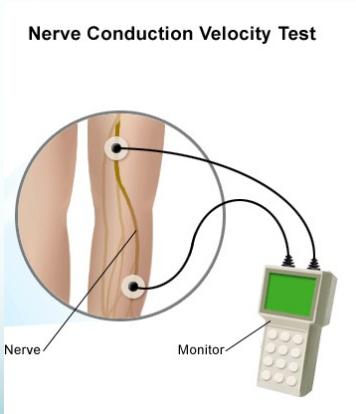
- Electrodiagnostic studies:
- Nerve conduction studies:
- Localizes injury site
- Determines severity of injury
- Assesses recovery progress
- Electromyography (EMG): Evaluates muscle denervation and reinnervation
- Nerve conduction studies:
- Imaging studies: MRI or ultrasound when indicated