Introduction
Limping is a common presentation in children seen by orthopedic surgeons, pediatricians, and primary care physicians. A proper evaluation requires:
- Comprehensive History
- Thorough Physical Examination
- Appropriate Investigations
Many conditions causing limping are age-specific, making age a crucial diagnostic factor.
Clinical Case Presentations
Case 1: 6-year-old, limping on left side

Case 2: 14-year-old boy, limping on left side

Case 3: 16-year-old, bilateral limping

History Taking
Essential Components
- Duration and onset - When first noticed
- Pain characteristics - Location, severity, timing
- History of trauma - Recent or remote
- Associated systemic symptoms
- Fever
- Night sweating
- Anorexia
- Weight loss
Common Pitfalls in History Taking
- Misled by parents’ history
- History of trauma may be unreliable
- Parents may notice leg length inequality that’s not clinically significant
- Misled by patients’ complaint
- Hip problems often present with knee pain
- Children below 5 years may not complain of pain!
Tutorial on Limping


Authors: Prof. Mamoun Kremli, Dr. Tarif Alakhras
Introduction
Limping is a common presentation in both children and adults, caused by numerous diseases. A proper evaluation requires:
- Comprehensive History
- Thorough Physical Examination
- Appropriate Investigations
Many conditions are age-specific, making chronological assessment crucial.
Definition of Limping
- A form of walking that favors the use of one leg over another
- An asymmetric abnormality of the gait pattern
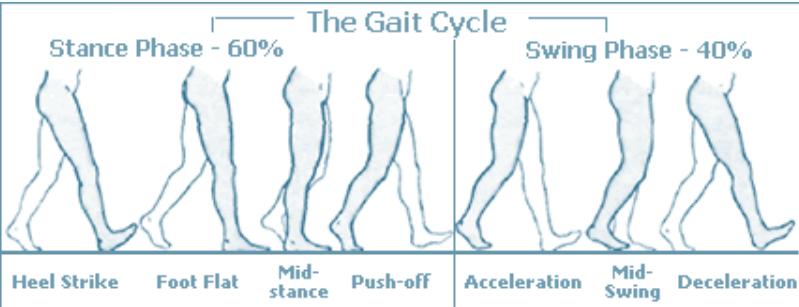
The Normal Gait Cycle
Understanding normal gait is essential for recognizing abnormalities:
Stance Phase (60% of gait cycle)
- Heel strike
- Foot flat / Mid-stance
- Push off
Swing Phase (40% of gait cycle)
- Acceleration
- Mid-swing
- Deceleration
Gait Cycle Overview: Stance Phase - 60% | Swing Phase - 40%
| Phase Component | Description |
|---|---|
| Heel Strike | Initial contact |
| Foot Flat | Weight acceptance |
| Mid-stance | Single limb support |
| Push-off | Propulsion |
| Acceleration | Initial swing |
| Mid-Swing | Mid-swing phase |
| Deceleration | Terminal swing |
Etiology of Limping
Limping can be categorized by underlying mechanism:
1. Pain-Related Limping
Painful limping presents as antalgic gait - shortened stance phase of the gait cycle.
Causes:
- Trauma
- Major musculoskeletal injuries
- Splinters, pricks, wounds in foot
- Infection
- Acute osteomyelitis
- Septic arthritis
- Inflammatory Joint Diseases
- Rheumatic conditions
- Degenerative arthritis
- Achilles tendinitis
- Plantar fasciitis
- Inflamed bunion
- Tumors
- Benign (e.g., osteoid osteoma)
- Malignant bone tumors
- Specific Orthopedic Conditions
- Acute SCFE
- Perthes disease (avascular necrosis)
- Systemic Diseases
- Sickle cell disease
- Osteochondritis
- Hemophilia
- Leukemia
- Appendicitis/Psoas abscess
2. Deformity-Related Limping
Congenital Deformities:
- Developmental Dysplasia of the Hip (DDH)
- Club foot
- Congenital limb shortening
Acquired Deformities:
- Malunion fractures
- Developmental abnormalities
- Metabolic bone disease
3. Weakness-Related Limping
-
Neurological causes:
- Nerve injuries/diseases
- Stroke
- Cerebral palsy
- Parkinson’s disease
- Multiple sclerosis
- Peripheral nerve disorders
-
Muscle weakness:
- Secondary to disuse
- Secondary to nerve injury
- Muscular dystrophy
4. Balance-Related Limping
- Inner ear infections
- Cerebellar ataxia
- Neurological conditions affecting
- stroke, cerebral palsy, parkinson’s disease, multiple sclerosis
- peripheral nerve disorder
5. Other Causes
• SCFE • Perthe’s disease • Sickle cell disease • Osteochondritis • Hemophilia • Leukemia • Appendicitis / Psoas abscess • Conversion disorders
- Conversion disorders (psychogenic)
- Idiopathic conditions
Classification by Pain Characteristics
Painful Limping
- Antalgic gait - short stance phase
- Causes: trauma, infection, inflammation, tumors, acute SCFE, Perthes disease
Painless Limping
- Normal or prolonged stance phase
- Causes:
- Congenital/developmental deformities
- Leg length discrepancy
- Benign bone tumors
- Chronic conditions (e.g., chronic SCFE, late Perthes)
Gait Pattern Analysis
Common Gait Abnormalities:
Group 1 - Primary Gait Patterns:
- High steppage gait: Foot drop - neurological disease
- Trendelenburg gait: DDH, weak hip abductors
- Circumduction gait: Stiff hip, neurological disease
- Tip-toe gait: Tight Achilles tendon, CTEV, cerebral palsy, habitual, compensating for length discrepancy
- Lurching gait: Short limb
Group 2 - Balance-Related Patterns:
- Wide-based gait: To gain balance - neurological disease
- Scissoring gait: Tight hip adductors - cerebral palsy
- Hemiplegic gait: Cerebral palsy, neurological conditions
- Ataxic gait: Neurological disease
- Foot inversion/eversion: Foot deformity or pain avoidance
Group 3 - Special Patterns:
- Stiff-knee gait: Knee disease, arthrogryposis
- Hand-knee gait: Weak quadriceps femoris muscle
History-Taking for Limping
Onset Characteristics:
- Sudden onset: Suggests trauma
- Gradual onset: Suggests progressive disease
Essential Historical Elements:
- Duration: When first noticed
- Associated features:
- Pain characteristics
- Visible deformity
- Swelling
- Systemic symptoms:
- Fever
- Night sweating
- Anorexia
- Weight loss