Hand, foot, and mouth disease (HFMD)
- HFMD: oral enanthem and a macular, maculopapular, or vesicular rash of the hands and feet (and possibly other locations).
- HFMD occur during summer & autumn, most cases occur in infants and children less than 7Y.
- Multiple enterovirus serotypes can cause HFMD. Coxsackievirus A16 and enterovirus A71 are the most common causes of HFMD.
- Transmitted from person to person by the fecal-oral route; oral and respiratory secretions and vesicle fluid.
- Incubation period is 3-5 D..
Clinical manifestations of hand, foot, and mouth disease associated with coxsackievirus A6 in Shizuoka, Japan, June-July 2011




(A) Hand and arm of a 2.5-year-old child. (B) Foot and (C) buttocks of a 6-year-old child. (D) Nail matrix of a 20-month-old child.
HFMD Clinical features
- Typical HFMD:
- Presents with complaints of mouth or throat pain or refusal to eat. Fever, if present, is usually <38.3°C.
- Prodromal symptoms usually are absent, include fever, fussiness, abdominal pain, emesis, diarrhea.
- Oral enanthem: begins as erythematous macules that progress to vesicles with diameters 1 - 5 mm.
- Vesicles quickly rupture and form superficial ulcers with diameters 1 - 10 mm.
- Painful oral lesions develop commonly on the tongue and buccal mucosa.
- Oral lesions may occur without skin lesions.
☐ The exanthem may be macular, maculopapular, or vesicular. ☐ Vesicles diameter 1 - 10 mm, contain a clear or turbid fluid and are surrounded by a 1 mm halo of erythema. ☐ The exanthem is nonpruritic and typically involves the hands, feet, buttocks, legs, and arms. ☐ Skin lesions may occur without oral lesions.
 Hand-foot-and-mouth disease
Small ulcers are present on the oral mucosa.
Hand-foot-and-mouth disease
Small ulcers are present on the oral mucosa.
 Hand-foot-and-mouth disease
Tongue and buccal ulcers are present on the tongue.
Hand-foot-and-mouth disease
Tongue and buccal ulcers are present on the tongue.
 Generalized hand-foot-and-mouth disease (HFMD)
Generalized hand-foot-and-mouth disease (HFMD)





(A-C) Generalized HFMD related to CV-A16 in a 13-month-old child. (D) Generalized HFMD related to CV-A6 in a 12-month-old child. (E) Grouped vesicles in a 23-month-old child with HFMD related to CV-A16. (F) Grouped vesicles in an 18-month-old child with HFMD related to CV-A6.
Clinical course and complications
- HFMD are generally mild, self-limited illnesses.
- HFMD usually resolves within 7 to 10 days.
- Complications of HFMD are rare and include encephalitis, meningitis, flaccid paralysis, or myocarditis. These are most commonly associated with Enterovirus A71 infection.
 Eczema coxsackium
Eczema coxsackium
 Eruption of painful vesicular lesions in a background of atopic dermatitis of the hands.
Eruption of painful vesicular lesions in a background of atopic dermatitis of the hands.
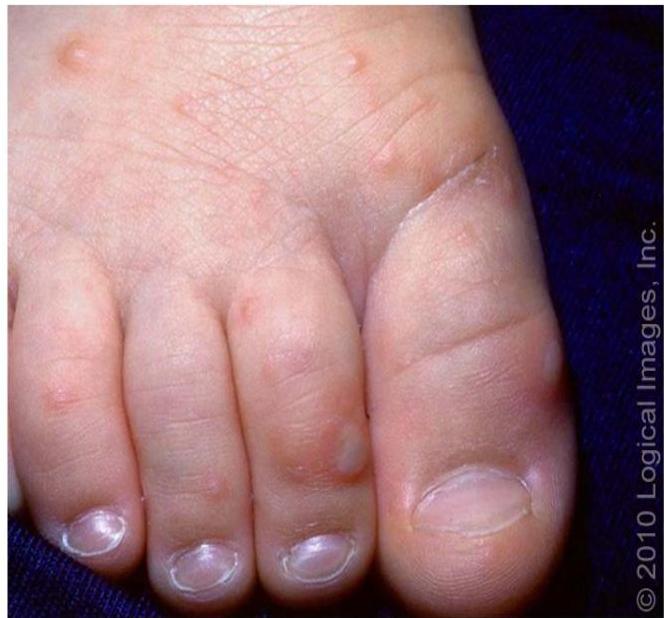 Hand-foot-and-mouth disease
Multiple vesicular lesions on an erythematous base are present on the foot.
Hand-foot-and-mouth disease
Multiple vesicular lesions on an erythematous base are present on the foot.
Diagnosis HFMD
- Diagnosis of HFMD is made clinically, based upon the typical appearance and location of the oral enanthem and exanthem.
- 75 % of patients have both the exanthem and the enanthem, and 10 % have only the enanthem or exanthem.
- Confirmation of a specific viral etiology is rarely necessary for uncomplicated HFMD.
- When etiologic confirmation is necessary, throat, stool, and vesicular fluid samples should be obtained for cell culture or nucleic acid amplification (eg, PCR).
- Identification or isolation of an enterovirus from vesicular fluid or CSF (meningitis complication) confirms the viral etiology of HFMD.
- Identification or isolation of an enterovirus from the stool or throat does not definitively establish causality. Following acute infection, enteroviruses are shed from the stool and throat for prolonged periods (6W to several M and up to 4 weeks, respectively) and the isolated virus may or may not be responsible for the current symptoms.
DIFFERENTIAL DIAGNOSIS HFMD
- Conditions associated with oral lesions:
- Herpangina.
- Aphthous ulcers: painful, shallow oral ulcerations with a greyish base, usually without skin lesions.
- Primary herpes simplex gingivostomatitis.
- Conditions with maculopapular or vesicular rashes:
- Insect bites (papular urticaria).
- Varicella.
- Eczema herpeticum.
- Mpox.
- Erythema multiforme major.
- Contact dermatitis.
- Autoeczematization (id reaction): pruritic, papulovesicular eruption and occurs secondary to tinea pedis, tinea corporis, or tinea capitis.
Management HFMD
- Most cases of uncomplicated HFMD resolve spontaneously within 7 days.
- Management is supportive. Pain and fever can be treated with ibuprofen or acetaminophen, as needed.
- Children who are unable to maintain adequate hydration may require hospitalization.
- For most children with HFMD-related oral lesions, do not use topical analgesic therapies. Evidence of benefit is lacking, and these therapies can cause toxicity from systemic absorption.
- Antiviral drugs with activity against enteroviruses have limited clinical availability.
- Evidence for IVIG efficacy in neonatal enterovirus infection is also mixed.
PREVENTION
- ☐ Hygiene – Hand hygiene is important in the prevention of community-acquired HFMD and herpangina.
- ☐ Surfaces that come in contact with oral secretions or feces should be cleaned and disinfected. Fomites that may spread the virus should also be cleaned and disinfected.
- ☐ Child care settings – Strict adherence to hand hygiene protocols is important when changing diapers because enteroviruses are shed in the stool for weeks following infection.
- ☐ Exclusion of infants and children from child care does not prevent the spread of HFMD. The viruses that cause HFMD can be spread by children without symptoms and children whose symptoms have resolved.
- ☐ Exclusion from child care is appropriate if the child is febrile or not feeling up to participating in class, and may be necessary if the child has many open blisters (to prevent secondary skin infection) or has extensive drooling from mouth lesions (which may require care from the child care provider that may compromise care for other children).
- ☐ Isolation – For hospitalized patients with HFMD, contact precautions, in addition to standard precautions, should be used for the duration of the illness.
- ☐ Vaccine – Three inactivated enterovirus A71 vaccines are available.