Herpes Simplex Virus type 1 (HSV-1)
- Worldwide, an estimated 67 percent of the population has herpes simplex virus type 1 (HSV-1) infection.
- The seroprevalence increased with age from 26% at 6 - 7 years to 36% at 12 to 13 years.
- Symptoms include recurrent oral or perioral lesions (“cold sores”), skin and mucous membrane lesions, genital lesions, ocular infections (eg, herpetic keratitis), and serious systemic illnesses such as encephalitis and neonatal disease involving multiple organs.
Transmission
- Transmission of HSV-1 occurs when someone with no prior infection with HSV-1 comes in contact with herpetic lesions, mucosal secretions, or skin that contain HSV-1.
- HSV-1 transmission typically occurs via oral-oral, oral-genital, or genital-genital contact, as well as contamination of skin abrasions with infected oral secretions.
- Primary genital HSV-1 infection is thought to be transmitted most frequently through oral-genital contact.
- Transmission can occur if the source is asymptomatic or symptomatic when contact occurs; however, transmission is more likely if the source is symptomatic since the viral quantity is greater when lesions are present. HSV-1 can also be transmitted during episodes of asymptomatic shedding in the saliva occurs on 3.6 - 25 % of saliva specimens from patients with evidence of HSV-1 infection only by clinical history or serology.
- In patients with herpes keratitis (which is due to reactivation of latent disease), the risk of transmitting HSV to others from the infected eye is thought to be extremely low. However, transmission of ocular HSV-1 has been documented in a case of corneal transplantation into an HSV-1-seronegative patient.
Populations at risk
- Most HSV-1 infections are acquired during intimate (but not necessarily sexual) contact. Under such circumstances, family members are the most likely source.
- Children are also at risk in day care centers where saliva sharing behavior can occur.
- Sexually active adolescents: acquire either oral or genital HSV-1 infection. Transmission via oral-genital or genital-genital contact.
- Athletes involved in contact sports eg wrestlers.
- Neonatal HSV-1 is transmitted from the maternal genital tract during delivery, often in the absence of history of genital herpes or lesions evident during labor.
- Health care workers – Occasional.
CLINICAL MANIFESTATIONS
- Asymptomatic infection — 80% patients with primary HSV-1 infections are asymptomatic.
- Oral infections — Inoculation of HSV-1 at mucosal surfaces or the skin results in viral replication at the epidermis and the dermis and infection of sensory and autonomic nerve endings. The virus then travels to sensory ganglia, where it establishes a latent reservoir that cannot be eliminated by the immune system. Once HSV-1 infection is established, the virus persists in a latent state in the trigeminal ganglia and reactivates intermittently.
- Gingivostomatitis and pharyngitis are the most frequent clinical manifestations of primary oral HSV-1 infection, whereas herpes labialis is the most frequent sign of reactivation disease.
CLINICAL MANIFESTATIONS
- Primary infection :
- Clinical illness typically occurs 2 - 12 days after exposure.
- Lesions occur anywhere on the pharyngeal and oral mucosa and progress over several days, eventually involving the soft palate, buccal mucosa, tongue, and the floor of the mouth. (herpetic gingivostomatitis).
- Intraoral vesicles ulcerate rapidly, gingivitis and extensions to lips and cheeks can be seen, with consequent difficulties in eating, drinking, and swallowing.
- Systemic symptoms : fever, malaise, myalgias, irritability and headache, with local lymphadenopathy.
- In the absence of antiviral therapy, lesions associated with primary HSV-1 infection last for 12 Days (Range 7 – 18 Days).
- Children may require hospitalization for pain control and/or dehydration.
Herpes Simplex Virus type 1
-
☐ Gingivostomatitis is the most common manifestation of primary herpes simplex virus (HSV) infection during childhood. (13- 30%).
-
☐ Primary herpetic gingivostomatitis is characterized by ulcerative lesions of the gingiva and mucous membranes of the mouth often with perioral vesicular lesions.
-
Recurrent HSV-1 infections of the lips and perioral area occur in 20 - 40 % of the infected population.
-
It is rarely associated with systemic symptoms.
-
Precipitating factors for HSV-1 recurrence include immunodeficiency, stress, exposure to sunlight, and fever.
-
Trauma to the area of primary infection, such as trigeminal nerve manipulation or dental procedures, may also trigger a recurrence.
-
Recurrences occurred as frequently as once per month (24 %) or as infrequently as twice per year (19 %).
-
Most patients (>85 %) develop prodromal symptoms about 24 hours before the appearance of painful lesions.
-
These symptoms can include pain, burning, tingling, and pruritus and last from 6 - 53 H prior to the appearance of the first vesicles.
-
Typically present as localized oral-labial ulceration (herpes labialis or cold sores).
-
Recurrences typically present at the vermillion border (where the colored portion of the lips meets the skin), although they can also occur on the buccal intraoral surface.
-
Recurrent lesions progress from vesicle to crust in 5-8 days in the absence of antiviral therapy, with significant diminution of pain after the first 24 hours.
 Herpetic gingivostomatitis
Herpetic gingivostomatitis
Scattered ulcerations with overlying slough on the tongue and lip of a child.
Cold sores (fever blisters)
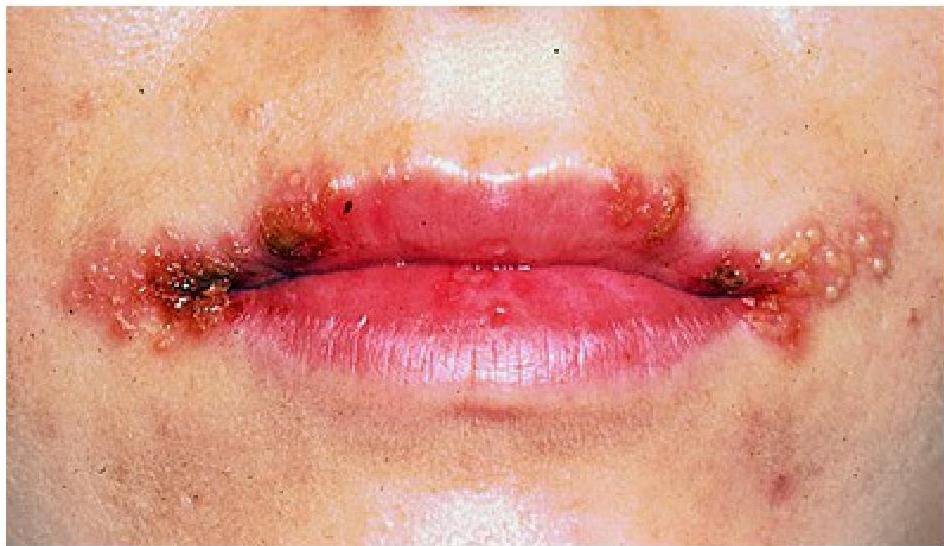
Cold sores are caused by reactivation of the herpes simplex virus. They are characterized by a vesicular eruption on the skin adjacent to the lips; the vesicles rupture to form ulcers and crusts that heal without scarring.

Cutaneous manifestations
Herpetic whitlow:
- HSV infection of the finger, known as herpetic whitlow, can occur by inoculation of the virus through a break in the skin barrier.
- Untreated, these infections gradually heal over 2-3 Weeks, but can recur.
- It is often misdiagnosed as a bacterial infection. The distinction is important, since antibiotics and drainage are not necessary.
- In young children, herpetic whitlow can occur at the time of primary oral infection through autoinoculation.
Erythema multiforme:
- HSV-1 infection is associated with the onset of erythema multiforme.
- It is an uncommon immune-mediated disorder that presents with cutaneous and/or mucosal lesions.
- HSV DNA may be detected from erythema multiforme lesions.
Eczema herpeticum:
- Patients with atopic dermatitis are at risk for developing an HSV-related skin complication called “eczema herpeticum”, particularly if they are taking immunosuppressive agents for control of eczema.
- It is characterized by cutaneous pain and vesicular new skin lesions secondary to a viral infection (usually HSV-1); in some cases, the rash may be difficult to distinguish from the patient’s baseline eczema if the latter is poorly controlled.
- It can spread rapidly, leading to severe morbidity and mortality in the absence of antiviral therapy; thus, prompt antiviral therapy is indicated while awaiting diagnostic testing for HSV, including administration of intravenous acyclovir in severe cases.
Ocular manifestations
- Ocular HSV infections occur in less than 5 % of patients.
- HSV keratitis has an acute onset with symptoms of pain, visual blurring and discharge. Signs are chemosis, conjunctivitis, decreased corneal sensation, and dendritic lesions of the cornea. Recurrent HSV-1 keratitis is a leading cause of corneal blindness.
- Acute retinal necrosis is a rare, potentially blinding, retinal disease resulting from HSV or VZV, characterized by decreased vision.
- Conjunctivitis and blepharitis: present as a unilateral conjunctivitis and/or blepharitis with the development of vesicles on the lid margin. Associated symptoms include chemosis, edema of the eyelids, and tearing.
- Chorioretinitis (posterior uveitis) is a manifestation of disseminated HSV infection, seen in neonates.
Other complications
- Encephalitis – is characterized by the rapid onset of fever, headache, seizures, focal neurologic signs, and impaired consciousness. Approximately one-third of cases occur in children and adolescents, with another peak among the elderly, likely reflecting primary HSV-1 infection in the former and reactivation in the latter.
- Bell’s palsy – HSV reactivation can cause Bell’s palsy. HSV-1 genomes were identified in facial nerve endoneurial fluid and auricular muscle in patients undergoing decompression surgery for Bell’s palsy.
- Aseptic meningitis
- Hepatitis — Disseminated disease with fulminant hepatitis is a rare complication of HSV infection.
- Respiratory tract infections — Children may develop epiglottitis or laryngitis (herpetic croup) with nonproductive cough and stridor. The illness is self-limited, lasting 10 - 14 days without complications

Herpetic whitlow

Herpetic whitlow
Grouped vesicles and erythema on the finger.

Erythema multiforme
Target lesions are present on the palm of this patient with erythema multiforme.
Cutaneous manifestations
Eczema herpticoform

Extensive herpes simplex virus infection manifesting with erythema, “punched-out” erosions, and crusts on the face of a child with preexisting dermatitis.
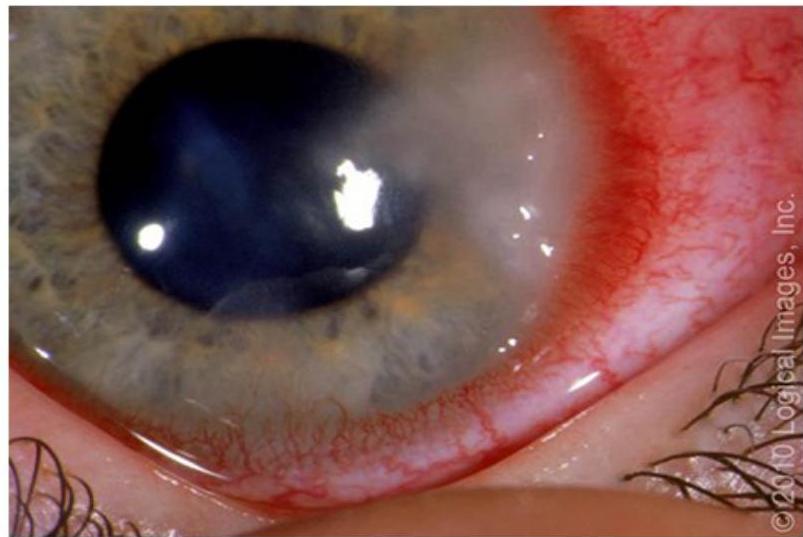 Herpes simplex keratitis
Herpes simplex keratitis
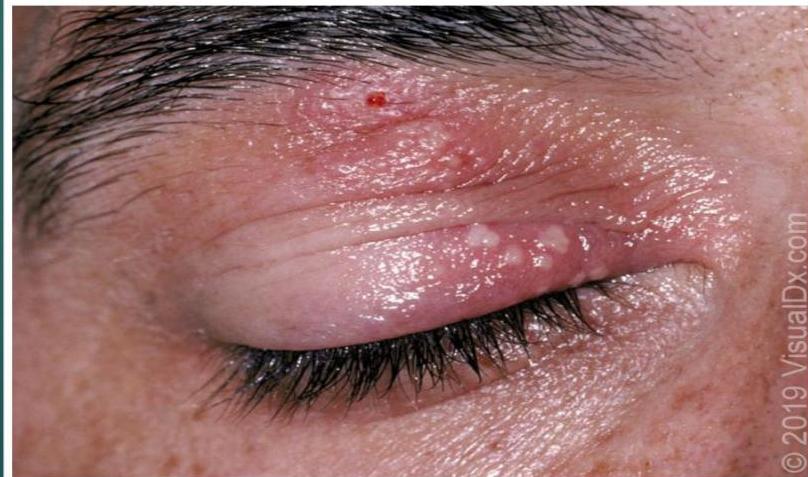 Herpes simplex virus blepharitis
Herpes simplex virus blepharitis
Grouped pustules on an erythematous base on the upper eyelid.
DIAGNOSIS
-
Mucosal or cutaneous disease :
-
The diagnosis of HSV infection is generally based upon virologic confirmation through DNA detection via PCR or culture of the virus. HSV PCR assays are most sensitive method to confirm HSV infection in clinical specimens obtained from mucocutaneous sites.
-
To obtain an adequate specimen for PCR or culture, the vesicle should be “unroofed” with a sterile swab. The base of the ulcer should be swabbed to isolate epidermal cells, which contain HSV.
-
Other tests, such as direct fluorescent antibody testing are less sensitive and less specific.
-
Serologic testing has limited application in confirming the diagnosis of acute HSV-1 infection. In addition, antibody titers have not been found to correlate with positive cultures or the presence of lesions.
-
Ocular disease - The diagnosis of ocular HSV-1 infection is often clinical, detection of viral DNA via PCR testing from intraocular fluid may be helpful to confirm the diagnosis of acute retinal necrosis.
-
Visceral and neurologic infection – HSV is often diagnosed by detecting:
-
HSV DNA from a sterile site (eg, CSF).
-
Identifying the organisms in a tissue biopsy (eg, lung, liver, or esophagus) based on pathologic findings (intranuclear inclusions and immunocytochemistry), or through culture.
-
HSV PCR from blood is helpful for diagnostic and clinical management purposes in cases of disseminated multi-organ neonatal herpes or fulminant HSV hepatitis.
Treatment
Treatment primary gingivostomatitis
Antiviral therapy :
- It is recommended for patients with primary gingivostomatitis who present within 72 hours of symptom onset. Early antiviral therapy leads to faster healing of lesions, decreased pain, and a shorter duration of fever.
- It still be offered if a patient presents with new lesions and/or significant pain after 72 hours of symptom onset.
- Oral treatment options for adolescents with primary infection include Acyclovir, Famciclovir, Valacyclovir.
- Patients with severe odynophagia may require hospitalization for intravenous acyclovir therapy,
- The usual duration of treatment is 7 to 10 days.
- Topical or oral analgesics. eg mouth rinses with viscous lidocaine or topical benzocaine.
- Intravenous rehydration may be required for patients with severe odynophagia.
Treatment of HSV-1 reactivation disease
-
Patients with mild to moderate symptoms:
-
In patients with minimal symptoms antiviral treatment is not necessary.
-
To help alleviate the minor discomfort, topical lidocaine can be given.
-
For patients who have occasional recurrences that are more severe, particularly those with a well-defined prodrome:
-
Episodic oral antiviral therapy is suggested, since treatment can decrease the length of recurrences if initiated promptly after onset.
-
Patients should have medications readily available so they can initiate therapy as soon as symptoms start to develop (eg, during the prodromal period).
-
Episodic treatment must be initiated quickly to be effective, given the rapid development of vesicles once prodromal symptoms occur and the rapid decline in viral shedding during reactivation disease (<48 hours).
-
Patients with severe disease :
-
Chronic suppressive antiviral therapy to reduce the number of clinical HSV episodes for the following patients :
-
Frequent recurrences of oral HSV-1, particularly if there is no clear prodrome.
-
Recurrences that are very bothersome to the patient (eg, disfiguring lesions or lesions associated with severe pain)
-
Recurrences that are associated with serious systemic complications (eg, erythema multiforme).
-
Suppressive therapy : acyclovir or valacyclovir .
-
In some patients, intense sunlight exposure can lead to HSV-1 reactivation, zinc-based sunscreen products and topical antiviral therapies is used to prevent these recurrences.
-
No approved vaccine available yet.