Dr. M. Almadani
How to solve it?
- HISTORY
- CLINICAL EXAMINATION
- CLINICAL DIAGNOSIS
- INVESTIGATIONS
- FINAL DIAGNOSIS
- TREATMENT
History
- Record date ozf history taking and examination
- Introduce yourself
- Explain & seek permission
- Full attention
- Treat with respect
- Let patient talk
- Guide, not dictate
- No leading question
- No short-cuts
- Try not to write and talk at the same time
- PERSONAL DETAILS
- PRESENTING COMPLAINT
- HISTORY OF PRESENT ILLNESS
- SYSTEMIC INQUIRY
- PAST MEDICAL/SURGICAL HISTORY
- HISTORY OF MEDICATIONS
- FAMILY HISTORY
- SOCIAL HISTORY
- OTHER HISTORY (Gyn.)
PERSONAL
- NAME
- AGE
- SEX
- NATIONALITY
- MARITAL STATUS
- OCCUPATION
PRESENTING COMPLAINT
What are you complaining of? (record in patient’s own words)
When more than one complain: Record in order of:
- Severity
- Chronicity
HISTORY OF PRESENT ILLNESS
- Full analysis of the complain or complaints
- Get right back to the beginning of the trouble
- Analysis of the possible related systems
COMMON COMPLAINTS
- Abdominal pain
- Abdominal mass/ swelling
- Abdominal distension
- Changes in bowel habit
- Vomiting
- Discharge (abdomen, perineum)
- Bleeding
- Weight loss
Analysis of pain
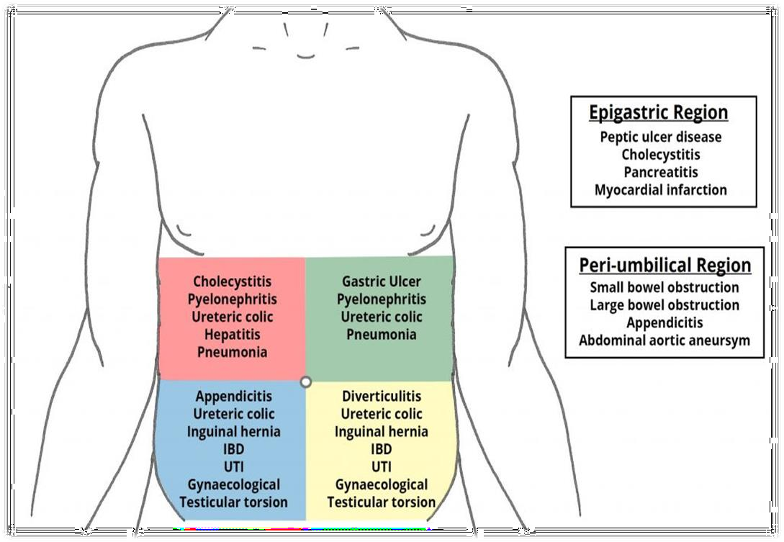
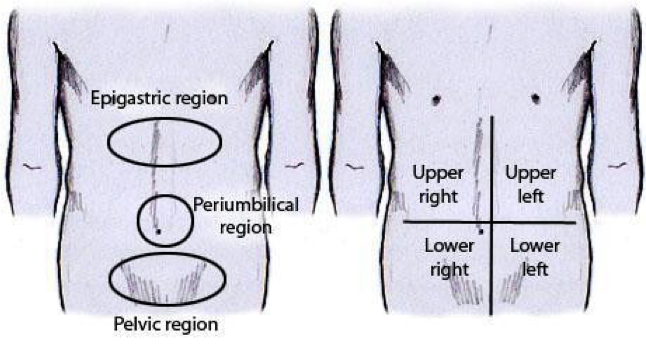
Site: where is the pain?
- Patients point with- finger vs hand
- Locations (Great degree of overlap)
- Right hypochondrium.- Hepatobiliary, gallbladder
- Left hypochondrium.- Spleen
- Epigastrium.- Stomach and duodenum
- Lumber- kidney
- Umbilical- small bowel, caecum, retroperitoneal
- Right iliac fossa- Appendix, caecum
- Left iliac fossa- Sigmoid colon
- Hypogastrium- Colon, urinary bladder, adenexae
Analysis of pain
Onset:
- Slow: inflammation
- Sudden: perforation, ischemia
Duration: acute or chronic
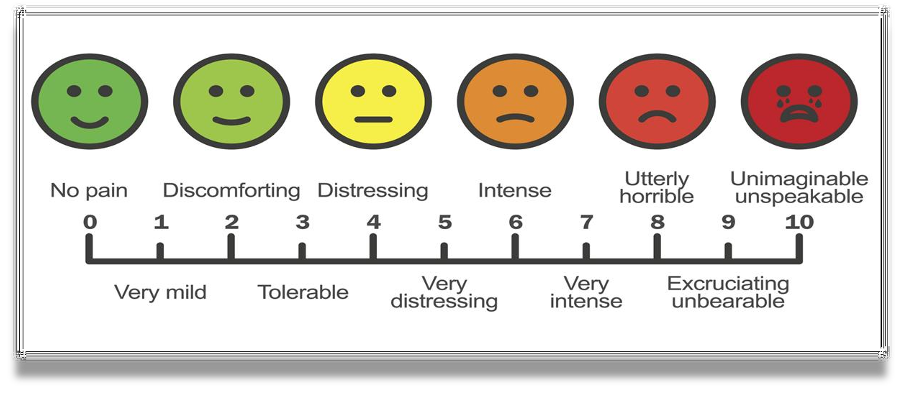
Severity: Numeric Pain Rating Scale (1-10)
- 4-6 – moderate pain
- Mild beginning- inflammation
- Severe- perforation, ischemia
Nature:
- Dull (inflammation),
- Sharp (rupture viscus),
- Colic (intermittent)
- Throbbing (abscess)
Progression:
- Steady increase (inflammation),
- Fluctuating (colic)
Aggravating factors:
- Fatty foods increases pain in gallstone disease
- Eating
- Fasting
Relieving factors:
- Sitting & leaning forward eases pain- acute pancreatitis.
- Eating relieves pain- duodenal ulcer
Radiation or referred pain:
- Shoulder- cholecystitis,
- Groin- ureteric colic
- Shifting or migration:
- periumbilical to RIF in acute appendicitis
Cause:
- Trauma,
- Food from outside- gastroenteritis
- Medication (NSAID)- perforation, bleeding
Swelling or mass
-
When noticed?
- Acute (hematoma, abscess)
- chronic- neoplasm, organomegaly
-
How noticed?
- Incidentally noticed swelling may be present for longer duration
-
Painful or painless?
- Inflammatory, neoplasm
-
Change in size
- since first noticed? Increase- neoplasms,
- disappear or reduce in size-?hernias/ improved inflammation
-
Aggravating/relieving factors:
- Hernias increase in size with activity/cough
-
Any cause?
- Trauma- hematoma, cough- hernia
B Symptoms
Weight loss, loss apetite, Night sweats
Vomiting
- Non- bilious: Early stage, late- pyloric obstruction
- Bilious: bowel obstruction
- Faeculent: late stage of bowel obstruction
- Blood: Duodenal ulcer, oesophageal varices, tumor
- Vomiting relieves pain- gastric ulcer
- Vomiting food taken few days ago: pyloric stenosis
Bowel habit
Constipation:
- habitual, recent (neoplasm)
- Absolute constipation (obstipation):
- Intestinal obstruction
Diarrhoea:
- Duration (acute, chronic)
- Number of stool
- Any blood or mucous (IBD)
Color of stool:
- Bright red (anal, rectum),
- maroon (colon) black-
- melena (upper GI)
History of discharge
-
Site: anal, perineum, wound
-
Duration
-
Nature:
- purulent (anal fistula),
- bloody (hemorrhoid),
- fecal from wound ( int. fistula)
-
Relationship to defecation/stool
- mixed with stool- IBD,
- independent of stool- hemorrhoids
-
Any pain?
- Hemorrhoids
- Anal fistula
SYSTEMIC INQUIRY
Begin with the involved or affected (chief complain) system
Example: If the chief complaint is related to gastrointestinal system(GI)- continue with the GIT inquiry.
Respiratory system:
- Cough, sputum, hemoptysis, wheeze, dyspnea, chest pain
Cardiovascular system:
- Angina (cardiac pain), dyspnea ( rest/ exercise),
- Palpitations, ankle swelling, claudication
Obstetric & Gynecology
- LMP
- Vaginal discharge
- Vaginal bleeding
- Pregnancies
Nervous system
- Headache
- Fits
- Depression
- Facial/limb weakness
METABOLIC/ENDOCRINE
- Muscular pain
- Bone & Joint pain
- Swelling of joints
- Limitation of movements
- Weakness
- Bruising/ bleeding (nutrients deficiencies)
- Sweating (thyrotoxicosis)
- Thirst (diabetes)
- Pruritus (skin infection, jaundice, uremia, Hodgkin’s)
- Alcohol
- Weight loss- ?dieting, amount and duration
PAST HISTORY
- Rheumatic Fever
- Tuberculosis/ asthma
- Diabetes
- Jaundice
- Blood transfusion
- Mental illness
- Operations/ accident
FAMILY HISTORY
- Diabetes
- Hypertension
- Heart disease
- Malignancy
- Cause of death
- Father/Mother/Siblings/Spouse/Children/Grand parents / Close relatives - Anybody with Sudden death - not clear/severe disease/died from… Z
HISTORY OF MEDICATIONS
- Insulin
- Steroids
- NSAID
- Contraceptive pills
- Antibiotics
- Others
SOCIAL HISTORY
- Marital status
- Occupation
- Travel abroad
- Accommodation
- Habits ( smoking, alcohol )
- Dependent relatives
- Psychiatric/ emotional background
Immunization & Allergies
- Allergies
- Food
- Drugs
- Immunizations
- Tetanus
- Diphtheria
- Tuberculosis
- Hepatitis
- Others
Before starting clinical examination:
- Analyze patient’s history.
- Probable diagnostic possibilities
- Think of the common diseases
- Determine physical findings consistent with these entities.
- Permission
- Privacy
- Presence of a nurse
- Precautions (hand hygiene)
Exposure:
- Exposure: nipples to knees (ideal)
- Cover genitalia
- Patient lying flat on a pillow
- Arms by the side (not under the head!)
- Sit or kneel beside the patient
- Adequate light
Observe your patient while history taking for:
- General health - emaciated (? Malignancy)
- Intelligence
- Attitude
- Mental state (dehydration, encephalopathy)
- Posture:
- Peritonitis - flexed & still
- Intestinal, biliary or renal colic - rolling around in agony
- Mobility
4 parts
-
Inspection
-
Palpation
-
Percussion
-
Auscultation
- Practice a standard routine every time
- Hand - head to toe
- Head to toe
General
Vitals
- Weight - loss (malignancy), gain (DU)
- Pulse (Tachycardia - infection, fluid/blood loss)
- Blood pressure (low - fluid loss, bleeding)
- Temperature (Fever - infection)
- Respiration rate - raised in infections
- Pulse - rate, rhythm, volume, nature
Hands
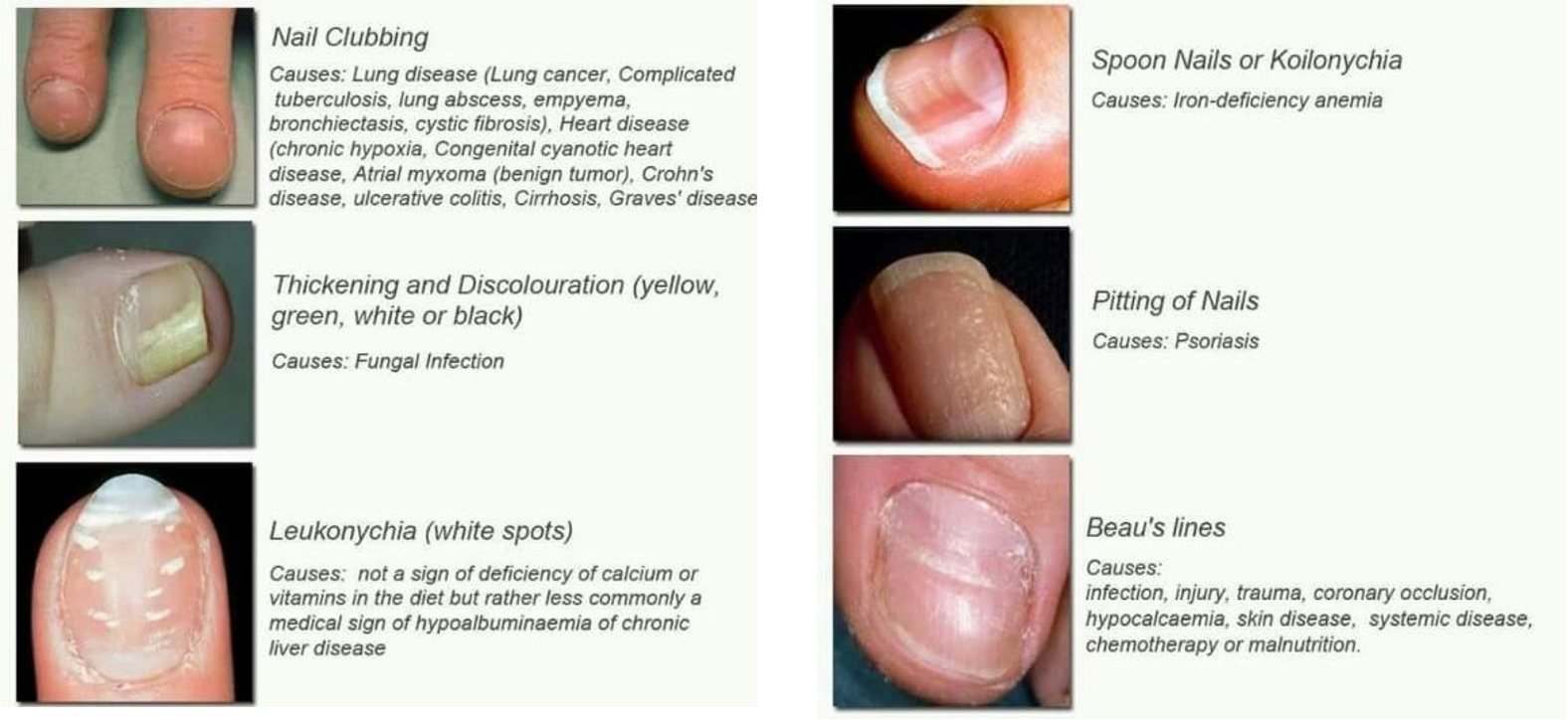
- Nails - koilonychia, clubbing, leukonychia
- Skin - dehydration, moist palm, anemia
- Anemia - conjunctiva, nail bed
- Jaundice - sclera, under the surface of the tongue
- Oral cavity - mucous membrane for hydration, tongue for coating
- Scalp
- Ear/nose
Head, Neck, chest, Abdomen extremities
- Neck - vein, goiter, lymph nodes, other swellings
- Chest - asymmetry, expansion, breath sound, added sound
- Cardiac - rhythm, heart sound, murmur
- Limbs - asymmetry, swelling, movement, pulses, power
- Abdomen (local examination)
Inspection
- Asymmetry - from the foot end of the bed - mass
- Movement with breathing (restricted in peritonitis)
- Swelling/mass - location
- Distension - central (SIO) or peripheral (LBO, ascites)
- Scar, sinus, wounds
- Prominent veins - portal hypertension
- Umbilicus - shape, discharge, swelling
- Cough impulse - groin, umbilicus, scar
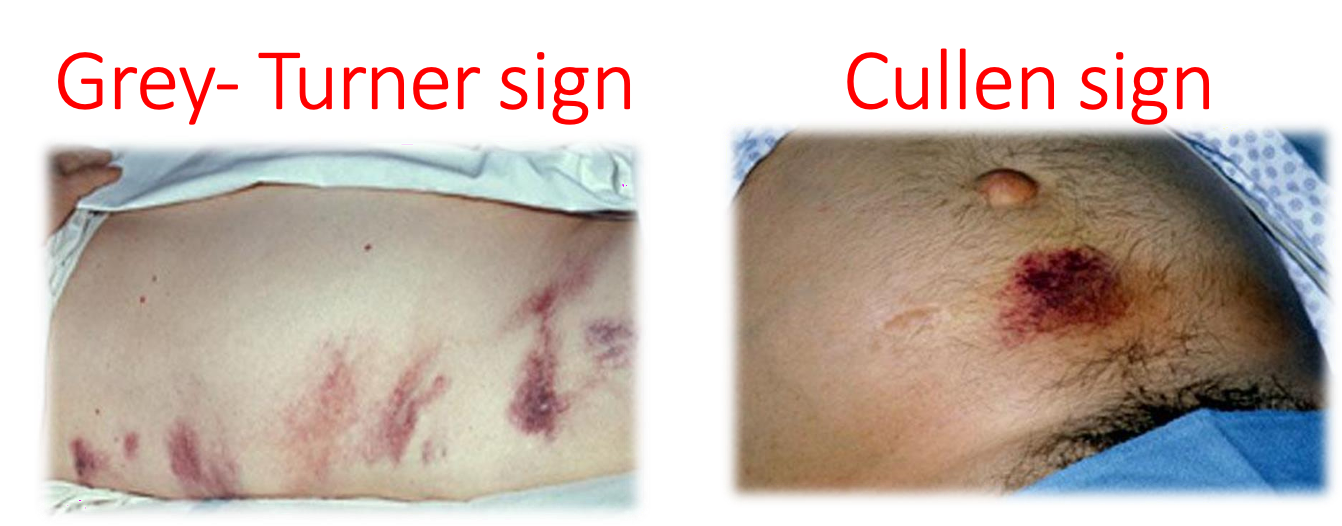
Grey-Turner sign & Cullen sign
 1- abcess 2- periumbilical hernia 3- inisional hernia
1- abcess 2- periumbilical hernia 3- inisional hernia
 ascites / caput medusa
ascites / caput medusa
Palpation
-
Gentle/superficial palpation:
- Start away from the area of pain
-
Deep palpation:
- Deep tenderness
- Guarding: muscle contracted overlying the tender area (acute inflammation)
- McBurney’s point
-
Abdominal signs:
- Rebound/Rovsing’s
- Murphy’s
- Obturator
- Psoas
-
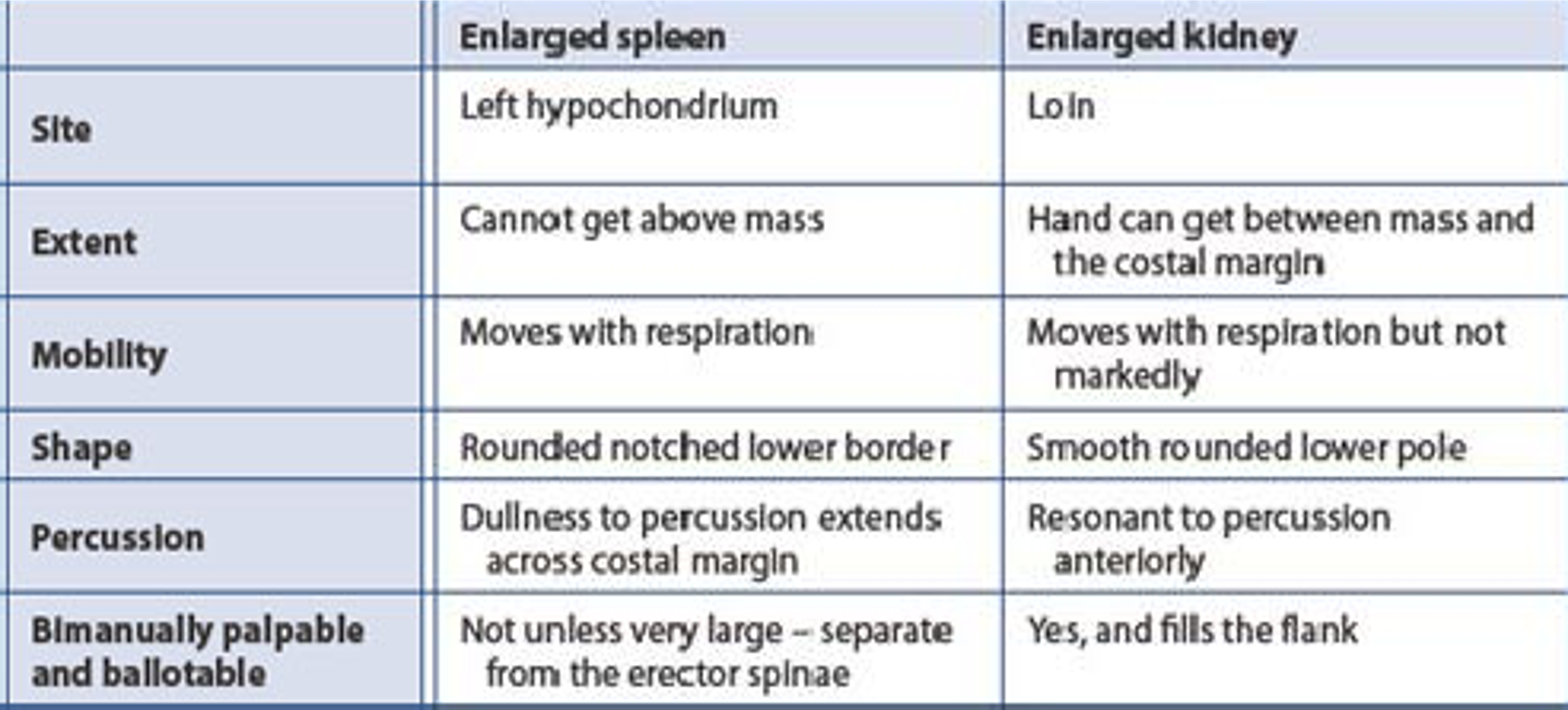
Organomegaly: liver, spleen, kidneys
-
Other masses - abdominal wall or intra-abdominal
-
Define all features of a mass: site, size, surface, borders, tenderness, pulsation, mobility
-
Cough impulse
Abdomen Mass Sites & Signs
| Mass Region | Possible Causes |
|---|---|
| RUQ | Ca. hepatic flexure, enlarged gallbladder, enlarged right kidney, hepatomegaly |
| epigastric region | Liver, gastric carcinoma, abdominal aortic aneurysm |
| LUQ | Splenomegaly, carcinoma descending colon, swelling in tail of pancreas, enlarged left kidney |
| periumbilical region | PUH, ca. transverse colon, tumour deposit (Sister Mary Joseph’s nodule) |
| LLQ | Descending colon (Benign, malignant Carcinoma), Sigmorectal - appendicitis could be transmitted from LLQ to RLQ |
| suprapubic region | Distended urinary bladder, pregnancy, ovarian mass |
| RLQ | Appendiceal disease, ca. ascending colon, Crohn’s disease of ileo-caecal area |
| inguinal region | Hernia, lymphadenopathy, aneurysm |
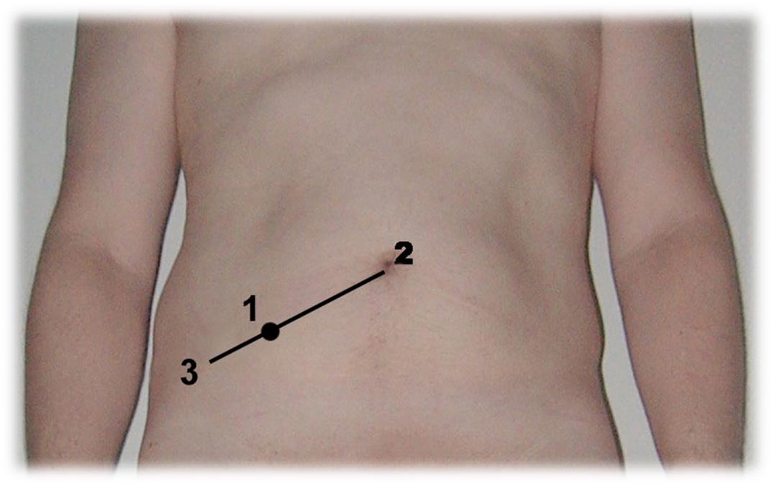 Mcburny pooint
Mcburny pooint
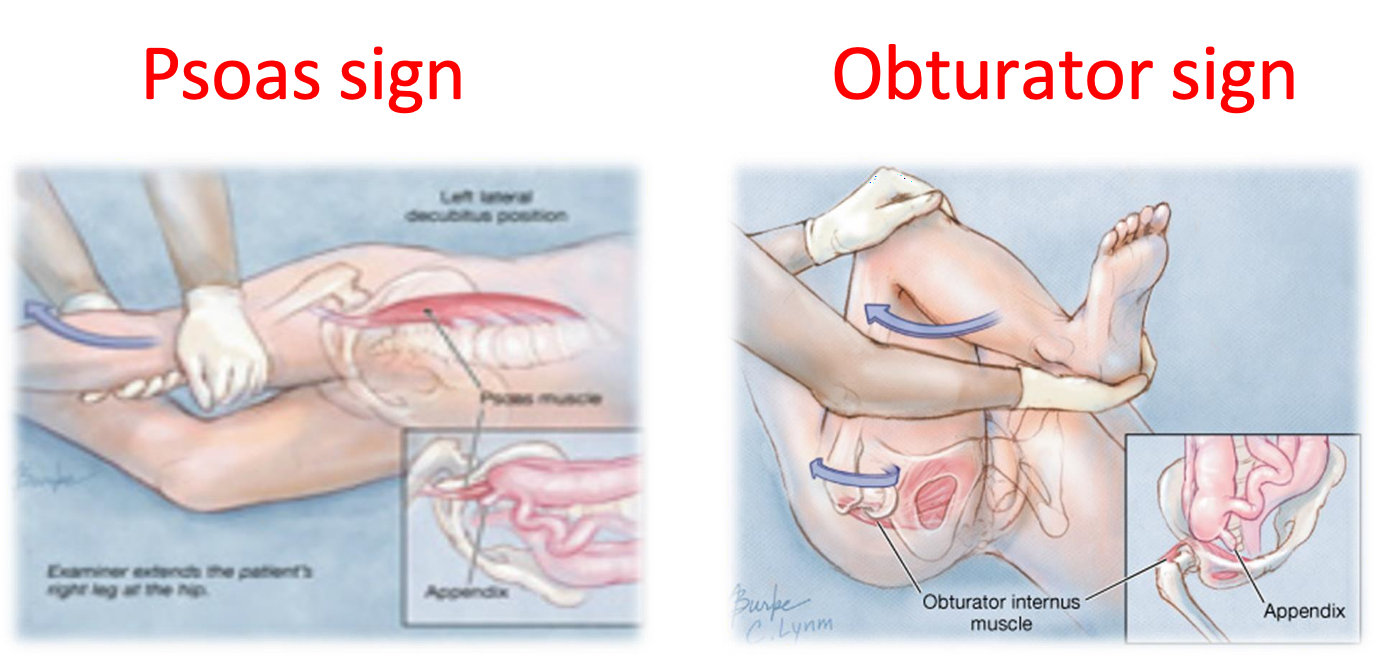 Psoas sign & Obturator sign
Psoas sign & Obturator sign
CC #Video


Percussion
- Organs and masses
- Liver span
- Ascites:
- Fluid thrill (large amount)
- Shifting dullness
Auscultation
- Bowel sounds
- Bruits
check inguinal hernia afterwards mention per rectal/vago examination