Acute Bacterial Rhinosinusitis (ABRS)
Defined by at least three symptoms/signs:
- Discolored mucus.
- Severe local pain (often unilateral).
- Fever > 38°C.
- Raised CRP/ESR.
- Double sickening.
Why bacterial infection happen?
- Obstruction of the various ostia
- Impairment in ciliary function
- Increased viscosity of secretions
- Impaired immunity
- Mucus accumulates
- Decrease in oxygenation in the sinuses
- Bacterial overgrowth
Common Clinical Presentations for ABS
- Persistent
- Worsening
- Symptoms
- Severe
Physical Findings
- Mucopurulent nasal discharge: Highest positive predictive value.
- Swelling of nasal mucosa.
- Mild erythema.
- Facial pain (unusual in children).
- Periorbital swelling.
Objectives of Treatment of Acute Bacterial Sinusitis
- Decrease time of recovery.
- Prevent chronic disease.
- Decrease exacerbations of asthma or other secondary diseases.
- Do so in a cost-effective way.
Suspected Microbiology of ABS (2013)
- Streptococcus pneumoniae: 15–20%
- Haemophilus influenzae: 45–50%
- Moraxella catarrhalis: 10–15%
- Streptococcus pyogenes: 5%
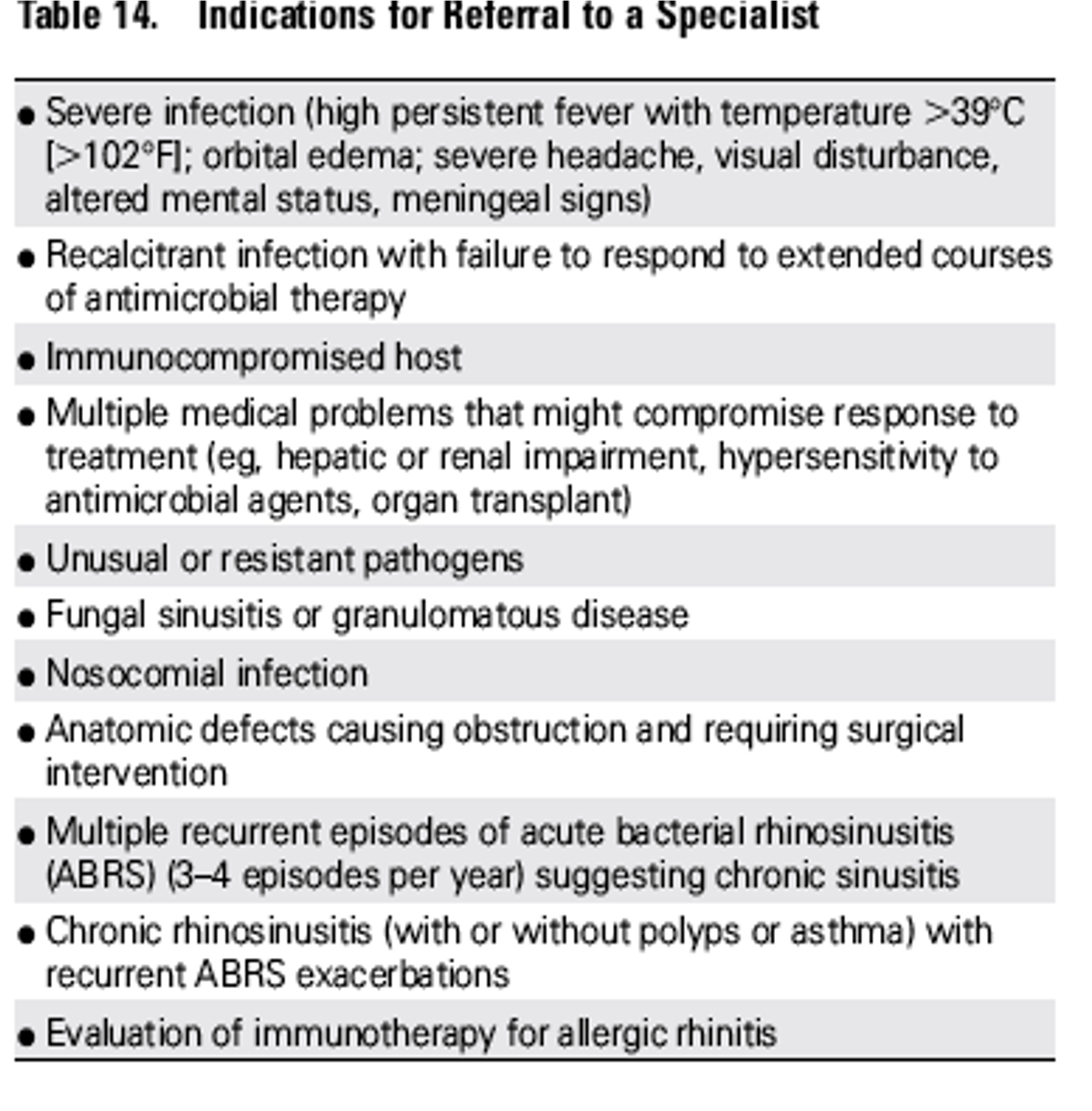
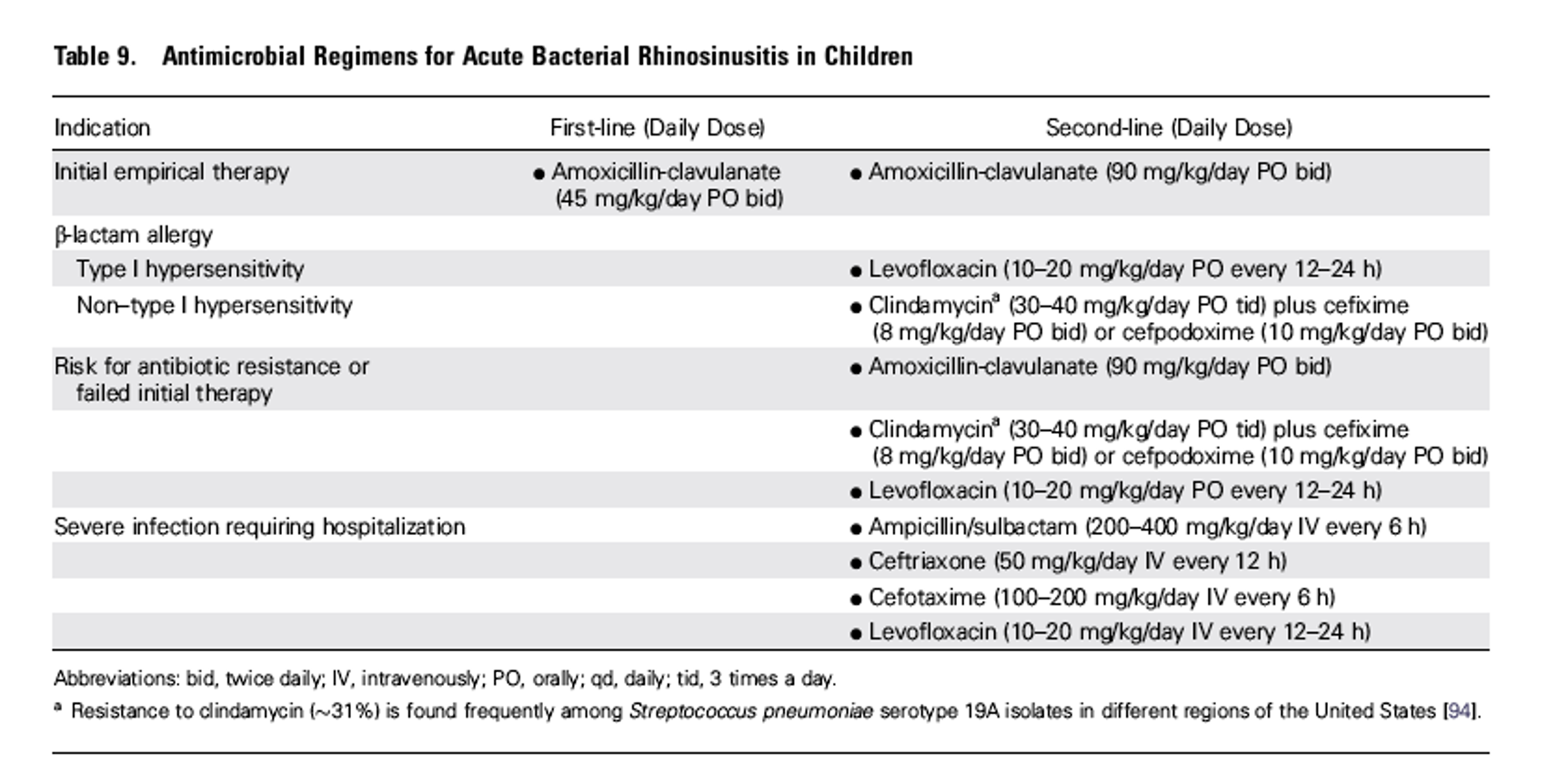
Treatment: Antimicrobial Regimens for Acute Bacterial Rhinosinusitis
Adjunctive Therapy
- Saline irrigation (physiological, hypertonic saline).
- Intranasal steroid.
- Topical/oral decongestants.
(All the above have weak recommendations.)
When Initial Empiric Antimicrobial Therapy Fails
- Symptoms worsen after 48-72 hours.
- Fail to improve after 3-5 days.
Look For…
- Resistant pathogen.
- Noninfectious etiology.
- Structural abnormality.
- Other causes for failure.
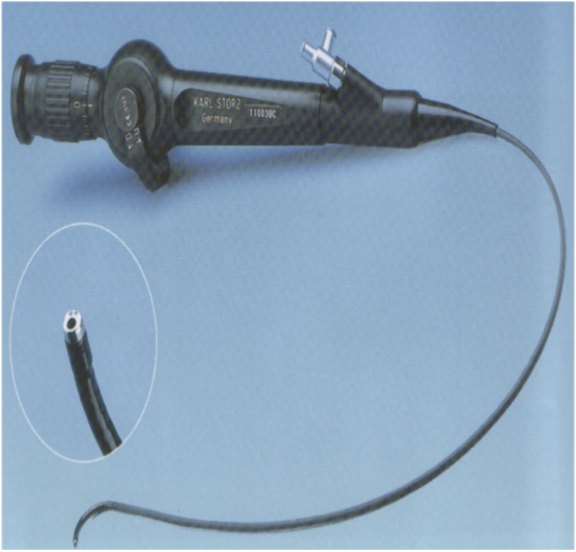
Rhinoscopy Findings
- Nasal polyps.
- Septal deviation.
- Concha bullosa.
- Eustachian tube dysfunction.
- Adenoid hyperplasia.
- Tumors.
Swab Culture
- Direct sinus aspiration better than nasopharyngeal swab.
Imaging Study
- Structural abnormality.
- Suppurative complications.
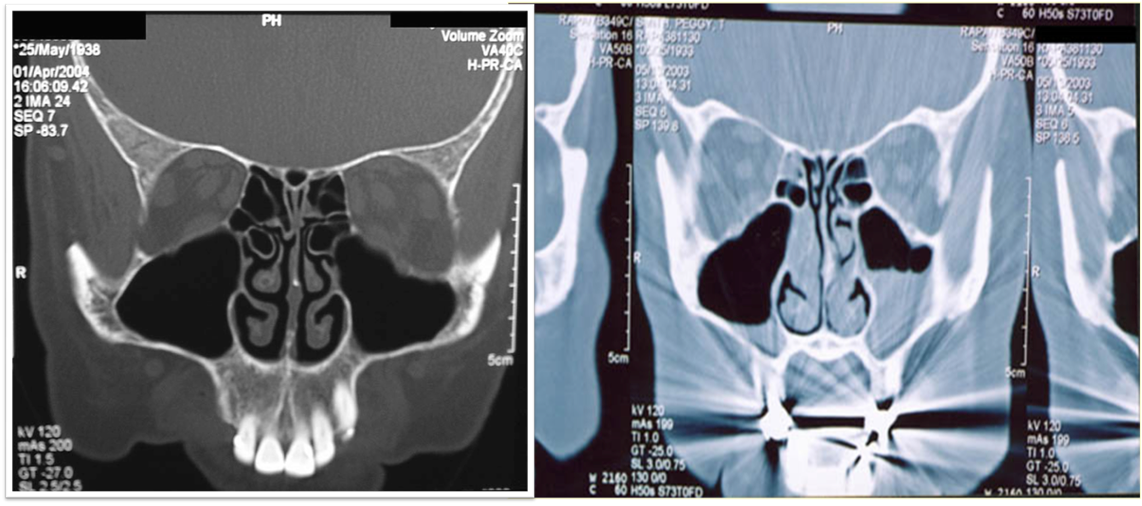
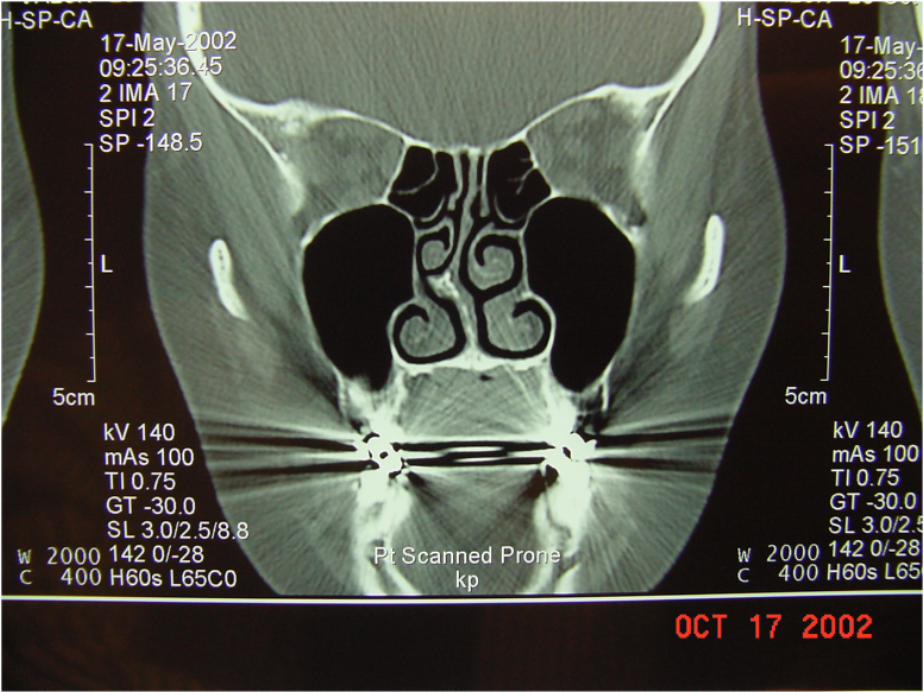 Clinicians should obtain a contrast-enhanced CT scan
Clinicians should obtain a contrast-enhanced CT scan
of the paranasal sinuses and/or an MRI with contrast whenever a child is suspected of having orbital or CNS complications of ABS
Complications of Acute Bacterial Sinusitis
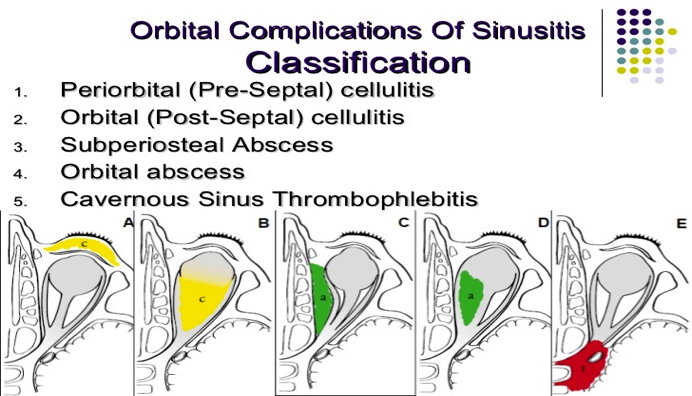
Orbital
-
Periorbital cellulitis.
-
Subperiosteal abscess.
-
Orbital abscess.
-
Optic neuritis.
-
Proptosis: Anterior and lateral displacement of the globe.
-
Impairment of extraocular movements.
-
Loss of visual acuity.
-
Chemosis: Edema of conjunctiva.

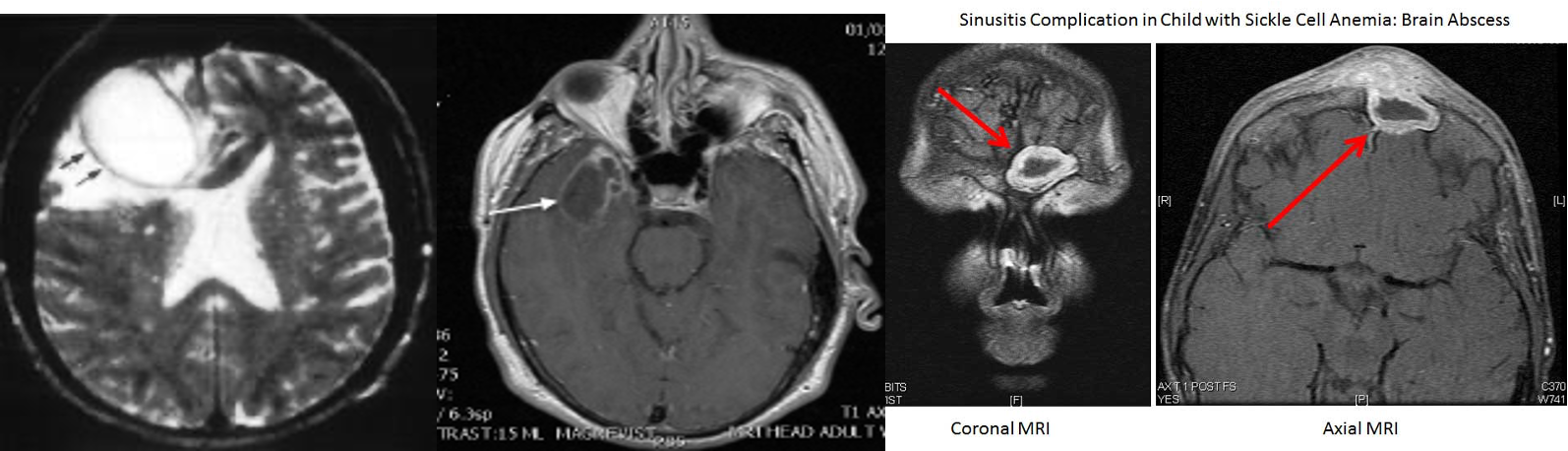
Central Nervous System
Suspected with:
- Very severe headache.
- Photophobia.
- Seizure.
- Other focal neurologic findings.
Complications
- Meningitis.
- Subdural empyema.
- Epidural abscess.
- Intracerebral abscess.
- Cavernous sinus thrombosis.
Other
- Septicemia.
- Osteomyelitis.
Suppurative Complications
- Rare, occurring in 3.7-11% of hospitalized pediatric patients with sinusitis.
- Primarily related to orbital cellulitis or intracranial infection.
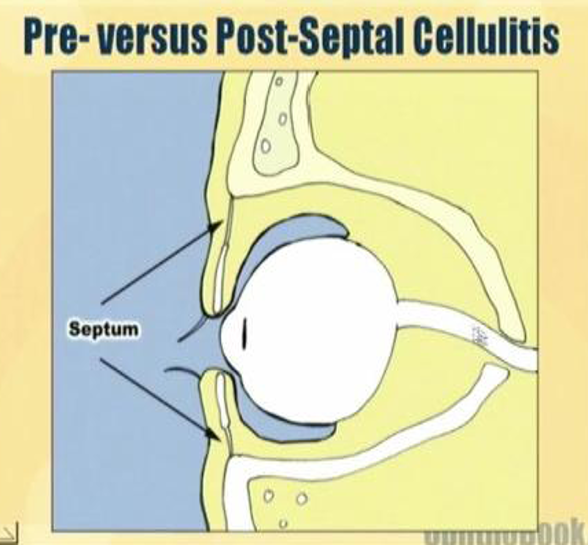
Periorbital and Orbital Cellulitis
- Orbital septum: Thin membrane separating superficial eyelid from deeper eye structures.
- Periorbital cellulitis: Bacterial infection of the eyelid and surrounding soft tissues (preseptal).
- Orbital cellulitis: Infection involving fat and muscles posterior to the orbital septum (postseptal).
Chandler Classification
- Preseptal cellulitis.
- Orbital cellulitis.
- Subperiosteal abscess.
- Intraorbital abscess.
- Cavernous sinus thrombosis.

 ccellulitis Z OSPE
subperisteal, sinusitis
ccellulitis Z OSPE
subperisteal, sinusitis
antibiotic, i/d
Indications for Hospitalization
- Acutely ill child or adult with high fever, severe head pain.
- Suspected sphenoid sinusitis.
- Complications involving eye, bone, or intracranial structures.