Table of Contents
- Case-7: Bronchial Asthma
- Brief Scenario
- Information for Student
- Task: What is Expected from a Student?
- Brief Scenario
- Information for the Simulated Patient
- Important Notes for the Simulated Patient (SP):
- Brief Scenario
- Case-7: Bronchial Asthma Checklist
- Professional Behavior
- History Taking Skills
- Clinical Examination
- Management
Case-7: Bronchial Asthma
Patient Brief Record / Brief Scenario
Information for Student
- Patient Name: Yasir
- Age: 30 years
- Occupation: Teacher, Private Primary School
- Location: Recently transferred from Jeddah to work in Riyadh.
- Today’s BP: 110/80 mm Hg
- Weight: 70 kg
- Height: 168 cm
Mr. Yasir is a 30-year-old who came today with complaints of difficulty in breathing and an on-and-off cough for the past two weeks.
Task: What is Expected from a Student?
- Take a focused history from this patient.
- Conduct a respiratory system examination, including Peak Flow Meter (PFM).
- Inform the patient about the possible diagnosis.
- Manage the case appropriately.
- Explain the management plan to the patient.
Patient Brief Record / Brief Scenario
Information for the Simulated Patient
- Patient Name: Yasir
- Age: 30 years
- Occupation: Teacher, Private Primary School
- Family: Married, with 2 children (1 and 3 years old).
You are a 30-year-old man who works as a teacher. You have transferred from Jeddah to work in Riyadh three weeks ago. A few days after arriving in Riyadh, you started experiencing cough and difficulty in breathing.
Opening Scenario: “I have difficulty in breathing and cough, doctor.” (You will admit only this information).
Tell your doctor about the following information only if specifically asked:
- Difficulty in breathing started a few days after arriving in Riyadh.
- Difficulty in breathing is more pronounced in the early morning, associated with a dry cough.
- You feel some wheezing during attacks.
- You have visited the Accident & Emergency (A&E) twice last week and were given oxygen and an injection.
- You were started on a Ventolin Inhaler, which provides some relief but not much.
- You are a non-smoker.
- Your younger brother is asthmatic.
- You are not known to have any other chronic illnesses.
- Patient’s Idea: Possibly, it is bronchial asthma, as your brother.
- Concern: Possibly, you will suffer from frequent visits to the Accident & Emergency.
- Expectation: To get medication that will relieve you completely.
- Any other points, please relate to your own personal and family history.
Important Notes for the Simulated Patient (SP):
- The doctor will examine your chest from the front and back to confirm the diagnosis.
Case-7: Bronchial Asthma Checklist
1. Professional Behavior
- Introduces himself and gets permission to take history and perform an examination.
- Starts with an open-ended question.
- Develops rapport with the patient.
2. History Taking Skills
- Explore the problem: time, duration, characteristics.
- Character of cough and sputum.
- Associated with wheezing?
- Aggravating and relieving factors.
- Family history of similar problems.
- Presence of plants or animals at home.
- Smoking history.
- Medications.
- Social history (home or work stress).
- Ongoing problems/past history.
- Summarizes the history taken from the patient.
- Explores the patient’s ideas, concerns, and expectations appropriately.
3. Clinical Examination
- General Examination:
- Vital signs.
- Respiratory system examination.
- Peak Flow Meter (PFM).
4. Management
- Explore the patient’s understanding of the problem.
- Explain the problem to the patient in a simple way.
- Inform about the diagnosis of Bronchial Asthma.
- Lab Investigations:
- Complete Blood Count (CBC).
- Pulmonary Function Test.
- Advise to avoid triggering factors.
- Prescribe a steroid inhaler and long-acting Salbutamol.
- Arrive at a shared understanding.
- Invite questions from the patient.
- Summarize at the end of the consultation.
- Arrange follow-up.
Asthma Q&A
Table of Contents
- Asthma Overview
- B. Asthma
- Key Questions
- Asthma Control and Management
- Asthma Control Test (ACT)
- Assessing Asthma Control in Adults
- Advanced Management
- Actions and Referrals
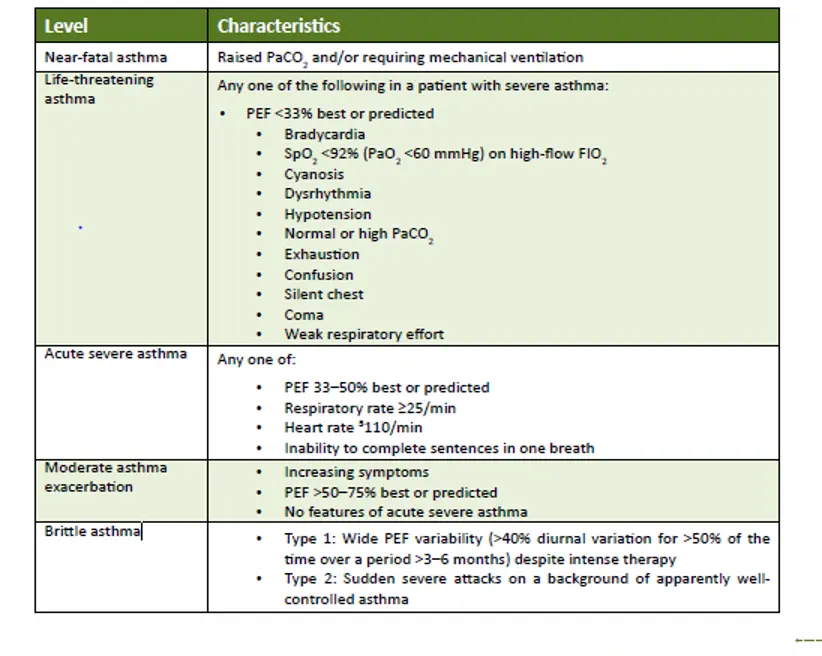
- Levels of Severity of Acute Asthma Exacerbations in Adults
Asthma
Overview
B. Asthma
-
What is the definition of bronchial Asthma?
- Bronchial asthma is a chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. It involves episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or early in the morning.
-
What are the symptoms and signs of Asthma?
- Common symptoms and signs of asthma include wheezing, shortness of breath, chest tightness, and coughing. These symptoms can vary in frequency and intensity and may worsen at night or with exercise.
-
How do you assess severity of Asthma?
- The severity of asthma is assessed based on the frequency and intensity of symptoms, the degree of airflow obstruction, and the impact on daily activities. It is often categorized into intermittent, mild persistent, moderate persistent, and severe persistent asthma.
-
What is the pathophysiology behind Asthma?
- Asthma is characterized by chronic inflammation of the airways, leading to increased airway hyperresponsiveness, mucus production, and bronchoconstriction. This results from a complex interaction between genetic predisposition and environmental factors, leading to immune system activation and inflammation.
-
Is Asthma reversible?
- Yes, asthma is considered a reversible condition, as the airflow obstruction can be reversed either spontaneously or with treatment, such as bronchodilators.
-
What investigations would you order for a patient you suspect having Asthma?
- Investigations for suspected asthma include spirometry to assess lung function, peak flow measurement, bronchoprovocation tests, allergy testing, and sometimes chest X-rays to rule out other conditions.
-
What are the parameters you use when measuring the severity of Asthma?
- Parameters include the frequency of symptoms, nighttime awakenings, use of rescue inhalers, impact on daily activities, lung function tests (FEV1 and FEV1/FVC ratio), and the frequency of exacerbations.
-
Is Asthma obstructive or restrictive lung disease and what is the difference?
- Asthma is an obstructive lung disease, characterized by difficulty in exhaling all the air from the lungs due to narrowed airways. In contrast, restrictive lung diseases involve reduced lung volume, making it difficult to fully expand the lungs.
-
What are some of the drugs we use in Asthma management?
- Drugs used in asthma management include short-acting beta-agonists (SABAs), long-acting beta-agonists (LABAs), inhaled corticosteroids (ICS), leukotriene receptor antagonists, and monoclonal antibodies like omalizumab.
-
What is the mechanism of the drugs used to reduce Asthma symptoms?
- SABAs and LABAs work by relaxing bronchial smooth muscle, leading to bronchodilation. Inhaled corticosteroids reduce airway inflammation. Leukotriene receptor antagonists block the effects of leukotrienes, reducing inflammation and bronchoconstriction.
-
What are some complications that could occur in long-lasting Asthma patients?
- Complications can include chronic airway remodeling, frequent respiratory infections, reduced lung function, and in severe cases, respiratory failure.
-
What does silent chest indicate?
- Silent chest is a clinical sign indicating severe airway obstruction in asthma, where airflow is so limited that wheezing is no longer heard. It is a medical emergency requiring immediate intervention.
-
What could be a possible differential diagnosis in a patient suspected with asthma?
- Differential diagnoses include chronic obstructive pulmonary disease (COPD), vocal cord dysfunction, heart failure, bronchiectasis, and pulmonary embolism.
-
What advice would you give an asthmatic?
- Advice includes avoiding known triggers, adhering to prescribed medication regimens, monitoring symptoms and peak flow, maintaining a healthy lifestyle, and having an action plan for exacerbations.
-
What is atopy?
- Atopy is a genetic predisposition to develop allergic reactions, such as asthma, allergic rhinitis, and atopic dermatitis, due to heightened immune responses to common allergens.
-
What is Churg Strauss syndrome?
- Churg-Strauss syndrome, now known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune condition characterized by asthma, eosinophilia, and systemic vasculitis affecting small to medium-sized blood vessels.
Key Questions
Key Questions
-
What is asthma?
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to difficulty in breathing. It is often associated with symptoms such as wheezing, coughing, shortness of breath, and chest tightness. Asthma can vary in severity and may be triggered by various factors, including allergens, exercise, cold air, and respiratory infections.
-
What is its impact?
Asthma can significantly impact an individual’s quality of life. It can lead to frequent hospital visits, missed school or workdays, and limitations in physical activities. Severe asthma attacks can be life-threatening if not properly managed. The condition also imposes a substantial economic burden due to healthcare costs and lost productivity.
-
Local reports suggest that the prevalence of asthma is increasing, why is that?
The increasing prevalence of asthma can be attributed to several factors, including urbanization, environmental pollution, changes in lifestyle, and increased awareness and diagnosis of the condition. Urban environments often have higher levels of air pollution and allergens, which can contribute to the development and exacerbation of asthma.
-
Why is the prevalence increasing among Saudi children?
The rise in asthma prevalence among Saudi children may be linked to factors such as increased exposure to indoor allergens, changes in diet, sedentary lifestyles, and higher rates of obesity. Additionally, environmental factors such as dust storms and air pollution in certain regions of Saudi Arabia may contribute to the increase.
-
What is the Pathophysiology of Asthma?
The pathophysiology of asthma involves chronic inflammation of the airways, leading to hyperresponsiveness and obstruction. This inflammation is characterized by the infiltration of inflammatory cells, such as eosinophils and T-lymphocytes, into the airway walls. The release of inflammatory mediators causes bronchoconstriction, mucus production, and airway remodeling, resulting in the characteristic symptoms of asthma.
-
How to diagnose asthma?
Asthma is diagnosed based on a combination of clinical history, physical examination, and pulmonary function tests. Spirometry is commonly used to assess lung function and measure the reversibility of airway obstruction after bronchodilator administration. A detailed history of symptoms, triggers, and family history of asthma or allergies is also crucial in making a diagnosis.
-
What questions do you ask in the history?
- What are the specific symptoms you experience, and how often do they occur?
- Do you have any known triggers, such as allergens, exercise, or cold air?
- Have you experienced any recent respiratory infections?
- Is there a family history of asthma or other allergic conditions?
- Have you noticed any patterns or times when symptoms worsen?
- What medications are you currently taking, and have they been effective?
-
What conditions & medications worsen symptoms of asthma?
Conditions that can worsen asthma symptoms include respiratory infections, allergic rhinitis, gastroesophageal reflux disease (GERD), and sinusitis. Medications that may exacerbate asthma symptoms include nonsteroidal anti-inflammatory drugs (NSAIDs) and beta-blockers. It is important for individuals with asthma to be aware of these potential triggers and manage them appropriately.
-
What will you find in the physical examination?
During a physical examination of a patient with asthma, you may find signs such as wheezing on auscultation, prolonged expiration, and decreased breath sounds. In some cases, there may be signs of allergic rhinitis or eczema, which are commonly associated with asthma. However, the physical examination may be normal between asthma attacks.
Asthma Control and Management
- How to diagnose Asthma?
- Asthma is typically diagnosed based on a combination of medical history, physical examination, and lung function tests. Key diagnostic tools include spirometry, which measures the amount and speed of air a person can inhale and exhale, and peak flow monitoring. A detailed history of symptoms such as wheezing, coughing, shortness of breath, and chest tightness, particularly if they worsen at night or with exercise, can also aid in diagnosis.
- What are the medications used?
- Medications for asthma are generally categorized into two types: quick-relief (rescue) medications and long-term control medications. Quick-relief medications, such as short-acting beta-agonists (e.g., albuterol), are used to relieve acute symptoms. Long-term control medications, such as inhaled corticosteroids, long-acting beta-agonists, leukotriene modifiers, and biologics, are used to manage chronic symptoms and prevent asthma attacks.
- What are the long-term goals of asthma management?
- The long-term goals of asthma management include achieving and maintaining control of symptoms, maintaining normal activity levels, preventing asthma exacerbations, minimizing the need for quick-relief medications, and preventing lung function decline. Additionally, reducing the risk of adverse effects from asthma medications is also a key goal.
- What are the trigger factors?
- Common trigger factors for asthma include allergens (such as pollen, dust mites, mold, and pet dander), respiratory infections, physical activity, cold air, smoke (including tobacco smoke), air pollution, strong odors or fumes, stress, and certain medications (such as aspirin or nonsteroidal anti-inflammatory drugs). Identifying and avoiding these triggers can help in managing asthma effectively.
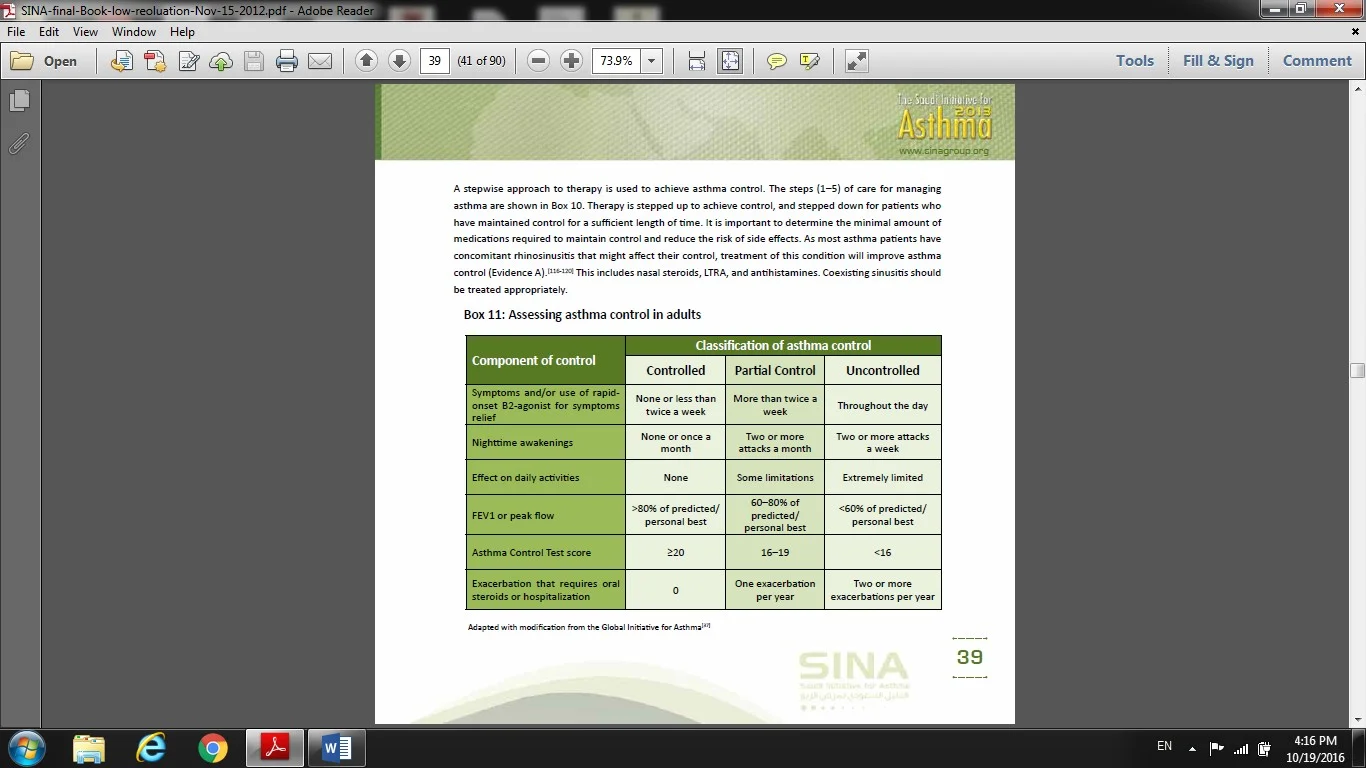
Assessing Asthma Control in Adults
| Component of Control | Controlled | Partial Control | Uncontrolled |
|---|---|---|---|
| Symptoms and/or use of rapid-onset B2-agonist for symptom relief | None or less than twice a week | More than twice a week | Throughout the day |
| Nighttime awakenings | None or once a month | Two or more attacks a month | Two or more attacks a week |
| Effect on daily activities | None | Some limitations | Extremely limited |
| FEV1 or peak flow | >80% of predicted/personal best | 60–80% of predicted/personal best | <60% of predicted/personal best |
| Asthma Control Test score | ≥20 | 16–19 | <16 |
| Exacerbation that requires oral steroids or hospitalization | 0 | One exacerbation per year | Two or more exacerbations per year |
- How to maintain control of Asthma?
To maintain control of asthma, it is important to follow a comprehensive asthma management plan, which includes:
- Regular monitoring of symptoms and lung function.
- Avoiding asthma triggers.
- Using prescribed medications correctly, including controller medications like inhaled corticosteroids and reliever medications like short-acting beta-agonists.
- Regular follow-up with a healthcare provider to adjust treatment as needed.
- Educating the patient about asthma and how to manage it effectively.
- If Asthma control is not achieved, which actions are recommended?
If asthma control is not achieved, the following actions are recommended:
- Review the patient’s adherence to the prescribed treatment plan.
- Ensure proper inhaler technique.
- Identify and manage any comorbid conditions or triggers.
- Consider stepping up the treatment according to asthma guidelines.
- Reassess the diagnosis to confirm it is asthma.
- Provide additional patient education and support.
- When referral to specialist is recommended?
Referral to a specialist is recommended in the following situations:
- When asthma control is not achieved despite optimal treatment.
- If there is uncertainty about the diagnosis.
- When the patient requires high-dose inhaled corticosteroids or frequent courses of oral corticosteroids.
- If there are significant side effects from medications.
- When additional testing or specialized treatments are needed.
- What treatment Steps in adult?
- Step 1: As-needed low-dose inhaled corticosteroid (ICS)-formoterol.
- Treatment at step 2: Daily low-dose ICS or as-needed low-dose ICS-formoterol.
- Treatment at step 3: Low-dose ICS-LABA (long-acting beta-agonist).
- Treatment at step 4: Medium-dose ICS-LABA.
- Treatment at step 5: High-dose ICS-LABA and consider add-on treatments like tiotropium or biologics.
- What should be considered for patients who require long-term systemic corticosteroids?
For patients who require long-term systemic corticosteroids, consider:
- Monitoring for potential side effects such as osteoporosis, hypertension, diabetes, and adrenal suppression.
- Using the lowest effective dose to minimize side effects.
- Considering alternative treatments or referral to a specialist to reduce the need for systemic corticosteroids.
- Implementing lifestyle modifications to mitigate side effects, such as calcium and vitamin D supplementation and regular exercise.
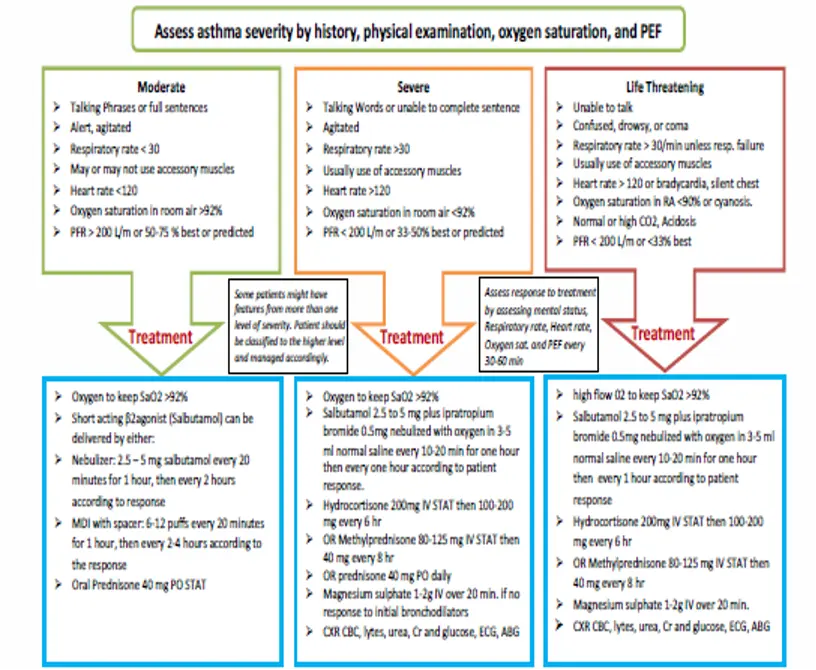
- How you manage acute asthma in adult?
To manage acute asthma in adults:
- Administer high-flow oxygen to maintain oxygen saturation above 92%.
- Use high-dose inhaled short-acting beta-agonists (SABA) via a nebulizer or metered-dose inhaler with a spacer.
- Administer systemic corticosteroids to reduce inflammation.
- Consider adding ipratropium bromide for severe exacerbations.
- Monitor the patient’s response to treatment and adjust as necessary.
- Provide continuous assessment and support, and consider hospitalization if there is no improvement.
- For whom ICU referral is recommended?
ICU referral is recommended for patients with:
- Severe asthma exacerbations not responding to initial treatment.
- Signs of respiratory failure or impending respiratory arrest.
- Decreased level of consciousness or confusion.
- Persistent hypoxemia or hypercapnia despite treatment.
- Need for mechanical ventilation or intensive monitoring.
- In outpatient management of asthma in children aged 5–11 years, according to SINA 2016.
- If the child is on short-acting beta agonist (prn) + low dose ICS and still not controlled, what is the best next option for him?
The best next option is to add a leukotriene receptor antagonist (LTRA) or increase the dose of inhaled corticosteroids.
- An adult patient known for bronchial asthma, came to the clinic on salbutamol inhaler + low medium dose of ICS & LABA, his ACT IS 17. During your assessment of the patient, he is adherent to treatment and taking the right dose. Decide to step up his treatment.
- Before you step up medication, which is another important factor to assess?
Before stepping up medication, it is important to assess the patient’s inhaler technique to ensure they are using the inhaler correctly and effectively.
Levels of severity of acute asthma exacerbations in adults