Acetaminophen Toxicity
Author: Fahad Abuguyan, MBBS, MBA, FRCPC Assistant Professor of Emergency Medicine
Table of Contents
Overview
Acetaminophen (paracetamol) is one of the most commonly used antipyretic and analgesic agents throughout the world. It is found as an isolated product or in combination with medications for the treatment of cold symptoms, pain, and headache.
Key Points:
- Widely available in both oral and IV formulations
- Toxicity is a concern in all intentional ingestions, repeated supratherapeutic dosing, and drug abuse
- Inhibits prostaglandin E2 (PGE2) synthesis, leading to antipyresis and analgesia
- Presents as a relatively silent clinical syndrome
- 18% of all unexplained liver failure is attributed to acetaminophen overdose
- One of the leading causes of hospital admission, antidote use, and fatalities from oral poisonings in the United States
Metabolism Overview:
- Rapid absorption within 1st hour
- Complete absorption within 4 hours
In acetaminophen overdoses, there are 3 primary goals:
- Determine the patient’s risk
- Perform diagnostic testing
- Administer the antidote
Principle of the Disease
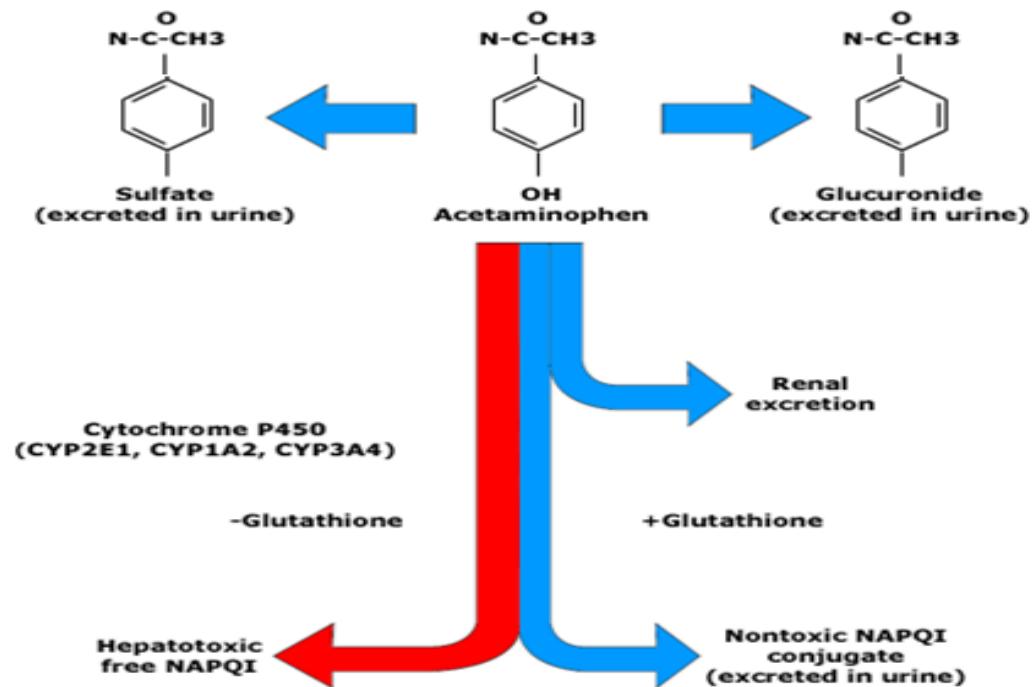
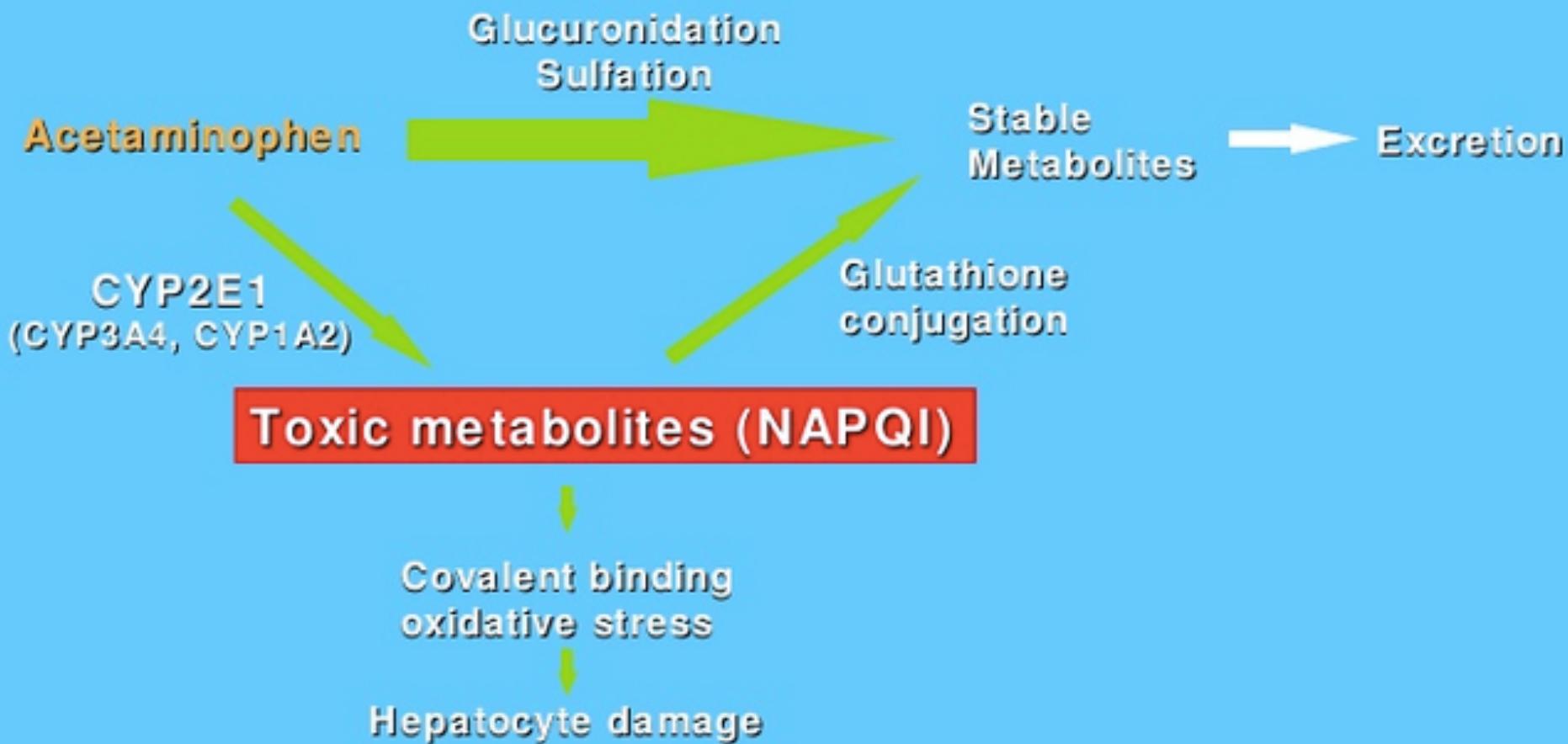
Acetaminophen Metabolism and Toxicity Mechanism
At Therapeutic Doses:
- 90% of acetaminophen is metabolized in the liver to sulfate and glucuronide conjugates, then excreted in the urine
- One-half of the remaining acetaminophen is excreted unchanged in the urine
- One-half is metabolized via hepatic cytochrome P450 to N-acetyl-p-benzoquinoneimine (NAPQI), which is hepatotoxic Z
With Normal Dose: NAPQI is rapidly conjugated to hepatic glutathione, forming nontoxic metabolite compounds that are excreted in the urine.
With Toxic Doses: Z
- The sulfate and glucuronide pathways become saturated
- Increased fraction of acetaminophen is metabolized by cytochrome P450 enzymes
- Once glutathione stores are depleted, NAPQI begins to accumulate and hepatic injury ensues
Metabolic Pathways
metabolism acetaminophen
Clinical Features
Types of Ingestion
Acute Ingestion
- Definition: Single ingestion or a series of ingestions occurring within 8 hours
- Toxic Dose: 10 gram in total or 150 mg/kg Z
Diagnosis
Acetaminophen toxicity should be considered in any patient with drug overdose.
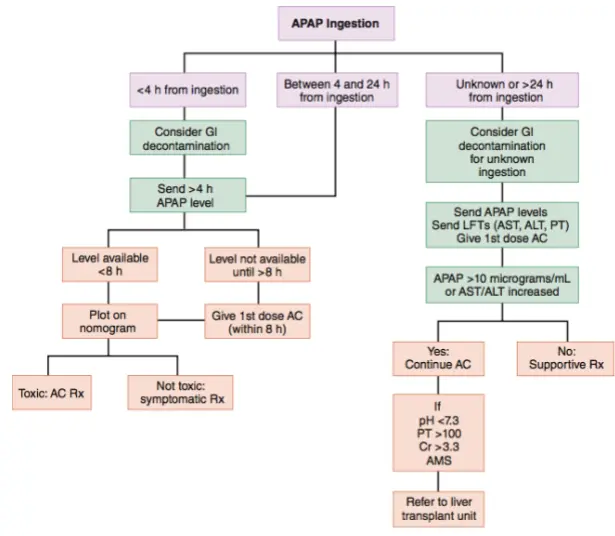
In acetaminophen overdose, there are 3 primary goals:
- Determine the patient’s risk
- Perform diagnostic testing
- Administer the antidote
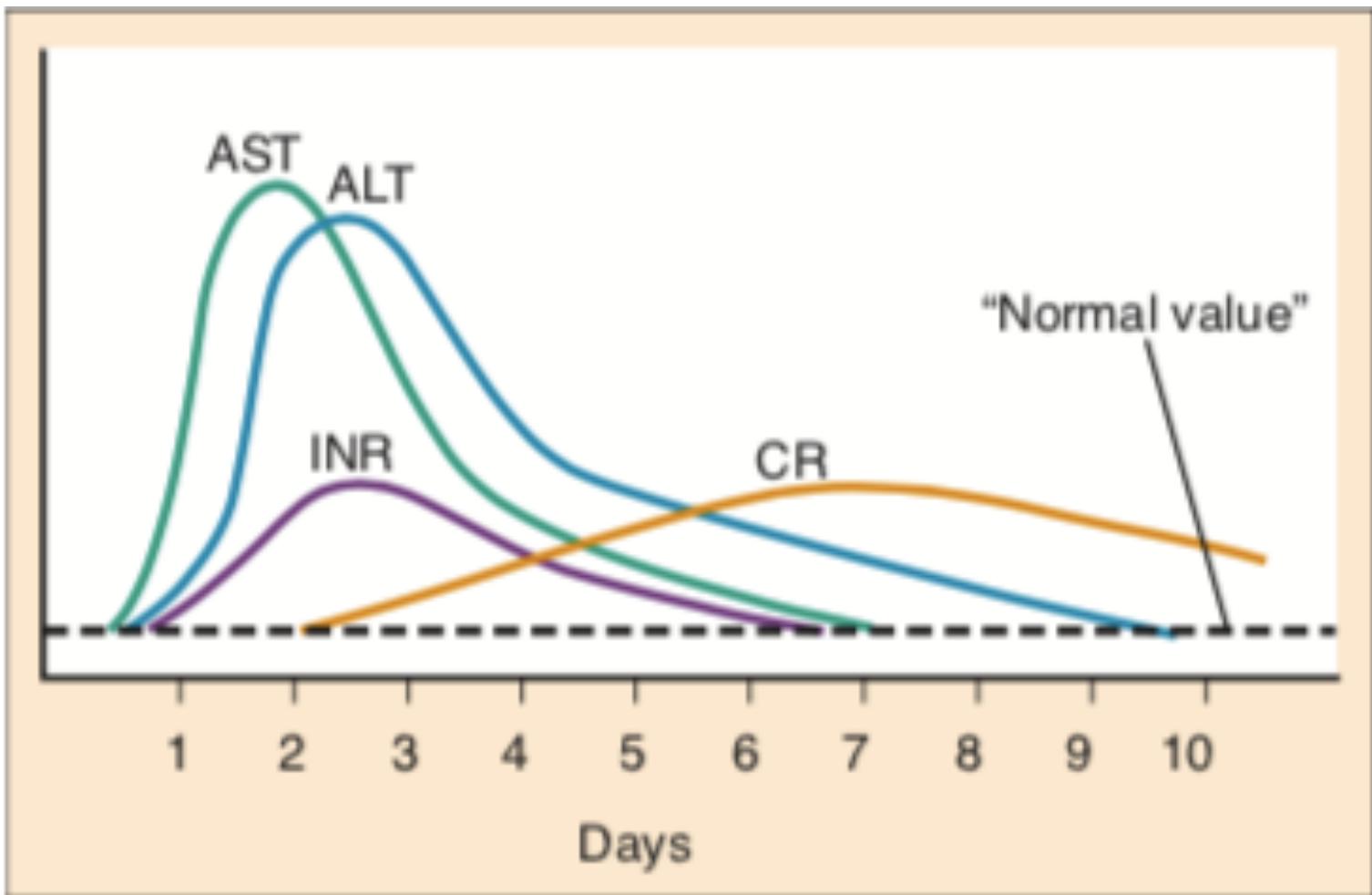
Time Course and Clinical Stages of Acetaminophen Toxicity
| STAGE | TIME COURSE | NAME | SYMPTOMS | SIGNS |
|---|---|---|---|---|
| 1 | 0 to 12 (up to 24 to 36) hours | Preinjury | Nausea, vomiting, anorexia, malaise | Elevated serum acetaminophen concentration |
| 2 | 8 to 36 hours | Liver injury | Nausea, vomiting, RUQ abdominal tenderness | Aminotransferase elevation (AST begins to rise 8 to 36 hours after ingestion) |
| 3 | 2 to 4 days | Maximum liver injury | Liver failure (encephalopathy, coagulopathy, hemorrhage, acidosis) | Hemorrhage, ARDS, sepsis/SIRS, multiorgan failure, cerebral edema |
| 4 | >4 days | Recovery | None | Complete hepatic histologic recovery |
- Oral acetaminophen is completely absorbed by 4 hours post ingestion (assuming single ingestion).
- NAC should be initiated within 8 hours (no harm delaying up until 8 hours)
- AST is the first transaminase to start rising in acetaminophen OD.
- AST will be elevated by 36hrs post ingestion if it will rise at all.
In acetaminophen overdose there are 3 goals:
- Determine the patient’s risk.
- Diagnostic testing.
- Give the antidote.
History:
The amount
- 150mg/kg
The time since ingestions
- 4 hours
- 8 hours
Laboratory :
- CBC
- U&Es
- LFTs
- VBG
- Serum level
- PT/INR, PTT
LFTs:
- AST is the first enzyme to rise.
- Alanine transaminase (ALT), prothrombin time, and bilirubin typically begin to rise and peak shortly after AST values.
- With severe toxicity, AST, ALT, and the prothrombin time may all be elevated within 24 hours.
Serum level:
- Serum acetaminophen concentration 4 hours after ingestion or as soon as possible after 4 hours.
- After a typical therapeutic dose of acetaminophen, serum acetaminophen concentration peaks below 30 and is less than 10 at 4 hours.
The serum acetaminophen concentration
and the time of ingestion determine the
need for antidote therapy
Severity of acetaminophen intoxication
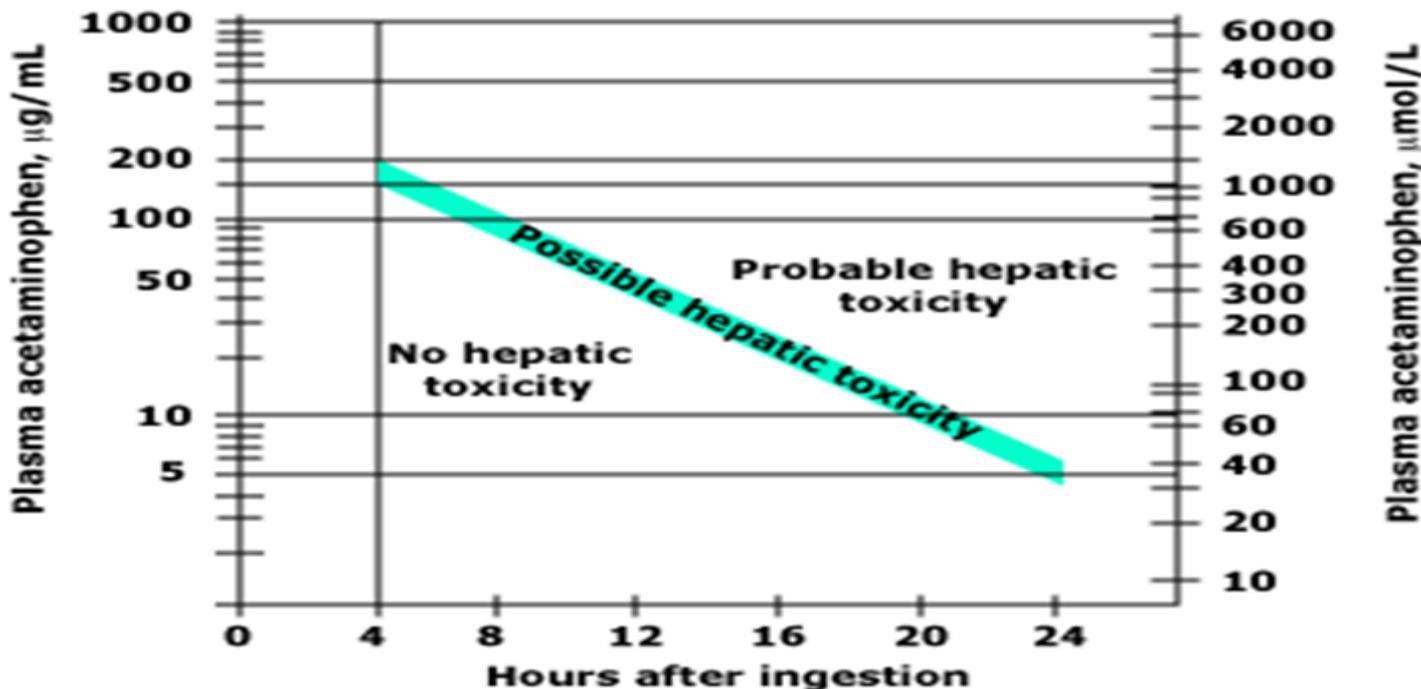
The Rumack-Matthews nomogram summarizes the relationship between plasma acetaminophen concentration (in or ), the time after drug ingestion, and the risk of hepatic toxicity. The thick diagonal line of possible hepatic toxicity represents a 25 percent likelihood of disease. A relatively low level (such as 10 ) is safe soon after ingestion, but associated with appreciable risk at 24 hours since it reflects a high initial load which has now distributed into the tissues.
Adapted from Rumack, BH, Matthews, H, Pediatrics 1975; 55:873.
Acetaminophen poisoning nomogram
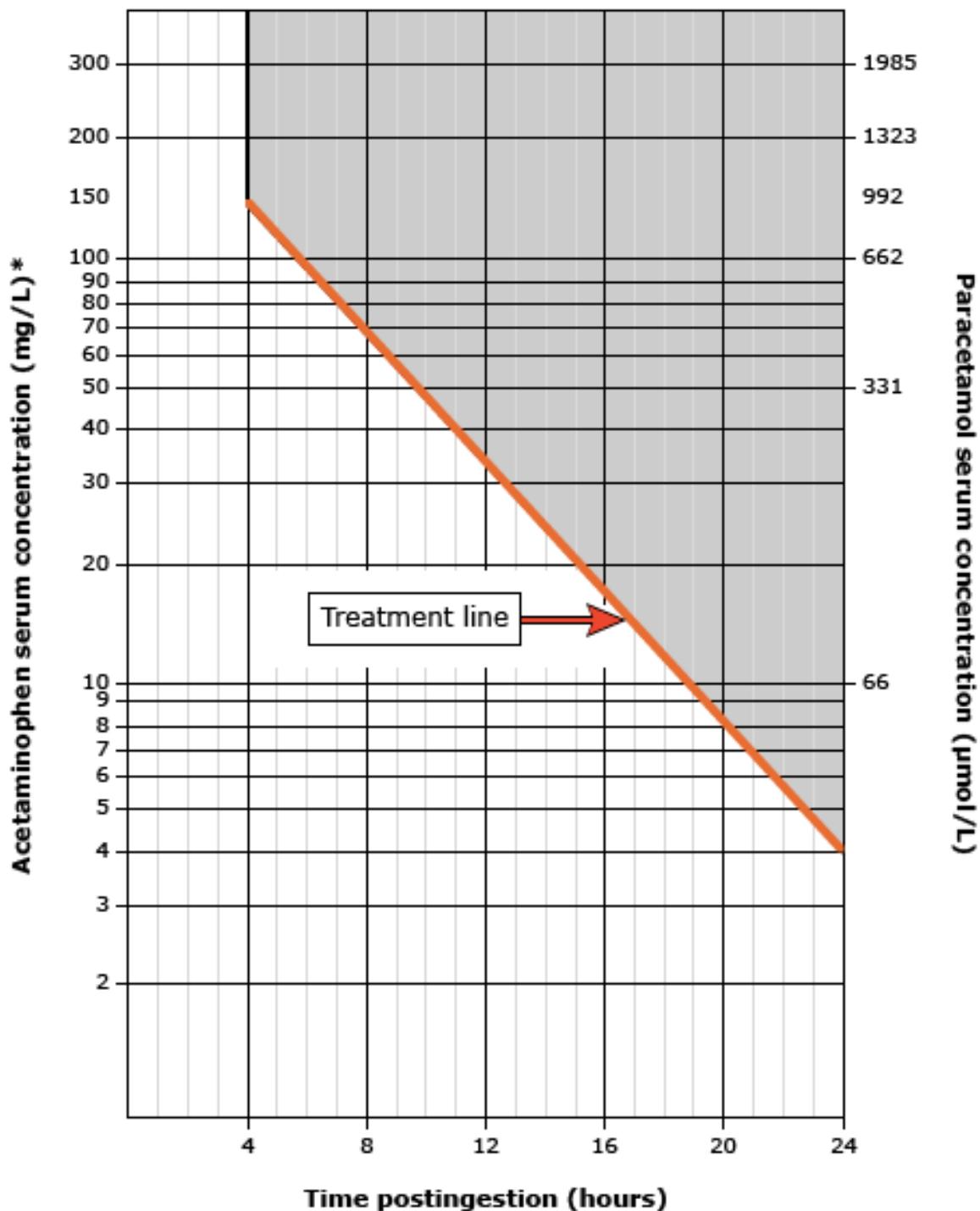
- Measurement of serum acetaminophen concentration before 4 hours is typically not necessary.
- There is little need to treat patients before 6 to 8 hours after ingestion.
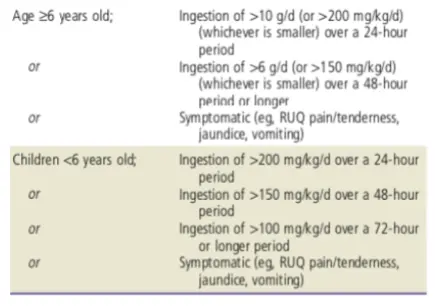
Chronic Ingestion:
- Risk assessment is more complex, and the treatment nomogram cannot be used.
- Determination of the need for NAC is based on assessment of the risk for hepatotoxicity and measurement of serum levels of acetaminophen and AST.
- Patients with chronic ingestions may benefit from antidotal therapy if they have evidence of liver injury (AST normal, or 120 IU/L) or if they have evidence of acetaminophen excess (serum acetaminophen mcg/mL)
Indications for Initiating Testing for Serum Acetaminophen Concentration and Aspartate Transaminase in Chronic Acetaminophen Ingestions
Management
The mainstay of management is to provide supportive care and to initiate NAC (N-Acetylcysteine) therapy when it is indicated.
Initial Management
Gastric Decontamination
- Usually not needed in most cases
- Activated Charcoal 50g can be used within 1 hour of ingestion unless contraindicated (e.g., sedated, not protecting airway)
N-Acetylcysteine (NAC) Therapy
Key Principles
- When indicated, NAC should be administered as early as possible
- Delay of NAC administration for more than 8 hours after ingestion significantly increases the risk of hepatotoxicity
Mechanisms of Action
- Increased glutathione availability
- Direct binding of NAPQI
- Reduction of NAPQI back to acetaminophen
Indications for NAC Therapy
For Acute Ingestion:
- Serum levels of ≥150 mcg/mL or higher
- Serum levels above the treatment line in nomogram
- Serum levels will not be back within 8 hours
- Serum levels >10 mcg/mL with unknown ingestion time
For Chronic Ingestion:
- Symptomatic regardless of APAP level
- Elevated AST (>2× upper limit normal or above 120 IU/L)
- Elevated APAP >30 mcg/mL
Role of Early NAC Administration
The main role of early NAC administration is to: Prevent hepatotoxicity by detoxifying NAPQI and decreasing NAPQI production
Critical Time Window: The risk of hepatotoxicity does not significantly increase unless NAC is delayed for 8 hours or longer after ingestion.
NAC Administration Protocols
NAC can be administered by the oral (PO) or IV route, with advantages and disadvantages for each. All formulations of NAC (PO and IV) are effective when they are started within 8 hours of ingestion.
NAC Treatment Protocols
| Route | Dosage Regimen |
|---|---|
| Oral (PO) | Loading dose: 140 mg/kg × 1 dose Maintenance: 70 mg/kg every 4 hours × 17 doses |
| IV | For treatment within 8 hours of ingestion: • Initial bolus: 150 mg/kg IV over 1 hour • Infusion: 12.5 mg/kg/hr over the next 4 hours • Then: 6.25 mg/kg/hr over the next 16 hours For treatment >8 hours after ingestion, chronic ingestions, and for those with hepatic failure: • Infusion: 12.5 mg/kg/hr over 48 hours |
Abbreviations: IV, intravenous; NAC, N-acetylcysteine.
NAC Side Effects
| NAC Formulation | Common Side Effects | Severe Side Effects |
|---|---|---|
| PO NAC | Vomiting (23%)¹⁵² | Very rare |
| IV NAC | Mild anaphylactoid reactions (e.g., rash, flushing, pruritus, vomiting), 2-18%¹⁴⁶⁻⁴⁹,⁵³ | Severe anaphylactoid reactions (e.g., hypotension), <1%¹⁴³,⁴⁶⁻⁴⁹ |
Treatment Algorithm
Supportive Care
Supportive care includes management of:
- Co-ingestions (other toxic substances)
- Nausea and vomiting related to acetaminophen poisoning
- Hepatic injury monitoring and support
- Renal dysfunction related to acetaminophen toxicity