Overall Assessment
- Category 1 – no risk
- Category II – intermediate risk (Most problamatic)
- Category III – HIGH RISK (rapid C/S or immediate vaginal delivery)
Category I
7 m
:Include all of the following
- Baseline rate:110–160 beats/minute-
- Baseline FHR variability: moderate
- Late or variable decelerations: absent
- Early decelerations: present or absent-
- Accelerations: present or absent -
 Nonreactive and reactive is cat 1 without stimulation
Nonreactive and reactive is cat 1 without stimulation
Category II
FHR tracings include any of the following: Tachycardia
- Baseline FHR with Absent or minimal or marked variability
- Absence induced Accelerations after fetal stimulation
- Recurrent (late or variable) decelerations with moderate variability
 After stimulation no reaction is not reassuring and is
cat 2
After stimulation no reaction is not reassuring and is
cat 2
Category III
Category III FHR tracings include either Absent baseline FHR variability and :any of the following
- Recurrent late decelerations
- Recurrent variable decelerations
- Bradycardia
- Sinusoidal pattern
Management
CTG is Normal/Reassuring/Category 1
- Healthy fetus -
- Continue CTG and normal care ---
Non-Reassuring/Category 2
10 s Think about possible underlying causes.
If the baseline fetal heart rate is over 160 beats/minute, check the woman’s temperature and pulse. If either are raised, offer fluids and paracetamol.
Noninvasive Management
- A left-lateral position, rule out cord prolapse
- Give O2 to mother
- Offer oral or intravenous fluids
- Discontinue oxytocin until the FHR and uterine activity become normal.
- Vibroacoustic stimulation (VAS) or fetal scalp stimulation (if reduce variability and or no acceleration)
- Tocolytic agents: Beta-adrenergic agonists (e.g., terbutaline, subcutaneously can be administered to decrease uterine activity in the presence of uterine tachysystole).
- Inform coordinating midwife and obstetrician.
Invasive Management
- Amniotomy: If the FHR cannot be monitored adequately externally, an amniotomy should be performed to place internal monitors.
- Fetal scalp electrode (FSE)
- contraindicated in cases of fetal coagulopathy or maternal infections such as HIV, active herpes simplex virus, and hepatitis (B or C). Z
Fetal Scalp Blood pH
(More accurate) Determination of fetal scalp blood pH can clarify the acid-base state of the fetus
- A pH value of 7.25 or higher is normal-
- A pH range of 7.20 to 7.24 is a borderline repeat in 30 minute
- A pH of <7.20 on two measurements 5 to 10-minutes apart may indicate sufficient fetal acidosis to warrant immediate delivery
Category 3 is Abnormal Indicates Need for Urgent Intervention - delivery
Case Studies
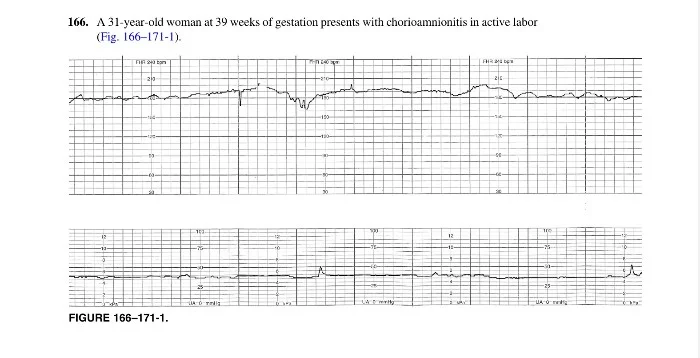
166. A 31-year-old woman at 39 weeks of gestation presents with chorioamnionitis in active labor
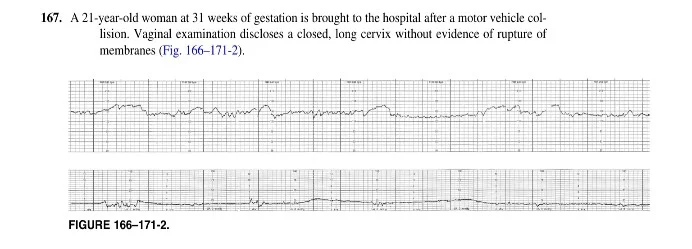
167. A 21-year-old woman at 31 weeks of gestation is brought to the hospital after a motor vehicle collision
168. A 39-year-old woman at 41 weeks of gestation is completely dilated and effaced and pushing with contractions
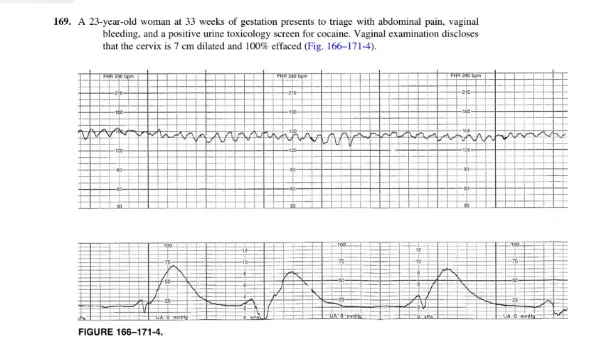
169. A 23-year-old woman at 33 weeks of gestation presents to triage with abdominal pain, vaginal bleeding, and a positive urine toxicology screen for cocaine
abruptio placentea
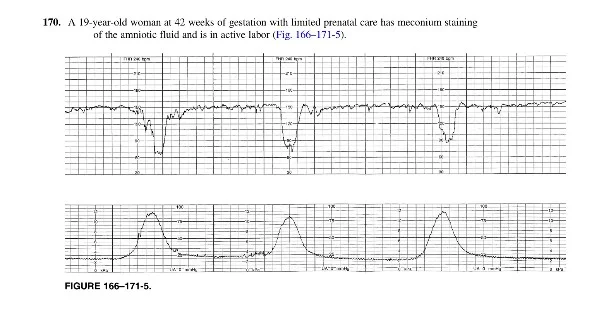
170. A 19-year-old woman at 42 weeks of gestation with limited prenatal care has meconium staining of the amniotic fluid and is in active labor
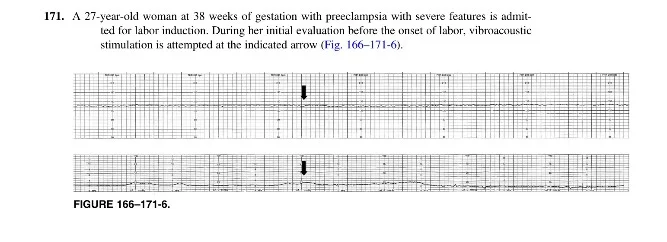
171. A 27-year-old woman at 38 weeks of gestation with preeclampsia with severe features is admitted for labor induction
Non-reactive