Osteoarthritis (OA)
Yousef T. Khoja
OBJECTIVES
- Identify the osteoarthritis and its predisposing factors.
- Specify the signs and symptoms of osteoarthritis.
- Assess osteoarthritic patient with appropriate investigation.
- Outline the principles of management of an osteoarthritic patient.
OUTLINE
- Definition
- Epidemiology
- Classification
- Pathogenesis
- Pathophysiology
- Management
- Presentation
- Investigations
- Treatment
DEFINITION
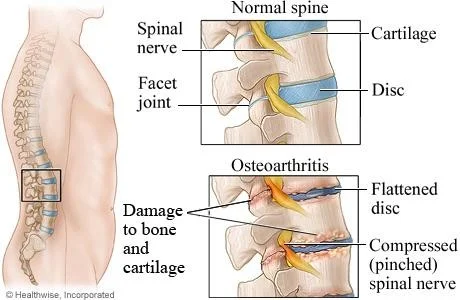
- Degenerative (non-inflammatory) disease of synovial joints that causes slow progressive loss of articular cartilage and proliferative changes of surrounding bones
- Known by many different names including Degenerative Joint Disease, Osteoarthrosis, Hypertrophic Arthritis and Degenerative Arthritis.
- No joint ankylosis is observed
EPIDEMIOLOGY
- Most common joint disease
- Leading to disability & functional loss.
- Under the age of 45, male > females. After that age, it is more common in women.
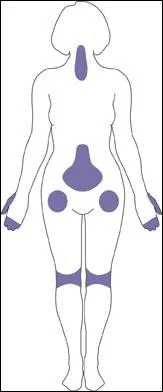
- Most commonly affecting joint: 1st CMCJ, IPJ, cervical spine, Lumber spine, Hips, Knees & 1st MTPJ.
- OA of the knee joint is found in 70% of the population over 60 years of age


CLASSIFICATION
- Primary
- Unknown Etiology
- Secondary
- Known Etiology
CLASSIFICATION
- Risk factors for Primary OA:
- Age
- Sex
- Genetics
CLASSIFICATION
- Conditions may cause Secondary OA:
- Obesity
- Trauma: Osteochondral defect, Malunion, Sport injury
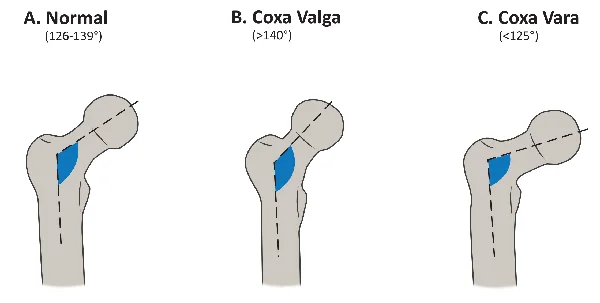
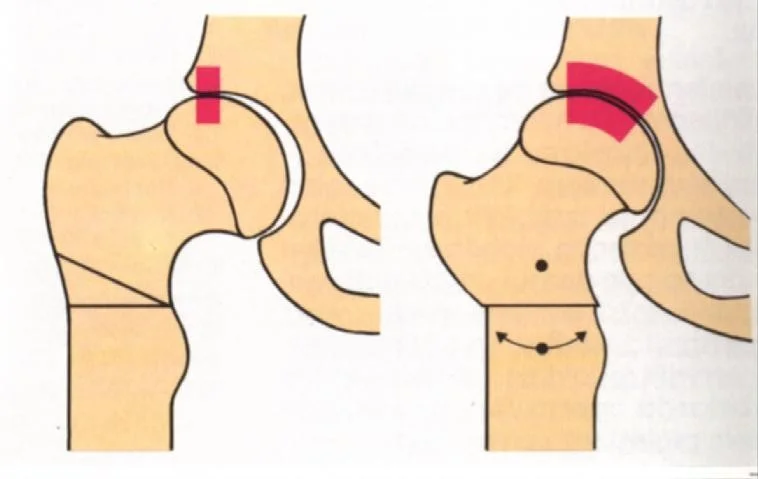
- Congenital/developmental: DDH or other Dysplasia
- Infection: Septic arthritis, Brucella, TB
- Necrosis: Perth`s disease, osteonecrosis, steroids
- Hematological: SCD or hemophilia
- Endocrine: DM or acromegaly
- Metabolic: Gout, Pseudogout or Paget disease
- Inflammatory joint disease
- Neuropathic: DM or syphilis
- Occupation: daily repetitive trauma
PATHOGENESIS
- Modifiable:
- Over-weight
- Trauma
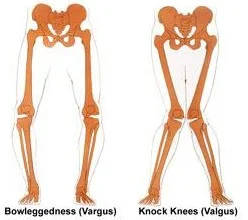
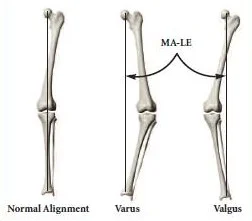
- Articular alignment
- Occupation or Overuse of joint
- Muscle weakness
Metabolic syndrome: - Central obesity, - Dyslipidemia, - High blood pressure, - Elevated fasting glucose levels
Non-modifiable:
- Gender
- Females > Males
- Increased age
- Genetics / heredity
- Race
- African American males < whites and Hispanics
Systemic factors
- Age
- Sex
- Ethnic characteristics
Bone density
- Estrogen replacement therapy (in post-menopausal women)
- Nutritional factors (?)
- Genetics
Other systemic factors
Flow: → Susceptibility to osteoarthritis → Local biomechanical factors
- Obesity
- Joint injury
- Joint deformity
- Sports participation
- Muscle weakness → Site and severity of osteoarthritis


PATHOPHYSIOLOGY
- Structure of joint cartilage:
- Hyaline cartilage is Avascular, Aneural and Alymphatic
- Receives nutrients and oxygen from synovial fluid via diffusion
- Composition of cartilage:
- Water (75% of wet weight)
- For nutrition and lubrication
- Collagen esp., type II (15% of wet weight)
- Provides stiffness
- Proteoglycans (10%)
- Provides elastic strength
- Chondrocytes (1-5%): the only cell of cartilage
- Non-collagenous proteins
- Water (75% of wet weight)
Changes
- Molecular Changes
- Biochemical Changes
- Histologic & Macroscopic Changes
Molecular Changes:

Biochemical Changes:
- Water content increase
- Proteoglycans amount decrease but synthesis increase
- Collagen organization & orientation are lost
- Chondrocyte amount & size remain the same
- Elasticity decrease
| Aging | Osteoarthritis | |
|---|---|---|
| Water Content | Decreased | Increased |
| Collagen | Same | Disorganized |
| Proteoglycan Content | Decreased | Decreased |
| Proteoglycan Synthesis | Same | Increased |
| Chondrocyte Size | Increased | Same |
| Chondrocyte Number | Decreased | Same |
| Modulus of Elasticity | Increased | Decreased |
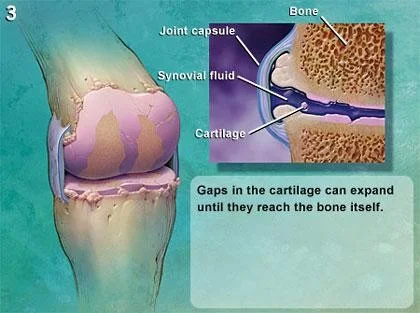
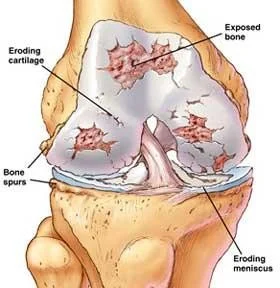
Histologic & Macroscopic Changes:
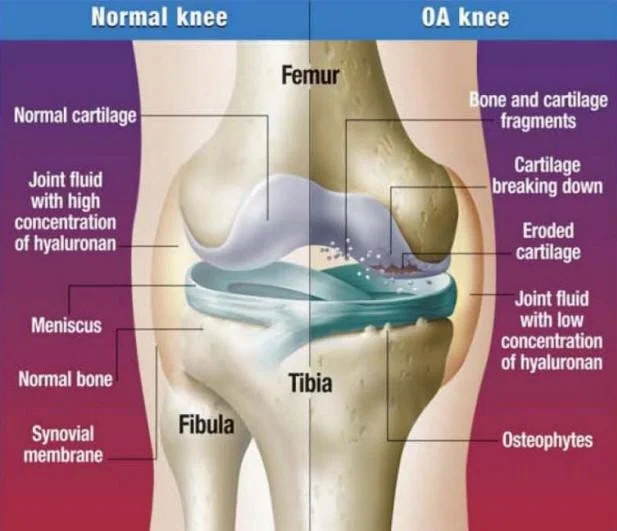
- Fibrillation & softening on weight bearing surfaces
- Loss of cartilage height → bone exposed → Decrease Joint Space
- Attempt of remodeling → Subchondral Sclerosis & Eburnation
- Fissuring → synovial fluid into subchondral bone → Subchondral Cyst
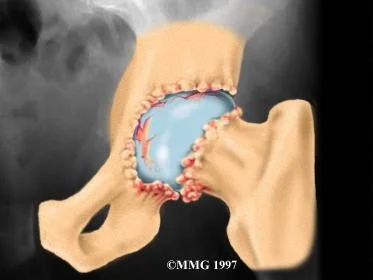
- Hypervascular synovium & subchondral bone → proliferation of adjacent cartilage → enchondral ossification → Osteophyte
- Synovial & capsular thickening
Histologic & Macroscopic Changes:
- Progressive bone erosion → Bone Collapse
- Loss of height & ligamentous laxity → Malalignment
- Fragmented osteophyte → Loose Bodies
In a normal joint, healthy cartilage, lubricated by synovial fluid, cushions the bones and allows them to move easily.
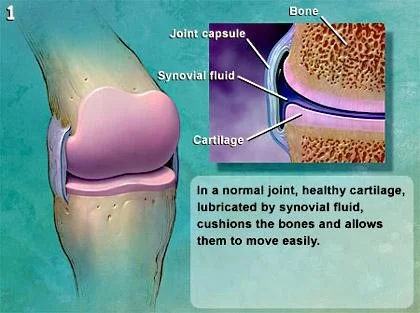
- Osteoarthritis causes the cartilage to begin breaking down, first making it thinner and then creating cracks in its surface.
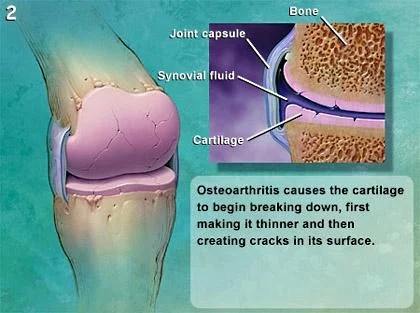
- Gaps in the cartilage can expand until they reach the bone itself.
- Synovial fluid leaks into cracks which can form in the bone’s surface when this replacement cartilage wears away. This causes further damage and in some cases can lead to cysts in the bone or other deformities.
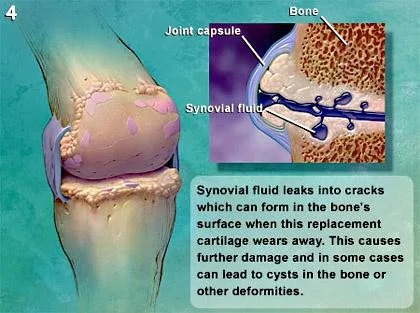
- If not treated, damage can progress to the point where the bones in the joint become seriously and permanently deformed.



THE VICIOUS CYCLE OF OA
- JOINT PAIN ⇒
- Reduced Mobility & Activity ⇒
- Weak Muscle ⇒
- Obesity ⇒
- Diabetes
- Depression
- Hypertension
- Increase Stress ⇒
- Cartilage Damage ⇒
- Synovitis ⇒
- JOINT PAIN ⇒
Management
-
Presentation
- History
- Physical Examination
-
Investigations
- Radiology
- Laboratory
- Arthrocentesis
-
Treatment
- Conservative
- Operative
History
Presentation
- History:
- Age & Gender
- Pain
- Stiffness & Limitation of ROM
- Deformity
- Swelling
- Functional limitation
- Crepitation
- Treatment History
Presentation
-
Physical Examination:
-
Weight, Height & BMI
-
Look
- Body habitus
- Gait
- Limb alignment
- Effusion
- Skin: scars, redness …
-
Feel
- Joint line tenderness
- Warmth
- Muscle strength
-
Range of motion
-
Special test
-
Distal N.V. examination
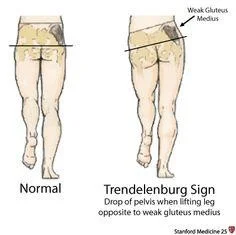
- Hip:
- Pain in Groin and Buttock
- Referred Pain in Knee and side of thigh
- Start-up pain or mechanical
- Antalgic or Trendelenburg gait
- Fixed Flexion Deformity:
- Thomas test
-
Normal
-
Trendelenburg Sign
- Drop of pelvis when lifting leg opposite to weak gluteus medius
-
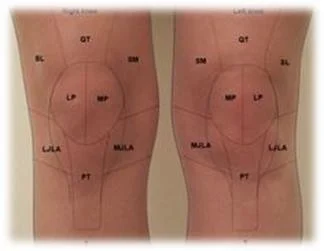
Knee:
- Pain when moving the Knee
- Catching when moving
- Pain when taking the Stairs or getting up from a Chair
- Weakened Thigh muscles
- Deformity
- Spine:
- Stiffness and Pain in the Neck and Lower Back
- Radiculopathy pain
- Weakness or Numbness
- Myelopathic symptoms
- Red Flags symptoms

Investigations
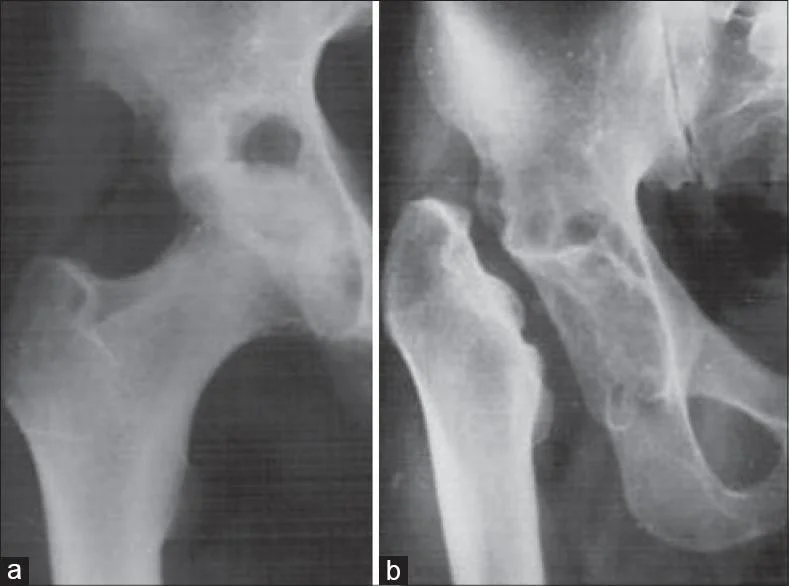
- Xray:
- AP & Lateral Weight-bearing views
- Pelvis:
- Standing AP pelvis
- Knee
- Sunrise / skyline
- PA view in 45 of flexion (Rosenberg view)



- Findings:
- Joint space narrowing
- Osteophytes formation
- Subchondral sclerosis
- Subchondral cysts
- loose bodies
- Deformity
Grading of Osteoarthritis
Kellgren-Lawrence (KL) grading scale

Radiographic Grading
The radiographic grading of osteoarthritis (OA) is as follows:
Grade 0 – No OA
Grade 1 – Doubtful OA
- Doubtful joint space narrowing, possible osteophytic lipping
Grade 2 – Mild OA
- Definite osteophytes, definite narrowing of joint space
Grade 3 – Moderate OA
- Moderate, multiple osteophytes, narrowing of joint, sclerosis and possible deformity of bone contour
Grade 4 – Severe OA
- Large osteophytes, marked narrowing of joint space, severe sclerosis and deformity of bone contour

-
CT scan:
- Pre-OP planning especially if there is bone loss
-
MRI:
- Rule out other differentials
-
Laboratory:
- No pathognomonic laboratory findings for OA
- To exclude secondary causes
-
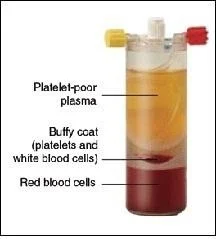
Arthrocentesis (Joint Aspiration)
-
Aspirate synovial fluid for analysis.
-
In OA:
- Clear fluid
- WBC <2000/mm3
- Normal viscosity
-
To exclude secondary causes


| Normal | Noninflammatory | Inflammatory | Septic | |
|---|---|---|---|---|
| Clarity | Transparent | Transparent | Cloudy | Cloudy |
| Color | Clear | Yellow | Yellow | Yellow |
| WBC/mL | <200 | <200-2000 | 200-50,000 | >50,000 |
| PMNs (%) | <25% | <25% | >50% | >50% |
| Culture | Negative | Negative | Negative | >50% positive |
| Crystals | None | None | Multiple or none | None |
| Associated conditions | — | Osteoarthritis, trauma | Gout, pseudogout, spondyloarthropathies, rheumatoid arthritis, Lyme disease, systemic lupus erythematosus | Nongonococcal or gonococcal septic arthritis |
Management
Treatment
- No known cure for OA
- Aims of Treatment:
- Slow Disease progression
- Control Pain
- Improve Joint Function
- Restore lifestyle
- Maintain Normal Body Weight
Education, Physio, Weight Loss & NSAIDs → Intra-articular Injection → Corrective Surgery or Arthroscopy → Arthroplasty
Conservative Treatment
-
Non-Pharmacological:
-
Patient Education RR
-
Weight loss programs
- symptomatic OA and BMI > 25
- Diet & low-impact aerobic
-
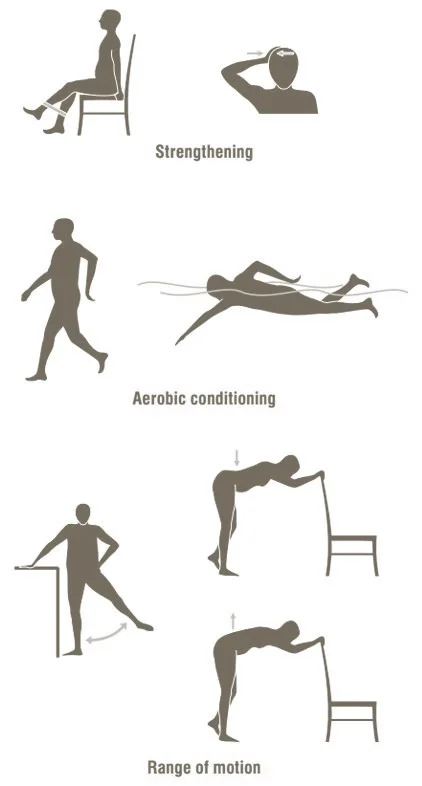
Physical Therapy
- Supervised exercises & home program
- ROM, Muscle strengthening & Prevent stiffness
-
Orthotics
- Splints & Braces
- Walking Aids
- Insoles
-
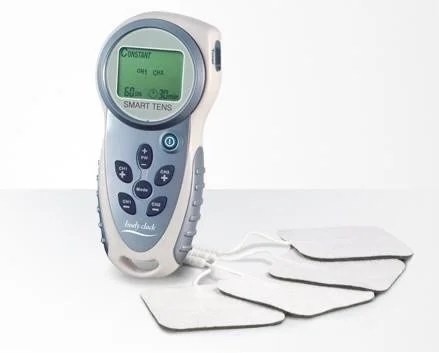
Other:
- Transcutaneous electrical nerve stimulation (TENS)
- Hot & Cold compression
- Acupuncture
- needle lavage



Pharmacological Treatment
-
Topical analgesics
-
Paracetamol:
- Not effective alone
- Caution in liver disease patients
-
NSAIDs
- Risks for GI & CVS.
- Monitor renal profile regularly
-
Glucosamine and chondroitin
- No strong evidence
- ? Placebo effect (20-30%)
-
Opioid
- Codeine + Paracetamol: Nausea, vomiting, dizziness and constipation
- Tramadol:
- Inhibits reuptake of serotonin & noradrenaline
- Contraindicated
- Seizure disorders
- Combination with selective serotonin reuptake inhibitors (risk of serotoninergic syndrome)
-
Intra-articular Injections: Corticosteroid injections:
- Short acting pain relief.
- Therapeutic and diagnostic
- Side effect:
- Flushing (40%)
- post-injection hyperglycaemia
- Infection (rare)

Advanced Pharmacological Interventions
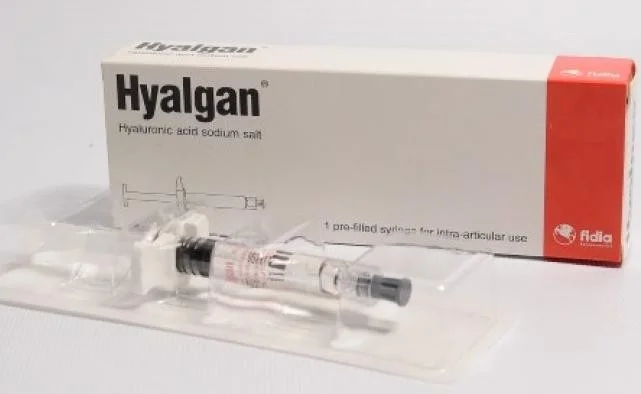
- Viscosupplementation (Hyaluronic acid) Injections:
- To improve elasticity and viscosity of synovial fluids.
- ? Placebo effect
- Platelet Rich Plasma (PRP) injection
- Stem Cell injection
Summary of Pharmacological Treatments
| Group of Drugs | Examples |
|---|---|
| Topical Analgesics | Deep heat, Methylsalicylate, NSAIDs |
| Analgesics | Acetaminophen, Hydrochloride, Tramadol |
| NSAIDs | Aspirin, Ibuprofen, Ketoprofen, Naproxen, Meloxicam |
| Cox-2 Drugs | Celecoxib |
| Corticosteroids | Injectable Glucocorticoids |
| Viscosupplements | Hyaluronic Acid Substitutes: Synvisc, Hyalgan |
Operative Treatment
Indications and Types
- Operative:
- Indication:
- Severe joint pain
- Functional Disabilities
- Deformity, angular deviations or instability
- Types:
- Arthroscopy debridement
- Corrective Osteotomy
- Arthroplasty
- Arthrodesis
Types
Arthroscopy debridement:
- Controversial
- Evidence of meniscus & labral degenerative tear
- No deformity


Corrective Osteotomy
- Realign axis & Redistribute weight bearing
- Indication:
- young patients with mild to moderate OA
- Thin & active with mobile joint
- Knee
- Valgus producing proximal tibial osteotomy
- Hip
- Valgus producing proximal femur osteotomy

Arthroplasty:
- Joint replacement
- Partial
- Total
- Resection
Partial Arthroplasty:
- Remove the articular surface to facilitate movements
- Indicated:
- Older (>60), lower-demand and thin (<82 kg) patients.
- Contraindication:
- Inflammatory arthritis
- Infected joint
- Bone stock deficiency
- Stiff joint & Abnormal geometry
- Used:
- Hip, knee & Shoulder.


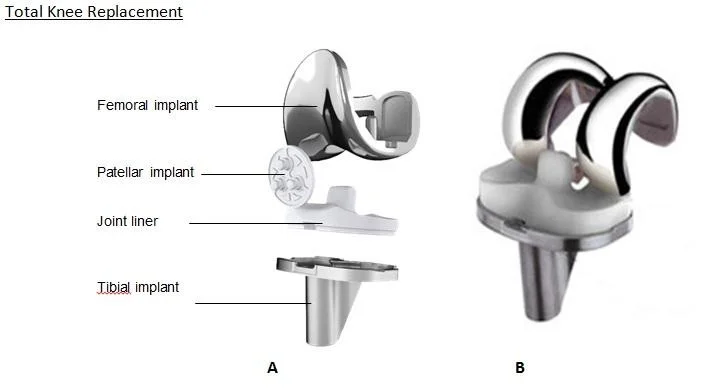
Total Joint Arthroplasty:
-
Replacing the native joint with prosthesis
-
Indicated:
- Old patient with deformed, stiff & painful joint.
-
Contraindication:
- Young active patients
- Infected joint
- Neuropathic joint
-
Used:
- All joints.


![]()

Resection Arthroplasty:
- Remove the articular surface to facilitate movements
- Indicated:
- Old non-ambulatory patient, poor bone and soft tissue quality, Medically unfit & failed multiple reimplantation.
- Contraindication:
- Young active patients
- Disadvantages:
- Short limb, weak muscle, poor function
- Used:
- Hip, Hand & Foot.
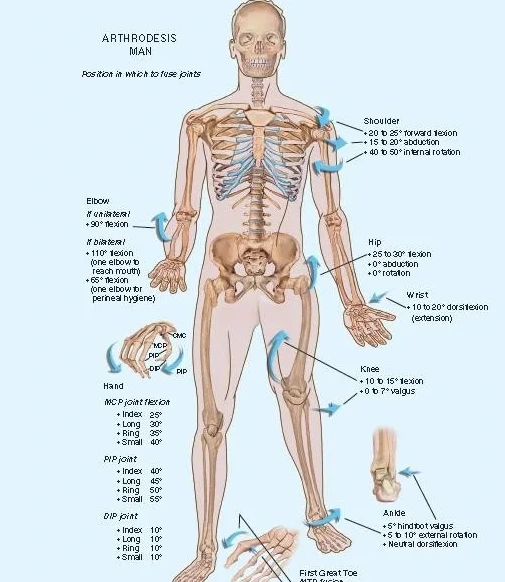
Arthrodesis / Fusion
- Arthrodesis / Fusion:
- Stabilizing the joint to make it painless
- Indicated:
- Loss of key muscles, Painful ankylosed joint in young patient, Failed previous total joint arthroplasty
- Contraindication:
- Active infection
- Adjacent joint or contralateral joint OA
- Used:
- Hand, Elbow, Shoulder, Spine, Ankle & foot
- Less likely in Hip & knee

References
- Apley’s System of Orthopaedics and Fractures, 9th ed.
- Miller’s Review of Orthopaedics 7th Ed.
- AAOS Comprehensive Orthopaedic Review, 1st ed.
- AAOS guideline.
- Orthobullets.com
- Emedicine.com
- Dr. Al-khawashki’s website