IM
Secondary Headaches
- Intracranial disease: (meningitis, brain hemorrhage, brain tumor)
- Eye diseases: (vision problems are the commonest)
- Sinusitis
- Temporal arteritis: (inflammation of the temporal artery)
- Head trauma
- Systemic diseases: (HTN)
FM
Urgent Considerations
Meningitis
- Presents with fever, headache, stiff neck.
- Patients may develop meningococcal sepsis, presenting with hypotension, altered mental state, and purpuric or petechial rash.
- Patients should have a lumbar puncture (LP) within 1 hour of arrival at hospital, provided it is safe to do so, and commence antibiotic treatment immediately afterwards.
- If high suspicion, antibiotics should be administered empirically before LP.
- If LP is delayed for CT, blood cultures should be obtained and broad-spectrum antibiotics given before CT.
Subarachnoid Haemorrhage (SAH) Z
- About 1% of all patients presenting to the emergency department with headaches have SAH.
- It may present with a ‘thunderclap’ headache (sudden onset of severe headache, seen in 12% of SAH).
Sudden onset, worst headache of life
- Immediate CT
Hypertensive Encephalopathy
- Elevated BP, mean arterial pressure >150 to 200 mmHg
- Immediate CT
- BP should be quickly lowered by 20% to 25% (labetalol, nicardipine).
Giant Cell Arteritis
- Patient >50 years, with their first severe headache
- Erythrocyte sedimentation rate is checked
- Immediate treatment with corticosteroids is required to prevent blindness if diagnosis is suspected.
Acute Angle-Closure Glaucoma
- Headache in older person (>50 years)
- Decreased visual acuity, nausea/vomiting, eye pain, mid-dilated fixed pupil
- Intra-ocular pressure should be reduced (pilocarpine, timolol, acetazolamide)
- Ophthalmology consultation.
Raised Intracranial Pressure
-
Untreated may lead to permanent sight loss, permanent neurological deficit, and death.
-
Constant, severe headache. May be aggravated by coughing, straining, or bending.
-
One third of patients report a headache that is worse on waking.
-
Patients also experience visual symptoms including blurred or double vision, and transient losses of vision.
-
Examine fundi for papilloedema.
-
Urgent neuroimaging looking for mass lesion, followed by lumbar puncture if safe.
-
Effect of pain on activity
-
Relationship with food
-
Response to any previous treatment
-
Any recent change in vision
-
Association with recent trauma
-
State of general health
Temporal Arteritis Z
Temporal arteritis (giant cell arteritis) is where the arteries, particularly those at the side of the head (the temples), become inflamed (vasculitis). It’s serious and needs urgent treatment.
- Commonly affects elderly female.
- The ESR is markedly elevated.
Symptoms
- Fatigue.
- Fever.
- Jaw pain that may become worse after chewing.
- Tenderness at the scalp or temples.
- Vision problems, such as double vision, blurry vision, or transient (brief) vision loss; if this is not treated, it could be followed by permanent, irreversible vision loss.
Treatment
-
The mainstay of therapy for temporal arteritis is glucocorticoids, such as oral prednisone in high dose. Z
-
Patients sometimes need to take glucocorticoids for up to two years.
Thunderclap Headaches
Sudden-onset headache pain, with peak intensity occurring within several minutes.
Causes:
-
Subarachnoid hemorrhage,
-
Hypertensive emergencies,
-
Vertebral artery dissections, and
-
Acute angle–closure glaucoma.
-
Known systemic illnesses that predispose to secondary headaches (cancer, HIV).
-
Altered mental status
-
History of trauma
-
History of malignancy
-
Pregnancy.
-
Neck stiffness
Rare/Serious
- Cough Headache – secondary.
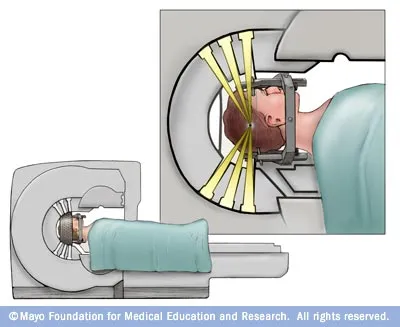
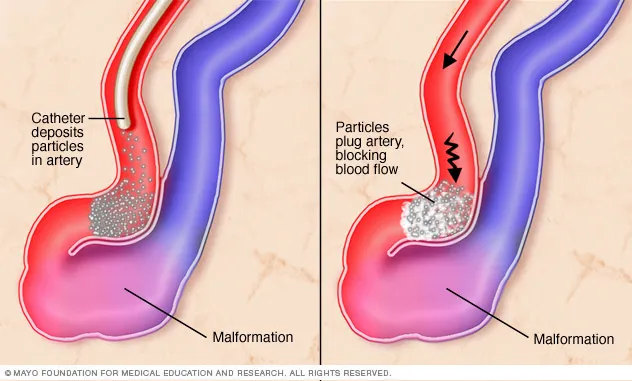
- Brain AVM (arteriovenous malformation).
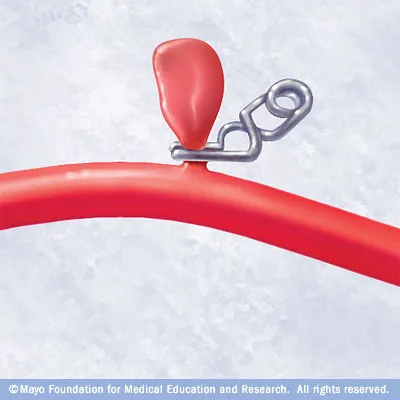
- Brain aneurysm.