Developmental Dysplasia of the Hip (DDH)
Overview
DDH - CDH (Congenital Dislocation of Hip)
Dr. Sultan Almisfer

Nomenclature
- CDH: Congenital Dislocation of the Hip
- DDH: Developmental Dysplasia of the Hip
- XCHD: (Congenital Heart Disease)!
Spectrum of Diseases
- Different etiologies, pathologies, and natural history
- Affects proximal femur and acetabulum
- Initial pathology is congenital, but:
- Progresses if untreated
- Does not always result in dislocation
CDH Spectrum
- Teratologic hip:
- Fixed dislocation at birth, often with other major anomalies
- Dislocated hip:
- May or may not be reducible
- Unstable hip:
- Dislocatable - Reducible
- Acetabular dysplasia:
- Shallow acetabulum
Incidence
- Hip instability at birth: 0.5 – 1%
- Classic DDH: 0.1%
- Mild dysplasia: Substantial
- Up to 50% of hip arthritis in ladies have underlying hip dysplasia
Etiology
Multi-factorial Causes
- Ligament laxity
- Hormonal factors:
- Estrogen, Relaxin: by mothers
- May affect baby girls more – receptors?
- Familial (congenital):
- Mild – Moderate – Sever – Ehler Danlos syndrome

Genetic Factors Z
- Females: 4-6 X more than males
- Twin studies:
- If one twin has DDH, the incidence of DDH in the second twin is:
- Monozygotic: 38%
- Dizygotic: 3% (similar to other siblings)
- If one twin has DDH, the incidence of DDH in the second twin is:
Mechanical Factors
- Prenatal:
- Breach position:
- Normally: 2-4%, In CDH: 16%
- Oligohydramnious – Primigravida
- Torticollis – metatarsus adductus
- Breach position:
- Postnatal:
- Swaddling / strapping hips adducted and extended, and knees extended


Risk Factors
- Positive family history: 10X
- A baby girl: 4-6 X
- Breach presentation: 5-10 X
- Torticollis: DDH in 10-20% of cases
- Foot deformities:
- Calcaneo-valgus and metatarsus adductus
- Knee deformities:
- Hyperextension and dislocation (Teratologic)
When risk factors are present:
- The infant should be examined repeatedly
- The hips should be imaged: (U/S or X-ray)
Clinical Examination
Physical Examination by Age Group
Neonatal Examination
- Ortolani Test: (reduces a dislocated hip)
- Feel a clunk
- Not hear a click!



- Barlow Test: (dislocated a reduced hip)!
- Feel a clunk
- Not hear a click!



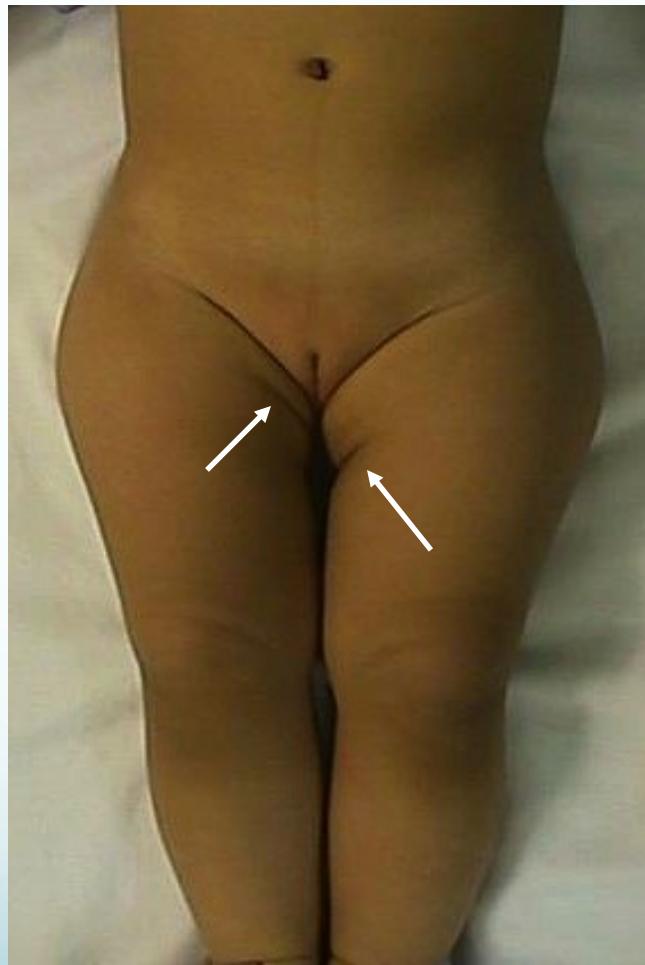
Visual Inspection
- Look for:
- Externally rotated hip
- Lateralized contour
- Wide perineum (in bilateral cases)
- Asymmetrical folds (Anterior - Posterior)
- Shortening (Galeazzi test)

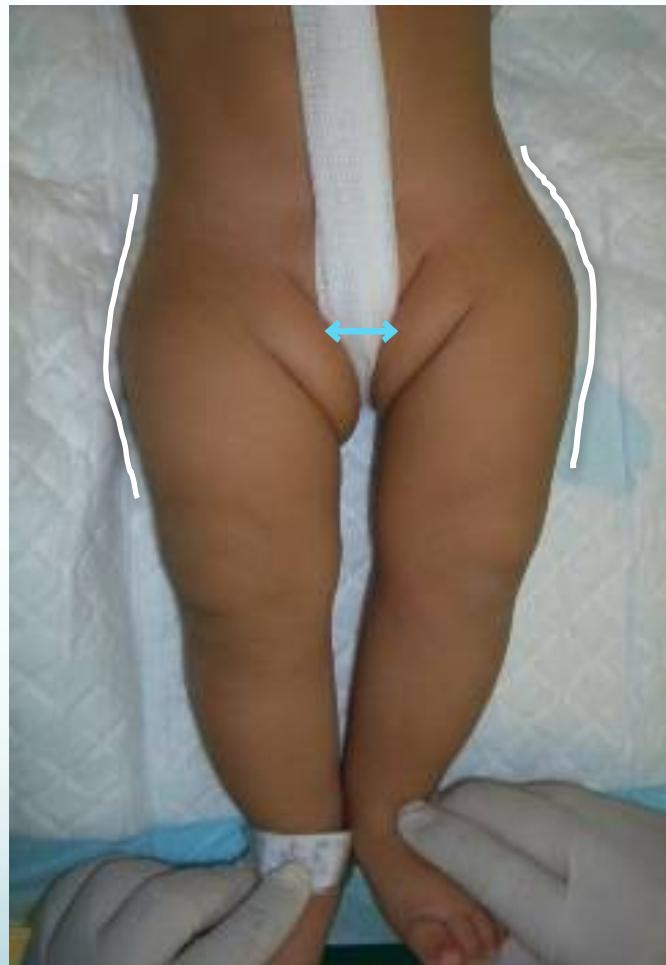



Range of Motion
- Move:
- Limitation of abduction in flexion
- Careful in bilateral cases
- Symmetrical limitation
- If abduction < 60° bilaterally: abnormal


The importance of a lollipop Galeazzi / Limited abduction in flexion



Functional Assessment
- Trendelenburg Sign:
- Unilateral: Trendelenburg gait
- Bilateral: Waddling gait
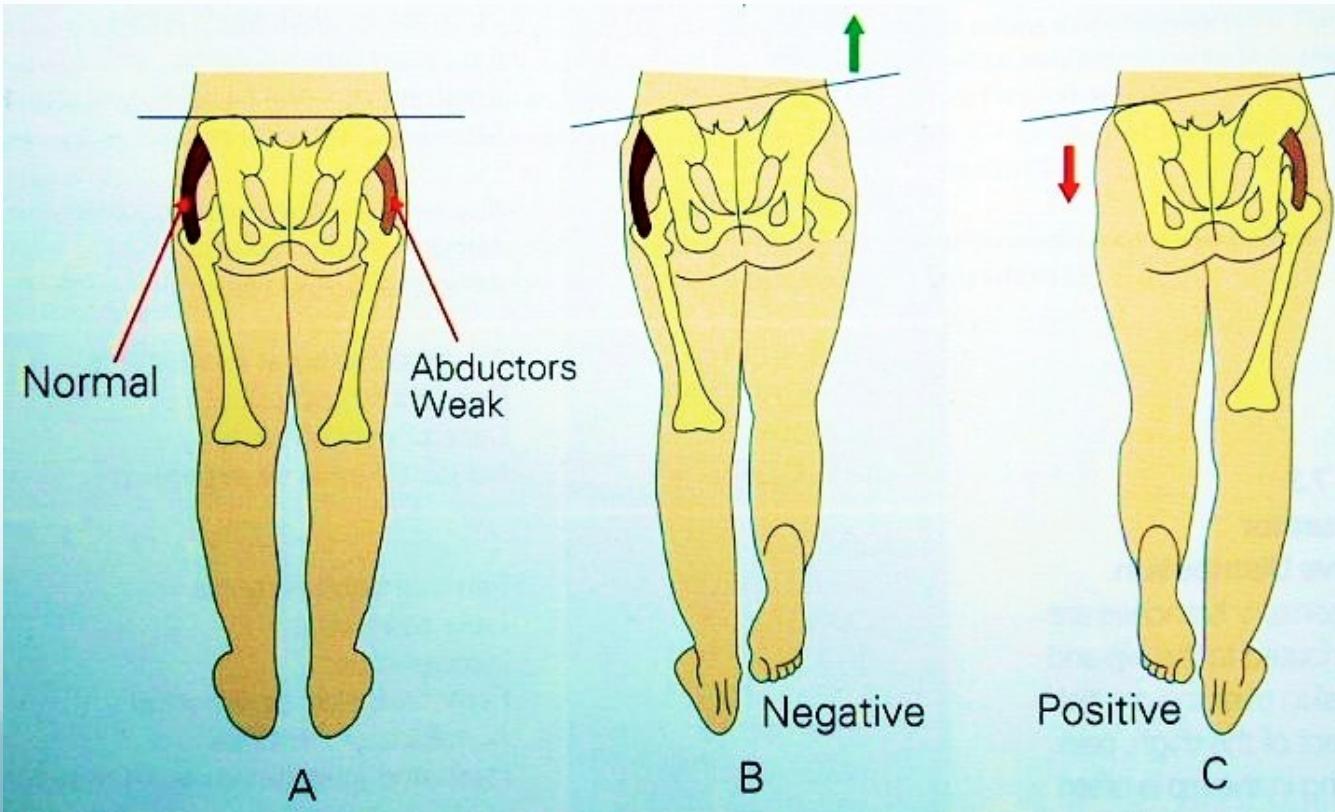
Examination Summary by Age
- Neonatal: Limited abduction, Ortolani/Barlow (up to 3m)
- Toddler: Shortening, limited abduction
- Walker: Shortening, limited abduction, Trendelenburg
Imaging
Ultrasound
- In early infancy U/S more reliable than x-ray
- Good in expert hands
- Incidence of hip stability declines rapidly to 50% within the first week of neonatal life
- Better to delay U/S to 4-6 weeks of age
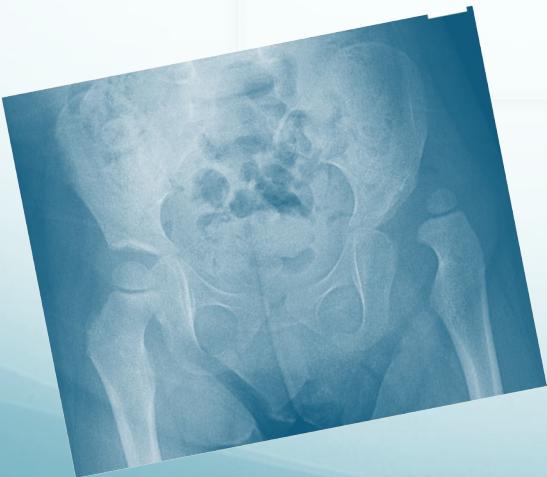
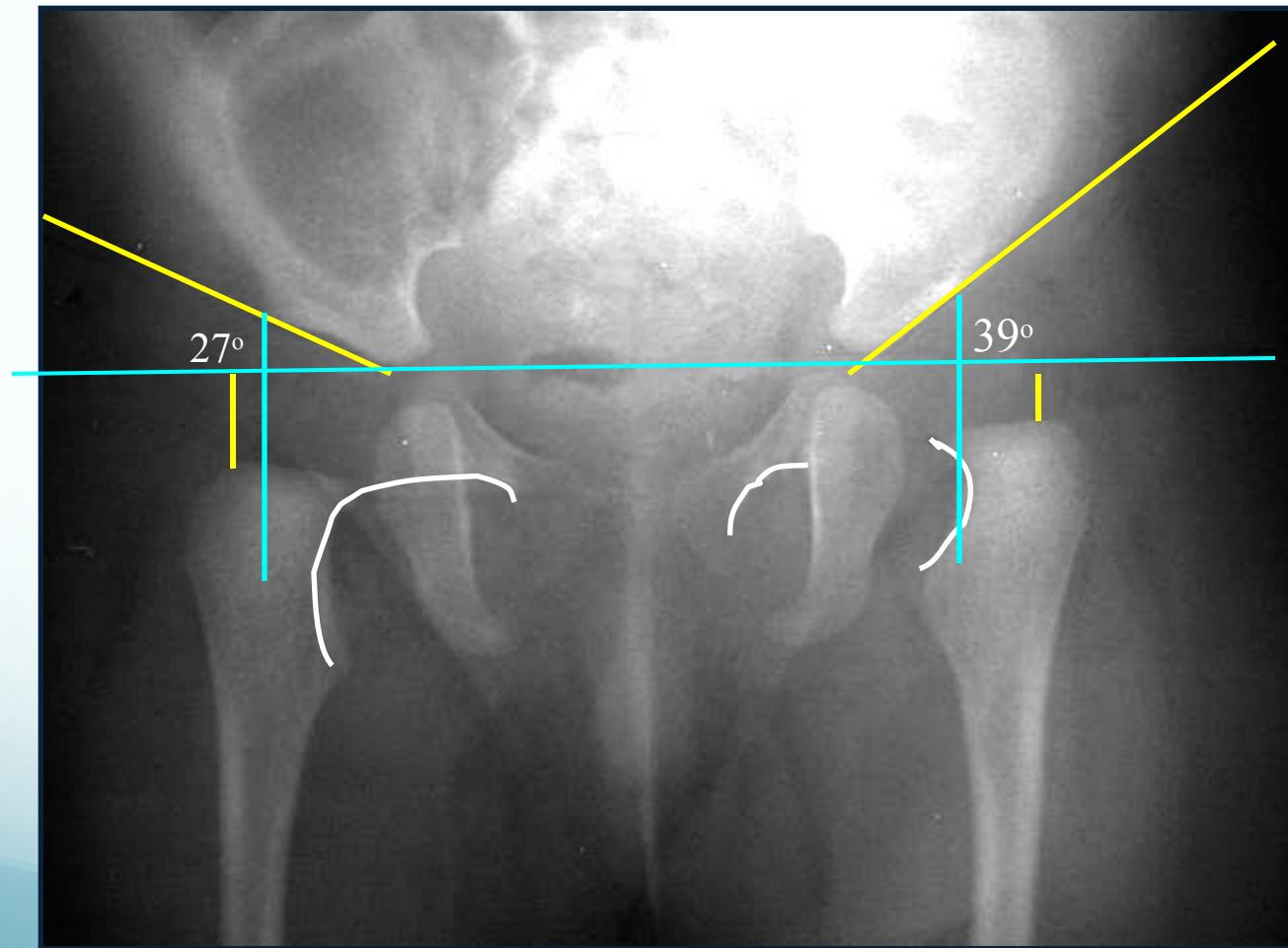
Radiology z
- After 3 months: more reliable
- Early infancy: not reliable - U/S better
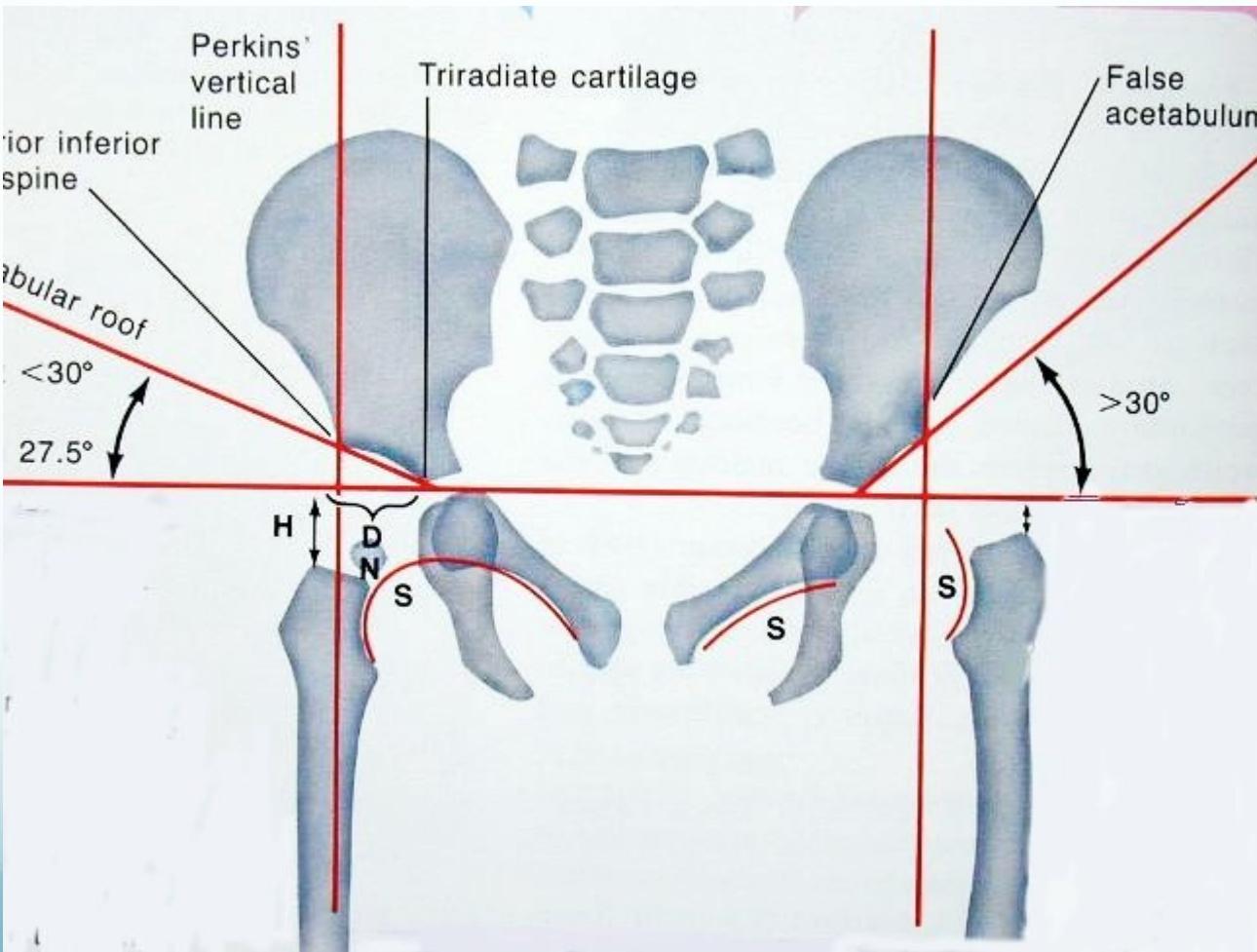

- AP abduction view
- Long axis of femur normally passes through acetabulum


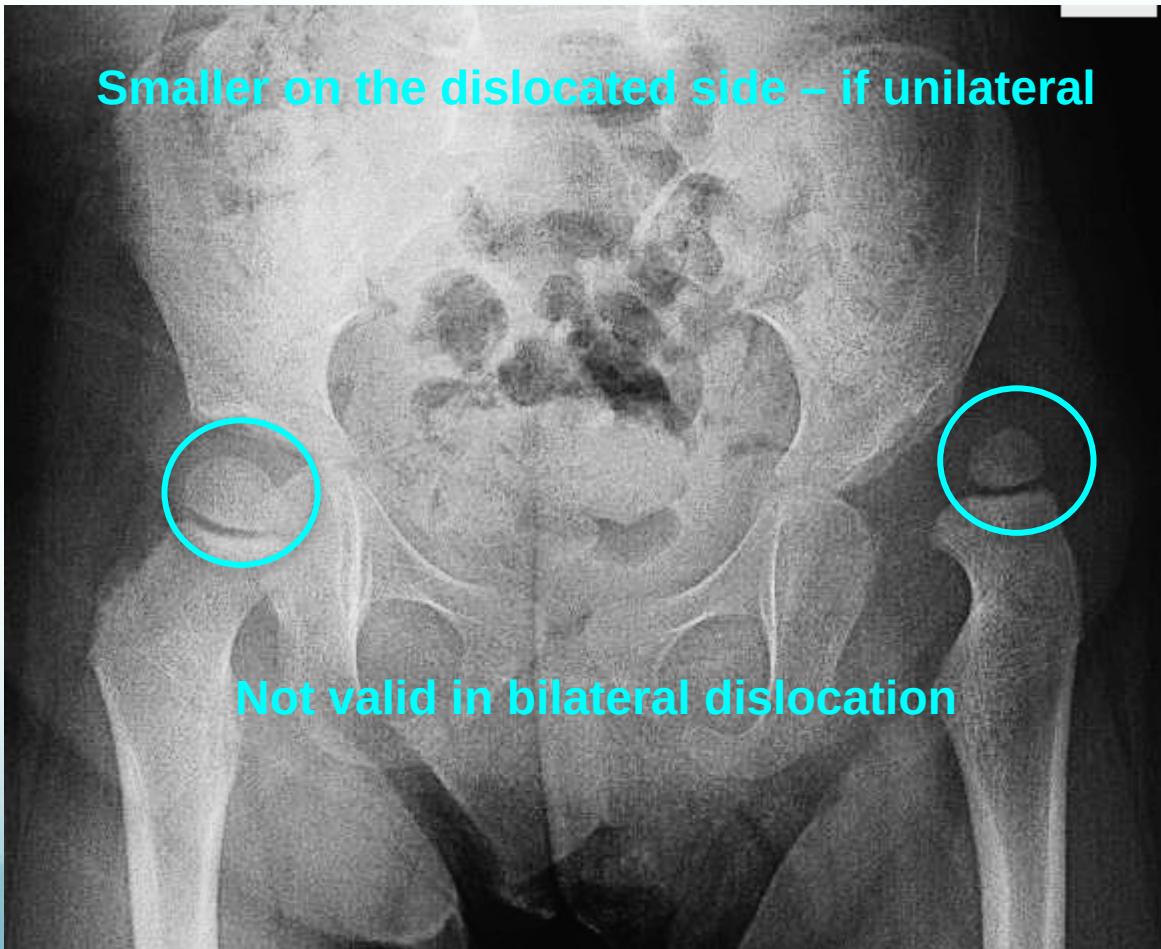
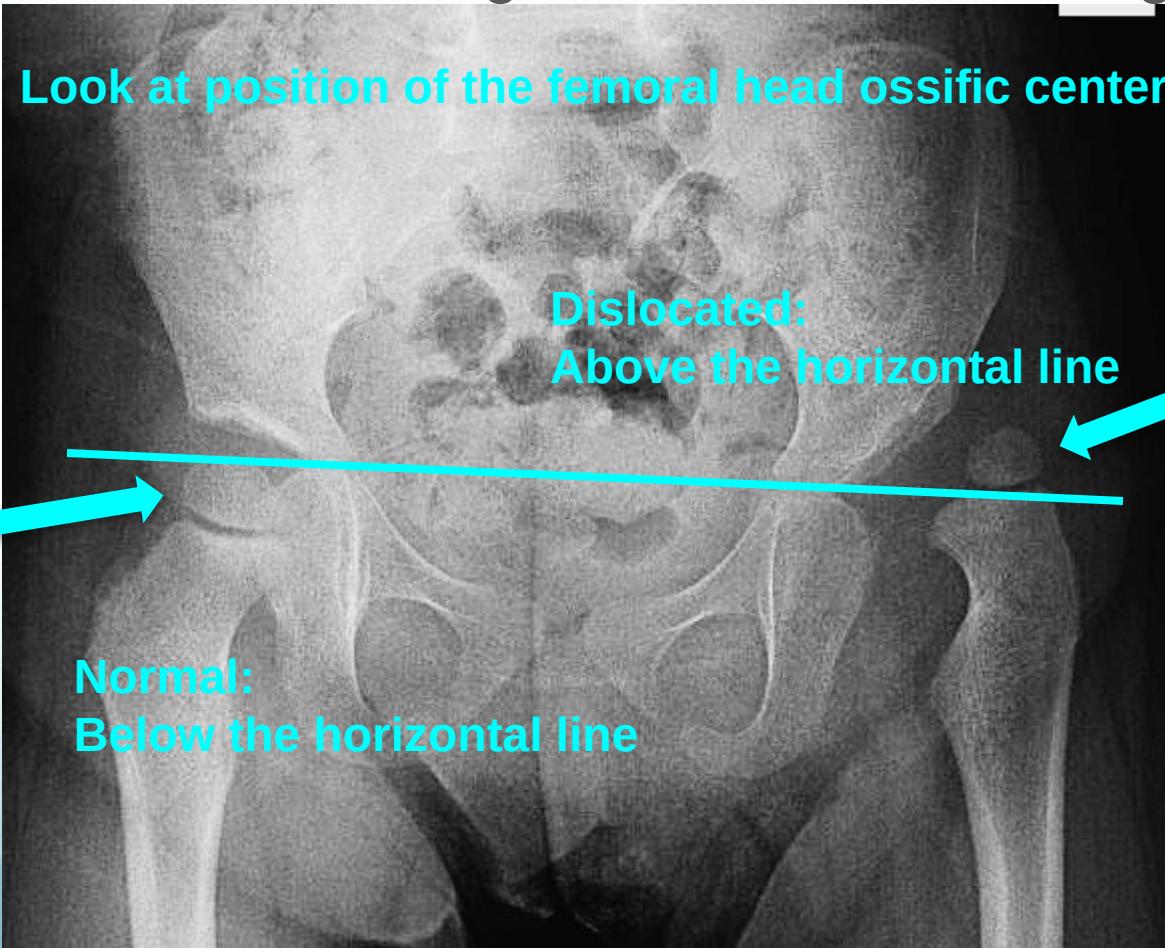
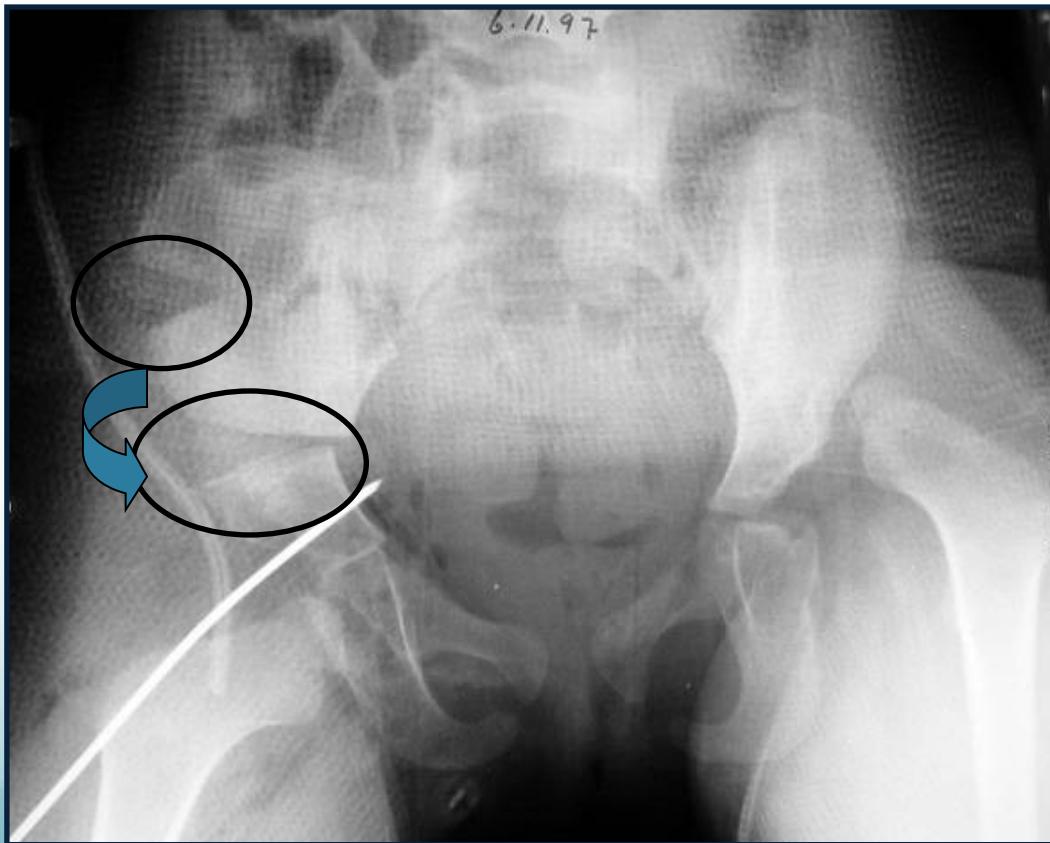
After 6 months:
- Clearly shows dislocation
- Size of femoral head ossific center
- Horizontal line through the tri-radiate cartilage
Position Assessment:
- Dislocated: Above the horizontal line
- Normal: Below the horizontal line

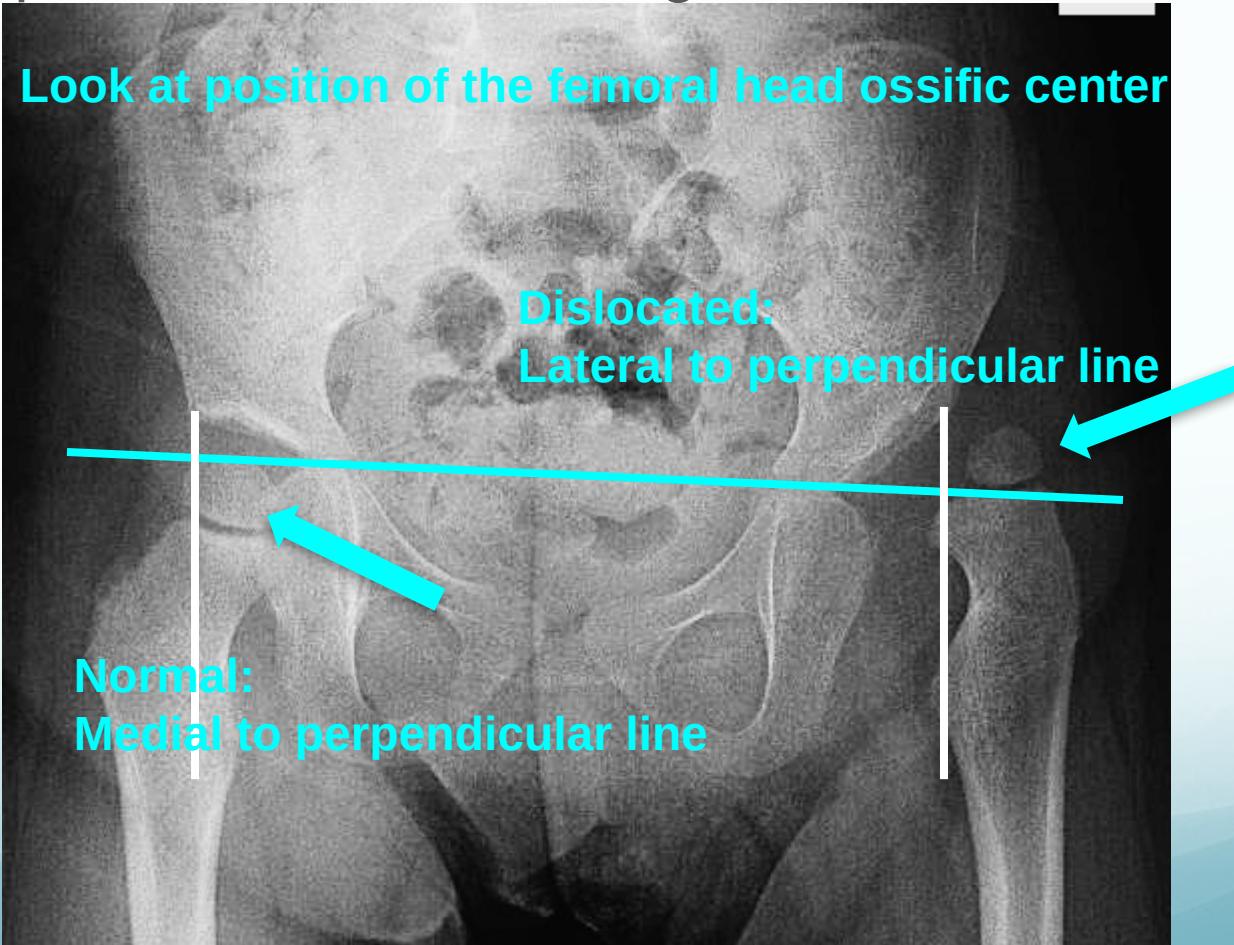
Radiographic Measurements
Perpendicular line from edge of acetabulum:
- Dislocated: Lateral to perpendicular line
- Normal: Medial to perpendicular line
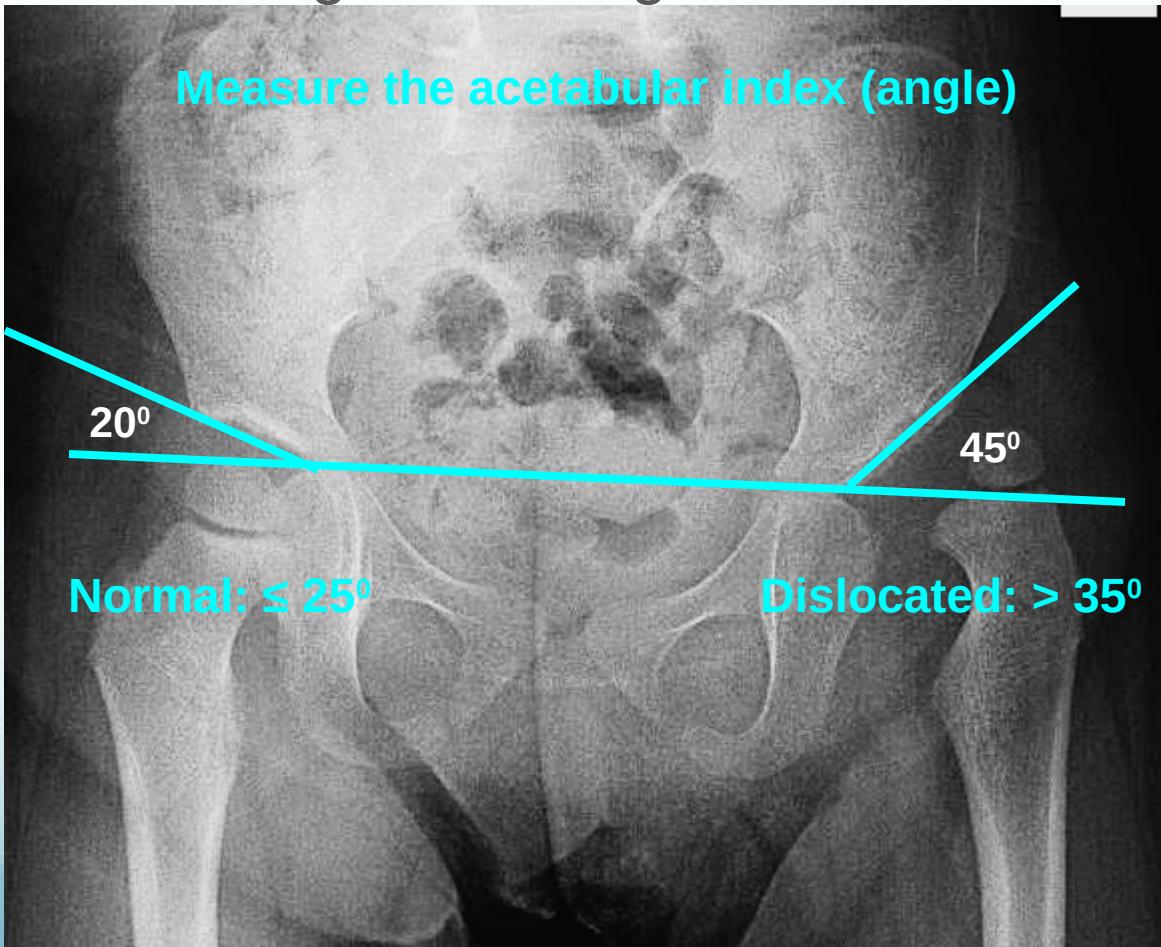
Acetabular angle (acetabular index):
- Normal: ≤ 25°
- Dislocated: > 35°
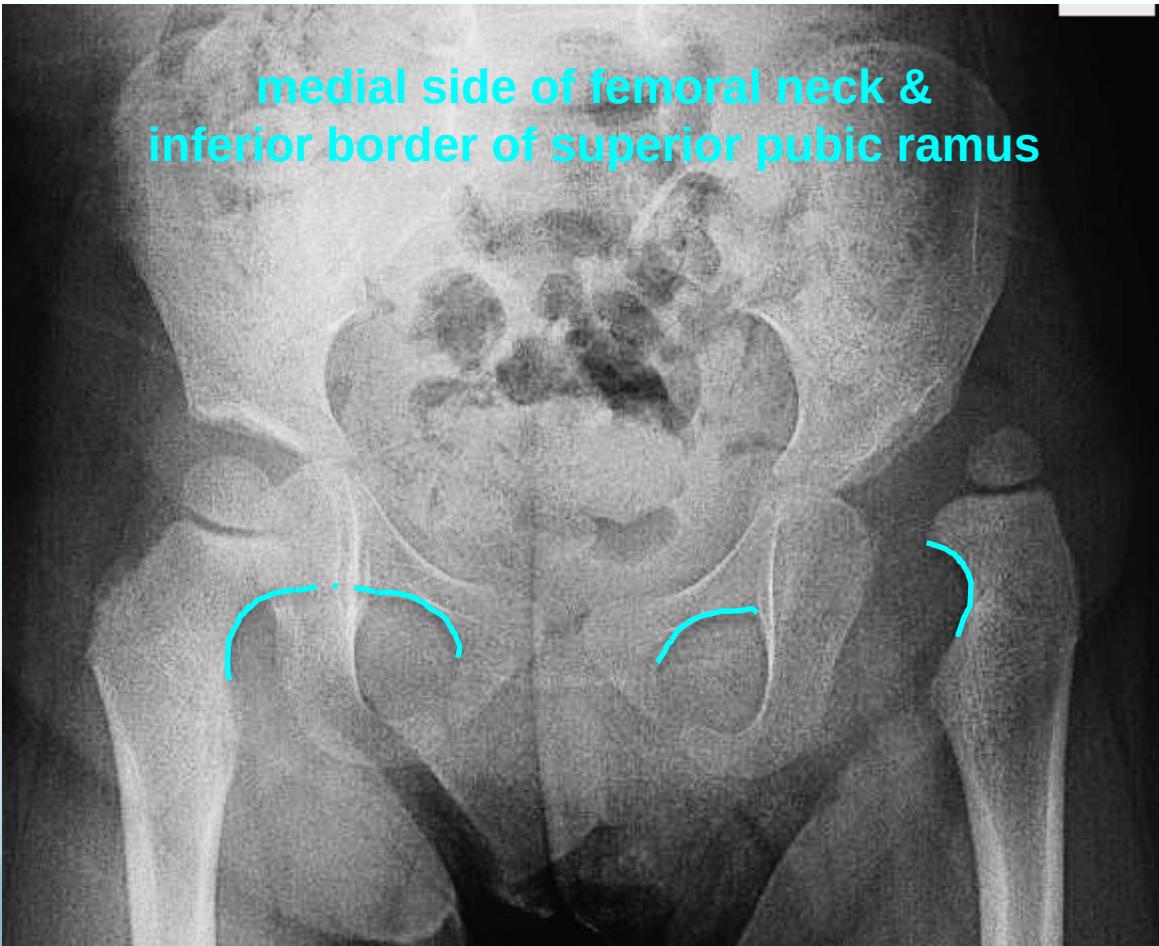
Shenton’s line:
Treatment
Treatment Goals
- Obtain concentric reduction
- In a non-traumatic fashion
- Without disrupting the blood supply to femoral head
Treatment Principles
- Method depends on age
- The earlier started, the easier it is
- The earlier started, the better the results are
- Should be detected EARLY
Treatment by Age Group
Neonatal Hip Instability (Birth - 6 months)
- Most resolve spontaneously
- Initial approach:
- Avoid adduction swaddle
- Apply double diapers – to bring back!!
- See at 2 weeks of age
- Unstable at 2 weeks:
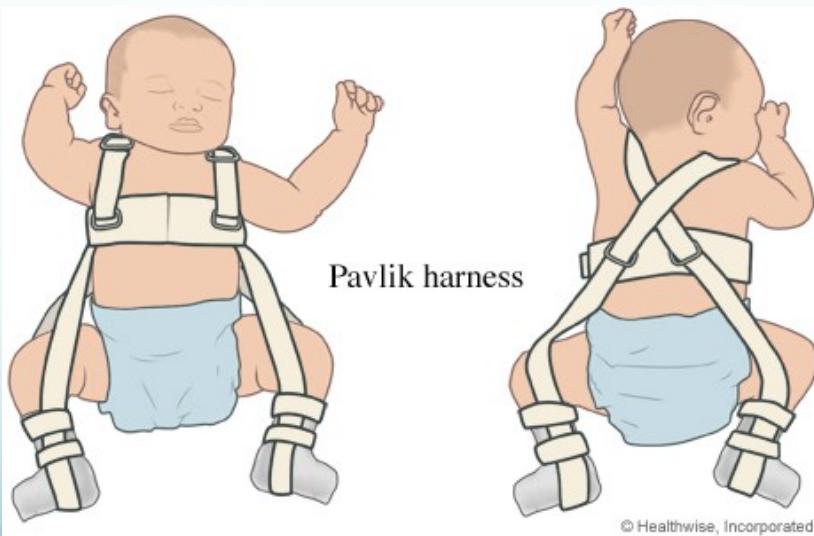
- Pavlik Harness
- Dynamic, effective, safe
- Pavlik Harness

6-12 months of age
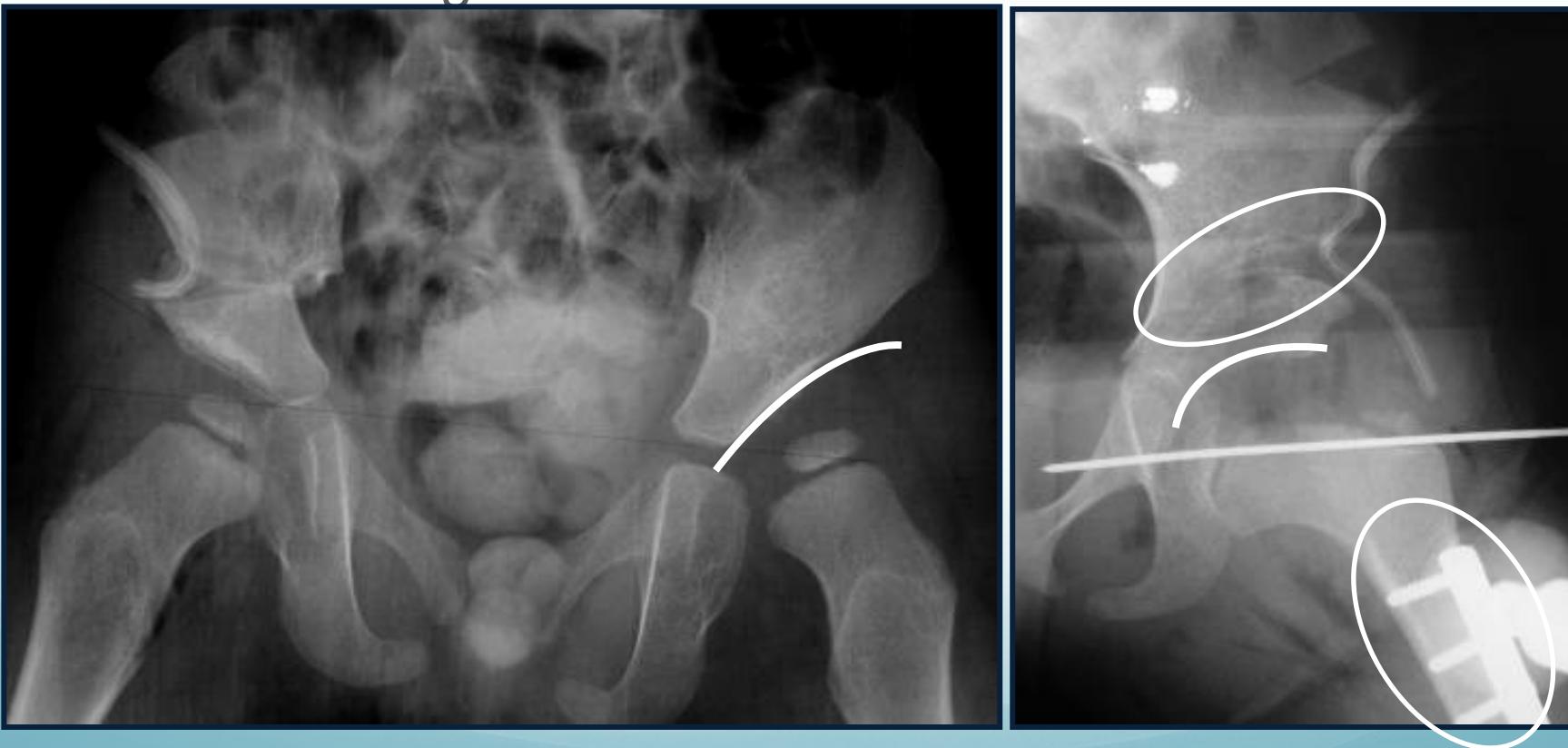
- Closed reduction & hip spica cast
- Arthrography-guided


12-24 months of age
- Surgery
- Open reduction & Acetabuloplasty (pelvic osteotomy)
Above 2 years of age
- Surgery
- Open reduction & Acetabuloplasty & Femoral shortening
Treatment Summary by Age
| Age Range | Treatment Approach |
|---|---|
| Birth – 6m | Pavlik harness or hip spica |
| 6-12m | Closed reduction under GA and hip spica |
| 12-18m | Open reduction and Acetabuloplasty |
| 2-8 years | Open reduction, Acetabuloplasty, and femoral shortening |
| Above 8 years | Open reduction, Acetabuloplasty cutting all three pelvic bones, and femoral shortening |
DDH Summary
- Complex multi-factorial, endemic disease
- Identify at risk groups
- Learning proper examination methods
- The earlier we treat the easier it is
- The earlier we treat the better the results