اللهم يا معلّم موسى علّمني، ويا مفهم سليمان فهّمني، ويا مؤتي لقمان الحكمة وفصل الخطاب آتني الحكمة وفصل الخطاب اللهم اجعل ألستنا عامرة بذكرك، وقلوبنا بخشيتك، وأسرارنا بطاعتك، إنك على كل شيء قدير، حسبنا الله ونعم الوكيل
Updates through https://medatlax.com/Clinical/Level-11/Orthopedics/OSCE/OSCE-Ortho/OSCE-Ortho - will be highlighted yellow - If there is any adjustment or edits please let me know Dr.alkharji@proton.me
Will be 4 stations
- History
- Joint exam
- Any skills we took (aspiration, cast, traction, etc.)
- Discussion from the lectures we took (Cauda equina, compartment, open fracture, septic arthritis, DDH, etc.)
Other exams and Other cases by end of file
collected from previous batches, Lina serhan, Ghuzlan, haya, Haneen Alsultan, Dania abuobaid, Alzahraa Ismaeel, Deema alsarawi, ~FA, Mujahid Almuhaydib, and Ola Al-Rayes
TOC
Hx&Ex
- History summarized
- Examination summarized
Skill
- Aspiration of knee, injection of elbow & shoulder
- Types of Casts (techniques), traction (techniques), Splints, nails, implants, slings, and mobility aid
Exam
- Examination of Shoulder
- Examination of the knee
Other Examinations
- Examination of Spine
- Neurological Examination
- Upper Limb Neurological Clinical Examination Station
- Lower Limb Neurological Clinical Examination Station
- Peripheral Nerve Examination
- Examination of the Spine / back
- Back ROM & Neurological
- McMaster MSK Examination Series
- Spine Examination – OSCE Guide
- Neurological Examination
Cases
-
Compartment Syndrome
-
Open Fracture
-
Septic Arthritis
-
DDH
-
Cauda Equina
-
Other Cases
OSCE
History
DDH, Knee pain, Shoulder stiffness, Back pain, Sport Injury
| Item | Details |
|---|---|
| Introduction | * Introduce self. |
| * Explain purpose of history. | |
| * Explain what you want to do. | |
| Patient’s Information/Demographics | * Patient (baby’s) name and age: (e.g., 3 months for DDH, 56-year-old lady for knee pain, 50-year-old man for shoulder stiffness, 53-year-old male for back pain, 23-year-old man for sport injury). |
| * Chaperone and their relationship to the baby (for DDH). | |
| * Name, Age, Occupation (for adults). | |
| Chief Complaint | * DDH: “The nurse mentioned there are some concerns about your baby’s left/right hip. Can you tell me more about what you’ve noticed or what the nurse observed?” |
| * Knee pain: Pain in both knees for 3 years. | |
| * Shoulder stiffness: Shoulder stiffness for 2 months. | |
| * Back pain: Progressive Back pain for one year. | |
| * Sport injury: Right knee pain after football injury 3 months ago. | |
| History of Present Illness - Onset | * When did you first notice anything unusual / when was it brought to attention? |
| * Sudden or gradual? (for all). | |
| * Acute after an incident, or Chronic (for back pain, sport injury). | |
| Site | * Where do you feel it? |
| * Baby’s hip. | |
| * Where in the back (low, mid, upper for back pain). | |
| * Exact site (for sport injury). | |
| * Shoulder for stiffness. | |
| Character | * Sharp, dull, throbbing? |
| * (difficult with infant for DDH). | |
| * Dull, aching, sharp, hot (for back pain, sport injury). | |
| Radiation | * Does the pain radiate elsewhere? |
| * (For discomfort/pain for DDH). | |
| * Down to thigh, leg, toes (for back pain). | |
| * Down or Upwards, back (for sport injury). | |
| Associations | * DDH: Clicking, popping, or clunking sounds from hip. |
| * Knee pain: Hotness, swelling. | |
| * Shoulder stiffness: Pain / Swelling / Clicking. | |
| * Back pain: Constitutional symptoms, others. | |
| * Sport injury: Fever, Swelling. | |
| Time Course | * Continuous, intermittent, worse at night/morning? (for DDH). |
| * Progressing/improving, all day / at end of day, at activity (for back pain, sport injury, shoulder stiffness). | |
| Exacerbating Factors | * What makes it better or worse (e.g., position, movement)? (for DDH). |
| * Activity, bending, coughing/sneezing, lifting (for back pain). | |
| * Activity, stairs (for sport injury). | |
| Relieving Factors | * What makes it better or worse (e.g., position, movement)? (for DDH). |
| * Medications, rest, position (for back pain, sport injury). | |
| Severity | * Getting worse, or staying the same? (for DDH). |
| * DDH: Scale 0-10 pain is difficult for infants, focus on behavioral changes. | |
| * Others: Scale 1-10 (for back pain, sport injury). | |
| SOCRATES (for discomfort/pain) | * Site, Onset, Character, Radiation, Alleviating/Aggravating Factors, Timing, Everyday Impact, Severity/Progression (for DDH). |
| Associated Symptoms (DDH Specific) | * Swelling, stiffness, deformity, instability? |
| * Limping, use of walking aids (less relevant for infant). | |
| * Swaddling practices (legs straight and tight vs. free movement). | |
| * Clicking, Locking (hip). | |
| * Does she favor one leg, move one leg less? | |
| * Asymmetry in thigh/gluteal folds? | |
| * Crying/discomfort with movement? | |
| * Difficulty changing diapers/dressing? | |
| DDH Risk Factors (“3 Fs” + others) | * Antenatal: Illnesses/complications during pregnancy, oligohydramnios. |
| * Birth History: Delivery complications, breech presentation (especially frank), APGAR score, C-section vs. vaginal, multiple birth, NICU admission. | |
| * Post-natal: Ever in Pavlik Harness or hip spica cast? | |
| * Family History: DDH or other hip problems? | |
| * First born child? | |
| * Female baby? | |
| * Foot abnormalities at birth? | |
| Developmental Milestones (DDH) | * Head control? |
| * Rolling? | |
| * Reaching for toys? | |
| * Meeting age-appropriate milestones (smiling, tracking, cooing)? | |
| Function / Normal Daily Activities | * Knee pain: Stiffness / Normal daily activities/ Walking / Sitting in prayer / cross-legged / Arabic toilet / Fitness Activity / Limping. |
| * Shoulder stiffness: Reaching / Putting shirt on / using hand / Fitness Activity. | |
| * Back pain: Stiffness / Normal daily activities / prayer / bending / lifting. | |
| * Sport injury: Walking, standing, praying, Sitting, Going up/ down stairs, Sports. | |
| Impairment to Sleep/Work | * Disturbing night’s sleep (for all). |
| * Affecting work / sick leaves (for all). | |
| Previous Problems (Specific Joint) | * Knee pain: Trauma: twisting/popping, Fractures / casting. |
| * Shoulder stiffness: Infection/Trauma. | |
| * Back pain: Trauma, lifting heavy weight. | |
| * Sport injury: Trauma twisting / popping / Fractures / casting / Surgery / Stiffness / Deformity / Crepitus. | |
| Other Problems in the Knee | * Instability - Giving way, Locking, Crepitation/Clicking sound (for knee pain). |
| Swelling | * DDH: Any visible swelling around the hip? |
| * Knee pain, Shoulder stiffness: Exact site: front, medial, behind. Onset: Acute / Chronic. Character: Soft / Hard. Progression: Same / increasing / reducing. Exacerbating / Relieving factors. | |
| * Back pain: Site, onset, progression. | |
| * Sport injury: When (sudden or late), how long, continuous, less or more, on/off. Swelling in /behind knee. | |
| Deformity | * DDH: Any visible deformity around the hip? |
| * Knee pain, Back pain, Shoulder stiffness: Site / Direction. Onset: Time. Progression: Same / increasing / reducing. | |
| Neurological (Back Pain Specific) | * Numbness/Tingling LL (where?). |
| * Heaviness / weakness. | |
| * Sexual ability. | |
| * Sphincter control— urine/stool. | |
| Giving Way (Sport Injury Specific) | * Sudden loss of stability in knee. |
| Locking (Sport Injury Specific) | * Painful / opens after a click. |
| Previous Management | * DDH: Has anything been done or tried for this hip problem (e.g., changes in swaddling, physiotherapy, repositioning)? |
| * Knee pain, Shoulder stiffness: Investigations / current or past treatment. | |
| * Back pain: Investigations: X-rays, CT, MRI, others. Treatment: Medications, Physiotherapy, Surgery. | |
| * Sport injury: Investigation & treatment. | |
| Past Medical History | * DDH: Any other medical problems or hospital admissions? Chronic illnesses? Blood transfusions? Seen other doctors for hip/related issues? |
| * Adult conditions: Medical: HT / DM / Osteoporosis. Infections (Pulmonary, GIT, Urinary), Fever, Cough. TB. Tumors breast, uterus, lungs/ Recent weight gain or loss (for back pain). | |
| Past Surgical History | * Knee pain: Knee or others. |
| * Shoulder stiffness: Shoulder or others. | |
| * Back pain: At Back or others. | |
| Drug History / Current Medications | * DDH: Currently on any medications (prescribed or over-the-counter)? What are they and why? |
| * Shoulder stiffness: Specific: NSAIDs, steroids, General. | |
| * Back pain: Hormones/ Steroids. | |
| Allergies | * DDH: Any known allergies (food, drugs, environmental)? Reaction? |
| * Shoulder stiffness: Drug allergies? | |
| Immunization History (DDH) | * Up-to-date with routine childhood immunizations? Last vaccination? |
| Other Joints Problems | * Joints affected / Problem (for all adult conditions). |
| Diet/Calcium intake/Vit. D/Sun Exposure | * (for knee pain, sport injury). |
| Family History | * Adult conditions: OA / Tumors / Osteoporosis / HT/DM (for knee pain, shoulder stiffness, sport injury). |
| * Back pain: Infection, TB, Back diseases, Scoliosis, Tumors. | |
| Systemic Inquiries (Review of Systems) | * DDH: General well-being: Headache, chest pain, palpitation, cough, joint pain, edema? (less relevant but general screening). Constitutional Symptoms: Fever, weight loss, night sweats, loss of appetite, loss of sensation/motor (less specific but for overall health). |
| * Adult conditions: CVS. Respiratory. GIT. Urogenital. CNS & PNS. MSK. Metabolic system. psychiatric. | |
| * Sport injury: History related to major body systems. | |
| Lifestyle / Social History / Living Conditions | * DDH: Feeding method, sleep pattern, recent travel, stress in household/support systems. Swaddling Practices. |
| * Sport injury: Residence. | |
| * Back pain: Stairs, helper at home. | |
| Smoking / Alcohol / Drug Abuse | * (for all adult conditions). |
| Attitude with patient & Showing concern | * Professional (for all). |
| Good question style / Confidence / no hesitation / no gaps | * (for all). |
| Summary (DDH) | * “Just to summarize, the nurse has noted a positive finding suggestive of DDH in your 3-month-old daughter’s [left/right] hip. From what you’ve told me, you haven’t noticed [mention positive/negative from above]. Is that correct?” |
| * “Is there anything else that you think is important or that I should know about your baby?” | |
| Mechanism of Injury (Sport Injury Specific) | * Twisting - varus/valgus stress. |
| * Direct fall - direct blow (direction). | |
| * Swelling after injury - how soon? How large? |
if recent truama take AMPLE
Examination summarized
General approach
| Phase | Procedure & Key Points | |
|---|---|---|
| 1. Opening & Preparation | • Introduction & Consent: Greet the patient, introduce yourself, explain the procedure, and gain informed consent. Ensure privacy. • Exposure: Adequately expose the joint being examined and the joints above and below. • Positioning: Start with the patient standing for gait/posture, then move to sitting and supine as needed. Always compare with the unaffected side. | |
| 2. Look (Inspection) | • Gait & Posture: Observe the patient walking for any limp (e.g., antalgic, Trendelenburg) and check their overall posture. • Local Inspection: From all angles, look for: - Scars, Swelling, Skin changes, Symmetry. - Atrophy (muscle wasting). - Deformity (angulation, fixed flexion). | |
| 3. Feel (Palpation) | • Temperature: Use the back of your hand to assess skin temperature, comparing it to the contralateral side. • Tenderness: Gently palpate key structures, starting away from the painful area: - Bony landmarks (joint lines, epicondyles). - Soft tissues (muscles, tendons, ligaments). • Effusion: Check for joint fluid (e.g., patellar tap for the knee). | |
| 4. Move (Movement) | • Active Range of Motion: Ask the patient to move the joint through its full range. Note any pain or limitation. • Passive Range of Motion: Gently move the patient’s joint through the same range. Feel for crepitus and assess the end-feel. • Power: Test the strength of key muscle groups against resistance. • Joints Above & Below: Briefly assess movement in adjacent joints to rule out referred pain. | |
| 5. Special Tests | • Perform joint-specific provocative tests to confirm a diagnosis. Examples: - Knee: Lachman’s, McMurray’s. - Shoulder: Apprehension, Neer’s. - Hip: Thomas, Trendelenburg. - Spine: Straight Leg Raise. | |
| 6. Completion | • Neurovascular Status: Always assess distal circulation (pulses, capillary refill), sensation, and motor function. • Final Steps: Thank the patient, help them get comfortable, and state that you would complete your assessment with a history and relevant imaging. |
Skill
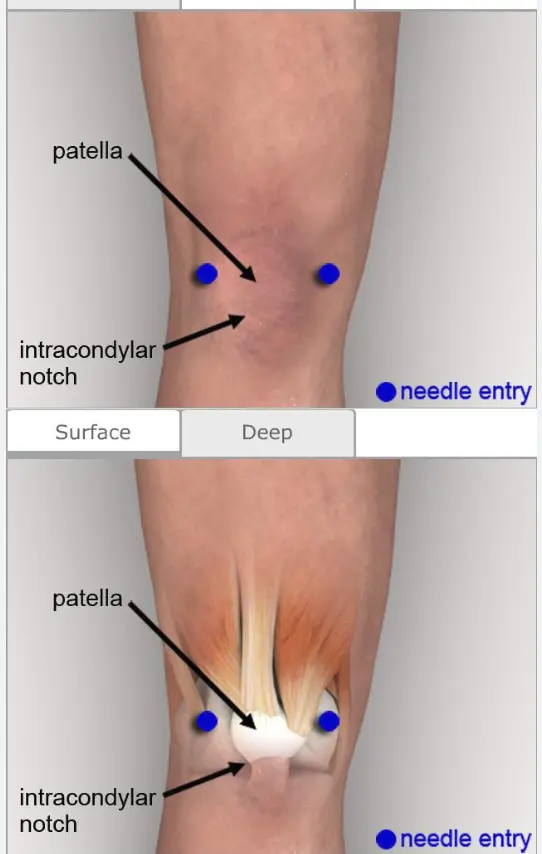
Knee Aspiration
https://www.youtube.com/watch?v=sRVAzsZEBVY&pp=ygUUS25lZSBhc3BpcmF0aW9uIG9zY2U%3D https://www.youtube.com/watch?v=ikXvLLlpoas&pp=ygUUS25lZSBhc3BpcmF0aW9uIG9zY2U%3D
| Item | Procedure |
|---|---|
| Indication Ask student |
|
| Contraindications Ask student |
|
| Introducing |
|
| Preparation / position Ask student | Patient in supine position Knee straight - slightly flexed (15-20°) on small support |
| Antiseptic technique |
|
| Aspiration |
|
| Post procedure instructions |
|
| Overall |
|

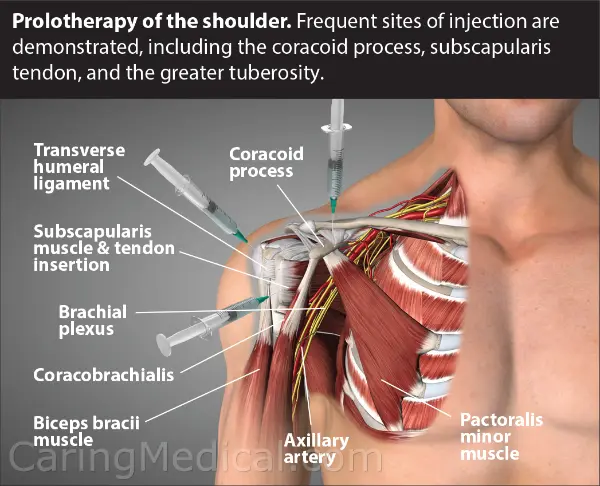
Injection of shoulder
https://www.youtube.com/watch?v=HvH__fP__RU&pp=ygUdc2hvdWxkZXIgam9pbnQgaW5qZWN0aW9uIG9zY2U%3D
https://www.youtube.com/watch?v=OAeOEc-X0kU
This patient has chronic shoulder pain (OA glenohumeral / subacromial pathology) has not responded to NSAIDs. You are required to inject the site with steroid and local anesthetic agent.
| Item | Procedure |
|---|---|
| Indication of arthrocentesis of the shoulder | Diagnostic: arthritis, septic |
| Therapeutic: reducing massive effusion | |
| Steroid Injection for : OA glenohumeral joint, AC joint, sub- acromial bursa | |
| Contraindications | Cellulitis over injection site |
| Skin lesion over injection site / psoriasis…..etc. | |
| Uncontrolled anticoagulation therapy / or sever coagulopathy | |
| Uncooperative patient | |
| Introducing | Explaining the procedure |
| Explain risks: Mild pain / Infection (1:10,000) / Bleeding | |
| Obtain consent / explain alternatives | |
| Preparation Antiseptic technique | Seating patient properly |
| Cleaning with antiseptic lotion or alcohol | |
| For Glenohumeral joint: | |
o Feel the coracoid, go lateral to it from anterior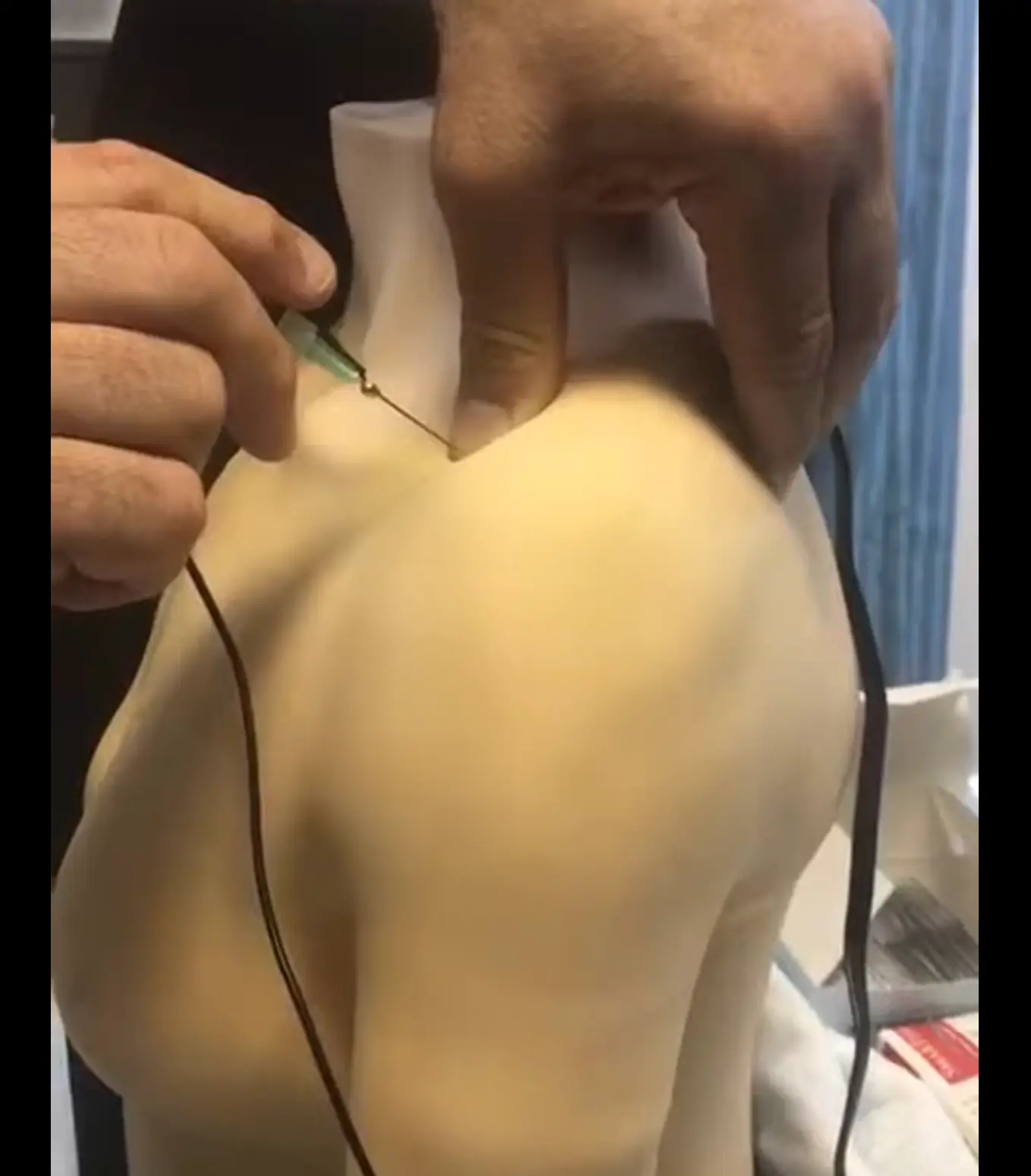  Posterior glenohumeral injection | |
| For subacromial bursa/space | |
| o Feel acromioclavicual joint, go under it from lateral - Feel acromioclavicual joint, go under it from lateral Subacromial (not in checklist)  Bicipital (not in checklist) | |
| If at proper site, the green light should turn on | |
| Post injection | Apply band aid |
| Remind patient to take NSAID as pain may increase initially | |
| Needle | Handling / disposal: No recapping - Disposal in sharp disposal box |
| Alcohol swab disposal in trash - not in sharp disposal box | |
| Overall | Attitude with patient |
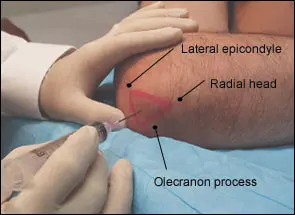
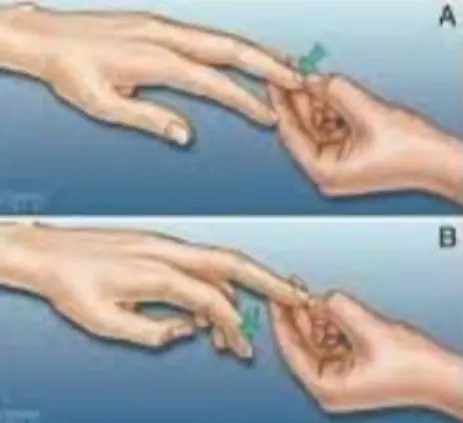
Injection for Tennis elbow (Lateral Epicondylitis)
This patient has lateral epicondylitis. You are required to give him an injection
| Item | Procedure |
|---|---|
| Indication | Failure to respond to conservative treatment |
| Ο Rest, NSAID orally and topically, Cold/hot packs, U/S Physiotherapy | |
| Introducing | Informing patient of the procedure |
| Explaining the procedure: | |
| Ο Mixture of steroid and local anesthetic | |
| Ο Pain may increase for 1-3 days – need to take oral NSAID | |
| Preparation / position | Ο Seating patient properly Ο Elbow flexed on chair in front of patient Or: sitting with flexed elbow on table in front (from front) |
| Antiseptic technique | Using gloves |
| Cleaning with antiseptic lotion or alcohol | |
| Ο Starting in center with circles enlarging to periphery | |
| Ο Not coming back from periphery to center | |
| Site of injection | Lateral epicondyle: → Common extensur |
| Ο Feel and identify area of maximum tenderness | |
| Ο Just distal to tip of lateral epicondyle | |
| Injection | Needle perpendicular to skin |
| Ο If at proper site, the green light should turn on | |
| Post injection | Apply band aid |
| Remind patient to take NSAID as pain may increase initially | |
| Needle | Handling / disposal: No recapping - Disposal in sharp disposal box |
| Alcohol swab disposal in trash - not in sharp disposal box | |
| Overall | Attitude with patient |
 |
Injection for golfer elbow (medial epicondylitis)
https://www.youtube.com/watch?v=eVaguVc53DM&pp=ygUfSW5qZWN0aW9uIGZvciBnb2xmZXIgZWxib3cgb3NjZQ%3D%3D
This patient has medial epicondylitis that has not responded to conservative management. You are required to inject the site with steroid and local anesthetic agent.
| Item | Procedure |
|---|---|
| Introducing | Informing patient of the procedure |
| Explaining the procedure: | |
| Mixture of steroid and local anesthetic | |
| Pain may increase for 1-3 days - need to take oral NSAID | |
| Preparation | Seating patient properly |
| Elbow flexed on chair in front of patient | |
| Or: sitting with shoulder externally rotated and flexed elbow | |
| Antiseptic technique | Using gloves |
| Cleaning with antiseptic lotion or alcohol | |
| Starting in center with circles enlarging to periphery | |
| Not coming back from periphery to center | |
| Site of injection | Medial epicondyle: |
| Feel and identify area of maximum tenderness | |
| Just distal and slightly anterior to tip of medial epicondyle | |
| Must avoid the ulnar nerve behind the medial epicondyle | |
| Injection | Needle perpendicular to skin |
| If at proper site, the green light should turn on | |
| Major mistake if the red light is turned on (injury to ulnar nerve) | |
| Post injection | Apply band aid |
| Remind patient to take NSAID as pain may increase initially | |
| Needle | Handling / disposal: No recapping - Disposal in sharp disposal box |
| Alcohol swab disposal in trash - not in sharp disposal box | |
| Overall | Attitude with patient |
| ![[MedAtlax/Clinical/Level 11/Orthopedics/OSCE/attachments/OSCE-Ortho-1762600385435.webp | 295x221]] |
Aspiration of knee, injection of elbow & shoulder
Joint Aspiration and Injection (and soft tissue)
Indications
Diagnostic Indications
- Evaluate an acutely swollen and inflamed ‘hot’ joint
- Rule out Infection (most important)
- Analyze synovial fluid
- Characterize mono- or polyarthritis
- Inflammatory
- Degenerative
- Crystalline (Gout, pseudogout)
- Characterize mono- or polyarthritis
Therapeutic Indications
- Drain large effusions / haemarthrosis
- Symptomatic relief
- Improves function
Contraindications
- ✓ Prosthetic joint
- ✓ Overlying cellulitis
- ✓ Active skin disease (e.g. psoriatic lesions at the site of injection)
- Flare in the joint post-injection when performed previously
- ✓ Bleeding diathesis
- anticoagulation, hemophilia, thrombocytopenia
- not an absolute contraindication, but be careful
- Two weeks before planned Arthroplasty
Complications
- ✓ Infection
- very rare if good sterile technique ()
- ✓ Bleeding / Haemarthrosis
- ✓ Vasovagal syncope
- ✓ Pain
- Cartilage injury
- Poor technique
What to Do with Aspirate?
Visual Assessment
- Check yourself
- Clear colorless: normal
- Clear yellow:
- can read through: non-inflammatory
- Turbid: Inflammatory
- Pus
- Blood


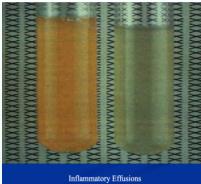
Laboratory Analysis
- Send for:
- ✓ Cell count with differential
- in purple-top tube
- ✓ Gram stain / Culture and sensitivity
- in sterile container or red-top tube
- ✓ Crystals
- In red-top tube
- ✓ Glucose, Total Protein
- ✓ Cell count with differential
Joint Injection
Medications
- ✓ Steroids
- ✓ Local anesthetics +/-
- Other material:
- ✓ Hyaluronic acid ?
- Glucosamine ???
- Chondroitin ???
Indications
1. Inflammatory Arthritis
- (e.g. rheumatoid arthritis, spondyloarthropathies)
- Up to six months improvement from a single joint injection
2. Osteoarthritis (OA)
- A weaker indication for steroid injection
Soft Tissue Injection
Treatment of Localized Inflammation
- Bursitis
- Trochanteric, subacromial, prepatellar, olecranon
- Flexor tenosynovitis (Trigger finger / thumb)
- Tenosynovitis (DeQuervain’s)
- Lateral epicondylitis (Tennis elbow)
- Medial epicondylitis (Golfer’s elbow)
- Plantar fasciitis
- Adhesive capsulitis – Frozen shoulder
- Carpal tunnel syndrome
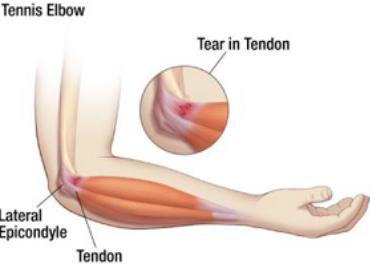
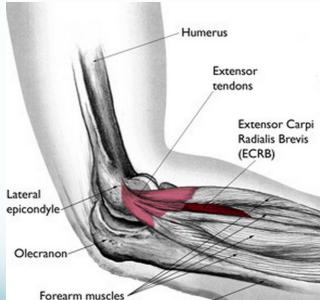
Tennis Elbow (Lateral Epicondylitis)
Have you ever heard of tennis elbow or suffered from elbow pain? Continue reading to learn about this condition and a new study that may change the way we approach treating this problem.

Steroid injection for tennis elbow

INJECTION TARGET Therapeutic agent is injected between the bone and the common extensor tendon (about 1 cm anterior to the lateral epicondyle with the elbow in a flexed position)
Golfer’s Elbow (Medial Epicondylitis)
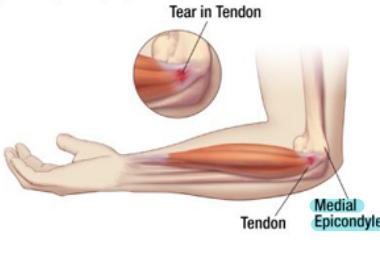
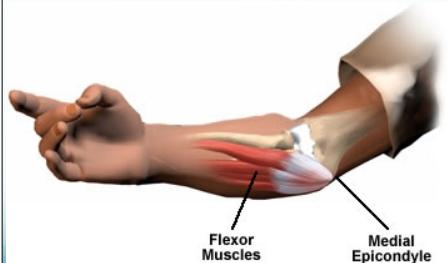
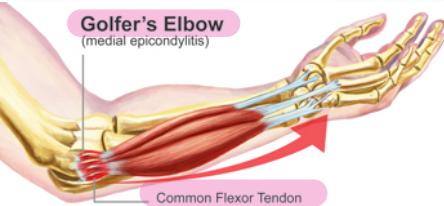
Pain occurs on the inside part of the elbow where the tendons of the forearm connect to the medial epicondyle. Pain may spread down the forearm to the wrist.
Types of Casts (techniques), traction (techniques), Splints, nails, implants, slings, and mobility aid
Traction
| Type of Traction | Purpose | Usage | Advantages | Attachments | Disadvantages/Complications |
|---|---|---|---|---|---|
| Manual Traction | Obtain closed reduction of a fracture or dislocation by direct pulling force from a physician. | During manipulation for fracture or dislocation reduction. | Direct and immediate control for reduction. | 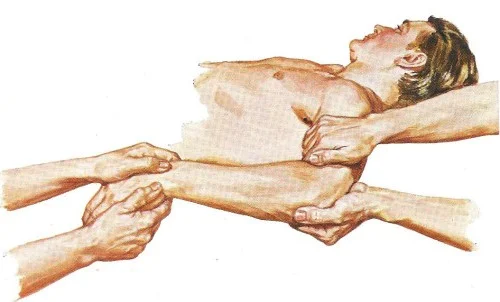 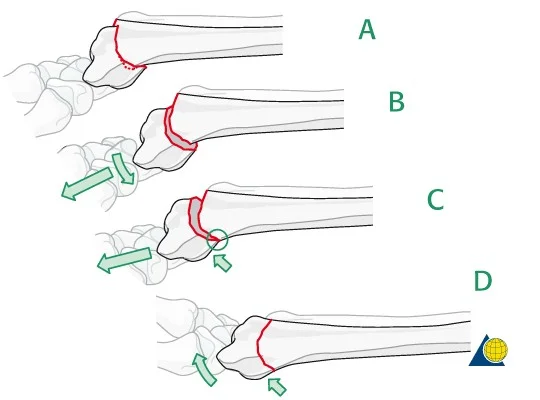 | Requires skilled practitioner; not sustained. |
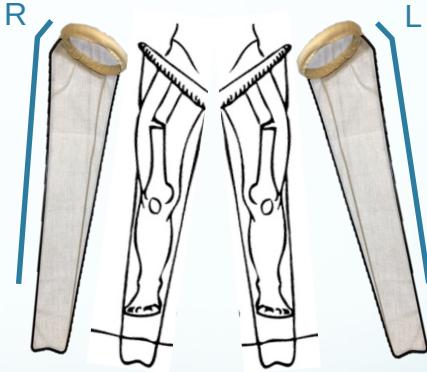
| Skin Traction | Reduction, maintaining alignment, immobilizing joints, pain relief. Primarily for muscle spasm, shortening, and overcoming gravity. | Children (<2 years for Gallows traction, max 10-12 kg) and temporary management in adults (<3 weeks duration, <4.5 kg weight limit). | Easy to apply; no risk of bone infection or epiphyseal plate injury. |     Types: Gallows Traction:   Fixed Traction (Thomas Splint):   Balanced Traction (Thomas Splint): 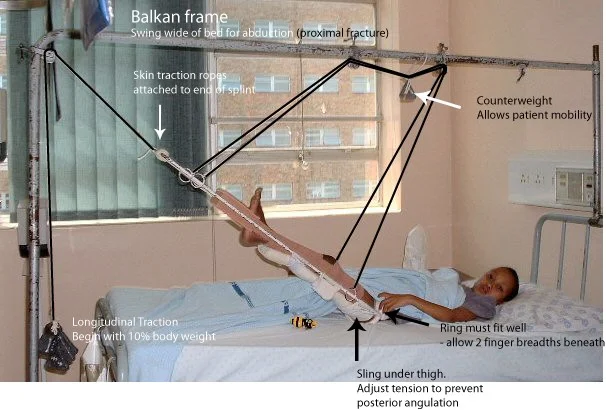 Cervical Skin Traction:   | Costly due to hospital stay; hazards of prolonged bed rest (thromboembolism, decubitus ulcers, pneumonia, UTI, depression); requires meticulous nursing care. Contraindicated with skin damage (DM, varicose ulcers), wounds, marked swelling, circulatory problems. |
| Skeletal Traction | Strong, sustained pulling force for fracture reduction and alignment, pain relief, and overcoming muscle spasms. Used when stronger force is needed or for longer duration. | Adults (when surgery is not possible/desirable), when >4.5 kg weight is needed, or traction needed for >3 weeks. Common pin sites: upper tibia, femoral condyle, calcaneum, skull. | Reduces and maintains limb length and alignment; maintains reduction; reduces pain and muscle spasm. | 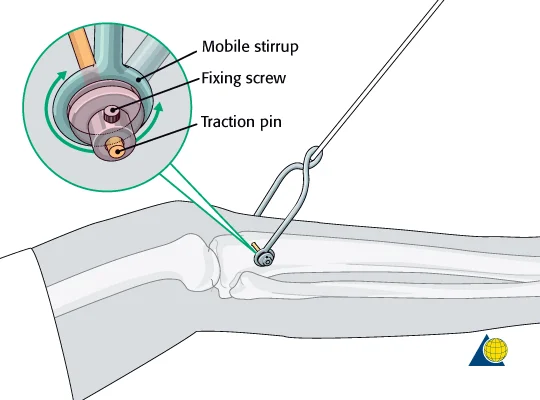 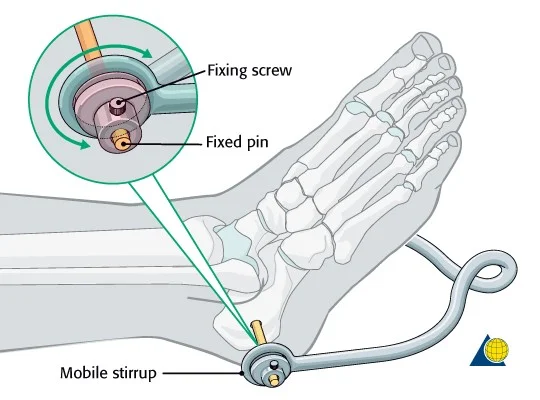 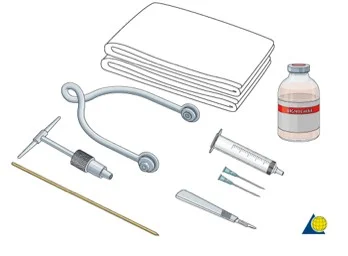 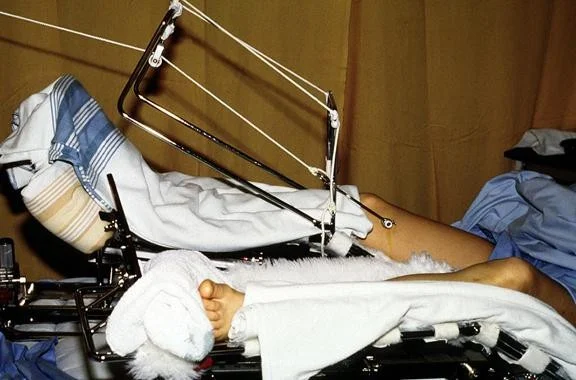   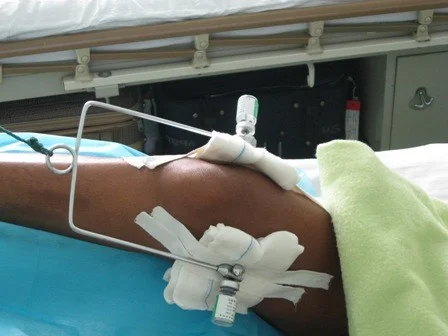   | Infection; over-distraction; nerve damage (from heavy force or direct injury during insertion, e.g., common peroneal nerve); bone fragmentation/break; pin breakage. |
Fixed Skin Traction on Thomas Splint
https://www.youtube.com/watch?v=wE21tHW7CPo
| Procedure Category | Steps | Key Considerations … | Attachments (for reference) |
|---|---|---|---|
| Skin Traction Application | 1. Two persons required. | Manual traction is performed by an assistant to realign the limb and reduce pain. The assistant continues pulling throughout the entire procedure. |  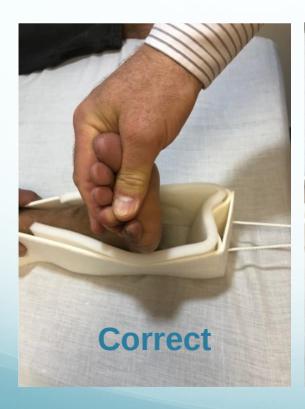 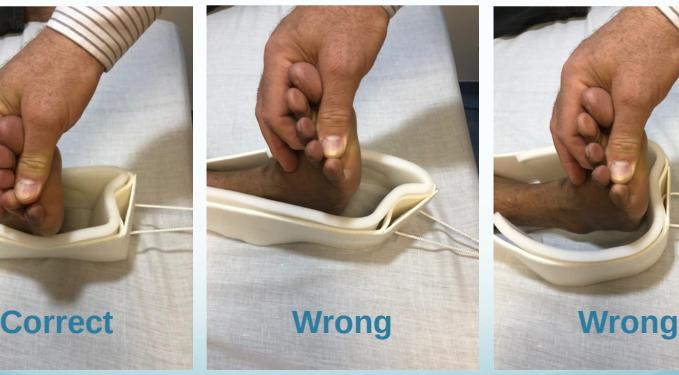 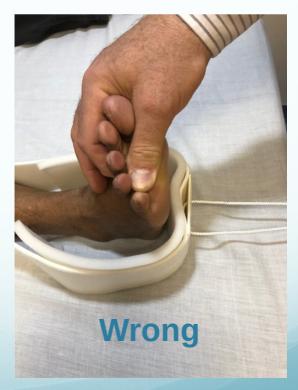  |
| 2. Apply skin traction with centralized end piece. | Ensures correct traction pull. Keep traction tape away from heel skin (5cm) to prevent skin breakdown and discomfort. |  | |
| 3. Smoothly apply traction tape on skin. | Ensures even pressure and adhesion. The upper part of the traction tape should be below the fracture level. | ||
| 4. Apply bandage evenly with 50% overlap. | Bandage should not be too tight or too loose. Prevents pressure on the fracture site. |   | |
| Thomas Splint Application | 1. Prepare splint by adding bandage or foam pads between medial and lateral bars. | Provides comfort and prevents skin irritation. |  |
| 2. Apply Thomas splint correctly while assistant continues pulling. | Ensures proper alignment and immobilization. Position the angulated bar on the lateral side for correct orientation and effective traction. |    | |
| 3. Push the ring as high as possible. | Allows for maximum leverage and traction. |   | |
| 4. Pull rope and fix to the end of Thomas splint. | Applies the fixed traction. |     | |
| 5. Apply a pillow under the splint (no pressure under the heel). | Prevents pressure sores on the heel. |  | |
| 6. Check tightness of rope. | Ensures appropriate and effective traction force. |  |
Application Procedure
- Describe this method of treatment
- Skin traction
- On Thomas splint
- Fixed at the end of splint
- What is this method used for?
- Immobilization of fracture femur
- For transportation to avoid complications
- What are the limitations of skin traction?
- Skin lesions/wound
- Weight needed above 10 Lbs. (4-5 Kg.)
- Duration more than 3 weeks What are the possible complications of skin traction?
- Skin problems: blisters, ulcers, allergies…
- Prolonged immobilization of patient:
- Bed sores
- UTI, chest infection
- Depression
- Cost of prolonged hospitalizatio
Overview of Fixed Skin Traction
Description: Skin traction applied on a Thomas splint, with the traction fixed at the end of the splint. Purpose: Immobilization of a fractured femur, particularly for transportation, to avoid complications.
Limitations of Skin Traction
- Presence of skin lesions or wounds.
- Required weight above 10 lbs. (4-5 kg).
- Duration exceeding 3 weeks.
Possible Complications of Skin Traction
- Skin problems: blisters, ulcers, allergies.
- Complications from prolonged immobilization:
- Bed sores
- Urinary Tract Infections (UTIs), chest infections
- Depression
- Cost of prolonged hospitalization
Additional Information:
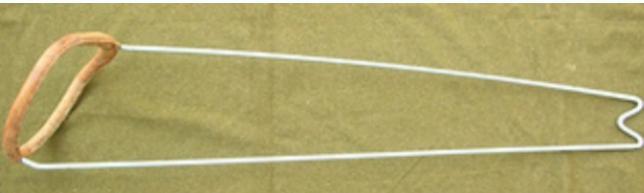
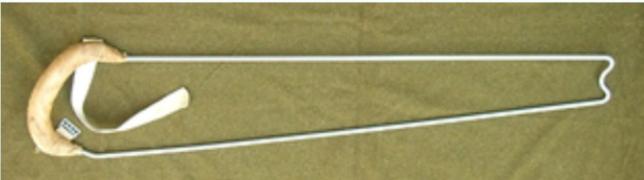
- Thomas Splint Indications: Immobilization of femur fractures for patient transportation; application of fixed traction.
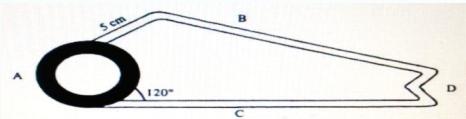
- Thomas Splint Parts: A. Ring, B. Lateral bar (angulated), C. Medial bar.
- Thomas Splint Types: Complete ring (original design) and Half-ring (easier to apply).
- Modern Traction Splint: Easily holds a lower limb with straps and simplifies fixed traction application.
Skeletal Traction: OSCE
https://www.youtube.com/watch?v=pbHRbdOsvH4
| Category | Detail … | Image Reference |
|---|---|---|
| Definition | Inserting a metal (Steinman pin) into the bone and applying traction on it. | 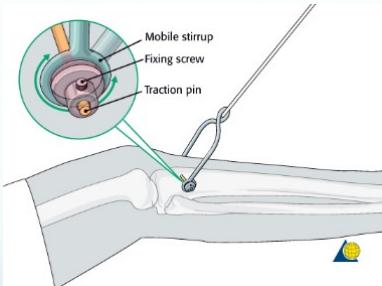 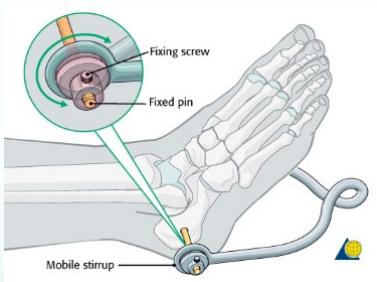 |
| General Technique Overview | 1. Sedation (if needed) 2. Antiseptic skin preparation and draping 3. Local anesthesia 4. Stab incision 5. Pin insertion with T-handle/drill 6. Second stab incision (exit site) 7. Sterile gauze application 8. Stirrup and traction application (10% of patient’s body weight) |      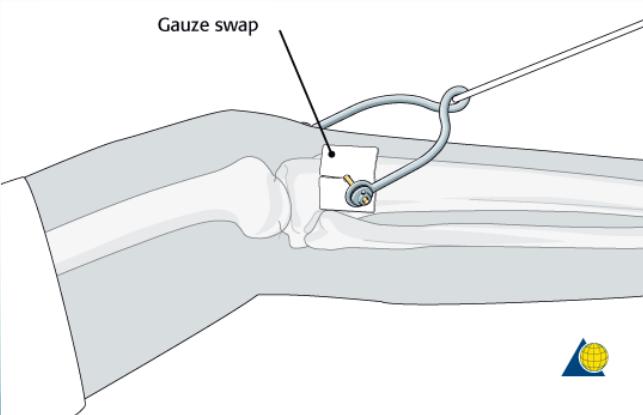 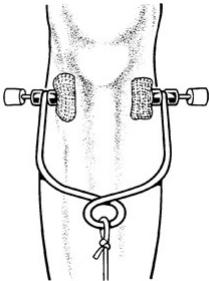  |
| Equipment Needed prior to starting | - Disinfectant - Sterile towels - Needles and Syringe - Local anesthetic (e.g., 5 ml of 2% lignocaine) - Scalpel with pointed blade - Sharp pointed Steinmann pin - T-handle - Stirrup |  |
| Entry Points | Proximal Tibial Site: - Insertion: Laterally at a point 2cm distal and 2cm posterior (lateral) to the Tibial tuberosity. - Exit: Medially. - Avoids: Injury to the common peroneal nerve. Distal Femoral Site: - Insertion: Medially at level of upper patella in-line with mid-femur. - Exit: Laterally. - Avoids: Popliteal vascular damage and intra-articular injury. | Proximal Tibial Site: 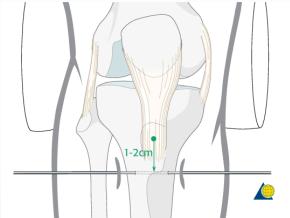 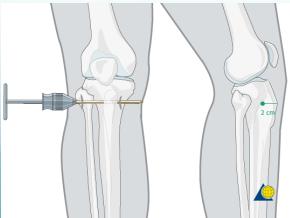  Distal Femoral Site:  |
Splints & Braces
| Splint/ Brace Type | Region | Indications | Application Notes … | Attachments |
|---|---|---|---|---|
| Figure-of-8 Brace | Upper Limb | Immobilization of clavicle fractures | Wear with shoulder pressing back in an arch position; can use ready-made brace or foam sling. |  , ,  , ,  |
| Arm Sling | Upper Limb | Shoulder support in shoulder and clavicle injuries; forearm support (in cast) | Shoulder adducted, elbow flexed 90°, wrist at neutral position; supports the elbow and overcomes gravity. |  ] ] |
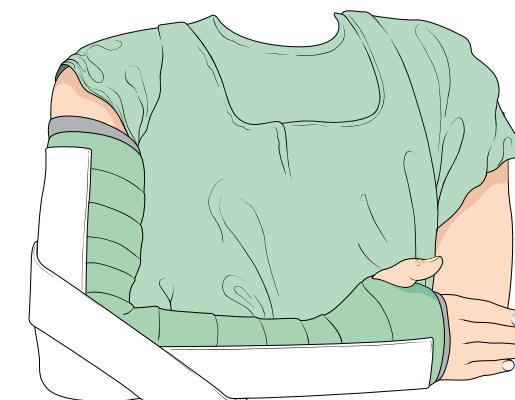
| Arm Sling with Shoulder Immobilizer | Upper Limb | Shoulder support after major surgeries | Shoulder adducted, elbow flexed 90°, wrist at neutral position; sling supports shoulder by applying waist sling keeping shoulder adducted. |  |
| Forearm Sling | Upper Limb | Support in humerus fractures (allowing traction by gravity); forearm support (in cast) | Shoulder adducted; elbow not supported to allow gravity to pull down on humerus. |  , ,  |
| Back Supports | Spinal | Limiting motion of spine to enhance healing (after surgery or in stable fractures); reduces back pain and discomfort (in back sprains/muscle pain) | Types: soft or rigid with rods; thoraco-lumbar, lumbar, lumbo-sacral. Precaution: Long-term use causes muscle weakness. |  , ,  , ,  |
| Soft Cervical Collar | Spinal | Partial support of cervical spine and neck muscles; muscle spasm, post-operative, nerve root entrapment syndrome in cervical spine | Choose proper size (height/length); apply reasonably tightly under the chin. Precaution: Long-term use causes muscle weakness. |  |
| Rigid Cervical Collar | Spinal | Trauma emergency (suspecting neck injuries); head/facial/forehead injuries, neck pain, unconscious patients | Adjust to proper height; use traction to support neck while applying; apply around neck with chin piece fitting well; optional anterior opening for tracheostomy. |  , ,  , ,  , ,  , ,  , ,  , ,  |
| Knee Immobilizer | Lower Limb | Immediate after knee injuries (instability, patellar fractures, haemarthrosis); post knee surgery | Apply with wider end on upper thigh; ensure opening is on the patella; apply tightly from up downwards. |  , ,  |
| Hinged Knee Splint | Lower Limb | Used in collateral ligament injuries | Supports and stabilizes injured knee (prevents varus/valgus movements); allows flexion/extension (hinged metal supports on sides). |  , ,  , ,  , ,  |
| Ankle Foot Orthosis (AFO) | Lower Limb | Foot support for foot drop | Wear shoe on top of brace. |  , ,  |
| Silicone Spacer/Splint | Lower Limb | Adolescent hallux valgus (cosmetic complaint); initial treatment choice in mild cases | N/A |  , ,  |
| Malleable Finger Splints | Hand and Wrist | Phalangeal fractures; sprained interphalangeal joints | Flexion of MCP joint and extension of interphalangeal joints. |  , ,  , ,  , ,  |
| Mallet Finger Splint | Hand and Wrist | Mallet finger injury (rupture/avulsion of extensor tendon at distal phalanx) | Finger must be fully extended in the DIPJ. |  , ,  , ,  |
| Wrist Splint | Hand and Wrist | Wrist support after minor soft tissue injuries and sprains; wrist immobilization for carpal tunnel syndrome (pre/post surgery); temporary intermittent support after cast removal post fractures | Rigid/metal part with a bend at the volar aspect; wrist immobilized in slight dorsiflexion. |  , ,  |
| Thumb Splint | Hand and Wrist | Thumb support after minor soft tissue injuries and sprains; Tenosynovitis (immobilizing thumb to reduce pain and inflammation of tendons) | Rigid/metal part on the dorsum of the thumb. |  , ,  |
Implants & Nail types
| Description | Specific Details … | Image Links |
|---|---|---|
| K-wire (Kirschner Wire) | Indications: Pediatric fractures, small bone fractures in adults. Advantages: Easy to apply/remove. Disadvantages: Not stable alone, risk of infection. |  , ,  , ,  , ,  , ,  , , 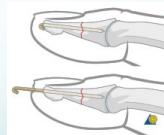 |
| Tension-band Wires | Indications: Patellar and olecranon fractures, possible in malleolar fractures. Application involves K-wires as a base. |  , , 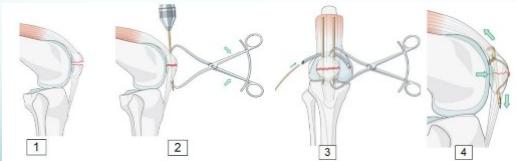 , ,  , ,  , ,  |
| Orthopedic Screws | Material: Stainless steel or Titanium. Thread design varies by bone type (Cortex vs. Cancellous screws). Available in various sizes and lengths. | 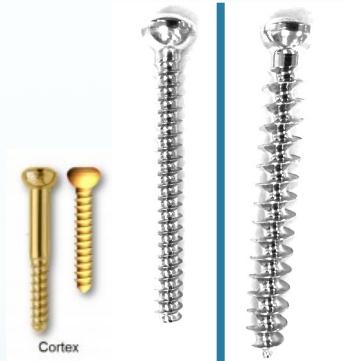 |
| Screw Types - Fully vs. Partially Threaded | Fully threaded: Provides purchase. Partially threaded: Provides lagging (compression). |  , ,  |
| Screw Types - Partially-threaded Screws | Function: Achieve compression across fracture site (lag screw). Fully threaded can compress if cortex is over-drilled. | 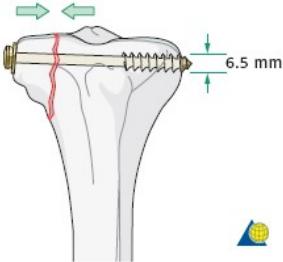 , , 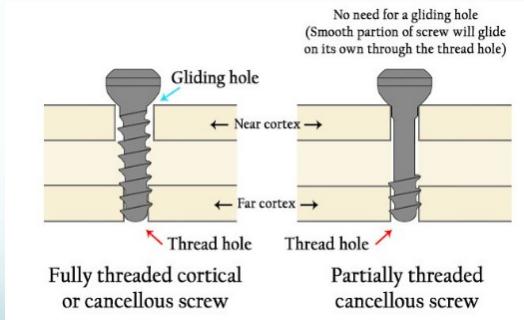 |
| Screw Types - Cannulated Screws | Feature: Hollow, inserted over a wire for accurate placement in minimally invasive techniques. |  , , 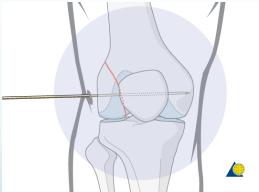 , , 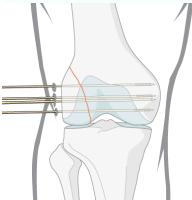 , , 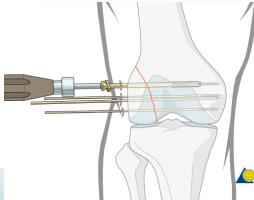 , , 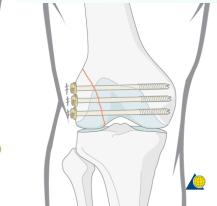 |
| Screw Types - Locked-head Screws | Feature: Threaded heads to anchor to special plates. Advantage: Good for osteoporotic bone, preserves periosteal blood supply by not pressing on bone. |  , ,  |
| Plate and Screws | Indications: Metaphyseal fractures, forearm fractures, complex long bone fractures. Advantages: Anatomical reduction. Disadvantages: Limits early weight-bearing, exposes fracture site. |  |
| Plate Functions | Functions: Compression, Bridging, Protection, Buttress. | 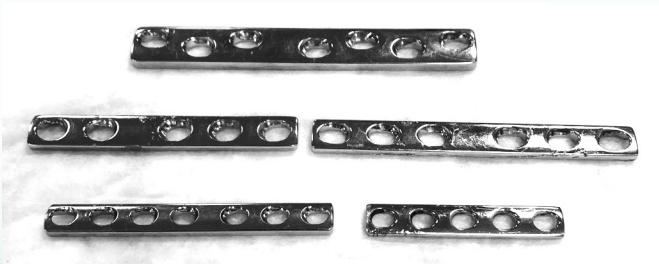 |
| Plate Types - Dynamic Compression Plate (DCP) | Feature: Oval holes designed for dynamic pressure between fracture fragments. Use: Simple diaphyseal fractures. |  , , 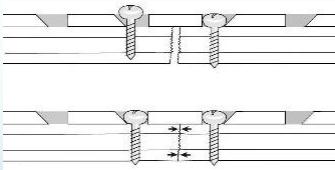 , ,  |
| Plate Types - Bridging Plate | Feature: Provides stable fixation, maintains length, alignment, and rotation. The fracture site is undisturbed. |  |
| Plate Types - Semi-tubular Plate | Design: Shaped like half a tube. Indications: Lateral malleolus/fibula, metacarpals/metatarsals. |  , ,  , ,  |
| Plate Types - Locked Compression Plate (LCP) | Feature: Combination hole (oval and serrated). Advantages: Resists screw loosening/pullout, good for osteoporotic bone, preserves periosteal blood supply. Indications: Osteoporotic bone fractures, bridging comminuted fractures. |  , ,  , ,  , ,  |
| Plate Types - Buttress Plate (T-Plate/L-Plate) | Indications: Lateral or medial tibial plateau fractures, distal radius fractures. |  , ,  , ,  , ,  |
| Plate Types - Anatomical Plates with Locked Screws | Indications: Metaphyseal fractures. Advantages: Anatomically contoured, excellent fixation in metaphyseal areas and osteoporotic bone. |  , ,  , ,  |
| Dynamic Hip Screw (DHS) | Indications: Fixation of intertrochanteric fractures. | 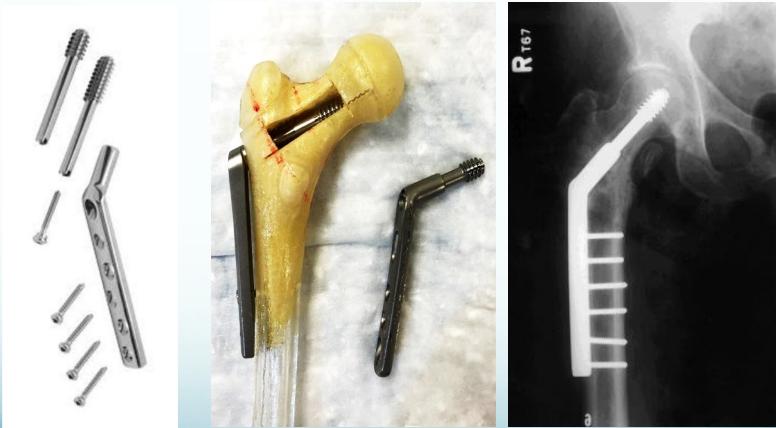 |
| Inter-locking Nail | Indications: Fractures of long bones. Advantages: Minimally invasive, preserves fracture hematoma, allows early weight-bearing on lower limb. |  , ,  , ,  , ,  |
| Orthopedic Staples | Indications: Foot surgery, epiphysiodesis for lower limb deformity correction. | 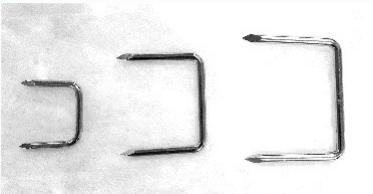 , ,  |
OSCE Procedure: Upper Limb Cast Application
https://www.youtube.com/watch?v=kmMgML5Hp0Y&t=260s
| Phase | Step | Action |
|---|---|---|
| 1. Preparation | Pre-procedure | 1. Introduce yourself, confirm patient identity, and explain the procedure, including risks and benefits, to obtain informed consent. 2. Ask about allergies to casting materials. |
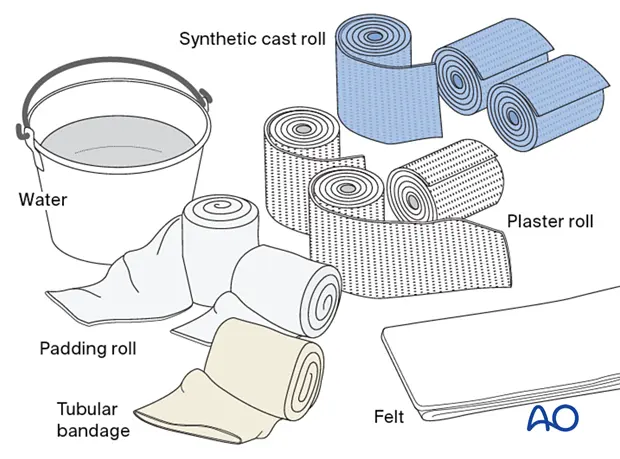
| Gather Equipment | Assemble all necessary materials on a trolley: • Stockinette • Padding roll (e.g., Soffban®) • Casting material (Plaster of Paris or Synthetic) • Bowl of water • Bandage scissors, crepe/conforming bandage • Sling, optional felt for bony prominences. | |
| Prepare the Patient | 1. Position the patient comfortably (usually seated). 2. Expose the limb adequately. 3. Have the limb held in the specific required position. Correct positioning is critical for functional outcome. • Above Elbow Cast: Elbow at ~90° flexion. • Colles’ Cast: Wrist in slight palmar flexion and ulnar deviation. | |
| 2. Application | 1. Apply Stockinette | Apply a tubular stockinette over the limb, ensuring it is smooth and extends beyond the planned cast margins. |
| 2. Apply Padding | 1. Apply the padding roll (wadding) over the stockinette using a 50/50 overlap technique. 2. Apply extra felt padding over bony prominences like the ulnar styloid. | |
| 3. Prepare & Apply Casting Material | 1. Submerge the plaster or synthetic roll in water until bubbling ceases. Gently squeeze out excess water. 2. Begin applying the roll, overlapping by 50% for even thickness. For wrist casts, roll from “within out” through the thumb grip. For synthetic casts, it helps to cut a small curve in the bandage to navigate the thumb web-space smoothly. 3. For a slab, measure and create a 5-8 layer slab, dip it, and apply it to the limb. Secure it with a pre-soaked and squeezed-out crepe bandage to prevent shrinkage and constriction. | |
| 4. Mould the Cast | While the material is setting, use the palms of your hands (not fingers) to mould the cast to the limb’s contours. For wrist casts, mould well into the palm to support the transverse metacarpal arch. | |
| 3. Finishing & Post-Application | 1. Trim the Cast | Before it fully hardens, trim the cast edges to allow full movement of uninvolved joints. • Below Elbow: Expose the palmar crease for full finger flexion and ensure the thumb is completely free. The cast should end two fingers below the elbow crease. • Above Elbow: The cast should extend from the axilla to the knuckles. |
| 2. Finish the Edges | Fold the excess stockinette back over the cast edges and secure it with a final strip of plaster or adhesive tape. | |
| 3. Final Checks | 1. Perform a full neurovascular assessment distal to the cast (check for the “5 Ps”: Pain, Pallor, Pulselessness, Paresthesia, Paralysis). 2. Rest the limb on a pillow or in a sling for elevation. | |
| 4. Patient Education | Provide clear verbal and written instructions on: • Cast care (keep dry, do not insert objects). • Warning signs requiring immediate medical attention. • Exercises for fingers, shoulder, and other free joints. • Arrange a follow-up appointment. |

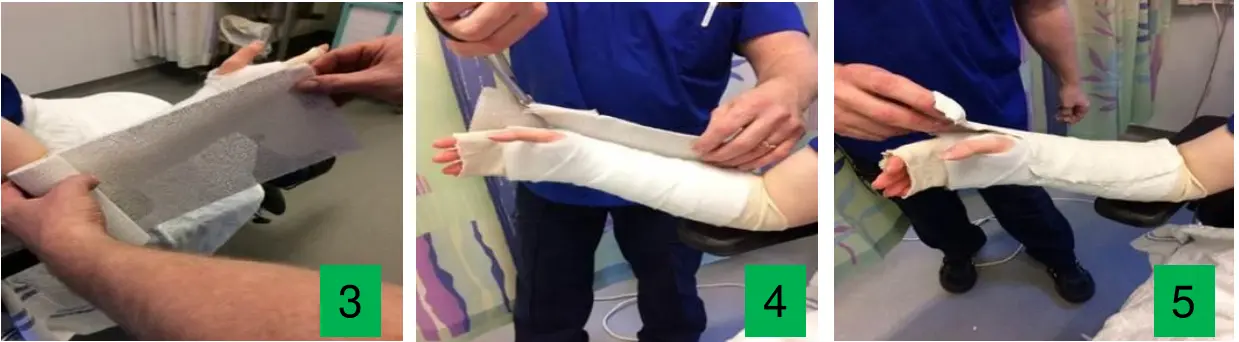

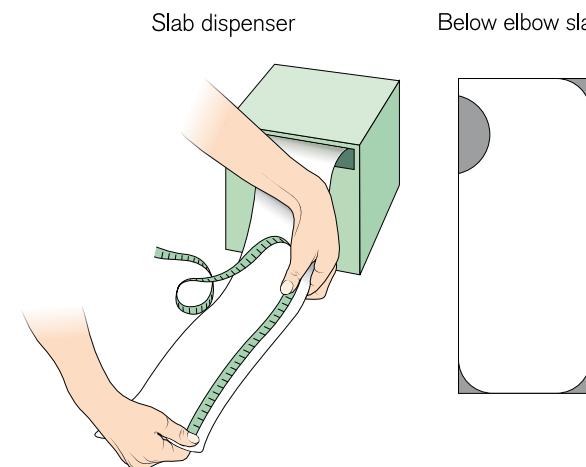
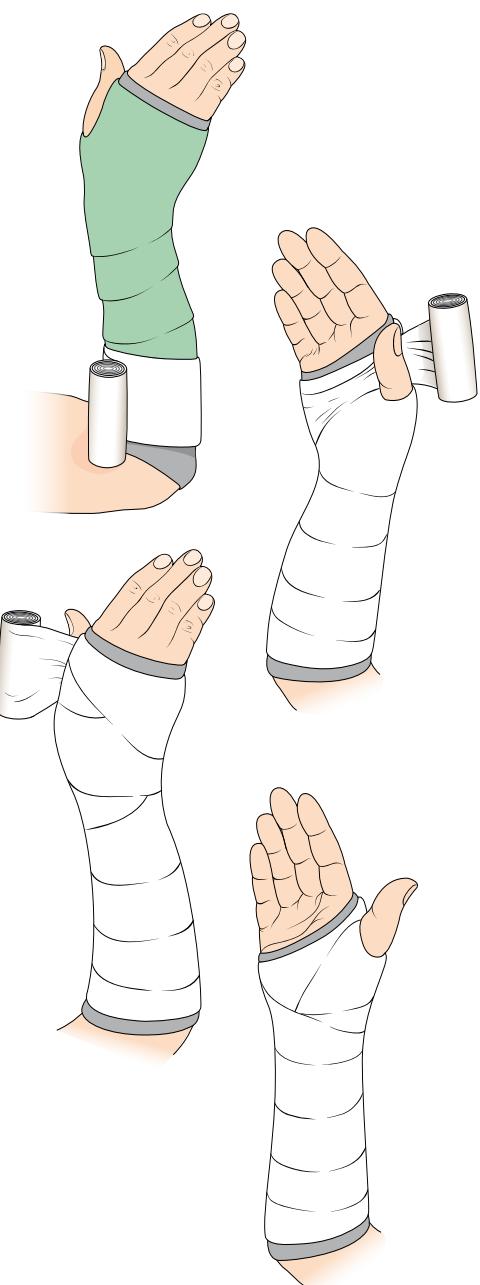






Cast of upper limb
Materials
-
Plaster of Paris (Gypsum)


-
Synthetic Fiberglass



Order of appliance
- Tubular Bandage
- (Optional) Felt padding for specific areas
- Padding Roll (Wadding)
- (Dip casting material in) Water (for activation)
- Plaster Roll OR Synthetic Cast Roll (applied and molded)
Exam
Examination of Shoulder
| Item | Procedure … | Related Attachments |
|---|---|---|
| Opening | • Greet the patient and Introduce yourself. • Ensure proper hygiene and Ensure adequate privacy. • Take permission and Expose the patient. • Note general position, swelling, etc. | |
| Look | • Inspect in all sides for scars, discolouration, swelling, and deformities from the front, sides, top, and back. • Look for muscle wasting of supraspinatus and infraspinatus muscles • Compare both deltoids; comment if they seem symmetrical. • Check for winged scapula. General on patient: Position, Major deformity- swelling, Extra (cast, splint, traction, dressing). Anatomic local: Skin, Subcut. (LN, veins, nerves, tendons), Muscles (bulk, wasting, twitches), Bones (landmarks, swelling, angulation and deformity), Joints (position, swelling, redness). Inspection from multiple angles: Anterior, Posterior, Lateral, Above, Axilla. Atrophy check (with patient sitting): supraspinatus fossa, infraspinatus fossa, deltoid. |       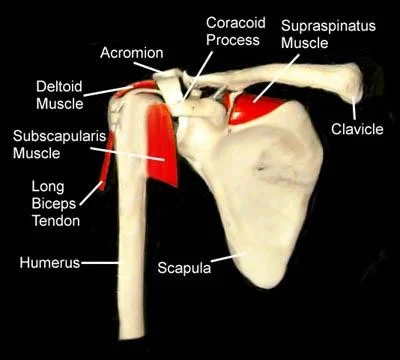 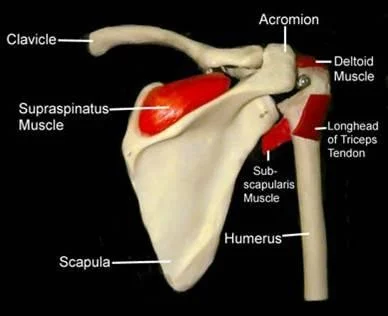       |
| Feel | • Temperature: Compare both sides (proximal to distal) and comment if symmetrical. • Tenderness: Palpate for tenderness (always compare to the left shoulder) starting at: • Sterno-clavicular (SC) joint • Clavicle • Acromio-clavicular (AC) joint • Greater Tuberosity (GT) & Biceps tendon • Scapular spine • Palpate and compare rotator cuffs (supraspinatus, infraspinatus) and deltoids. General: Tenderness (Generalized/specific), Temperature (compare distal/proximal, Rt/Lt). Anatomic: Skin, Subcut., Muscle (tone, bulk, twitches, gaps, tenderness), Bone (tenderness, mass, crepitus, landmarks: Sternoclavicular, Acromioclavicular, Coracoid Process, Greater Tuberosity, scapular spine, and scapula), Joint (swelling, effusion, crepitation, synovial thickening, joint line tenderness). Specific areas: Acromio-clavicular Jt., Bicipital groove. |   |
| Move | • Ask the patient to stand up. • Active ROM: First Assess range of motion - screen for pain. Ask to perform: • Forward flexion / Extension • Abduction / Adduction • External / Internal rotation • Comment on the motion (e.g., “full active motion, no need for passive”). • Passive ROM: If active motion is limited, assess passively. • Examine joints above and below (e.g., C-spine, elbow). Movement Directions (normal range): Abduction (150°), Forward flexion (180°), Extension (45°), External Rotation (90°), Internal rotation (90°). Flexion / Extension: Look at range, smoothness, painful motion. Abduction / Adduction: Shoulder joint motion is associated with Scapulo-thoracic motion. The first 20°-30° of abduction should not require scapulo-thoracic motion. Note the arc of painful movement (Painful Arc: Supraspinatus, Rotator cuff, Acromio-clavicular). Internal / External Rotation: Apley’s Scratch Test. |           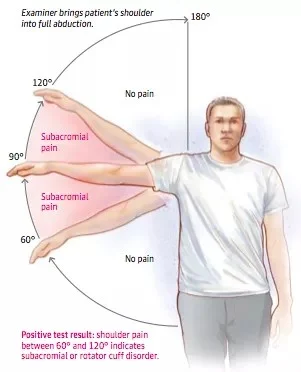  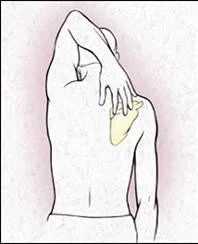   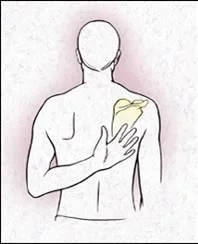  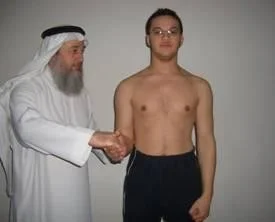  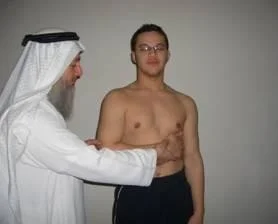      |
| Special Tests | Rotator Cuff Power (compare both sides): • Instability (Bankart): Apprehension Test (abduct and externally rotate arm, apply anterior pressure, watch patient’s face). • Supraspinatus (Empty Can Test): Flex shoulder to 30° with thumbs down; ask patient to resist. • Impingement tests: Neer’s Impingement Test, Hawkins’ Impingement Test. or neer’s rotator cuff + abduction resistance for supraspinatus • Infraspinatus: Ask patient to perform external rotation against resistance (elbows at 90°). • Subscapularis: Ask patient to perform internal rotation against resistance OR use the Lift-Off Test. • Teres Minor: Ask patient to perform external rotation against resistance in 90° of shoulder abduction. • Biceps Tendon: Speed’s Test (resisted shoulder flexion with elbow extended and supinated) OR Yergason Test. • Deltoid: Axillary nerve assessment: Motor (active abduction - then drop test- Deltoid), Sensory (upper lateral aspect of arm). Serratus Anterior - Scapular Winging; long thoracic nerve: push against wall - observe back • AC Joint: Cross Body Adduction Test. • Muscle power tests: Abductors/Adductors, Internal/External Rotators, Serratus Anterior (winging), Biceps Brachii. | Apprehension test:    Neer’s Impingement Test: 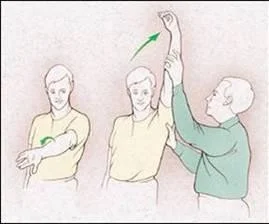  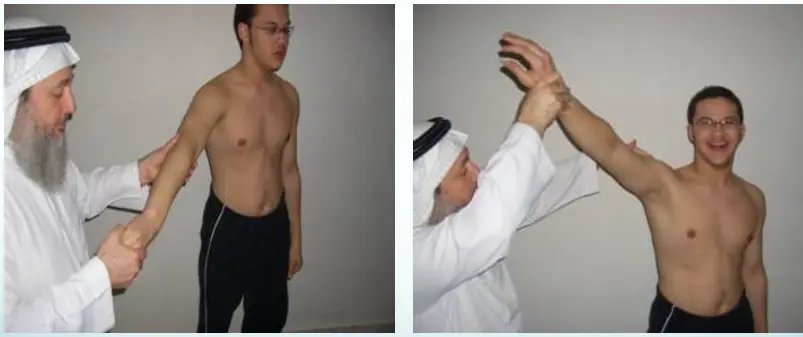 Yergason Test: 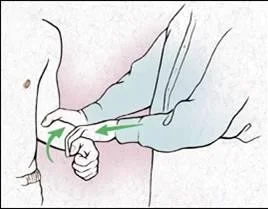 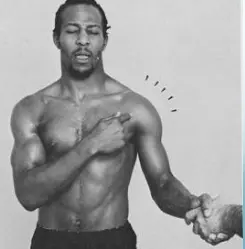 External / Internal Rotators Strength Test:    Supraspinatus Test:   Serratus Anterior - Scapular Winging; long thoracic nerve:   Biceps Tendon & Ruptured long head:  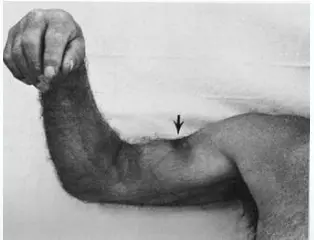 |
| Overall | End your exam with full neurovascular examination, and systemic examination • Thank patient, cover, document. Maintain a professional and empathetic attitude with the patient. |
Case: Adhesive Capsulitis (Frozen Shoulder)
Clinical Scenario
- Patient: 55-year-old male, diabetic
- Complaint: Pain and restriction of shoulder movement
Physical Examination Findings:
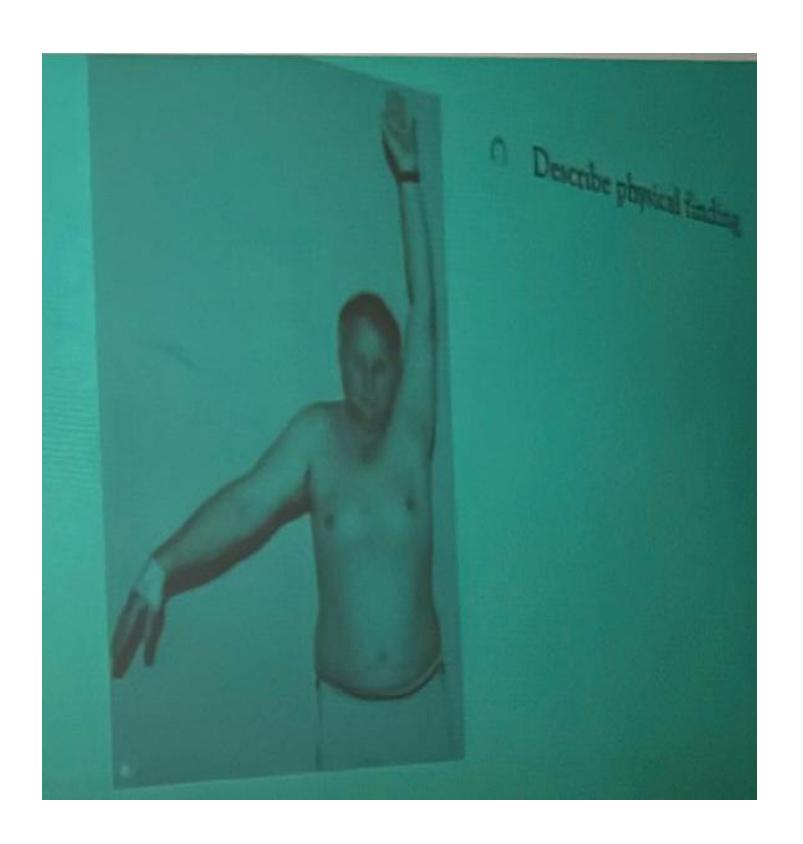
Assessment Questions
Q1: Describe the physical finding?
- The patient is unable to raise his right hand above his head
Q2: What is your differential diagnosis?
- Adhesive capsulitis (Frozen Shoulder) - Primary diagnosis
- Acromioclavicular arthritis
Q3: What is the treatment for such a case?
- Steroid injection
- Physiotherapy
- Arthroscopic release
Section 3: Shoulder Pathology & Examination
Questions 17-20: Shoulder Injuries and Tests
Clinical Scenario: 45 years old male fell from height and landed on his shoulder and presented to your clinic with painful shoulder.
Q17: What is the following test name and what does it test?
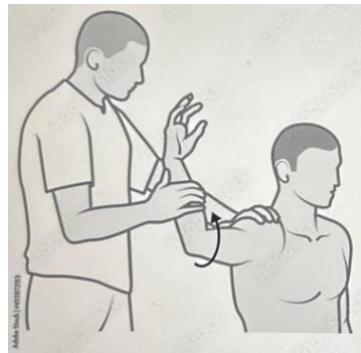
Apprehension test for anterior shoulder instability
Q18: What is the following test name and what does it test?
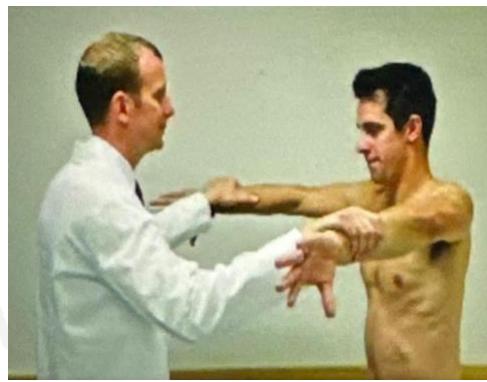
Empty can test for Supraspinatus power
Examination of the knee
Knee Exam
https://www.youtube.com/watch?v=17ZKya9yR2Y
https://www.youtube.com/watch?v=oyKH4EYfJDM
| Item | Procedure | Purpose/ Indication … | Attachment Links | Positive Finding/Interpretation |
|---|---|---|---|---|
| Opening | Introduction, Privacy, Permission & Exposure | Initial patient interaction and setup | ||
| Deformity and Extra | Initial visual assessment for gross abnormalities | |||
| Look | Compare both limbs, Skin, Muscle bulk, bony landmarks, hair distribution | Assess symmetry, signs of trauma, inflammation, muscle atrophy, structural changes | Visual examples - Skin, Muscle, Bone, Joint:           | Swelling, scars, discoloration, hair changes, muscle wasting, bony protrusions, angulation, redness |
| Back of knee | Assess for posterior aspect abnormalities, such as Baker’s cyst | Posterior aspect:  | Swelling, tenderness, masses in the popliteal fossa | |
| Feel | Tenderness (General, Localized): Quadriceps, Patella, Patellar tendon, Tibial tuberosity, Origin, and insertion of collateral ligaments, ACL, MCL | Identify areas of pain and inflammation in relevant structures | Tenderness - General: 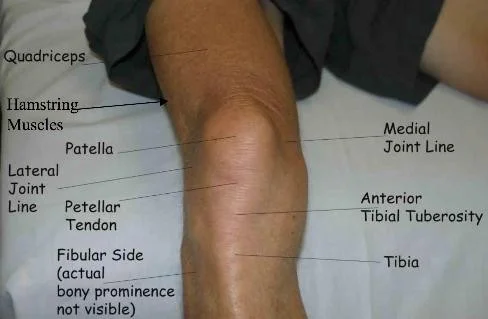 Tenderness - Localized: 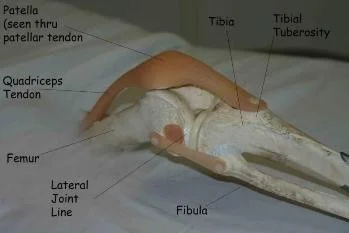 Medial Structures (Tibial Tuberosity, Joint Line, Medial Tibial Condyle, Patella, Medial Femoral Condyle, Joint Space, MCL): 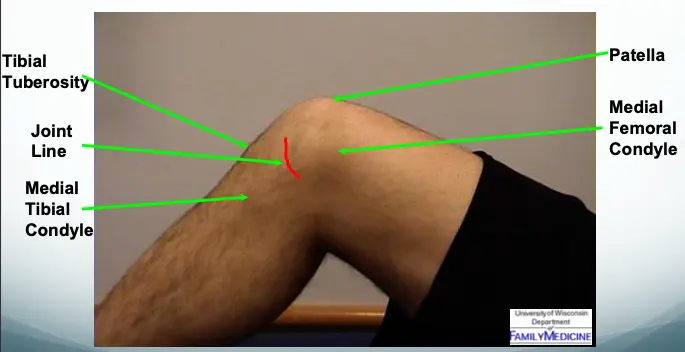 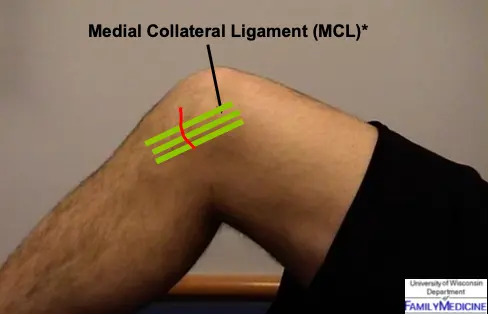 Lateral Structures (Quadriceps, Patella, Tibial Tuberosity, Head of Fibula, LCL, Lateral joint line): 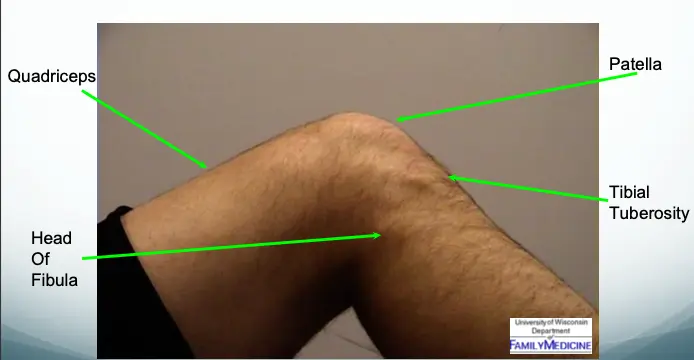 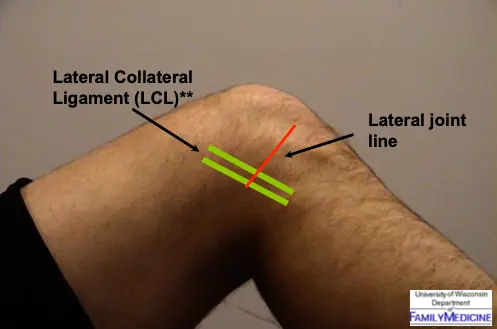 | Localized pain upon palpation |
| Joint-line tenderness, medial and lateral | Assess for meniscal or collateral ligament pathology | Joint lines:  | Pain upon palpation along the joint line | |
| Temperature: compare R & L, distal & proximal | Identify signs of active inflammation or infection | Temperature Comparison:  | Increased warmth compared to contralateral side or unaffected areas | |
| Back of knee, baker’s cyst and tenderness | Further assess posterior knee for specific pathologies | Tenderness or swelling indicating a Baker’s cyst or other posterior pathology | ||
| Anatomic Examination: Muscle (Quadriceps) | Assess muscle tone, bulk, and tenderness | Muscle (Quadriceps):   | Abnormal tone, wasting, twitches, tenderness | |
| Anatomic Examination: Bone (Patella, Tibial Tuberosity, head of Fibula) | Assess bony landmarks for tenderness or deformity | Bone Landmarks:    | Tenderness, mass, crepitus, abnormal landmarks | |
| Anatomic Examination: Joint assessment | Assess for swelling, effusion, crepitation, and synovial thickening | Joint Assessment:   | Presence of swelling, effusion, crepitation, synovial thickening, joint line tenderness | |
| Move | Active first: General screening for pain, then passive | Assess patient’s voluntary range of motion and pain patterns | Limited or painful active movement indicating muscle or joint involvement | |
| Flexion & Extension (Normal: Extension: 0° → Flexion: 140°) | Quantify the knee’s range of motion | Extension:  Flexion:  | Reduced or excessive range of motion; “lacks X degrees of extension” | |
| Locking (due to mechanical blockage) | Assess for mechanical obstruction within the joint | Locking:  | Patient unable to fully extend or flex knee; suggests loose body or meniscal tear | |
| Hyper-extension | Identify excessive extension range | Hyper-extension:  | Greater than normal extension of the knee joint | |
| Effusion: Milking OR Patellar Tap | Detect presence and severity of joint fluid | Large Effusion visible:   Patellar Tap (Balloting):  | Minimal effusion: Fluid demonstrable with “milking.” Mild effusion: Fluid pushed away, then reappears. Moderate effusion: Fluid not pushed away. Moderate/severe effusion: Positive patellar tap (balloting). | |
| Special Tests | Collateral Ligaments: Varus and Valgus stress at 30 degree | Assess integrity of Medial (Valgus) and Lateral (Varus) Collateral Ligaments | Collateral Ligament Testing:     Collateral Ligament Testing Views:   Alternative Collateral Ligament Technique:  | Increased laxity or pain during stress, indicating ligamentous injury |
| Cruciate Ligaments: Overall indication | Assess integrity of Anterior and Posterior Cruciate Ligaments | Cruciate Ligaments Overview: 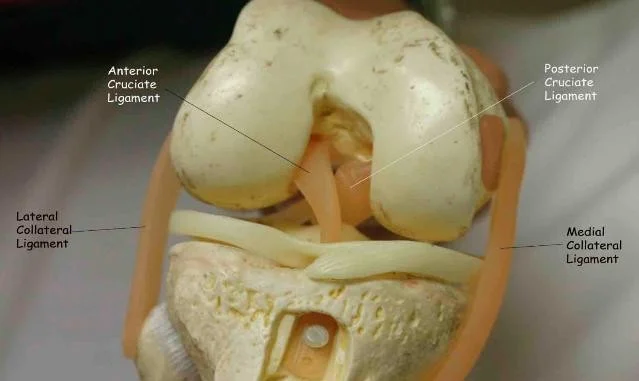 | ||
| ACL & PCL: Anterior/Posterior Drawer Test OR Lachman’s test OR Pivot Shift test | Assess integrity of Anterior and Posterior Cruciate Ligaments specifically | Anterior/Posterior Drawer Test:  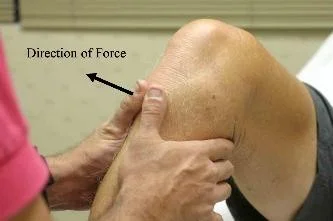  Lachman’s test:  | Excessive anterior or posterior translation of the tibia, indicating ACL or PCL injury | |
| PCL: Drawer test OR posterior Sag test | Specifically assess Posterior Cruciate Ligament integrity | Sagging sign:  | Posterior sagging of the tibia when the knee is flexed, indicating PCL tear | |
| Meniscus: McMurry’s test OR Medial & Lateral joint tenderness Apley grinding test | Assess for meniscal tears | McMurry’s test:  Apley grinding test:  | Click, thud, or pain during knee flexion, extension, and rotation during McMurray’s; pain during compression and rotation during Apley’s. | |
| Patellar test: Patellar Tracking Patellofemoral grind test Patellofemoral resistance test Patellar apprehension test | Assess patellar stability, patellofemoral pain, and chondromalacia | Patellar Tracking:   Patellofemoral Grind Test:  Patellofemoral Resistance Test:   Patellar Apprehension Test: 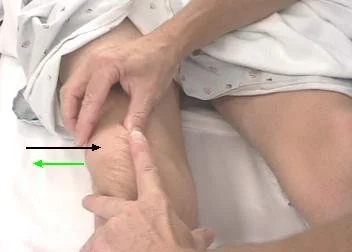 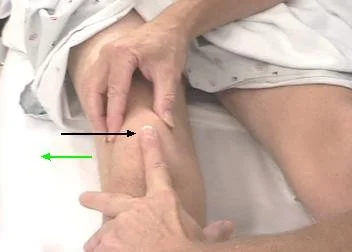 Summary of Patellar Tests:   | Patellar Tracking: Abnormal movement of patella. Patellofemoral grind test: Pain during compression and quadriceps tightening. Patellofemoral resistance test: Pain with resisted patellar motion. Patellar apprehension test: Patient apprehension/discomfort when patella is pushed laterally. | |
| Gait | Walking gait analysis (Normal, Antalgic, Lurch, Circumduction, High Step, Tip-toe) | Assess overall walking pattern and identify abnormalities Stance phase (60%) - Heel strike - Foot flat = mid-stance - Push off Swing phase (40%) (while foot is in air) - Acceleration - Mid-swing - Deceleration | Walking Gait Analysis:  Normal Gait Cycle: 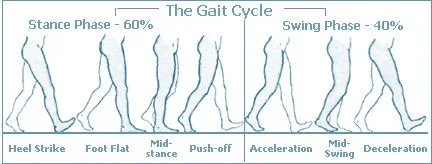 | Deviations from normal gait cycle (e.g., painful weight-bearing, limping, compensatory movements). Normal: Normal stance and swing phases Antalgic: Painful to weight-bear – short stance phase Lurch: Shortening – painless limping – normal stance period Circumduction: Stiff hip – motion of pelvis compensates High Step: Foot drop – more hip & knee flexion needed to free toes from ground Tip-toe: Heel off the ground |
| Overall | Attitude with patient | Professional demeanor and interaction |
Other Examinations
Examination of Spine
https://www.youtube.com/watch?v=5_txE56X2-8&pp=ygUZRXhhbWluYXRpb24gb2YgU3BpbmUgT1NDRQ%3D%3D
https://www.youtube.com/watch?v=pClOlpzo-Jc&pp=ygUZRXhhbWluYXRpb24gb2YgU3BpbmUgT1NDRQ%3D%3D
Spine Examination
- Perform a general spinal examination.
| Item | Procedure |
|---|---|
| Opening | • Introduction, Privacy, Permission & Exposure .Walk |
| Look | • General Position & Deformity • Skin, Muscles, and bony landmarks • Shoulder height from back • front, back, side: Standing OR Sitting . |
| Feel | • Tenderness, Temperature • Landmarks and muscles (central and paraspinal) • Sacro-iliac joints / Coccyx . |
| Move | • Forward flexion / Backward extension • R and L lateral flexion • R and L rotation . |
| Special Test (Ask to perform it & interpretation) | • Hoffmann’s sign: sitting ( Finger) • Spurling’s test: sitting (head) |
| • Adam Foreword test: standing (Scoliosis, can be done with forward flexion) | |
| Sciatic - 45 degree pain - passive dorsiflex below it when no pain , test for tenderness • Straight Leg Raise test: supine • SLR Confirmatory test | |
| • Patrick / FABER test: supine | |
| Femoral Nerve • Femoral Stretch test: lateral or prone - Extend and flex the knee | |
| Neurological (NOT IN CHECKLIST) | dermatome (fine, prick), myotome (power), reflexes, proprioception |
| General | • Attitude towards patient |
https://www.youtube.com/watch?v=pJxMHa6SCgU&pp=ygUXU3BpbmUgTmV1cm9sb2dpY2FsIE9TQ0U%3D https://www.youtube.com/watch?v=pClOlpzo-Jc&pp=ygULU3BpbmUgIE9TQ0U%3D
Back ROM & Neurological
This patient has back pain radiating down to his right leg. examine the back
| Item | Procedure | Technique … | Attachments |
|---|---|---|---|
| Look | General Examination | ||
| On Patient | Standing, tilting forwards with hand on left side of lower back |  | |
| Local (Back, Shoulder, Flanks, Chest) | Position (best in standing), Views (Posterior, Lateral, Anterior), Normal curves and alignment | 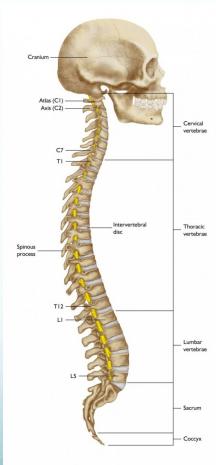 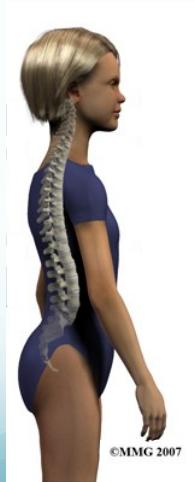   | |
| Major Deformity and Swelling Assessment | Shoulder height, Deformity, Flanks, Space between arm and trunk, Masses |   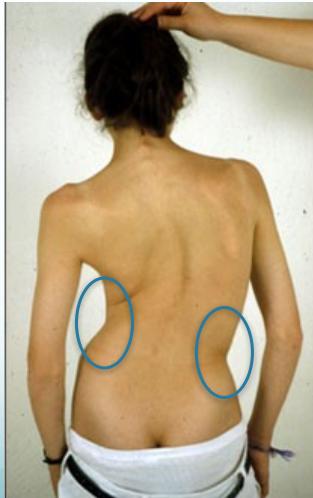   | |
| Extra Items | Support (braces, walkers, etc.), Dressings |  | |
| Anatomic Local Examination | |||
| Systematic Assessment | Skin (swelling, scars, color, hair, dryness), Subcutaneous (lymph nodes, veins, nerves, tendons), Muscles (bulk, wasting, twitches), Bones (landmarks, swelling, angulation, deformity), Joints (position, swelling, redness) |   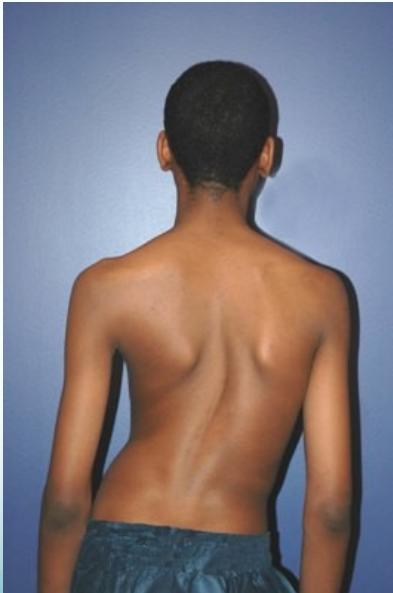  | |
| Proper Exposure |  | ||
| Comprehensive Look Assessment | 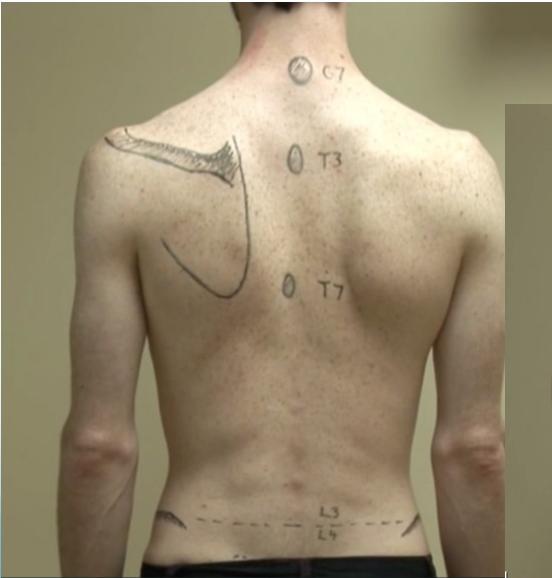 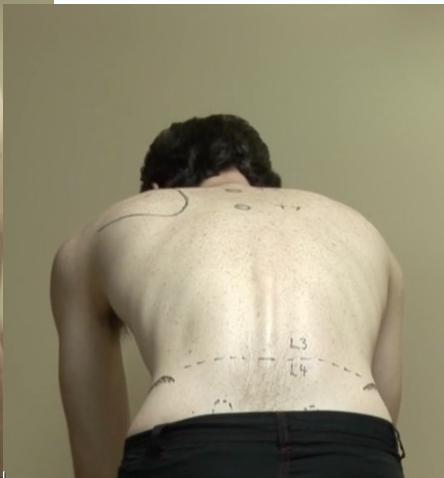 | ||
| Feel | Tenderness Assessment | Generalized (to start with), Specific (Spinous processes, Sacroiliac joints, Paravertebral muscles) | 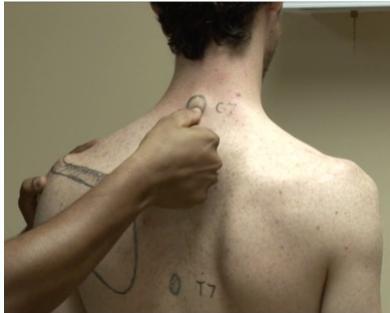 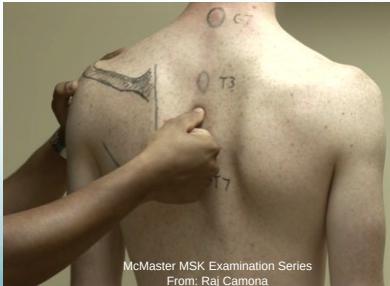  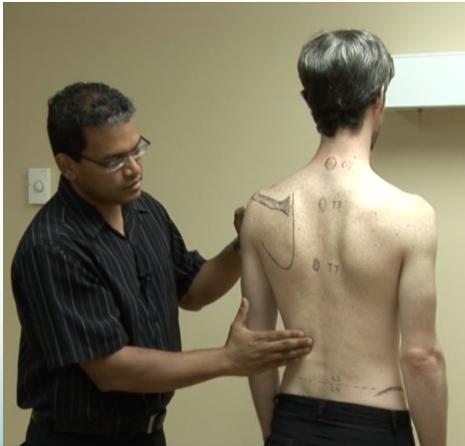 |
| Temperature Assessment | Compare distal/proximal, Compare right/left | ||
| Anatomic Assessment | Skin (dryness, scars), Subcutaneous (nodules), Muscles (Paravertebral: spasm, bulk, tenderness), Bones (landmarks: spinous processes, iliac crest, coccyx - tenderness, mass), Joints (sacroiliac tenderness) | ||
| Move | General Motion Assessment | Change of shape/deformity during motion, Smoothness of motion, Extent (Range) |  |
| Specific Movements | |||
| Flexion and Extension |       | ||
| R and L lateral flexion | Sideway Bending |  | |
| R and L rotation | Must be in Sitting position, help patient understand rotation movements |      | |
| Special Tests | Structural Assessment Tests | ||
| Adam’s Forward Test | 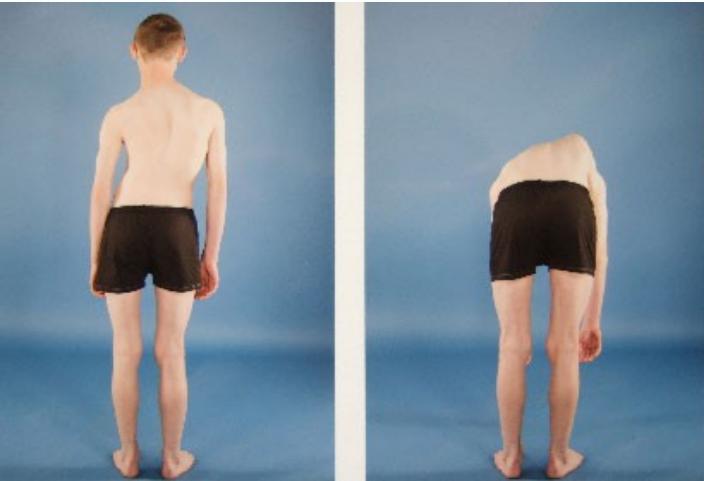 | ||
| Sacro-iliac stress | Figure of four / or other tests (FABER Patrick Test) |  | |
| Neurological Tests | |||
| Straight leg raise (Lasègue test) | In supine position, raise leg up with knee straight. Look and ask for pain. When pain starts, reduce leg raise, pain disappears. Now passively dorsi-flex ankle to reproduce pain. |     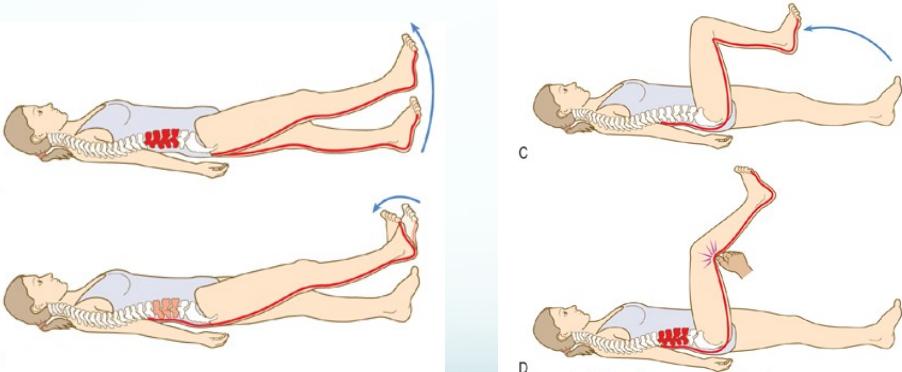 | |
| Femoral stretch | Femoral Stretch Test |   | |
| Neurological Lower Limb Examination | |||
| Dermatomes | L1, L2, L3, L4, L5, S1 |     | |
| Myotomes | Knee extension (L3,4), Knee Flexion (L5, S1), Ankle dorsiflexion (L4), EHL (L5), Ankle plantar flexion (S1), Eversion (S1), Great Toe Flexion (S1), hip L2-L3 flexor, hip extension (S1-S2) |     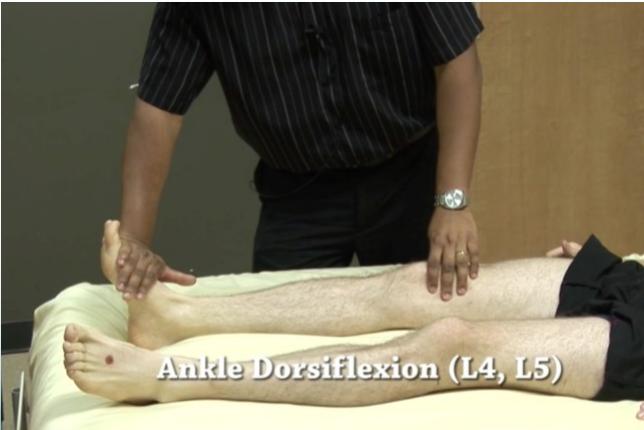   | |
| Reflexes | Knee jerk (L3,4), Ankle jerk (L5, S1) Babinski |     | |
| Functional Assessment | |||
| Gait Assessment |  | ||
| Standing and Sitting Assessment | Smoothness of action | ||
| PR Examination | Per rectal examination when indicated | ||
| General | Attitude towards patient | ||
| Scoliosis Screening | Frontal Assessment | With child standing and facing you: Is one shoulder higher than the other? Is one arm farther away from the body? Are the hips level? |  (Normal) (Normal)  (Abnormal) (Abnormal)  (Abnormal) (Abnormal) |
| Posterior Assessment | With child standing and facing away from you: Is one shoulder higher than the other? Is one shoulder blade higher than the other? Do the hips look uneven? | 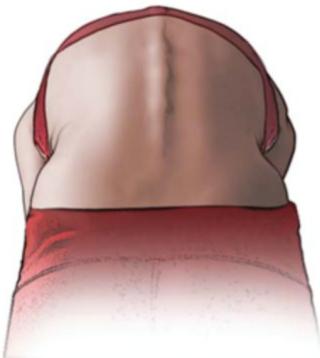 (Normal) (Normal) 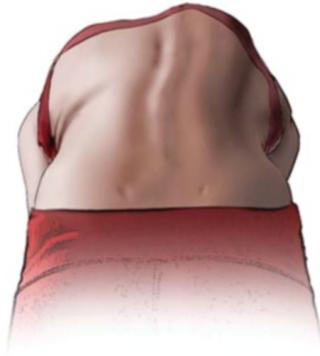 (Abnormal) (Abnormal) | |
| Forward Bending Assessment | With child bending away from you: Is one side of the rib cage higher than the other? Is the lower back uneven? | 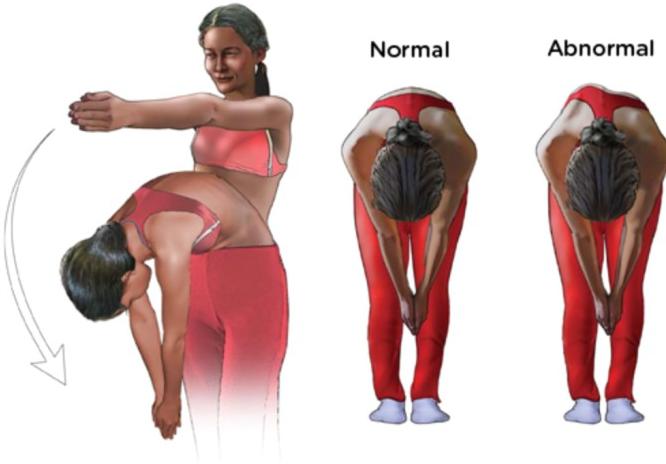 | |
| With child bending toward you: Is one side of the rib cage higher than the other? Is the lower back uneven? Are the hips level? |  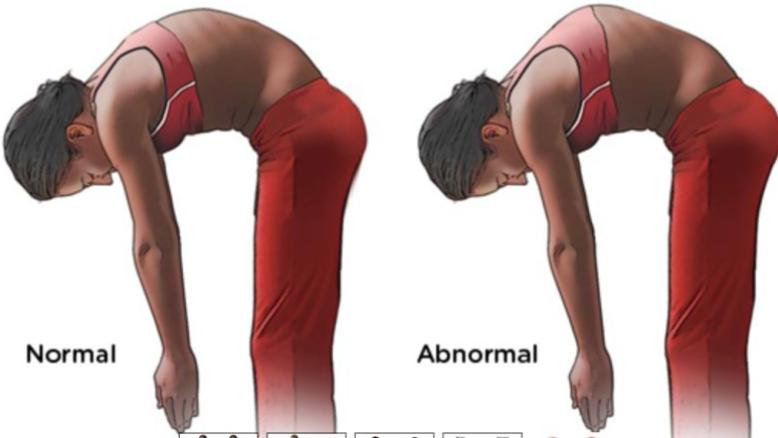 |
McMaster MSK Examination Series
- From: Raj Camona
- Link: https://vimeo.com/36295624
Spine Examination – OSCE Guide
- By: Lewis Potter
- Link: http://geekymedics.com/spine-examination/
Examination of HIP
https://www.youtube.com/watch?v=Hkqr3mg6IWQ&pp=ygUUSGlwIEV4YW1pbmF0aW9uIE9TQ0U%3D
https://www.youtube.com/watch?v=R9IiCO9QjPY&pp=ygUUSGlwIEV4YW1pbmF0aW9uIE9TQ0U%3D
| Item | Procedure | Additional Information … | Attachments |
|---|---|---|---|
| Look | General statement on the patient | General Assessment: Patient’s overall condition and comfort level. Local hip-thigh-lower limb assessment: Position and alignment, major deformities and swelling, external devices (casts, splints, traction, dressings). Anatomical Local Assessment: Skin (swelling, scars, color, hair distribution, dryness), Subcutaneous tissue (lymph nodes, veins, nerves, tendons), Muscles (bulk, wasting, fasciculations), Bones (landmarks, swelling, angulation, deformity), Joints (position, swelling, redness). Important: Always examine the posterior aspect. | Normal Positioning Left hip abnormal positioning  Bilateral hip abnormal positioning  Wheelchair positioning  Local Hip-Thigh-Lower Limb Assessment (Position): Position assessment  Postural Changes: Lumbar lordosis  Major Deformities and Swelling: Major deformities 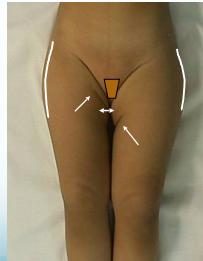 Additional deformity examples  More deformity examples  External Devices (Immobilization): Cast example  Additional cast examples  More cast examples  External Devices (Traction): Traction examples  Additional traction examples  More traction examples  External Devices (Orthotics): Orthotics example 1  Orthotics example 2  |
| General on hip: Position/Swelling & deformity/ Attitude & extra | |||
| - Anatomical: skin, subcutaneous | |||
| - Muscles: Quadriceps, Gluteus Maximus | |||
| - Bony landmarks: ASIS, Iliac crest, Lumbar lordosis | |||
| Look at the back | |||
| Feel | Tenderness: Generalized/Specific points of tenderness | Palpation Assessment: - Tenderness: Diffuse vs. specific points. - Temperature: Compare distal/proximal and right/left sides. - Anatomical structures: Skin (dryness, hypo/hyperesthesia, scars), Subcutaneous (lymph nodes, nerves, vessels, tendons, nodules), Muscles (tone, bulk, fasciculations, gaps, tenderness), Bone (landmarks: ASIS, Greater Trochanter, Ischial Tuberosity; tenderness, masses, crepitus), Joint (swelling, effusion, crepitation, synovial thickening, joint line tenderness - hip joint too deep to elicit). | |
| - Bony landmarks: ASIS, Iliac crest, Lumbar lordosis | |||
| - Temperature: Compare both sides, proximal and distal | |||
| - Muscles: Quadriceps, Gluteus Maximus | |||
| Move | Active: General screening for pain | Movement Assessment Principles: - Active vs. Passive: Start with active movement to screen for pain. Passive assessment when needed for painless vs. painful ROM and muscle power. - Critical Technical Considerations: Differentiate true hip joint motion from pelvic motion. Stabilize the pelvis in neutral position. - Important note: Patients with fixed hip flexion may appear to have full range when supine by tilting the pelvis forward, which creates increased lumbar lordosis. | |
| Abduction / Adduction (compare with other side): ( ANY OF THESE) - Both together - Anchor one side at edge of table - Hold ASIS | Range of motion: Abduction: , Adduction: . Pelvic stabilization techniques: Perform motion on both hips simultaneously, anchor knee of opposite side over examination table edge, palpate ASIS to assess pelvic motion. | Range of Motion Assessment (Abduction/Adduction): Simultaneous abduction/adduction in flexion - Normal ranges: - Abduction: 45° - Adduction: 15° - Pelvic stabilization techniques: - Perform motion on both hips simultaneously - Anchor knee of opposite side over examination table edge - Palpate ASIS to assess pelvic motion Both hips simultaneously: - Stabilizes pelvis and compares both sides - Can be performed in flexion or extension 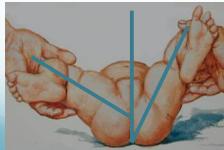 Simultaneous abduction/adduction in extension  Simultaneous assessment technique  Edge of table stabilization Stabilizing the other hip at the edge of couch  ASIS palpation technique Holding ASIS to assess beginning of pelvic motion 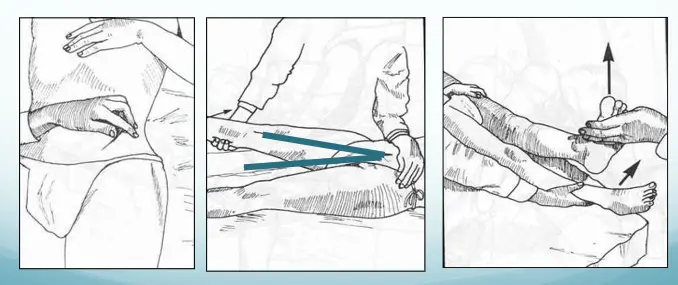 | |
| - Flexion (compare with other side): - Extension (compare with other side): | Flexion: Initial position determined by Thomas Test. Procedure: Check for lumbar lordosis, flex opposite hip fully (lumbar lordosis disappears), check hip position, flex hip to assess range. Range of motion: Flexion from to . Extension: Normal range: . Positions for assessment: Lateral and prone. Important: In presence of fixed flexion deformity, extension is already in “minus” range and doesn’t require assessment. | Range of Motion Assessment (Flexion): Thomas Test positioning 1. Check for lumbar lordosis 2. Flex opposite hip fully 3. Lumbar lordosis disappears 4. Check hip position 5. Flex hip to assess range 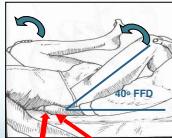 Flexion range measurement 30° to 90° - From 30° fixed flexion - To 90° flexion 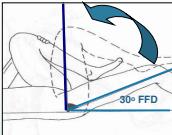 Flexion range measurement (alternative)  Range of Motion Assessment (Extension): Extension - lateral position - Normal range: 30° - Positions for assessment: - Lateral position  Extension - prone position  | |
| Any of these two - External / Internal rotation: In extension, (both together) - External / Internal rotation: In flexion (compare with other side) | Must stabilize pelvis to prevent pelvic motion. Best technique: Perform on both hips simultaneously. Assessment positions: Supine with hips extended (observe patella orientation), Supine with hips flexed (use leg as pointer), Prone with hips extended. | Range of Motion Assessment (Internal/External Rotation): Supine with hips extended (observe patella orientation) 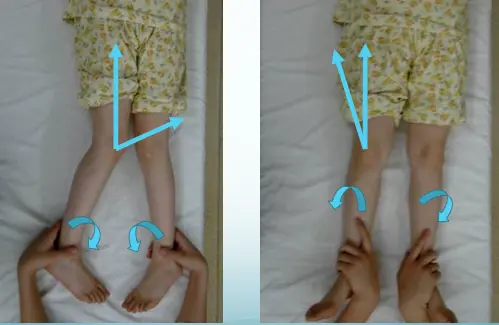 Supine with hips flexed (use leg as pointer)  Prone with hips extended 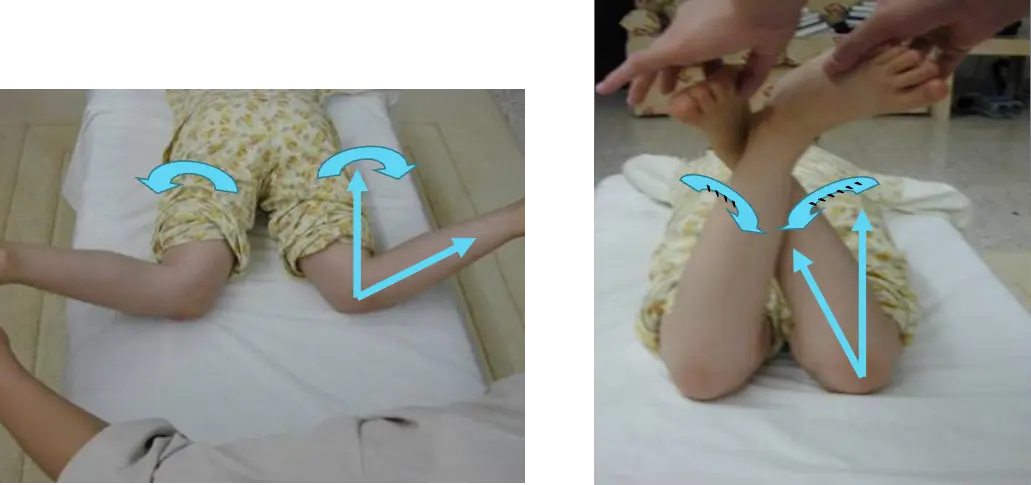 | |
| Special tests | - Thomas test | Purpose: Detect fixed flexion deformity of the hip. Positive Thomas test in neonates and young children is normal. Procedure: Assess lumbar lordosis before testing. Precaution: When knee has fixed flexion deformity, keep knee outside edge of couch. | Thomas Test (Precaution)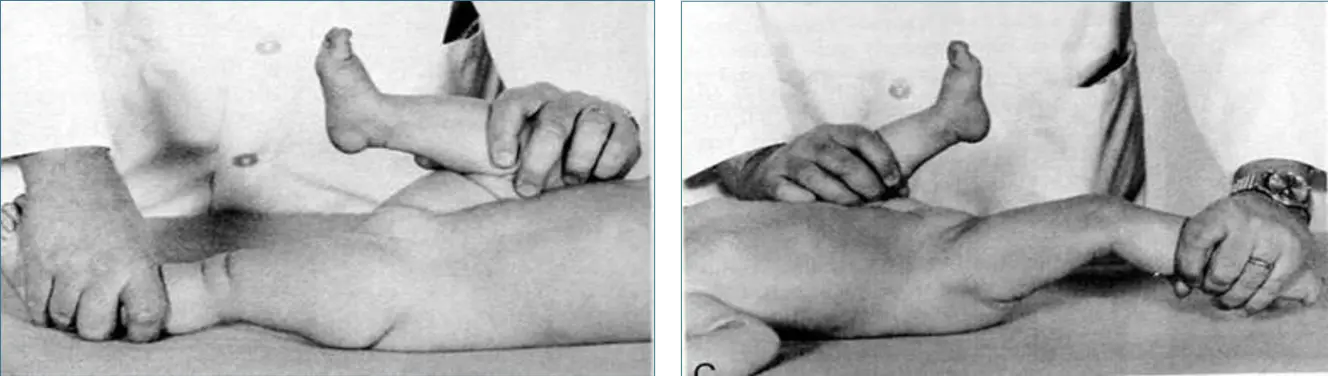 Thomas Test (Solution)  |
| - Trendelenburg test | Purpose: Assess hip abductor strength and stability. Principle: Testing the hip the patient is standing on. Normal: Pelvis tilts down on weight-bearing hip (performed by hip abductors). Positive: Pelvis on non-weight-bearing hip tilts down AND trunk tilts to weight-bearing side. Causes of Positive Trendelenburg: Weak hip abductors, mechanically inefficient hip abductors, unstable pivot of motion, inhibited hip abductors (painful), reduced range of motion. Note: Almost any hip disease can cause a positive Trendelenburg test. | Trendelenburg Test setup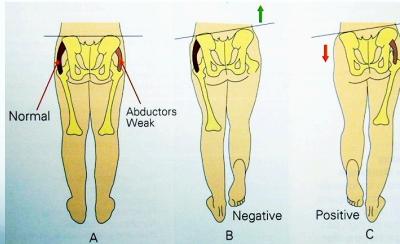 Trendelenburg Test execution 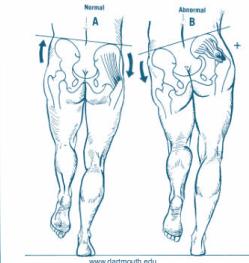 Normal vs Positive comparison 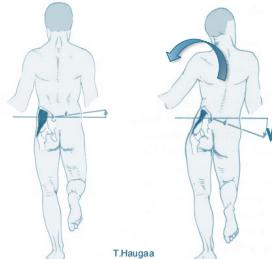 Trendelenburg Test detailed 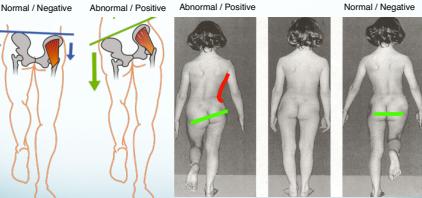 Trendelenburg results 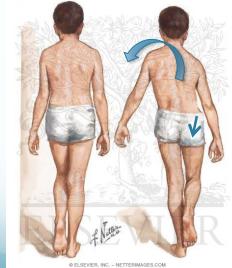 | |
| - Leg length: True / Apparent | Galleazzi Test Purpose: Detect leg length discrepancy. Technique: Both heels must be at the same level. Apparent Length: Measurement: Midpoint to medial malleolus. Affected by: Pelvic tilt. Both lower limbs - Should be Parallel. True Length: Measurement: ASIS to medial malleolus. Not affected by Pelvic tilt. Position of both lower limbs - Should be identical. | Galleazzi  Galleazzi  Purpose: Detect leg length discrepancy Technique: Both heels must be at the same level ---- 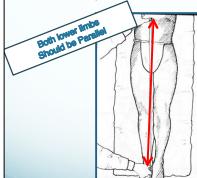 Apparent length measurement - Measurement: Midpoint to medial malleolus - Affected by: Pelvic tilt  True length measurement - Measurement: ASIS to medial malleolus - Not affected by Pelvic tilt 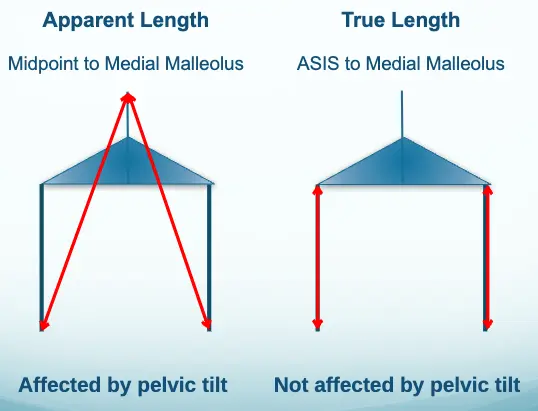 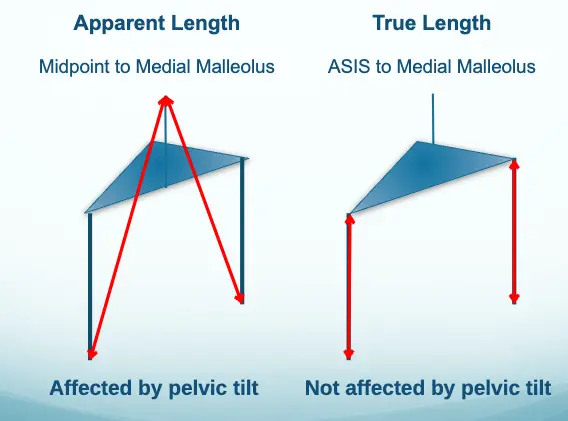 | |
| Neonatal Examination for Developmental Dysplasia of the Hip (DDH) - Ortolani Test / Barlow Test (NOT PART OF OSCE) | Ortolani Test Purpose: Reduces a dislocated hip. Expected finding: Feel a “clunk” (not a “click”). Barlow Test Purpose: Dislocates a reduced hip. Expected finding: Feel a “clunk” (not a “click”). | Ortolani Test technique Purpose: Reduces a dislocated hip - Expected finding: Feel a “clunk” (not a “click”)  Barlow Test technique Purpose: Dislocates a reduced hip - Expected finding: Feel a “clunk” (not a “click”)  Combined Ortolani/Barlow technique   | |
| Gait | - Walking | Normal Gait Cycle: Stance phase (60%): Heel strike, foot flat - mid-stance, push off. Swing phase (40%): Acceleration, mid-swing, deceleration. Abnormal Gait Patterns: Antalgic (painful to weight-bear - short stance phase), Lurch (shortening - painless limping - normal stance period), Circumduction (stiff hip - motion of pelvis compensates), High Step (foot drop - more hip & knee flexion needed to free toes from ground), Tip-toe (Heel off the ground - L4/L5). | Normal gait cycle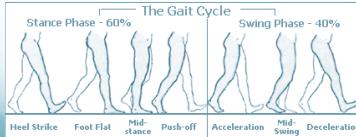 |
| Overall | Attitude with patient | Summary of Orthopedic Examination System: Look, Feel, Move, Special tests. Sub-system helps ensure no steps are forgotten. Key considerations for hip examination: Important exposure considerations, stabilize pelvis in “Move” assessment, Special tests (Thomas, Trendelenburg, instability tests, length measurements), Gait assessment is essential. |
- examiner focused on movement and special tests
- Compare between both hips during movement assessment
- Perform both active and passive movements
- Assess Range of Motion (ROM) and pain
Station 3: Hip Examination
Hip Examination
Case B: Pelvic Trauma
4.1) Open Book Fracture Management
1. Diagnosis? Answer: Open book fracture
2. Initial management? Answer: ATLS protocol, pelvic binder application
3. Mention 3 complications: Answer:
- Bleeding
- Pelvic instability
- Neurological injuries
4. Difference between stable and unstable management:
Stable open book fractures can typically be managed non-operatively, with the use of a pelvic binder or external fixation to stabilize the anterior pelvic ring until the injury heals.
Unstable open book fractures require surgical intervention to achieve anatomic reduction and stabilization of both the anterior and posterior pelvic rings.
Neurological Examination
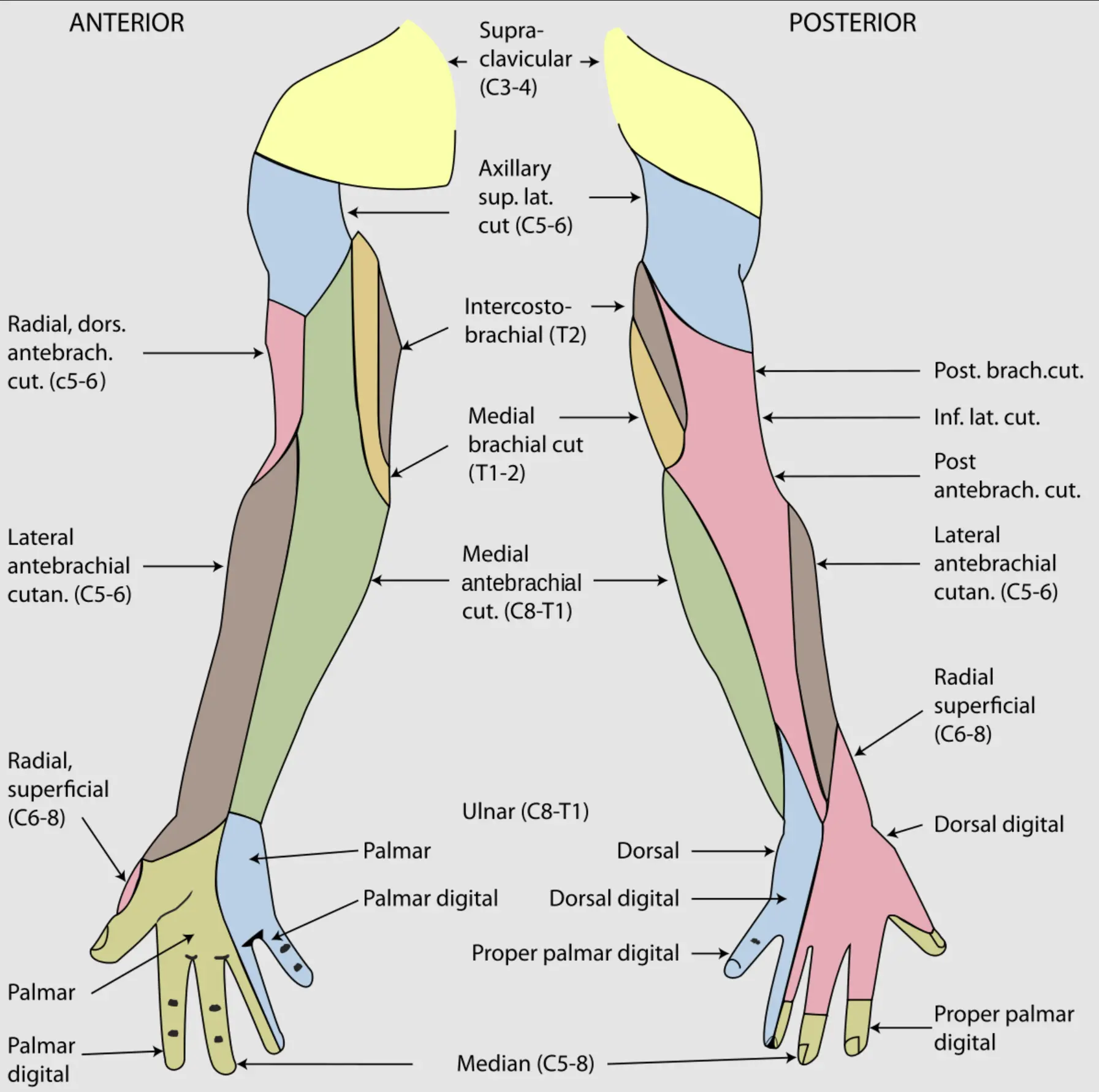
Upper Limb Neurological Clinical Examination Station
Upper Limb Neurological Clinical Examination Station
https://www.youtube.com/watch?v=4uAAjYzi7SY&pp=ygUcVXBwZXIgbGltYiBuZXVyb2xvZ2ljYWwgT1NDRQ%3D%3D
| Section | Item … | Procedure |
|---|---|---|
| Look | Skin | Dryness/scars/wounds/ulcers. (Can’t do abduction of the thumb so it will be in adduction position. Specific for each.) |
| Median | Thenar Muscles wasting and adducted thumb (ape hand), Pointing Index. | |
 | ||
| Ulnar | Hypothenar muscle wasting, Ulnar Claw hand – in low lesions (in high lesions ulnar ½ of FDP is paralyzed, no claw hand) (ulnar paradox). | |
   | ||
| Radial | Wrist drop. | |
| Feel | Ulnar | Ulnar one and a half fingers (volar aspect medial half of forearm). |
| Sensation | Median | Sensation lateral three and half digits on palmar surface & distal phal. on dorsum (volar aspect lateral half). |
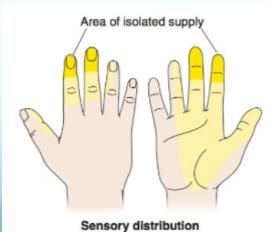 | ||
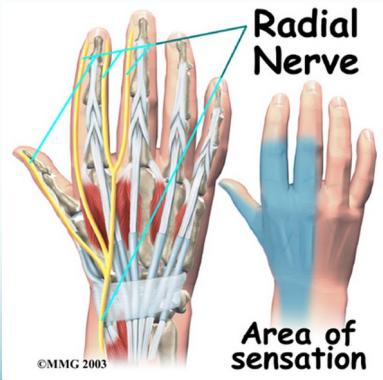
| Radial Nerve | dorsal aspect. over lateral part of the dorsum of the hand (more prominent at anatomical snuffbox) | |
 | ||
| Ulnar Nerve |  | |
| Median N (Lesion above elbow) | Loss of wrist flexors | (Flexor-carpi-radialis). |
| OK sign not possible | Loss of flexion of thumb and index finger (Flexor Pollicis longus and Flexor Digitorum Profundus for index finger). | |
   | ||
| Loss of forearm pronation | (both Pronators): pronate against resistance. | |
| Loss of thumb opposition | (Opponens Pollicis). | |
| Carpal Tunnel | Tinel’s sign | (It came with numbness in Median N Sensation). |
  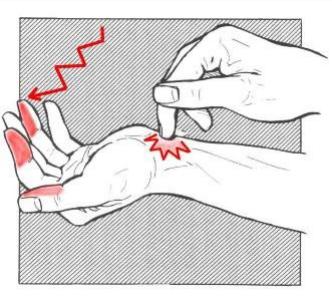 | ||
| Phalen’s sign | ||
  | ||
| Ulnar N | Adductor Pollicis | Froment’s sign. |
| Palmar & Dorsal Interossi | Abduction/Adduction of fingers (against resistance). | |
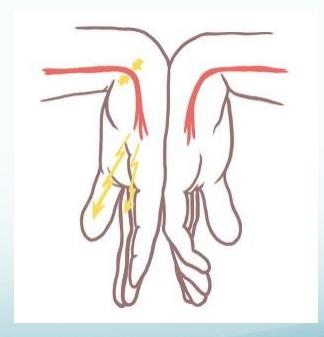
| Paralysis of 3rd & 4th Lumbricals | The lumbrals are deep muscles of the hand that flex the metacarpophalangeal joints and extend the interphalangeal joints. (In lesion extension of MCP and flexion of IP).  | |
| Abductor digiti minimi | Abduction of little finger against resistance. | |
| Radial N | Loss of elbow extension | (Triceps) – in high lesions. |
| Loss of wrist extension | ||
| Loss of thumb extension | (Extensor Pollicis longus and brevis). | |
| Loss of extension of fingers MP joints | (Extensor Digitorum). (If I can extend my wrist, but I can’t extend my PI. So, the problem is in the Posterior Interosseous Nerve). | |
| Axillary N (NOT IN CHECKLIST) | Arm Drop Test (Deltoid Test) | Patient stands with arm at side. Examiner passively abducts arm to approximately 90°. Patient asked to actively maintain position. Examiner releases support. Positive Test Result: Arm drops from abducted position. Inability to maintain shoulder abduction. Indicates: Deltoid weakness/paralysis. |
 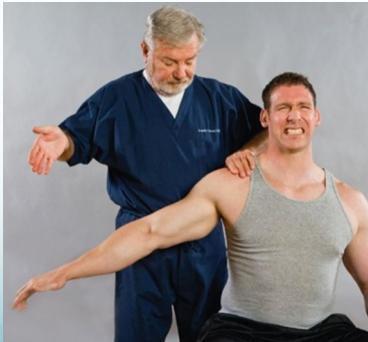 | ||
| Overall | Attitude with patient | (throughout the examination). |
Lower Limb Neurological Clinical Examination Station
https://www.youtube.com/watch?v=-7ERNH_o5Ss&pp=ygUcTG93ZXIgbGltYiBuZXVyb2xvZ2ljYWwgT1NDRQ%3D%3D
https://www.youtube.com/watch?v=LH-HuLSGNC8&pp=ygUcQmFjayBST00gJiBOZXVyb2xvZ2ljYWwgT1NDRQ%3D%3D
• Perform a neurological exam of the lower limb.
| Item | Procedure |
|---|---|
| Opening | • Introduction, Privacy, Permission & Exposure |
| Dermatomes | • L1, L2, L3 |
| • L4, L5, S1 | |
| Myotomes | HIP - L3 • Knee extension (L3, L4) |
| • Knee Flexion (S1, S2) | |
| • Ankle dorsiflexion (L4) | |
| • Great Toe Extension (L5) | |
| • Ankle plantar flexion (S1) | |
| • Great Toe Flexion (S2) | |
| Reflexes | • Knee jerk (L3, L4) - gaurd hand |
| • Ankle jerk (L5, S1) | |
| General | • Attitude towards patient |
hof clonus babinsk .. rev- UML signs…
Name this test and what it’s indicating for?
- Hoffman’s sign
- It indicates an upper motor neuron lesion.
Peripheral Nerve Examination
Cases
Orthopedic Emergencies Summary
| Condition | Definition & Risk Factors | Assessment Plan (History, Clinical Features, Investigations) | Management Plan | Differential Diagnosis | Complications & Contraindications |
|---|---|---|---|---|---|
| Compartment Syndrome | Increased pressure within a closed fascial compartment, leading to reduced tissue perfusion, hypoxia, and irreversible muscle and nerve damage. Causes: Fractures (especially tibia/forearm), severe soft tissue trauma, arterial injury, burns, tight casts/dressings, post-ischemic reperfusion swelling, IV fluid extravasation, and bleeding disorders (e.g., hemophilia). High-Risk Notes: Pain may be absent in altered consciousness, children (monitor analgesia response), polytrauma, sedated/epidural cases, or concomitant nerve damage. Open fractures do not always decompress pressure. Gross/Clinical:  -tense, shiny leg swelling with blisters in compartment syndrome. -tense, shiny leg swelling with blisters in compartment syndrome.Imaging:  - Intraoperative fasciotomy - Intraoperative fasciotomy | History/Symptoms: Pain out of proportion to the injury (e.g., a “bursting” sensation), which is not relieved by analgesia. Clinical Features (The 5 P’s): - Pain with passive stretch (early, key sign; e.g., ankle dorsiflexion for leg, wrist for forearm). - Paresthesia (early). - Palpable tense swelling (shiny skin, blisters: clear=mild, serosanguinous=severe, bloody=worst; dusky/pallor skin). - Pallor, Paralysis, Pulselessness (late, ominous signs; pulses often palpable until late). Investigations: Primarily a clinical diagnosis (high suspicion key). Compartment pressure measurement can confirm: absolute pressure >30 mmHg or Delta Pressure (Diastolic BP - Compartment P) ≤ 25 mmHg. | Initial: ABCs, supplemental oxygen. Remove all circumferential dressings, casts (bivalve to skin), and splints. Elevate the limb to heart level (not above; higher reduces inflow). Correct any hypotension. Surgical: Urgent Fasciotomy if no response within 1h or confirmed pressure (prophylactic in high-risk like major osteotomy). Release all compartments/skin with long incisions; debride necrotic muscle via 4C’s (early: pink/red, soft, contracts/bleeds on pinch; late: dark, firm, no response); preserve neurovascular. Wound open (bulky dressing/splint, VAC, or boot-lace gradual closure); repeated inspections x48h; coverage in 3-5 days (skin graft usual; flap if nerves/vessels/bone exposed). | Cellulitis, Deep Vein Thrombosis (DVT), Arterial occlusion, Severe soft tissue injury without compartment syndrome; equivocal cases in polytrauma. | Complications: Volkmann’s ischemic contracture (permanent deformity, weakness, sensory loss, chronic pain). Contraindications (Fasciotomy): Confirmed >48h (irreversible damage, high infection risk from dead tissue); crush injuries with already necrotic muscle. |
| Open Fracture | A fracture with a breach in the overlying skin and soft tissues, creating communication with the external environment. All open fractures are considered contaminated (even small punctures; aka compound fracture). Causes: Can result from high-energy trauma (RTAs, falls, firearms; signs: degloving, crush syndrome, bone loss, segmental) or low-energy trauma. Contamination risk higher with farm/soil injuries, bites, delayed presentation (>12h), fecal/oral/soil/water exposure. Mechanism: Low/high velocity missiles (cavitation >300 m/s); in-out (cleaner) vs. out-in (dirtier). Gross/Clinical:   | History: Mechanism of injury (energy, time, place, type/impact method), consciousness, wound size/bleeding amount, other injuries (often missed), tetanus status. Assessment: ATLS protocol (ABCDE) first (treat patient, not fracture; exclude shock/brain injury, monitor vitals; viscera exam: ribs=lungs/liver/spleen, pelvis=bladder/urethra). Examine wound (look/feel/move carefully post-splint), check distal neurovascular status, compartment syndrome. Photograph/remove gross contamination; cover with saline dressing. Classification (Gustilo-Anderson): - Type I: <1 cm wound, clean, minimal soft tissue. - Type II: >1 cm wound, moderate soft tissue (no stripping). - Type IIIA: Extensive soft tissue damage, but adequate bone coverage. - Type IIIB: Extensive soft tissue loss with periosteal stripping; bone exposed, requires flap coverage. - Type IIIC: Any open fracture with an arterial injury requiring repair. | Initial (ER): ATLS first. Cover wound with sterile saline-soaked dressing, splint limb, IV fluids (request blood if needed); traction if no distal pulse/deformity. Prophylaxis: Tetanus prophylaxis/serum and broad-spectrum IV antibiotics immediately (culture tissue/blood); clean major contamination. Surgical: Urgent debridement/irrigation within 6-12h (“Dilution is the solution to pollution”; pulse-irrigate 3-6-9L saline; excise non-viable tissue/foreign material, trim skin edges, remove dead muscle/detached bone, preserve N/V). Stabilization: external fixator (preferred severe; replace with cast post-infection); internal if clean/minimal. Wound closure delayed (primary if small/clean; secondary if contaminated/large). Early soft tissue cover. | The diagnosis is typically obvious. Key: Classify severity; identify associated injuries like compartment syndrome, vascular damage, or high-energy signs (e.g., crush). Differentials for contamination: Primary (field debris) vs. secondary (post-fixation if poor debridement). | Complications: Infection (cellulitis, osteomyelitis, chronic with sequestra/drainage, gas gangrene), tetanus; higher with delay/exposure/bites. - embolisms fat, thrombi others.. Case Insight: Unconscious patient (e.g., open tibia post-RTA): ABCDE/cervical collar, distal pulses/traction, admit for debridement; ankle fall: Splint post-ABC, assess neurovascular. |
| Septic Arthritis | An infection within a joint space, leading to purulent effusion and rapid destruction of articular cartilage (damage within 8 hours). Risk Factors: All ages; pediatric (<2y, hip; prematurity/C-section); adult (>80y, knee; diabetes, RA, cirrhosis, HIV, crystal arthropathy, endocarditis/bacteremia, IV drug use; psudomonas, recent surgery). Route: Hematogenous (most common), direct inoculation/trauma/surgery, contiguous from osteomyelitis/soft tissue (esp. intracapsular metaphysis: hip/shoulder/elbow/ankle/umbilicus). S. aureus most frequent (>50%). ⇒  - Swollen and erythematous knee joint with visible effusion in septic arthritis. - Swollen and erythematous knee joint with visible effusion in septic arthritis.Imaging:  - X-ray demonstrating early joint space changes in pediatric hip septic arthritis. - X-ray demonstrating early joint space changes in pediatric hip septic arthritis. | History: Acute onset of single hot, swollen, painful joint, fever/malaise; vaccination history (children). Age-specific: Neonates (irritability, feeding refusal, pseudo-paralysis, no fever); children (ill appearance, high fever, no weight-bearing); adults (superficial: knee/ankle/wrist). Clinical Features: Joint in resting position; extreme pain on movement (active/passive); inflammation (red, hot, swollen, effusion/fluctuation). Investigations: - Labs: High WBC (neutrophils), ESR/CRP (CRP early); Blood cultures positive ~50%. - Joint Aspiration: (guide via US); fluid: WBC >50,000/μL, >50% PMNs, positive Gram/culture (>50%); glucose/protein low, no crystals; alpha-defensin. Table: Normal (<200 WBC, clear); Noninflammatory (<2k WBC, yellow); Inflammatory (2-50k WBC, cloudy); Septic (>50k WBC, pus/yellow, culture+). - Imaging: Early X-ray normal/widened space/subluxation (infants: lateral femur); later narrowing/bone involvement; US for effusion; MRI for effusion/bone (emergent challenge). Kocher criteria (children hip): Fever >38.5°C, non-weight bearing, WBC >12k, ESR >40 mm/h (0=0.2%, 1=3%, 2=40%, 3=93%, 4=99% septic); CRP >2 mg/dL predictor. | This is an orthopedic emergency. Medical: Admit, NPO, IV fluids, splint joint. Joint aspiration first, then empiric IV antibiotics (age/risk-based: flucloxacillin Gram+; 3rd-gen cephalosporin neonates; Lyme if endemic; don’t delay surgery; IV 3 weeks + oral 2-3 weeks; monitor WBC/ESR/CRP; organism-specific post-culture). Surgical: Emergency irrigation/debridement (arthrotomy/washout); if pus/turbid, open drainage. | Transient Synovitis (children 4-8y, M:F 2:1, self-limited 2-7 days w/NSAIDs like ibuprofen; risk: trauma/viral; resolves <1 week; table: fever <38.5, weight-bearing yes, WBC <12k, ESR <40), Gout/Pseudogout (crystals+), Other differentials Reactive arthritis, Hemarthrosis (trauma/hemophilia), Lyme disease, Cellulitis, Acute osteomyelitis (nearby metaphysis), Rheumatic fever. | Complications: Rapid cartilage destruction, osteoarthrosis (partial), joint dislocation (tense effusion), epiphyseal destruction (neonates: pseudoarthrosis), ankylosis (massive; adhesions/fibrosis). Case Insight: 14y boy hip post-fall (fever, limited motion, WBC 13k, ESR 23; early X-ray normal, late destruction if delayed). |
| Cauda Equina Syndrome | Compression of the bundle of nerve roots at the lower end of the spinal cord (the cauda equina; thecal sac). Causes: Most commonly large central lumbar disc herniation. Other: spinal stenosis, tumor, epidural abscess/hematoma, trauma. 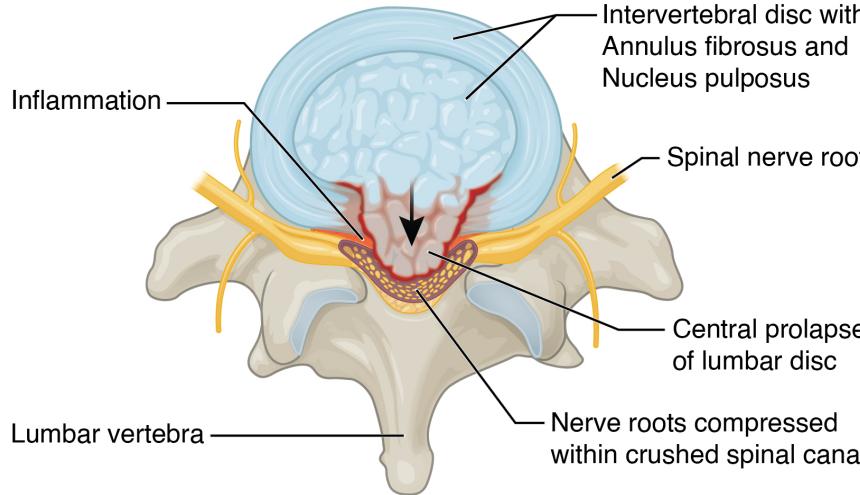  - Sagittal MRI of lumbar spine showing central disc herniation compressing nerve roots. - Sagittal MRI of lumbar spine showing central disc herniation compressing nerve roots. | History/Symptoms (Red Flags): - Back pain (most common), bilateral sciatica/leg pain (2nd). - Saddle anesthesia (numbness in perineum, buttocks, genitals; highly specific). - Bladder/Bowel Dysfunction: Urinary retention (early) → overflow incontinence (late); unilateral/bilateral leg sensory/motor changes. Clinical Exam: Reduced anal tone, perineal sensory loss, lower limb weakness. Investigations: Urgent MRI to confirm diagnosis/cause (essential for early detection). | This is a neurosurgical emergency. Surgical: Immediate decompression to prevent permanent deficits; perform within 24h (absolutely <48h) of symptom onset. | Conus Medullaris Syndrome, Severe bilateral radiculopathy, Peripheral neuropathy. | Complications: Permanent leg paralysis, urinary/fecal incontinence, sensory/motor deficits. |
| Joint Dislocation | A complete disruption and loss of contact between the articular surfaces of a joint. Neurovascular status must be checked/documented before/after reduction (3 E’s for shoulder: epilepsy, electric shock, ETOH). Causes: Vary by joint. Shoulder most common (sports; anterior 98%, shallow glenoid/wide ROM; static: ligaments/labrum/capsule; dynamic: muscles). Hip/Knee high-energy (RTA; hip stable via labrum/ligaments). Small joints/AC/Patellar sports/falls (AC: cyclists, no vascular emergency unless open). - Shoulder (Anterior): 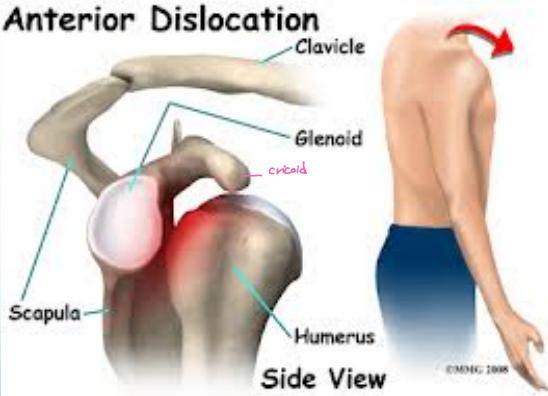 - Flattened shoulder contour with subcoracoid humeral head bulge in anterior dislocation. - Flattened shoulder contour with subcoracoid humeral head bulge in anterior dislocation.- Hip (Posterior):  - Leg shortened, adducted, internally rotated; X-ray confirms femoral head displacement posterior to acetabulum. - Leg shortened, adducted, internally rotated; X-ray confirms femoral head displacement posterior to acetabulum.- Knee:  - Gross tibiofemoral misalignment with potential popliteal artery compromise from high-energy trauma. - Gross tibiofemoral misalignment with potential popliteal artery compromise from high-energy trauma.- Small Joints (Fingers):  - Dorsal dislocation of proximal interphalangeal joint showing angular deformity from hyperextension. - Dorsal dislocation of proximal interphalangeal joint showing angular deformity from hyperextension. | Shoulder: Ant: Arm adducted, loss of deltoid contour, bulge below clavicle (flattened lateral); axillary nerve check. Post: Locked internal rotation, flat front/prominent coracoid (missed >50%, light bulb/empty glenoid signs); rule out greater tuberosity/neck/lesser tuberosity/glenoid fractures. X-ray (AP/axillary/scapular; CT if doubt). Hip: Post (90%): Short, adducted, internally rotated/flexed; sciatic nerve check; rule out femur/acetabulum/patella fractures/intraarticular fragments (RTA dashboard). Ant (rare): Abducted, externally rotated/flexed; palpable groin head. X-ray + post-reduction CT. Knee: Gross deformity; popliteal artery (pulses/ABI; angiography even if intact/suspicion), peroneal nerve. X-ray (avulsions: tibial spine cruciate, fibular styloid collateral) + CTA. Small Joints/Patellar/AC: Obvious deformity (patellar: adolescent females, genu valgum/↑Q angle, high patella, spontaneous via quad); X-ray (standard knee for patellar). | General: Prompt closed reduction under analgesia/sedation; immobilize post-reduction (sling for AC/shoulder; splint/buddy taping for small). Specifics: - Shoulder/Hip/Small/AC/Patellar: Closed reduction (traction/counter for small; self for patellar); surgery if recurrent/unstable/displaced (AC stages 1-3 conservative first). - Knee: Immediate reduction, external fixation; urgent vascular repair; delayed ligament reconstruction (acute if needed). - ANKLE: immediate management (realignment, X-ray, back slab) and complications (AVN risk). | Fracture, Fracture-dislocation, Subluxation; shoulder: 3 E’s mechanisms; patellar: recurrent risk (laxity/valgum). | Shoulder: Axillary nerve injury, recurrent instability, greater tuberosity fracture. Hip: Sciatic nerve palsy, AVN, acetabular fracture. Knee: Popliteal artery injury/limb loss. Patellar/AC/Small: Recurrent dislocation, ligament laxity. |
Compartment Syndrome
Section 5: Trauma & Fracture Management
Questions 8-12: Lower Limb Trauma
Clinical Scenario: 22 years old medical student involved in RTA who sustained this leg injury.
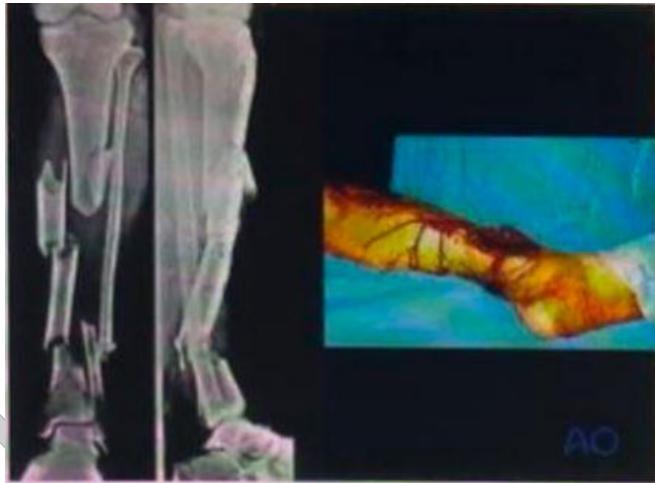
Q8: Before assessing his leg, what protocol should you use? ATLS
Q9: What is your diagnosis according to x-ray? middle third tibia diaphysis comminuted segmental fracture and lower third fibula fracture
Q10: Describe the injury in the photo knowing that the victim foot is cold and pulseless? gustilo anderson open fracture 3c
Q11: What is your initial management in ER? realignment check pulse again, lavage, IV ATB empirical, prepare for urgent surgery once stable
Q12: What is your temporary and definitive management, which other surgeons should be working with you and for what?
- Begin with ATLS to identify and manage any life threatening injuries
- Debridement of the open fracture to remove foreign materials
- Lavage using 3-9 of normal saline cleanse the wounds
- Realignment to restore the normal alignment of the bone
- IV broad spectrum Antibiotics and tetanus vaccine
- Cover the bone with sheets apply pelvic binder to protect the bone
- External fixation as a temporary management to protect soft tissues
- Second debridement after 2 days to remove any necrotic tissues
- Reassess and monitor for infections
- Consult vascular surgeon to correct the vascular injury
- Definitive management by Open Reduction and Internal Fixation by Intramedullary Nail
Station 2: Acute Case Discussion
Topic: Open Fracture Management



A patient came to the ER following a MVA and had a closed tibial fracture.
• First Take AMPLE history
- Allergies
- Medications
- Past medical history
- Last oral intake
- Events leading to injury/illness
Q: What are you seeing? Open fracture in lower half of tibia.
Q: What will you do in examination? (ATLS is intact) Examine the pt “Look, Feel, Move”
- Neurovascular assessment
- Soft tissue examination
- Size of wound measurement
- Rule out other injuries
- Rule out compartment syndrome
apply a passive e stretch to the anterior leg compartment for example (Perform passive plantar flexion), and assess
if there’s any pain (But that’s not the scope of the discussion, hat matters is that you have to say that compartment syndrome has to be ruled out).
Q: How will you manage it in Emergency room?
-
IV antibiotics
-
Tetanus prophylaxis
-
Apply direct pressure to control bleeding
-
NSAIDs for pain control
-
Remove gross debris from the wound
-
Place sterile dressing on the wound
-
Realign the limb and apply splint
-
Prepare for surgery
-
The examiner will tell you that the wound measures around 5 cm, and there is no periosteal stripping. What type of open fracture?
- Gustilo type 2
The examiner will say: The patient had severe pain with passive stretch and tense compartments when you felt his leg
- What is the Dx? Compartment syndrome
- How many compartments in the leg? 4 (ant., lateral and two post.)
- How can you measure the compartment pressure? Manometer
- What is the treatment of this patient? Fasciotomy
Open Fracture
Open Fracture Management
Clinical Scenario
- Patient: 30-year-old man
- Mechanism: Car accident
- Presentation: Unconscious, large anterior left leg wound, severe deformity, exposed bone
- Task: Describe emergency management actions

Emergency Management Protocol
Immediate Actions (ABCDE):
- Save life, save limb, save function
- Cervical spine protection
- Wound management:
- Cover with sterile dressing
- Splint leg
- Take photograph before dressing
- Secondary survey:
- Check distal pulses
- If no pulse, correct major deformity by traction
- IV fluids: Request blood if needed
- Anti-tetanus prophylaxis
- Antibiotics: Broad-spectrum coverage

Further Assessment:
- Accident details: Type, mechanism, location, time since injury
- Pre-hospital management
- Patient factors: Age, comorbidities, medications, consciousness status
- Tetanus vaccination status
Gustilo Classification:
- Essential for surgical planning and prognosis
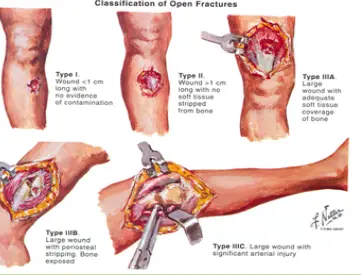
Surgical Management Principles
Debridement Protocol:
- Principle: “Dilution is the solution to pollution”
- Thorough irrigation and debridement
- Remove all contaminated and non-viable tissue
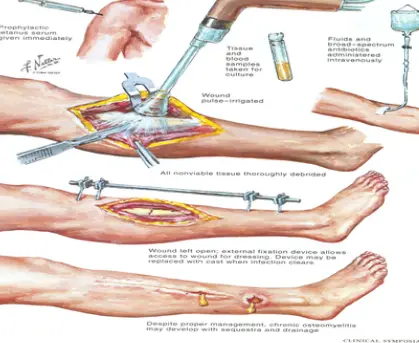
Fixation Options:
- External fixation (initial management)
- Internal fixation (when indicated)
Complications:
- Despite proper management, chronic osteomyelitis may develop
- Risk of sequestrum formation and persistent drainage
Embolism
- Management for the fractures till the permanent fixation – external fixation
- After 4 days this is his picture: What’s the name of the condition shown in the picture? “Fat Embolism Syndrome”
- What’s your management “after the previous condition”? Respiratory support
Case C: Lower Limb Trauma
4.2) Open Fracture Management Protocol
1. Diagnosis? Answer: Open fracture in distal tibia
2. Emergency Management?
- IV antibiotics
- Tetanus vaccine
- Apply pressure to control bleeding
- Give NSAIDs for pain
- Debridement and apply sterile dressing
- Realign by splint
- Admit and prepare for surgery (ORIF)
- Wound closure
3. Mention 3 complications:
- Infections
- Compartment syndrome
- Vascular injury
4. Specialist referrals:
- Vascular surgeon
- Plastic surgeon
Ankle Fracture-Dislocation
- Immediate management after ABC protocol:
- Realignment
- Send to x-ray
- Temporary back slab
- Complication of dislocated talus: High risk of AVN
Arthrodesis

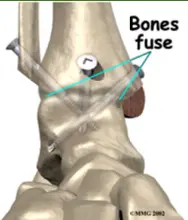
Septic Arthritis
Case: Septic Arthritis in Infant (10 months)
Clinical Presentation
- History: Fever for 2 days, poor feeding, cries with diaper changes
- Examination: Ill appearance, temperature 39.4°C, normal chest and abdomen, moves all limbs except left lower limb
- Key Finding: Left hip held in flexion, painful on passive movement
Assessment Questions
Q1: Write TWO differential diagnoses?
- Septic arthritis
- Osteomyelitis
Q2: Write FOUR blood investigations?
- WBC count
- CBC with differential
- CRP
- ESR
Q3: Write TWO abnormalities on x-ray?
- Widening of joint space (left hip)
- Left hip increased opacity
Q4: Write TWO imaging studies you would request?
- MRI
- CT scan
Q5: Management plan after admission and supportive measures?
- Aspirate joint and send for culture
- Drain if pus found
- Antibiotic Therapy:
- IV flucloxacillin + 3rd generation cephalosporin for 7-10 days
- Followed by 3-6 weeks oral antibiotics
- Change antibiotic according to sensitivity
- Surgical drainage (arthrotomy) - MUST be included in answer
Questions 13-16: Pediatric Hip Pathology
Clinical Scenario: A 1-year-old boy. He was brought to the emergency department by his mother, complaining of irritability associated with constitutional symptoms for 10 hours. He had a history of otitis media 2 weeks ago. The laboratory investigation showed WBC 18000, CRP 130, and ESR 60.
Q13: List three symptoms considered constitutional symptoms.

Answer:
- High grade fever
- Loss of appetite
- Fatigue
Q14: What is the next step to confirm the diagnosis?
 Clinical Presentation
Clinical Presentation
- Patient: 2-year-old child
- Symptoms: Fever, vomiting, left hip pain, limited range of motion
- X-ray Findings: Localized osteopenic lesion in upper metaphysis of left femur, reaching epiphyseal plate
Differential Diagnosis
- Osteomyelitis
- Septic Arthritis
- Further investigation needed
Recommended Investigations
- Laboratory: CBC with differential, CRP, ESR
- Imaging: Ultrasound, MRI
Answer: Arthrocentesis (Sending for Culture, WBC Count, Glucose, & Protein)
Q15: What is the most likely diagnosis? Septic Arthritis
Q16: What is the gold standard treatment for his condition? Answer: Sending to OR for debridement and irrigation (arthrotomy washout) then giving a proper antibiotic after receiving the result of arthrocentesis
Station 2: Septic Arthritis Case Discussion


Clinical Scenario: A 50-year-old female presented to the ER with history of left knee swelling for 6 hours and positive constitutional symptoms. No history of trauma. On examination, she is febrile 38.5°C. Locally: redness, hotness, severe swelling and restricted range of motion. Q: 18-months old baby, febrile and unable to move his limb, no history of trauma. X-ray provided
Questions:
Q1: What is your differential diagnosis?
- Septic arthritis
- Osteomyelitis
- Transient synovitis
B) What are the x-ray findings on child
- Left hip dislocation
- Wide joint space
- Left hip increased opacity.
Q2: How would you treat?
- Admission and IV antibiotic
- Emergent arthrotomy and washout
Q3: What investigation would you order?
- CBC, wbc
- ESR, CRP
- Blood culture
- Joint aspiration (cell count, glucose, protein, culture, color, crystals) -
Q4. Write TWO images that would you request?
- MRI
- CT
Q5. After admission and giving supportive measures: Analgesic, antipyretic, IV fluid, What is your management plan for this patient.
- IV flucloxacillin and 3rd generation cephalosporin for 7-10 days + 3-6 weeks oral antibiotic. 1. Aspirate and send to culture, drain if pus found.
- Change antibiotic according to sensitivity.
Septic Arthritis Cases
Case: Septic Arthritis of the Hip
Clinical Presentation
- Patient: 14-year-old boy
- History: Right hip pain following a fall with abrasions few days prior
- Symptoms: Fever, limited right hip motion
- Laboratory Findings:
- WBC: 13,000 (not significantly elevated)
- ESR: 23mm/hour (not significantly elevated)
- Initial X-ray: No significant findings
Diagnostic Imaging
Initial X-ray Findings:

Pediatric Elbow Infection
- Age: 6-year-old
- Presentation: Localized tenderness, hotness, swelling, edema, reduced elbow ROM
- Differential Diagnosis:
- Cellulitis
- Osteomyelitis
- Septic arthritis
- both septic & osteomyelitis
- Ewing’s sarcoma
nvestigations
- • WBC: leukocytosis, neutrophils
- • C-reactive protein: raises very early
- • ESR: raises several days later
- • Blood culture
- • Aspiration from sub-periosteal collection or joint
- • Gram stain
- • Culture /
• Check yourself
- • Clear colorless: normal
- • Clear yellow:
- • can read through:
- • non-inflammatory
- • Turbid: Inflammatory
- • Pus
- • Blood



DDH
full case can be found in history beginning of the document
Case: Developmental Dysplasia of the Hip (DDH)
Clinical Assessment
Inspection Findings:
- Describe abnormalities on hip inspection
- Assess for limited abduction
Imaging: Required for diagnosis (ultrasound in infants, X-ray in older children)
Of course. Here are some clinical scenario questions and answers based on your note on DDH.
A 6-day-old female infant, born in a breech position, is presented for her newborn check. During the examination, you flex her hips and knees to 90 degrees. As you gently abduct the left hip, you feel a distinct “clunk” as the femoral head seems to relocate into the acetabulum.
Question: What is this clinical sign called, and what risk factors for DDH are present in this infant? What is the recommended initial management?
Answer:
- Sign: This is a positive Ortolani test, which signifies the reduction of a dislocated hip.
- Risk Factors: The infant has three major risk factors: being a baby girl (4-6x), breech presentation (5-10x), and a positive physical finding.
- Initial Management: For a neonate under 2 weeks, the initial approach is to avoid adduction swaddling and consider using double diapers. The infant should be seen again at 2 weeks of age. If the hip remains unstable, a Pavlik harness is the treatment of choice.
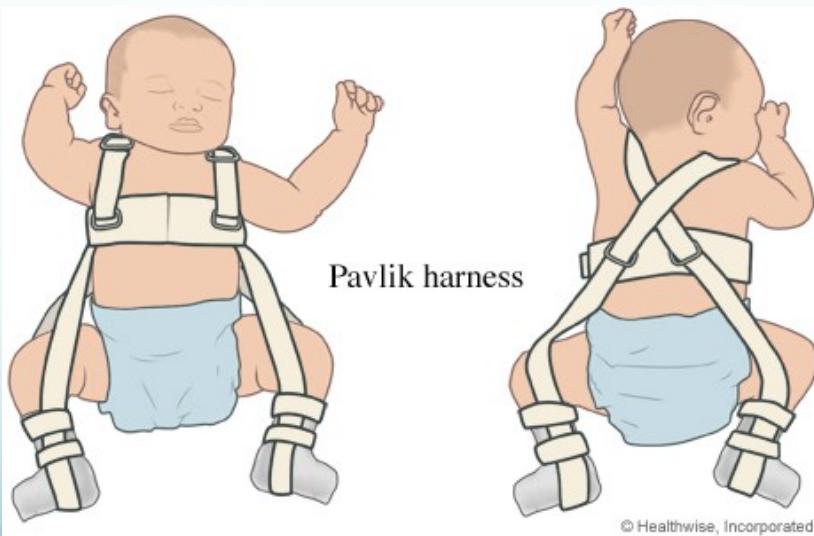

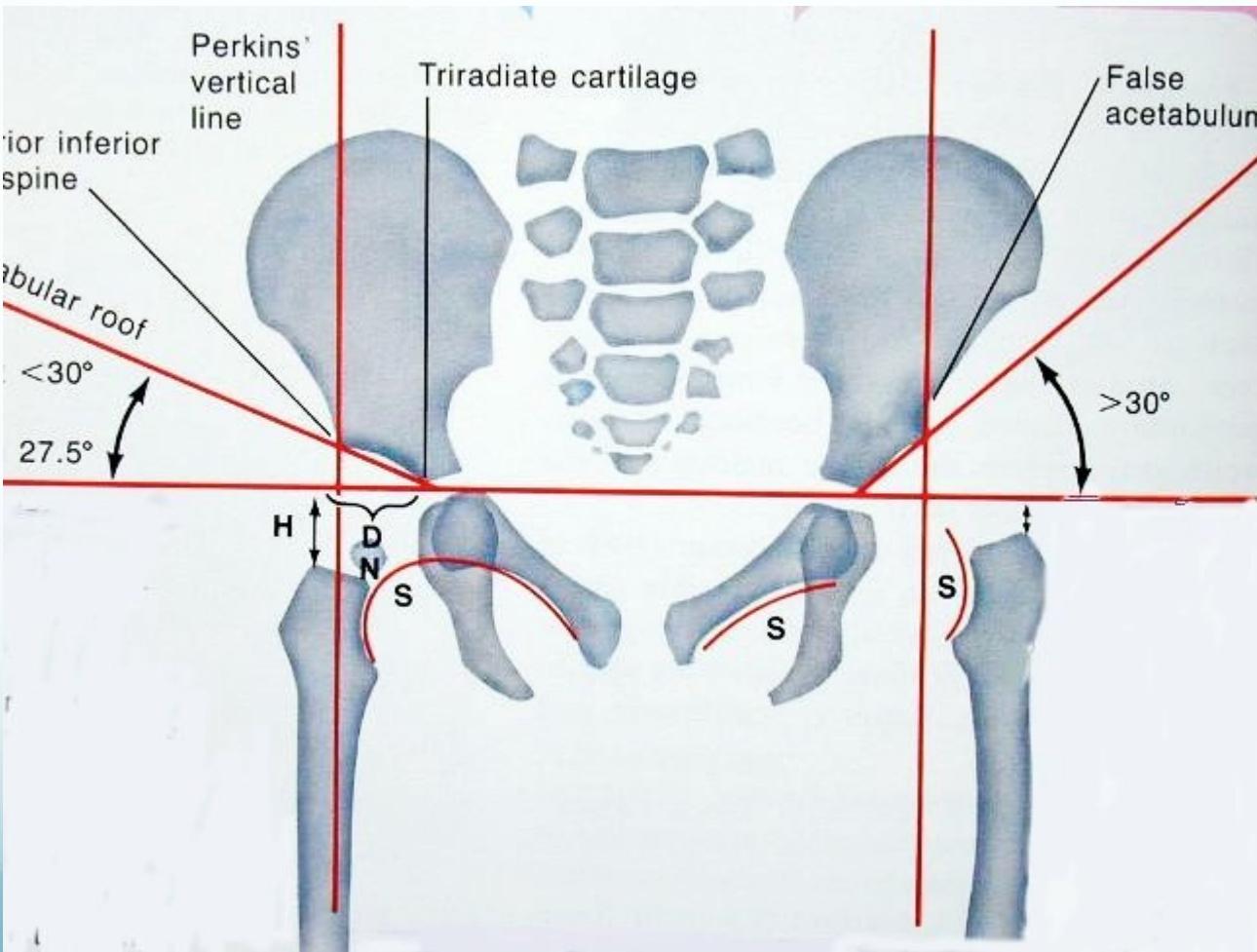

A 7-month-old infant is brought for evaluation. The parents noticed asymmetrical thigh folds and that the left leg appears shorter than the right when they change his diapers. On examination, there is a clear limitation of abduction on the left hip. An X-ray is ordered.
Question: What is the sign related to leg length discrepancy called? According to the note, what radiographic findings would confirm a dislocation, and what is the standard treatment for this age?
Answer:
- Sign: The apparent shortening of the femur is confirmed with the Galeazzi test.
- Radiographic Findings: On an AP X-ray, the femoral head would appear above the horizontal line drawn through the tri-radiate cartilage and lateral to the perpendicular line from the edge of the acetabulum. Shenton’s line would also be broken.
- Treatment: For an infant between 6-12 months, the standard treatment is a closed reduction under general anesthesia, followed by a hip spica cast.


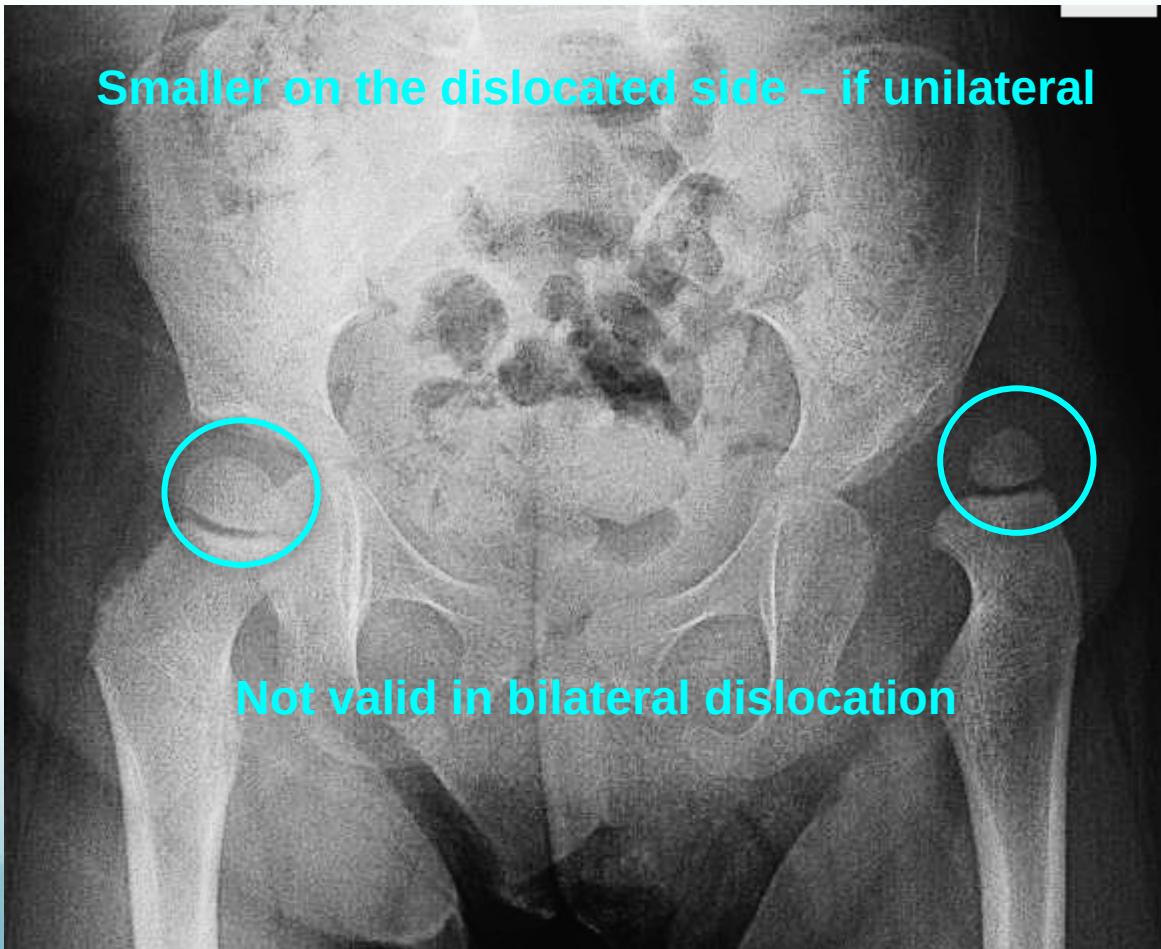
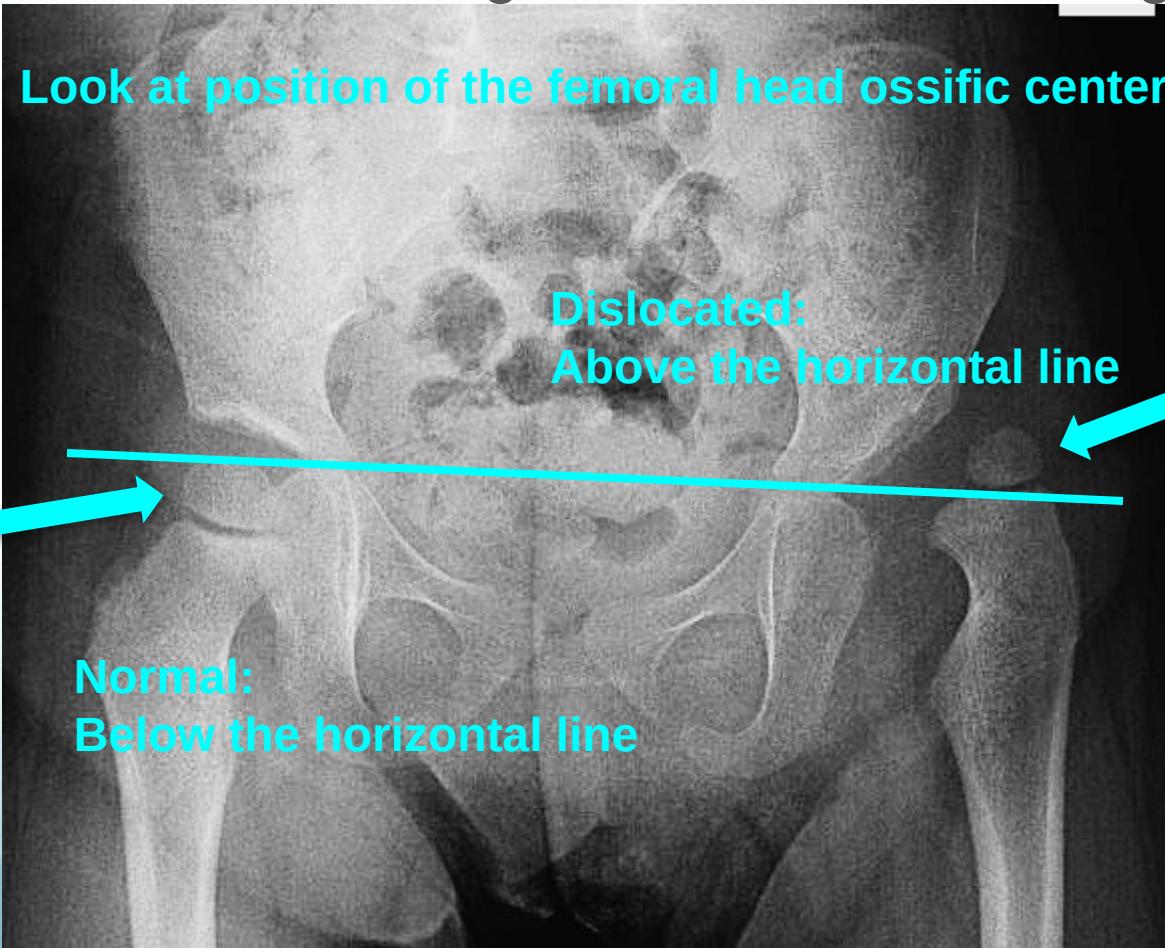
Acetabular angle (acetabular index):
Normal: ≤ 25° Dislocated: > 35°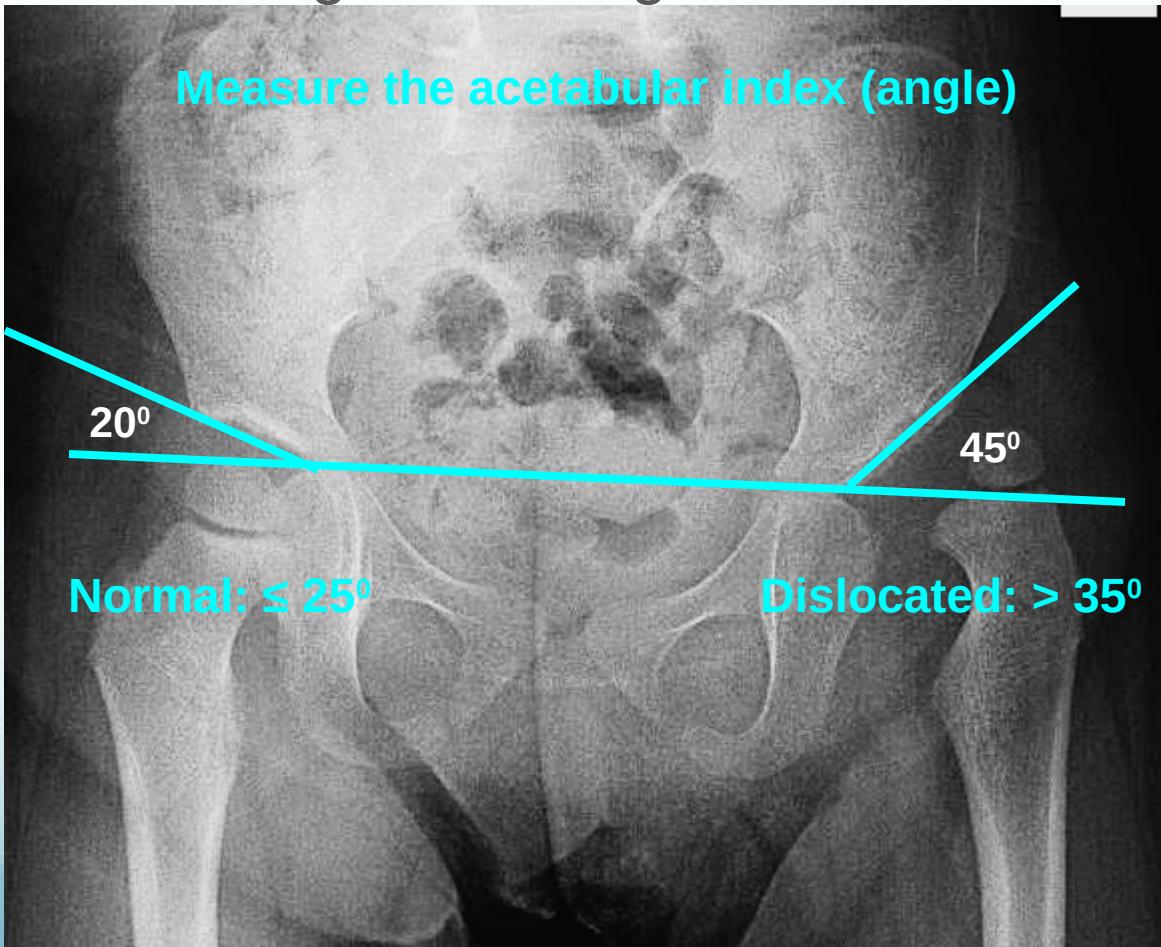
Shenton’s line: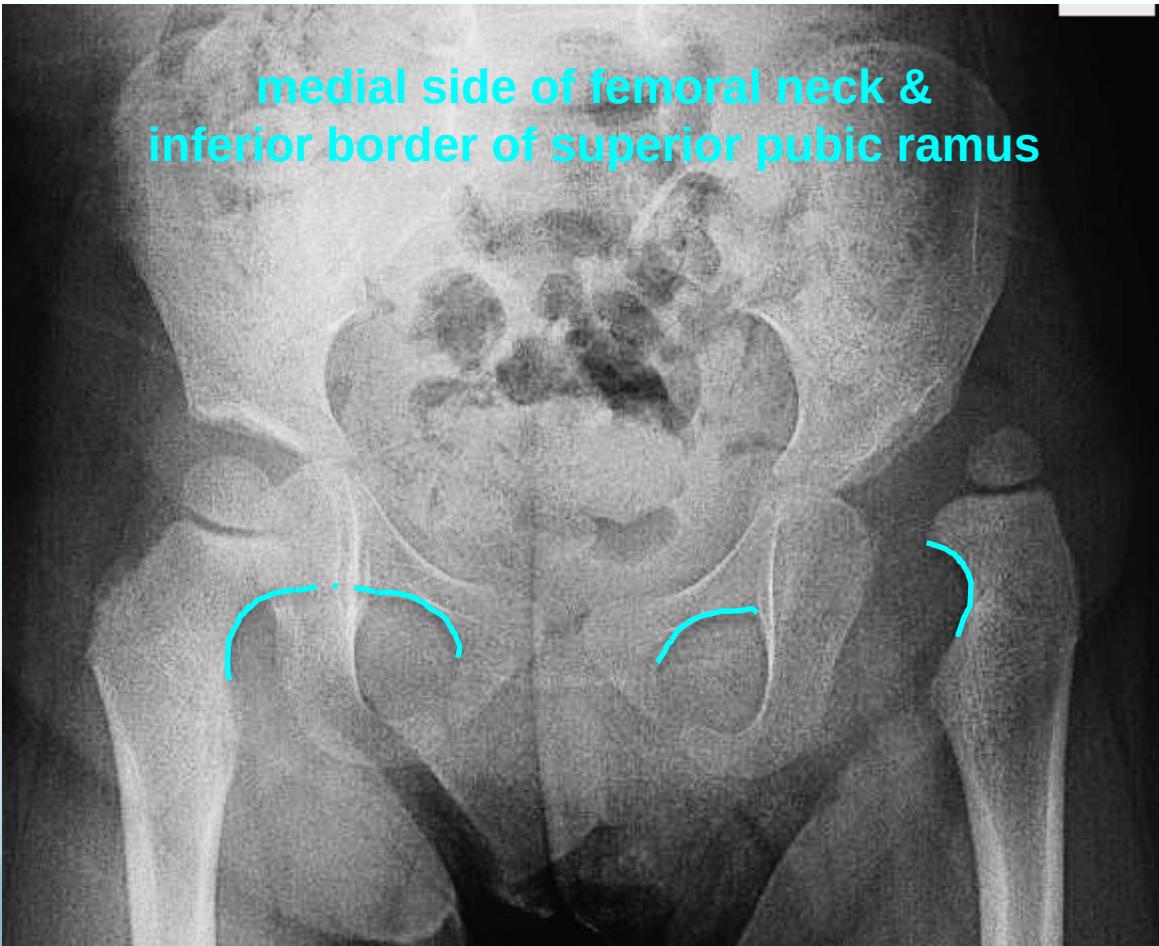
A 2.5-year-old child presents with a noticeable limp since she started walking. Her parents describe it as a “waddling” motion. An orthopedic surgeon confirms a diagnosis of bilateral DDH.
Question: What is the gait pattern described called when it is bilateral? What is the recommended surgical management for a child of this age?
Answer:
- Gait: A bilateral Trendelenburg sign results in a waddling gait.
- Surgical Management: For a child over 2 years of age, the treatment is more complex and involves surgery: open reduction, acetabuloplasty (pelvic osteotomy), and femoral shortening.
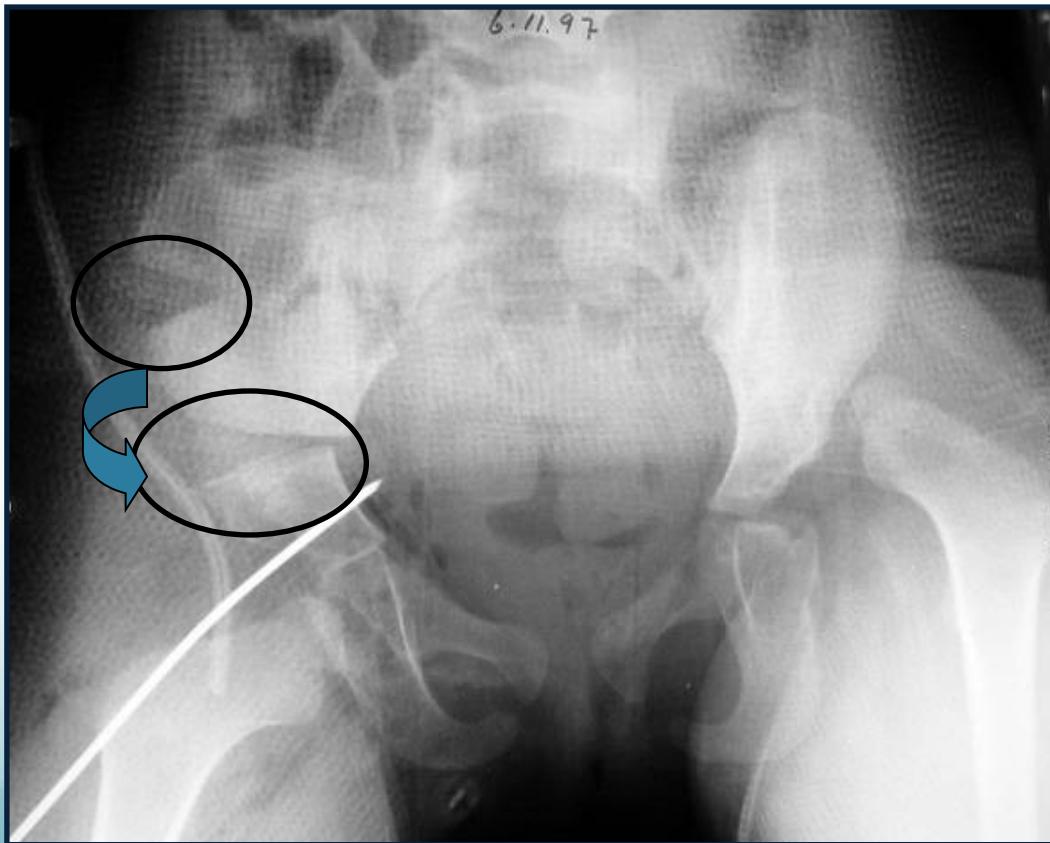 12-24m⇒
12-24m⇒  24m
24m
Cauda Equina
- Etiology: Severe compression of nerve roots in the thecal sac of lumbar spine, most commonly due to acute lumbar disc herniation
- Critical: Early diagnosis is essential
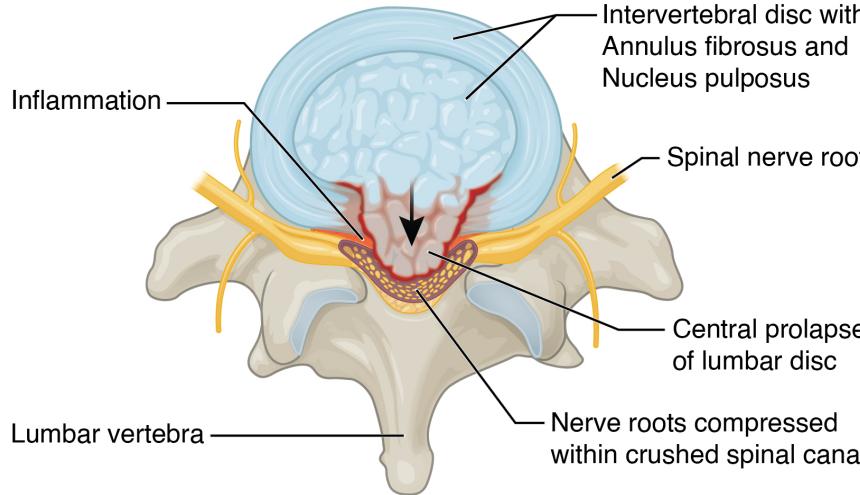
Clinical Features:
- Back pain (most common)
- Unilateral or bilateral leg pain (2nd most common)
- Saddle anesthesia (highly specific)
- Bladder dysfunction: Urinary retention → overflow incontinence
- Unilateral or bilateral sensory changes in legs
- Unilateral or bilateral motor weakness in legs
Diagnosis:
- Urgent MRI to confirm cause

Treatment:
- Prompt surgical decompression
- Should be performed within 24 hours, absolutely within 48 hours
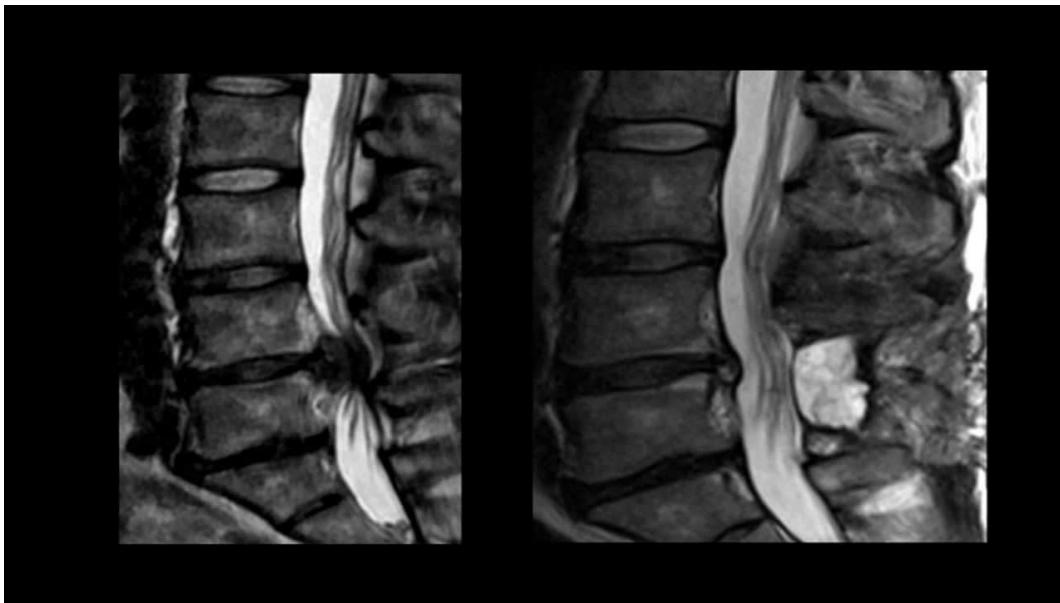
Section 2: Lower Limb Neuroanatomy
Questions 4-7: Peripheral Cutaneous Nerve Supply
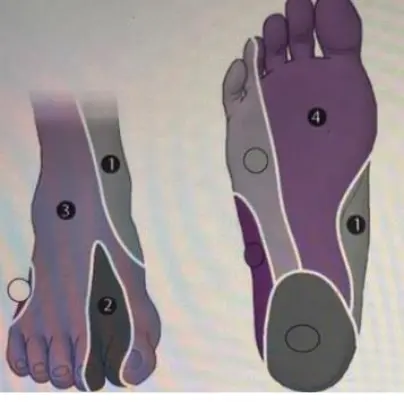 Interpret each nerve:
1- Saphenous nerve
2- Deep peroneal nerve
3- Superficial peroneal nerve
4- Medial planter nerve
Interpret each nerve:
1- Saphenous nerve
2- Deep peroneal nerve
3- Superficial peroneal nerve
4- Medial planter nerve
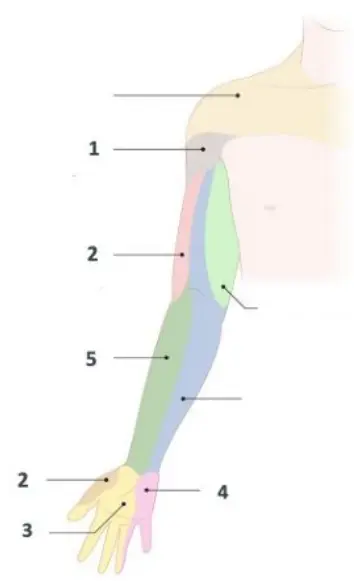 Interpret each nerve:
Interpret each nerve:
- Axillary neve
- Radial nerve
- Median nerve
- Ulnar nerve
- Musculocutaneous nerve
Other Cases
Sport Casse
Q19: What is the pathology in the shown image? 45 years old male fell from highet and landed on his shoulder and presented to your clinic with painful shoulder, What is the the pathology in the shown image?
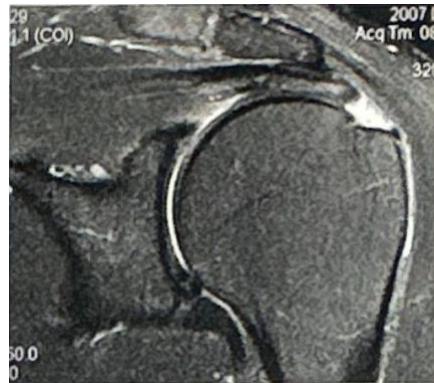
Supraspinatus tear
Q20: The yellow arrow indicates what pathology?
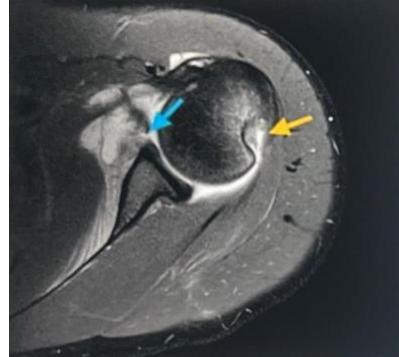
Hill-Sach lesion
Case: Rotator Cuff Tear
Clinical Presentation (2022)
- Patient: Chronic shoulder pain with limited abduction
- Imaging: MRI provided
- Assessment Required:
- Identify 2 signs on inspection (ale - making of supraspinatus)
- Describe painful arc test to identify subacromial impingement syndrome
- Identify imaging technique (MRI)
- Diagnosis: Rotator cuff tear with impingement syndrome
Imaging Findings:

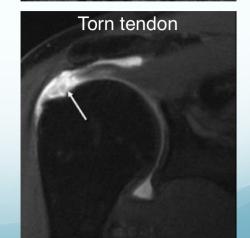
Clinical Presentation
- History: Previous shoulder dislocation
- Assessment: Describe inspection findings, painful arc, imaging studies
clinical features
- age 40-60 years
- pain
- shoulder looks normal or wasted
- tenderness
- painful abduction arch 60 to 120 degree
- neer’s test (+ve)
- Hawkin’s test (+ve)

Xray
- calcification
- degenerated ac jt
MRI
- brusitis / thickening of tendon

| Case Study | Patient Presentation | Mechanism of Injury | Key Symptoms/Examination Findings | Imaging Findings | Treatment Plan (Conservative & Surgical) |
|---|---|---|---|---|---|
| Acute ACL Injury | 23 y.o. male, right knee pain after sports injury | Twisting injury | Heard a “pop”, cannot bear weight, swelling/bruising. Positive Lachman, Anterior drawer, Pivot shift tests. | ACL tear  | Conservative: Physical therapy. Surgical: ACL reconstruction (if failed PT, high activity, desires pivoting sports). |
| Medial Meniscus Tear | 31 y.o. male, left knee pain for 4 weeks | Twisting injury after stepping in a hole | Painful with walking, limited flexion, history of “locking” and “clicking”. Joint line tenderness on medial aspect. Positive McMurray’s test. | Meniscus tear 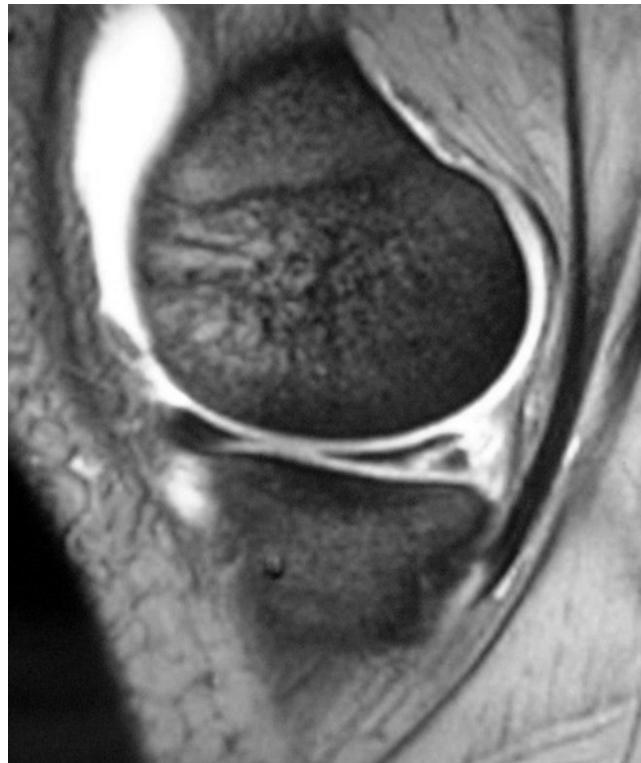  | Conservative: Physical therapy. Surgical: Diagnostic arthroscopy, Meniscal repair vs. Meniscectomy (if conservative fails). |
| Posterior Shoulder Dislocation | 29 y.o. male with seizure disorder, left shoulder pain for 2 weeks | Preceded by seizure | Shoulder locked in internal rotation, limited external rotation. Asymmetry of shoulders. | Posterior shoulder dislocation  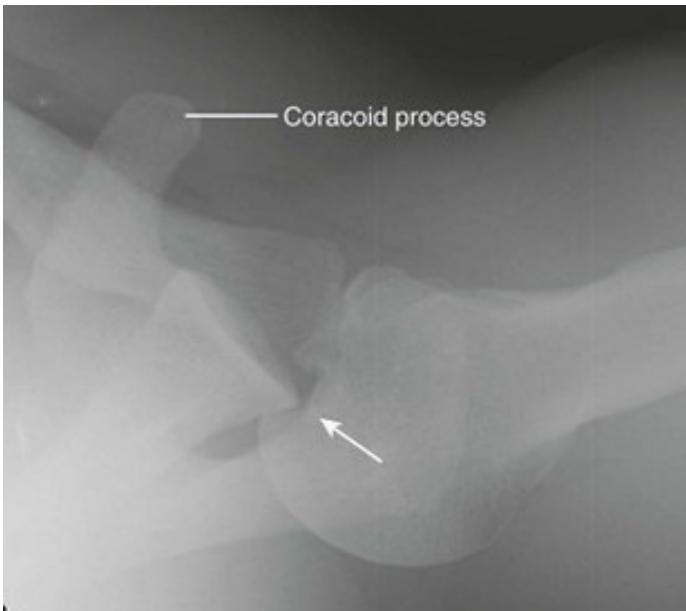  | Early (<2 weeks): Closed reduction, immobilization, physical therapy. Late (>2 weeks): Surgical intervention. Important: Seizure control. |
| Recurrent Shoulder Instability | 35 y.o. male, left shoulder pain and instability | Recurrent dislocation history | Multiple previous reductions/PT failure. Good and pain-free ROM. Positive Apprehension test. | Hill-Sachs lesion, Bankart lesion 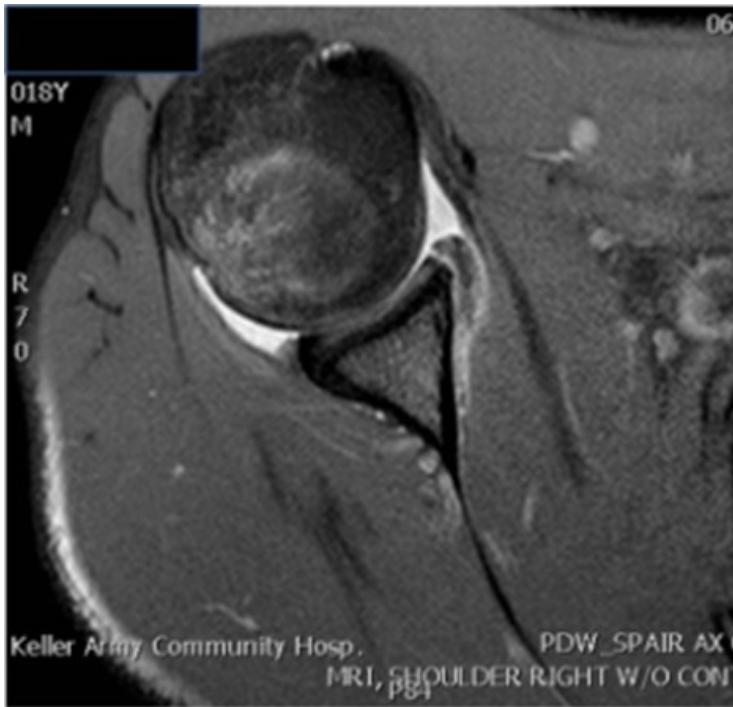 | Surgical: Bankart repair, consider capsular shift, post-op rehab. |
| Rotator Cuff Tear | 55 y.o. female, right shoulder pain | No history of trauma (insidious onset) | Night pain, cannot raise hand above head, worsening over time. Atrophy of shoulder muscles, tenderness at greater tuberosity. Limited abduction, weak abduction/ER. Positive Neer’s & Hawkin’s tests. | Rotator cuff tear 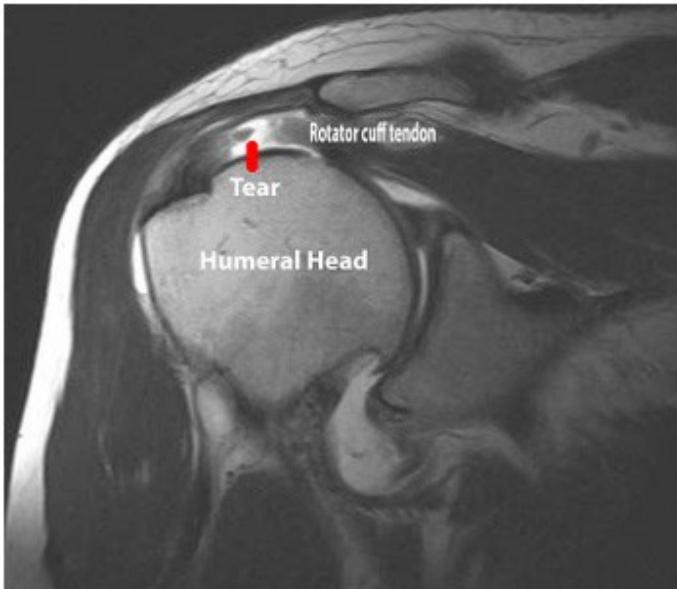  | Surgical: Arthroscopic rotator cuff repair (since PT failed, complete tear). |
Orthopedics cases
Section 1: Hip Pathology & Management
Question 1-3: Hip Osteoarthritis Case
Clinical Scenario: A 65-year-old male presented to your clinic complaining of left hip pain and stiffness for 5 years, progressive with time and affecting his activities of daily living. Conservative treatment failed to improve his pain & range of motion. On examination, there was pain and a limited range of motion, and Thomas’s test was positive.

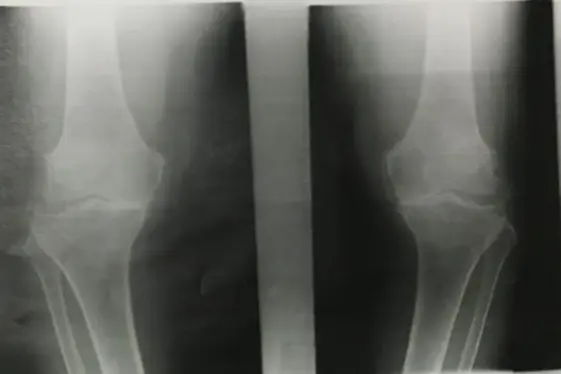

Q1: List 3 findings in the x-ray. Answer:
- Narrowing of joint space
- Osteophyte formation
- Subchondral cyst and sclerosis
- Varus deformity (knee image)
Q2: What is the diagnosis & its grade? Answer: Osteoarthritis – Grade 3-4?
Q3: What is the gold standard treatment for this patient at this stage? Total hip Arthroplasty for hip image
generally treatment Start with conservative treatment: patient education, weight loss and physical therapy. Pharmacological ( Paracetamol, NSAIDs). If conservative failed, surgery as above
Case: Posterior Hip Dislocation
Clinical Scenario
- Patient: 28-year-old car driver involved in motor vehicle accident
- Presentation: Conscious and oriented, left hip pain, unwilling to move hip due to pain
Physical Examination Findings:

Assessment Questions
Q1: Describe what the clinical picture shows?
- Short limb, internally rotated and adducted hip, flexed knee
Q2: Write three differential diagnoses?
- Posterior hip dislocation
- Femur fracture (neck, midshaft, distal)
- Pelvis fracture
Radiographic Findings:

Q3: What is the diagnosis? Posterior hip dislocation
Q4: Describe the management plan?
- Start with ATLS protocol (ABC)
- Control bleeding, immobilize limb, provide analgesia
- Most important: Reduction under anesthesia and sedation
- Imaging after reduction, CT to ensure no bony fragments disturb joint movement
Q5: Mention two possible complications?
- Avascular necrosis (AVN)
- Sciatic nerve injury
Infections & Tumours
Infections & tumor
| Case | Initial Workup | Diagnosis | Key Characteristics | Treatment Options | Image Attachments … |
|---|---|---|---|---|---|
| 1: Pediatric Elbow Infection 6 years old Localized tenderness, hotness & local redness, swelling & edema, reduced ROM of elbow | CBC, CRP, ESR, Blood culture, Aspiration (Gram stain, C&S), Imaging Studies (X-ray, Bone Scan, MRI) | Osteomyelitis, Cellulitis, Septic arthritis (DDx), Ewing sarcoma (DDx) | Early onset, inflammatory signs, pain, fever, leukocytosis, elevated CRP/ESR. Aspiration fluid analysis (clear colorless, clear yellow, turbid, pus, blood). X-ray signs (10-14 days), MRI perfect for early detection. | Supportive treatment, Splint immobilization, Antibiotic therapy (I.V. flucloxacillin, modify based on C&S, consult microbiologist), Surgical intervention (debridement, drainage) |   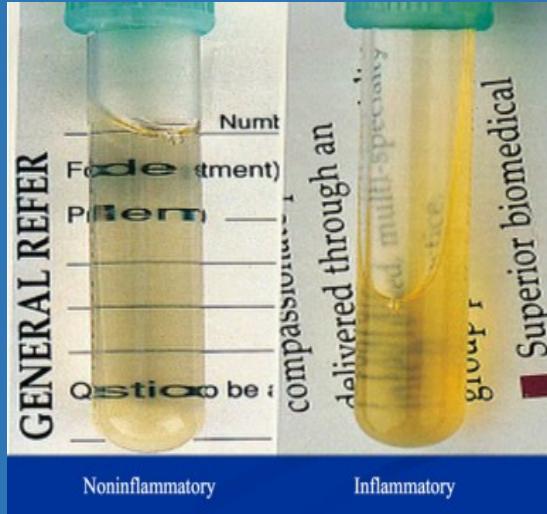  |
| 2: Distal Femur Mass 16 years old Painless swelling at distal right femur, no inflammatory signs, no systemic symptoms | X-ray imaging of distal femur | Osteochondroma (Exostosis) | Bony exostosis with hyaline cartilaginous cap. Usually asymptomatic, common complaint: hard palpable mass. Symptoms from location, size, or pressure effects. Complications: growth disturbance, rare malignant transformation (1% in solitary). | Observation for asymptomatic lesions, Surgical excision for symptomatic/complicated cases, Regular monitoring. |   |
| 3: Pathological Fracture 11 years old Pain in right arm after fall, no significant medical history, incidental discovery of bone lesion on X-ray | X-ray | Simple Bone Cyst | Solitary (unicameral) lesion. Affects children (5-15 years), metaphyseal location, not in adults. Commonly discovered by pathological fracture. Differentiated from Aneurysmal Bone Cyst (expansile) and Giant Cell Tumor (sub-articular, after physeal fusion). | Observation (cyst might heal spontaneously), Multiple bone marrow injections, Fracture fixation (flexible IM nailing), Surgical curettage and bone grafting. | 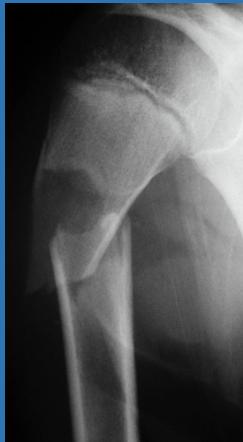      |
| 4: Aggressive Bone Tumor 18 years old Painful mass at right femur, limited knee joint motion, history of trauma (8 weeks prior) | Radiographic findings, Staging Investigations (CT chest, MRI entire bone, Bone scan) | Osteosarcoma | Radiographic features: Radiolucency, sclerosis, poorly defined margins, extension into soft tissue. Periosteal reaction: Sunburst appearance, Codman’s triangle. History of trauma with initial misdiagnosis as contusion. Mandatory staging. | Metastasis workup (well-planned incision for biopsy), Neoadjuvant chemotherapy, Surgical management (wide resection, custom prosthesis), Adjuvant chemotherapy. | 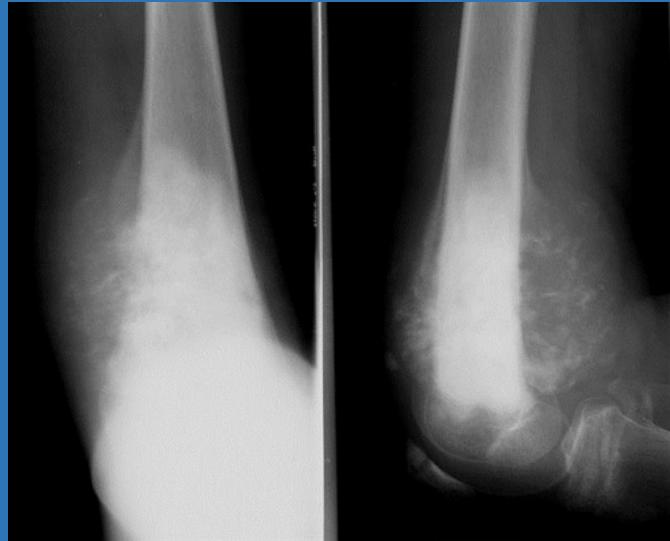 |
Station 5: Tumor Assessment
Bone Tumor Radiological Assessment:
Clinical Scenario: A 30-year-old male complaining of left knee pain for the last 3 months. Physical examination: patient is limping, local exam unremarkable.
Radiological Findings:

Questions:
a) Mention four x-ray descriptions:
- Eccentric lesion
- Radiolucent
- Soap bubble appearance
- Abuts against the joint
- Thin cortex
- Narrow zone of transition
- No periosteal reaction
b) Does the lesion look benign or malignant? Benign

- Mention three X-ray findings:
- Periosteal reaction involving the mid-tibia
- Sunburst sign
- Wide zone of transition
- Is it benign or malignant?
- Malignant
- How can you reach a definitive diagnosis?
- Diagnosis is made with a biopsy
Osteomyelitis Cases
Subacute/Chronic Osteomyelitis
Clinical Presentation
- Common Age: 7-year-old boy
- Symptoms: Pain in right thigh and knee for 3 weeks, swollen tender thigh
- X-ray Findings: Metaphyseal rarefaction, periosteal formation, cavitation, sequestrum formation in distal femur
Diagnostic Criteria
X-ray Findings:
- Osteopenic tibial metaphyseal rarefaction
- Periosteal reaction (new bone formation)
- Later changes: Increasing ragged appearance (mottling), sclerosis, rarefaction, cavitation, sequestrum, involucrum
Most Common Causative Organism: Staphylococcus aureus
Clinical Features
- Severe pain, malaise, fever
- Reluctant to move (“pseudoparalysis”)
- History of previous source of infection
- Localized pinpoint tenderness, hotness, local redness, swelling
Timeline Progression:
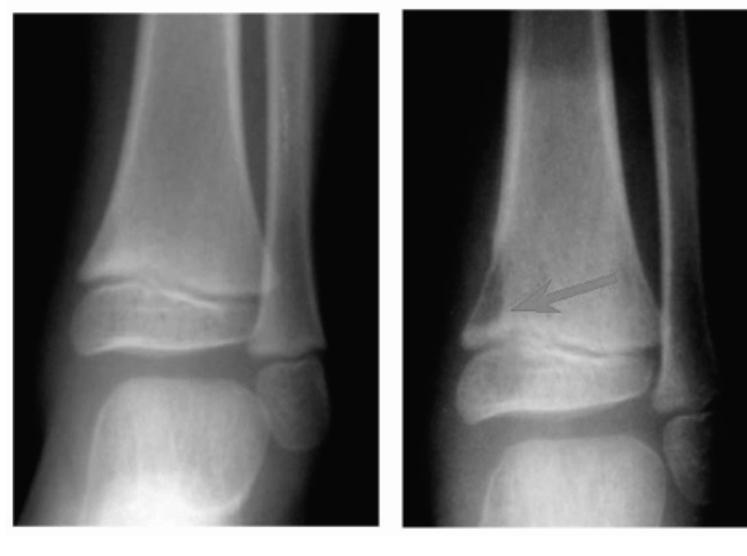 Initial X-ray → After 2 weeks
Initial X-ray → After 2 weeks
Advanced Imaging
MRI Findings:
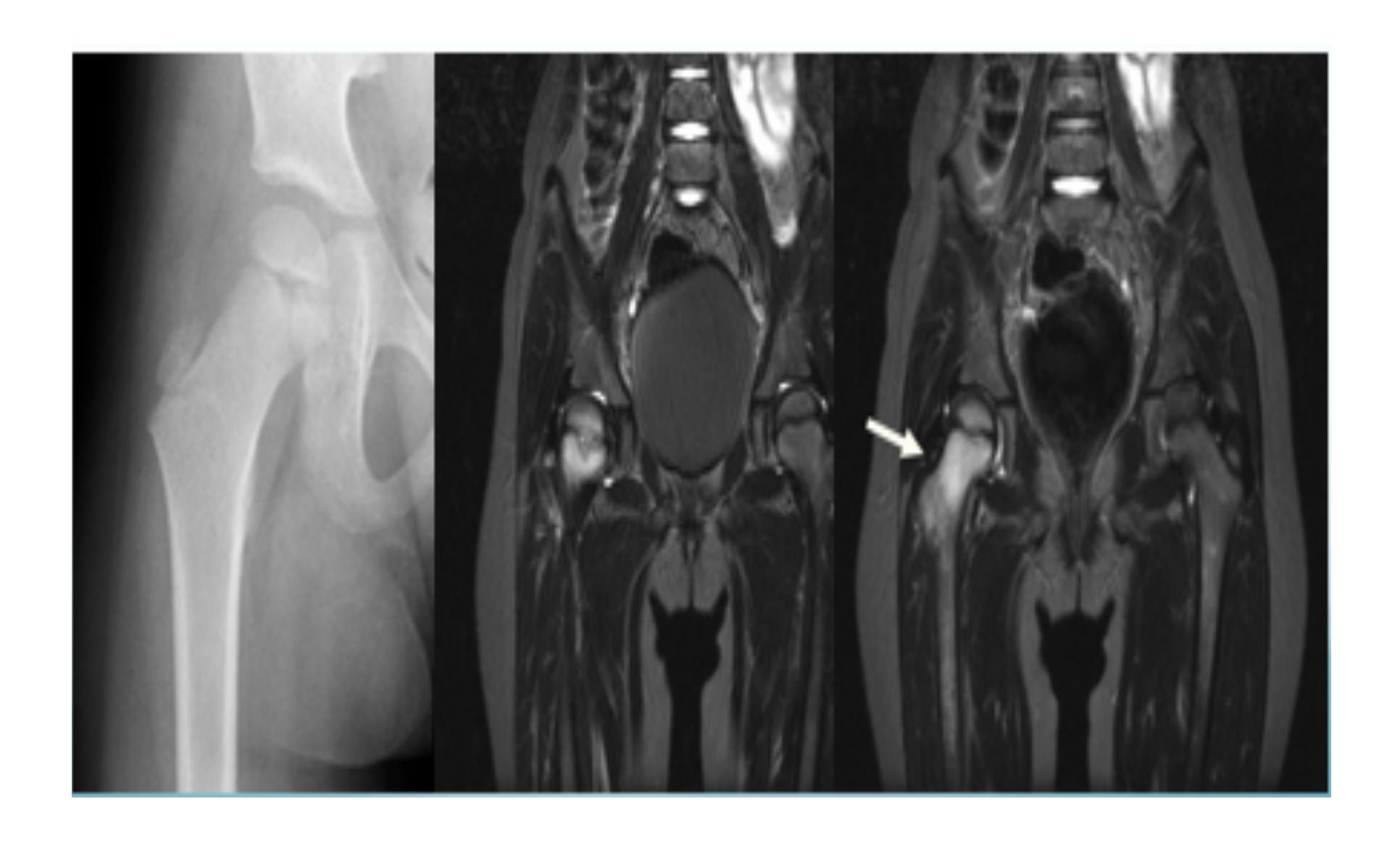
Ultrasound Findings:
- Sub-periosteal pus collection
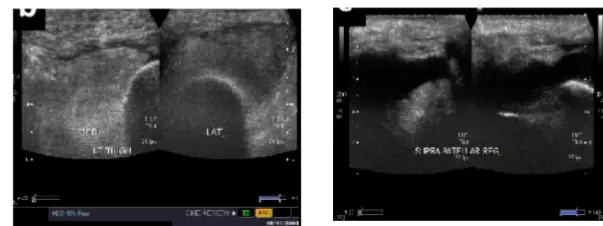
Differential Diagnosis
- Cellulitis
- Acute septic arthritis
- Acute rheumatism
Treatment Protocol
- Supportive Treatment: Pain control, hydration
- Immobilization: Splint
- Antibiotics:
- I.V. antibiotics for 6 weeks
- Oral antibiotics for 3-6 weeks (if CRP returns to normal)
- Surgical Drainage: If fever and tenderness persist >36 hours after starting antibiotics
Complications
- Septicemia
- Metastatic infection
- Septic arthritis
- Chronic osteomyelitis
Subacute Osteomyelitis (Brodie’s Abscess)
Clinical Features
- X-ray Findings: Well-defined cavity in metaphysis
- Presentation: Long history of pain, swelling, local tenderness
- Treatment: Antibiotics for 6 months, surgical evacuation of abscess
Imaging Findings:
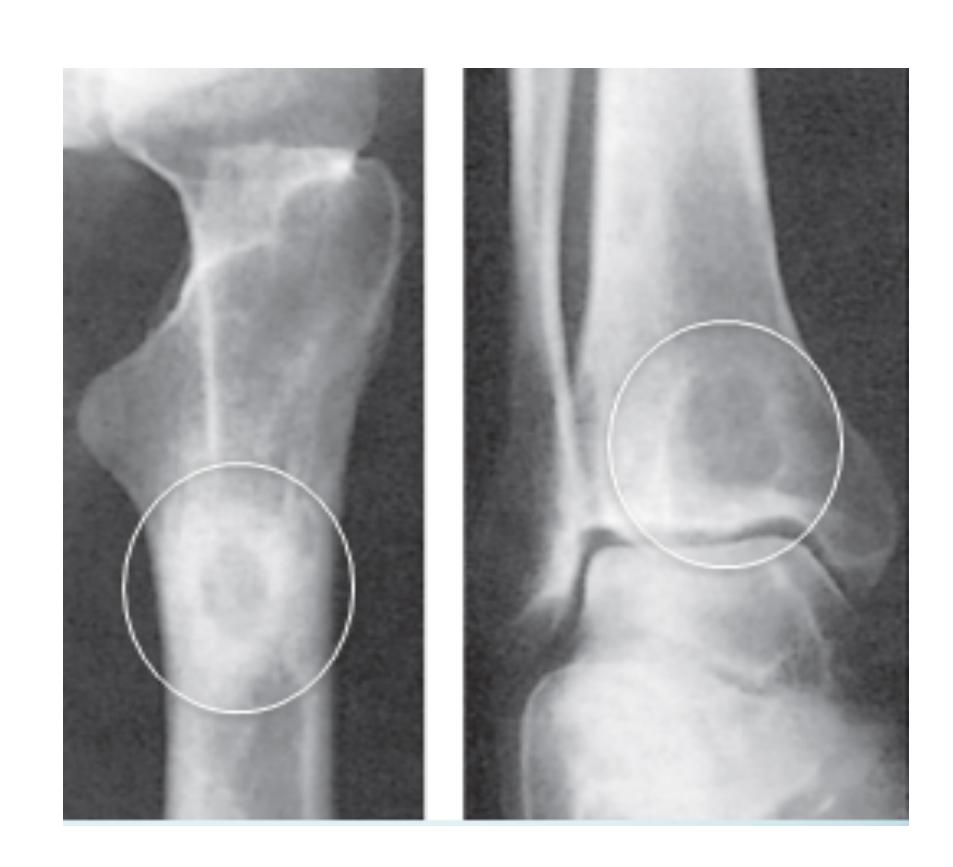
Chronic Osteomyelitis
Clinical Features
- X-ray Findings: Rarefaction surrounded by sclerosis, cavities, sequestra
- Presentation: Recurrent bouts of pain, redness, tenderness, fever, sinuses
- Treatment: Antibiotics, sinogram, sequestrectomy, surgical debridement
- Complications: Recurrence, pathological fracture, growth disturbance
Imaging Findings:


Bone Tumors
Benign Tumors
Osteochondroma (Exostosis)
Clinical Features:
- Age: 16-year-old boy
- Presentation: Painless swelling at distal right femur
- No inflammatory signs, no systemic symptoms
Nerve? Common peroneal nerve (doreseflexion)
X-ray Findings:
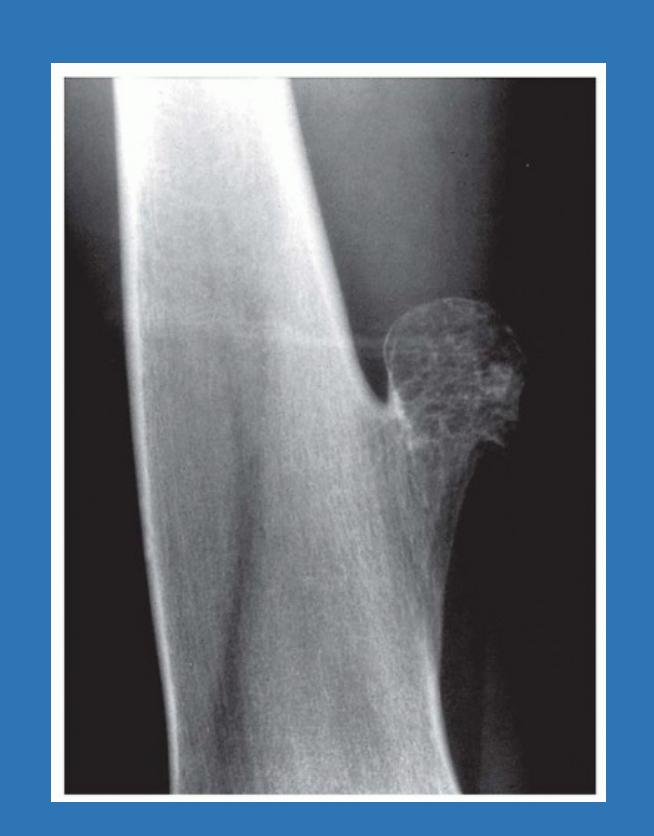
Characteristics:
- Bony exostosis projecting from external surface of bone
- Hyaline cartilaginous cap
- Usually asymptomatic
- Symptoms from location, size, pressure on adjacent structures
Complications:
- Growth disturbance (in multiple lesions)
- Malignant transformation (rare in solitary lesions: 1%)
Simple Bone Cyst
Clinical Features:
- Age: 11-year-old boy
- History: Right arm pain after fall
- No medical illness
Characteristics:
- Solitary unicameral cyst
- Children (not seen in adults)
- Metaphyseal location
- Often discovered by pathological fracture
Treatment Options:
- Observation (may heal spontaneously)
- Multiple bone marrow injections
- Fracture fixation (flexible nail)
- Surgical curettage and bone grafting

Differential Diagnosis of Cyst-like Lesions:
| Lesion Type | Location | Expansion Pattern | Age Group |
|---|---|---|---|
| Simple Bone Cyst | Fills medullary cavity | Does not expand bone | Children |
| Aneurysmal Bone Cyst | Metaphyseal side of physis | Expansile | Variable |
| Giant Cell Tumor | After physeal fusion | Extends to sub-articular | Young adults |
| ![[MedAtlax/Clinical/Level 11/Orthopedics/OSCE/attachments/attachments/cases-1762476028972.webp | 300 | 700x204]] |
Malignant Tumors
Osteosarcoma
Clinical Features:
- Age: 18-year-old female
- Presentation: Painful mass in right femur
- Limited knee joint motion
- History: Trauma 8 weeks ago (initially diagnosed as contusion)
- Red Flag: Night pain
X-ray Findings:
- Radiolucency and sclerosis
- Poorly defined margins
- Extension into soft tissue
- Periosteal reaction:
- Sunburst (sun-ray) appearance
- Codman’s triangle
Staging Investigations:
- CT Chest: Mandatory for pulmonary metastasis evaluation
- MRI: Entire involved bone, determines soft tissue/marrow involvement
- Bone Scan: Discover skip lesions (always hot)
Treatment Protocol:
- Search for metastasis
- Well-planned incision
- Chemotherapy
- Surgical wide resection with custom-made prosthesis
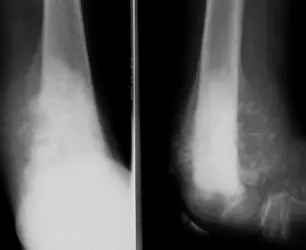
Knee pain & Degenerative disease
Degenerative Joint Disease
Osteoarthritis of the Knee
Clinical Presentation
- Age: 54-year-old lady
- Duration: Bilateral knee pain for 3 years
- History: No clear trauma history
History Taking Framework (SOCRATES)
- Pain: Site, onset, character, radiation, associated symptoms, time course, exacerbating/relieving factors, severity
- Activity-related pain: Increases with movement
- Sleep disturbance: Pain affects sleep
- Functional impact: Stiffness, limited ROM, difficulty with stairs, chair rising
- Medical history: Menopause, diet (osteoporosis risk), chronic diseases
Physical Examination Protocol
General Assessment:
- Weight, height, BMI
- Pain level, comfort, overall appearance
Local Examination (Look, Feel, Move):
- Deformity: Usually genu varus
- Muscle wasting: Thigh muscle atrophy
- Swelling/Effusion: Joint line swelling, Baker’s cyst (popliteal cyst)
- Tenderness: Joint line tenderness, warmth
- Range of Motion: Limited movement
- Special tests: Gait assessment, neurovascular examination
Investigation Protocol
Radiographic Studies:
- AP & lateral weight-bearing views
- Sunrise view (patellofemoral assessment)
- PA view in 30° flexion
X-ray Findings:
- Joint space narrowing (medially)
- Osteophyte formation
- Subchondral sclerosis
- Subchondral cysts
- Loose bodies
- Deformity

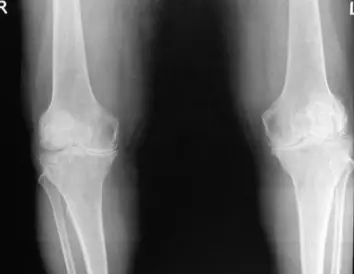
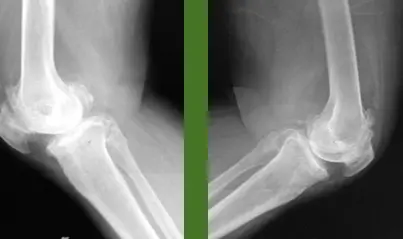
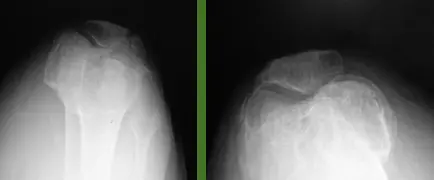
Additional Investigations:
- CT scan (for surgical planning)
- MRI (for soft tissue assessment)
- Laboratory studies (to rule out other differentials)
- Arthrocentesis (joint aspiration):
- Clear fluid, WBC <2000/mm³, normal viscosity
Management Protocol
Conservative Management:
- Weight reduction
- Walking aids
- Physiotherapy
- Pain management (NSAIDs, analgesics)
Surgical Management:
- Timing based on severity and functional limitation
- Options range from arthroscopy to total knee replacement
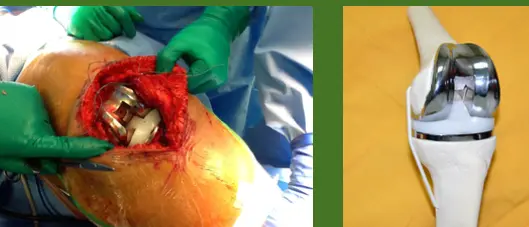
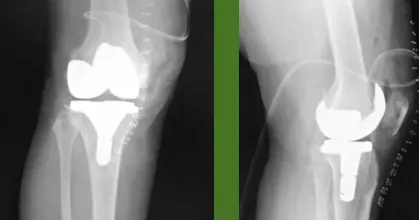


| Section | Topic | Details | Attachment Link |
|---|---|---|---|
| Case 1: Lady with Chronic Knee Pain | Patient Presentation | 54-year-old lady, pain in both knees for 3 years, no clear trauma history. | |
| Comprehensive History | Pain assessment (characteristics, severity, impact), Medical background (occupation, meds, comorbidities, menopause, diet). | ||
| Clinical Examination | General assessment (pain level, comfort, weight, general appearance), Local Examination (position, attitude, extra-articular findings, systematic exam: Look, Feel, Move). |  | |
| Diagnostic Investigations | Laboratory Studies (CBC, inflammatory markers, metabolic panel, RF if indicated), Imaging Studies (AP standing, lateral, skyline views of both knees). |       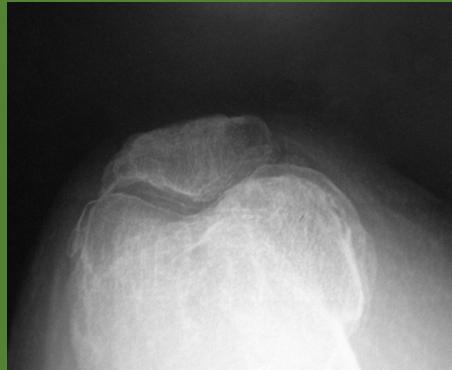 | |
| Management Strategy | Conservative (weight reduction, walking aid, PT), Medical (NSAIDs, analgesics, disease-modifying agents, intra-articular injections), Surgical (timing, arthroscopy, osteotomy, TKA). |     | |
| Case 2: Young Patient with Acute Knee Injury | Patient Presentation | 25-year-old patient, right knee pain, history of acute sports injury. | |
| Injury Mechanism | Acute Phase (immediate pain, violent rotation with flexion, immediate swelling/hemarthrosis, delayed swelling/effusion), Subacute/Chronic Phase (giving way episodes, repeated attacks of swelling/pain, functional limitation). | ||
| Clinical Examination Findings | Physical Signs (swelling pattern, quadriceps wasting, functional instability), Special Ligament Tests (Anterior drawer, Lachman’s, Pivot shift). |  | |
| Diagnostic Imaging | Hip osteoarthritis comparison images (for context, not direct knee injury imaging). |  | |
| Treatment Approach | Non-Surgical (PT for quad strengthening, proprioception, ROM, activity modification, bracing), Surgical Indications (active individuals with instability, recurrent instability, failed conservative, early arthritic changes). |      | |
| Post-Operative Rehabilitation | Phase 1 (protected/early controlled motion), Phase 2 (strengthening, proprioception), Phase 3 (return to specific activities), Phase 4 (return to sports). | 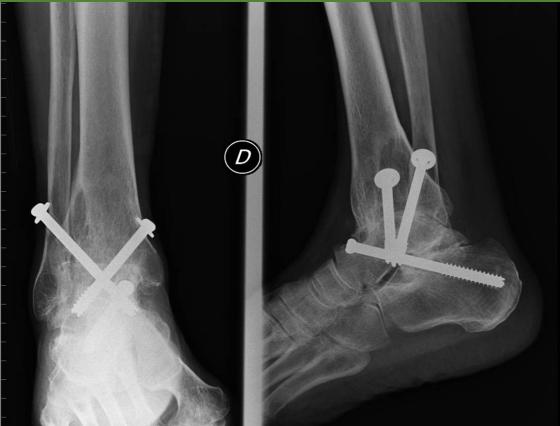 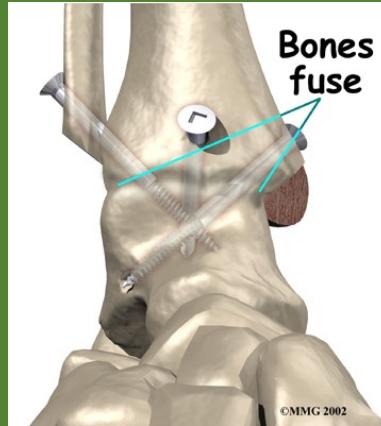 |
Station 1: Knee Ligament History Taking
Clinical Scenario: A 21-year-old male presented to the clinic with history of right knee instability for three months.
ACL Injury History Framework:
Demographic Data:
- Name, Age, Gender, Occupation, current living location
- Chief complaint: Instability, knee pain
- Onset: Since when? Was it preceded by any event? & How did it occur?
Key Questions for Knee Ligament Injuries:
- SOGRATES pain assessment
- Have you heard popping sound?
- Were you able to complete the game?
- Did you notice any knee swelling at the time of event?
- Giving away sensation (“can’t trust your knee”)?
- Mechanical symptoms (“Locking & clicking”)?
- First aid provided?
- Limited range of movement or stiffness?
Associated Symptoms:
- Deformity, Pain, Swelling, Stiffness, Instability
- Altered sensation, Weakness, Loss of functions
- Limping & constitutional symptoms
Past Medical History:
- Similar episodes, Chronic diseases
- History of surgery, trauma, blood transfusion
- Hospital admissions, medications, known allergies
- Use of orthotics
Functional Assessment:
- Difficulty rising from chair, climbing stairs, praying?
- Walking distance capacity
- Level of activity: Type of sport & intensity
Differential Diagnosis Table:
| Condition | Mechanism of Injury (MOI) | History and Symptoms (Hx/ssx) | Special Tests | Diagnosis (Dx.) | Treatment (Tx.) |
|---|---|---|---|---|---|
| ACL | Non-contact pivoting injury (+/- lateral meniscal tear) | Deep knee pain, Pop during event, immediate Swelling, pt leaves filed, in chronic phase= Giving away | 1. Ant drawer test 90flexion 2. Lachman’s test most sensitive 30flexion 3. Pivot shift test (extension-flexion w/ internal rotation) | X-ray (NL or Segond fracture) + MRI (sagittal view) shows high signal sign | 1. Low demand pt: Non-OP: physiotherapy = Hamstring strengthening 2. Young pt or Active “athletic” =ACL reconstruction arthroscopy |
| PCL | Direct blow to prox tibia w/flexed knee “Dashboard injury” or Hyperextension | Post knee pain or asymptomatic (isolated PCL) | 1. Post. drawer test 90flexion 2. Post. Sag sign | X-ray (+/- avulsion fractures) + MRI (sagittal view) shows high signal sign | 1. Isolated PCL = Non-OP: physiotherapy = Quadriceps strengthening 2. Combined ligament injury or Bony avulsion =PCL reconstruction arthroscopy +/- bony avulsion repair |
| Meniscus | Foot’s planted & sudden change in direction “twisting knee” occurs e.g., basketball, football | Localized pain, Swelling & mechanical symptoms (locking & clicking) | 1. Joint line tenderness 2. McMurray’s test (pain or pop = +ve test) IR = testing Lateral meniscus ER = testing medial meniscus | X-ray NL, MRI (sagittal view) shows “double PCL” sign = Bucket handle tear | 1. Degenerative tear = Non-OP 2. Non-vascularized white zone, complex, degenerative= Partial meniscectomy 3. Vasularized region “red zone” = Meniscal repair (NB. Repair ACL first if concomitant ACL tear) |
Emergency Case
Case D: Femoral Shaft Fracture

Clinical Scenario: Adult patient victim of MVA, brought to ER by red crescent, isolated injury shown in radiograph.
Questions:
-
What is the diagnosis?
- Answer: Proximal 1/3 femur fracture
-
Describe the position of proximal fragment?
- Answer: Laterally
-
What is the muscle responsible for adduction (varus angulation) of distal fragment?
- Answer: Adductor magnus, adductor longus, adductor brevis
-
What is the first line of management in emergency room?
- Answer: Apply ATLS, Realign the limb, Apply neurovascular assessment, Immobilization
Spine case
Case: Spondylolisthesis
Clinical Presentation
- Patient: 45-year-old lady
- Complaint: Disturbing low back pain radiating to buttock
- Aggravating Factors: Increased by physical activity
- Clinical Findings: No neurological deficit, flat buttock, step sign on back examination
Q1: What is the most probable diagnosis? Spondylolisthesis (spondylolytic type)
Q2: What imaging do you need to confirm your diagnosis? X-ray (oblique views & lateral)
Radiographic Findings:

Q3: X-ray was done, mention 2 abnormalities showing in the image?
- Anterior vertebral displacement
- Affection (disruption) of the pars interarticularis
Q5: What is your management plan?
- Conservative Treatment: NSAIDs, local heat packs, physiotherapy (patient not older with no severe symptoms)
- Surgical Treatment: Spine fusion (if severe symptoms and older patient)
Station 4: Data Interpretation
Case A: Spinal Trauma

A ) What is the most likely diagnosis?
- L2 Burst fracture
B ) Is it stable or unstable?
- unstable
C ) What is your management in the emergency room?
- Primary and secondary ATLS surveys
- Neurovascular examination
- strict log‑rolling and collar
- Admission
- Book for surgery
Note: you should mention neurovascular examination separately, not as part of primary and secondary surveys.
Name this test and what it’s indicating for?
- Spurling test
- Cervical radiculopathy
Case: Lumbar Disc Herniation
Clinical Presentation
- Patient: 48-year-old man
- Complaint: Low back pain radiating to right leg
- Clinical Findings: Limited forward flexion of spine, positive SLR test
X-ray Interpretation:
- AP + Lat view of the spine
- Disc prolapse in L4-5, going to the right (as mentioned in scenario)
- Osteophytes present
- Narrow intervertebral spaces
- Slight loss of lordosis
- Maintained alignment
- No sclerosis
MRI Interpretation:
- Narrow disc space between L4-5
- Disc bulging (herniation) to the right
- L5 Root will be affected
- Query L4 Root affection
MRI Findings:
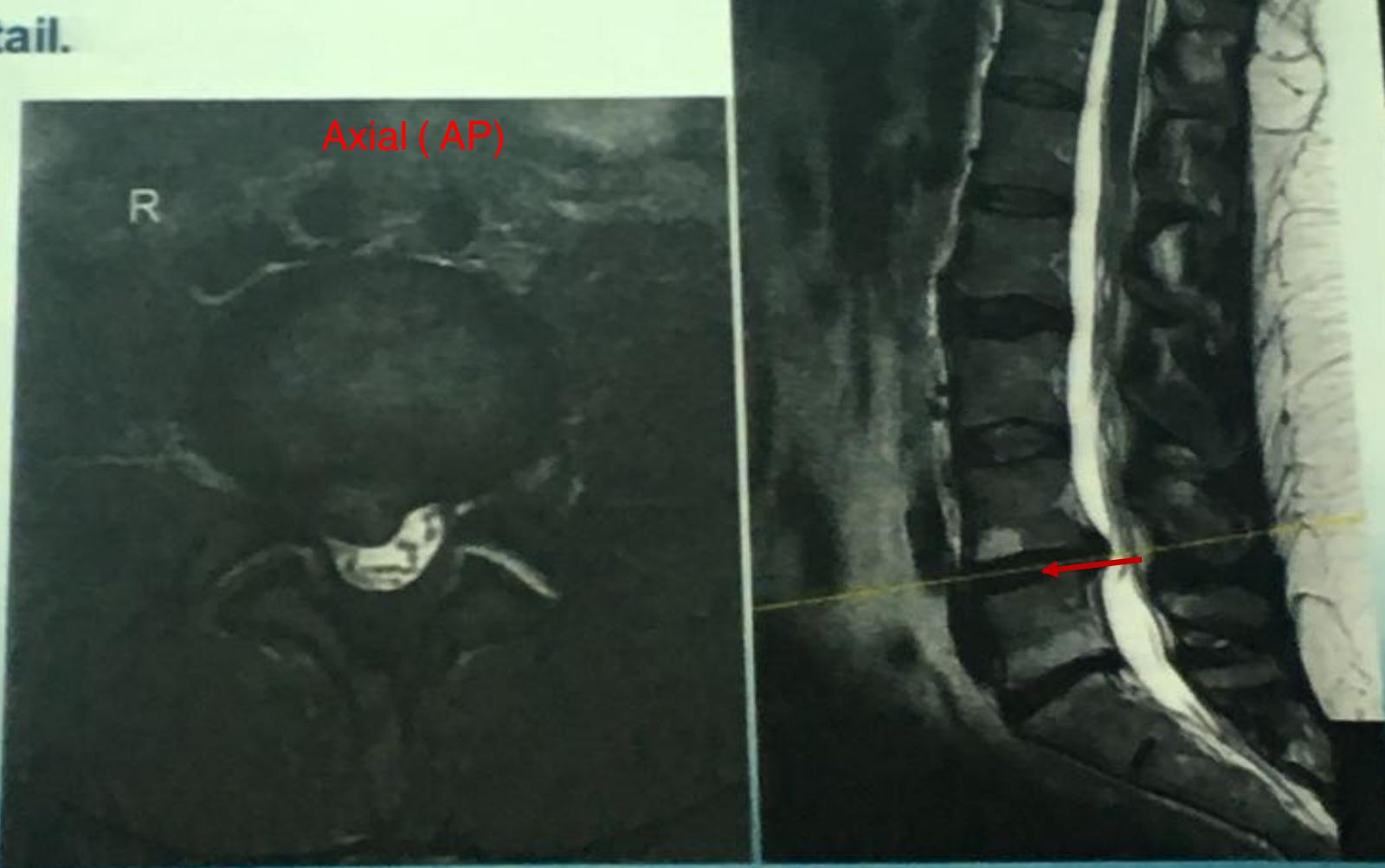
Management Plan
- Conservative Treatment: Analgesics, pain control, physiotherapy, weight control, stretching
- Surgical Treatment: Discectomy (for persistent pain)
21st Case: A 45-year-old man came with back pain radiated to his left leg.
Abnormalities in X-ray (AP and lateral views):
- Loss of lumbar lordosis
- Deformity in vertebral bodies
- Narrow cartilage space between L2-L3 and L4-L5
- Reduced bone density
Most appropriate next investigation:
- MRI
Pathological
Osteoporosis Pathological Fracture
Clinical Scenario
- Patient: 44-year-old female
- Presentation: Right leg pain, no trauma history
- Medical History: Malabsorption or GI problems
- Presumptive Diagnosis: Metabolic or endocrine disorder causing pathological fracture
Recommended Investigations:
- DEXA scans
- ESR, serum calcium and phosphate
- Urinary calcium and phosphate
- Vitamin D level
- PTH level
- Serum ALP
- CRP
- Osteoclastic activity markers
- Bone turnover rate measures
- Renal profile, LFT
Osteomalacia Pathological Fracture
Clinical Scenario
- Patient: 38-year-old vegetarian lady
- Presentation: Pain for one year
- X-ray: Pathological fracture
Diagnostic Workup:
- Serum Calcium: Slightly low/normal
- Serum Phosphate: Slightly low/normal
- Vitamin D Level: Low
- Urinary Calcium: Very low
- Alkaline Phosphatase: High (increased bone turnover)
- PTH Level: Increased (secondary to maintain serum calcium)
Clinical Picture:
- Osteopenia
- Thin cortex
- Deformity
- Severe cases: Tetany, convulsions
Common Orthopedic Emergencies
| Condition | Key Features | Immediate Management |
|---|---|---|
| Open Fracture | Skin break, exposed bone | ABC, cover wound, splint, antibiotics |
| Posterior Hip Dislocation | Short limb, internal rotation | ABC, reduction under anesthesia |
| Septic Arthritis | Fever, joint pain, refused movement | Aspiration, IV antibiotics, drainage |
| Compartment Syndrome | Pain out of proportion, pallor | Fasciotomy |
Differential Diagnosis by Joint
| Joint | Common Conditions | Key Distinguishing Features |
|---|---|---|
| Shoulder | Frozen shoulder, impingement, dislocation | Pain pattern, ROM limitation, instability |
| Knee | ACL tear, meniscal tear, OA | Mechanism of injury, special tests, age |
| Hip | Septic arthritis, DDH, AVN | Age, fever, pain pattern, imaging |
| Spine | Disc herniation, spondylolisthesis | Radiation pattern, neurological signs |
Red Flags in Orthopedic Practice
| Red Flag | Significance | Immediate Action |
|---|---|---|
| Night pain | Possible tumor/malignancy | Urgent imaging |
| Fever + joint pain | Septic arthritis | Emergency aspiration |
| Neurological deficit | Nerve compression/spinal cord | Urgent surgical referral |
| Inability to bear weight | Significant pathology | Immediate imaging |