Internal Medicine
HYPOTHYROIDISM (underactive gland)
| Feature | Primary | Secondary |
|---|---|---|
| Location of Problem | Thyroid gland | TSH secretion from brain (very rare) |
| T3/T4 levels | Low | Low |
| TSH levels | High | Low (main problem) |
PRIMARY HYPOTHYROIDISM
ETIOLOGIES
- Hashimoto thyroiditis ( most common cause)
- Iodine deficiency
- Surgical gland removal
- Radio-iodine therapy for hyperthyroidism (gland destruction)
- Radiotherapy to the neck region
- Hypothyroidism induced Drugs (Interferon, amiodarone)
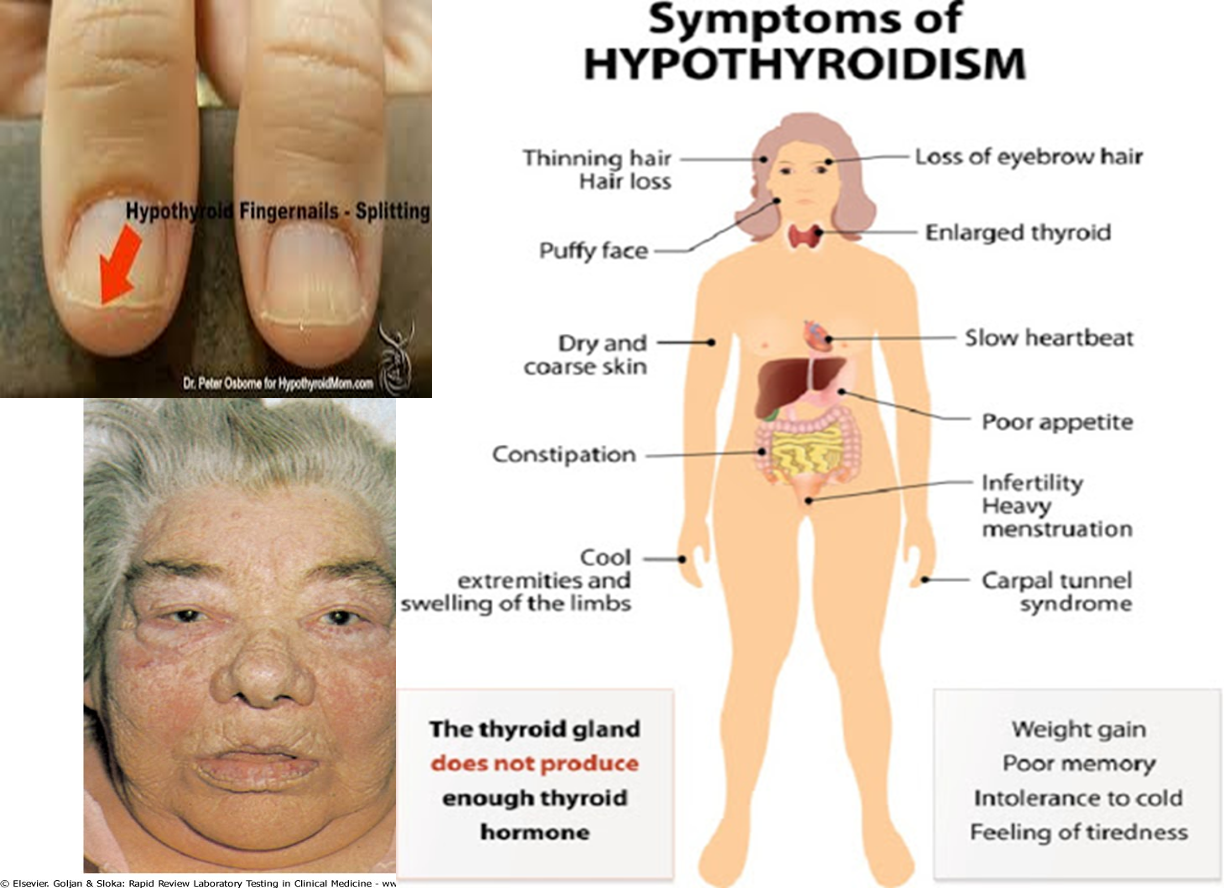
S/S of hypothyroidism
- Weight gain
- Tiredness/ fatigue
- Cold intolerance
- Constipation
- Dry skin, dry hair
- Hair fall
- Bradycardia
- Hyporeflexia
- Menstrual irregularities
- Infertility ( rule out hypothy. in any female with 9 or 10)
- Increased sleep
- Slowed actions
- Dementia, mental slowness, psychosis
- Puffy eyes
- Myalgias, arthralgias
- *Carpal tunnel syndrome *
WHAT IS MYXEDEMA
Hypothyroidism plus generalised edema due to deposition of subcutaneous mucopolysaccharides. Leads to thickening of facial features & generalised edema
All hypothyroid patients do not have myxedema

MYXEDEMA COMA
Patients with myxedema may go into coma ( due to infection, surgery, non compliance)
- Needs ICU
- Altered mental status, hypothermia,hypotension, hypoventilation, hypoglycemia, cardiac failure,hyponatremia
- In addition to TFTs, check cortisol levels also ( frequently low)
TREATMENT OF MYXED. COMA
- i.v. thyroxine
- i.v fluids (saline)
- Gradual rewarming the body(warming blankets)
- O2
- i.v. steroids & glucose
Investigations in hypothy.
1) TFTs:
- Low fT4 & fT3
- High TSH ( low in sec. hypo)
2) In Hashimoto’s thyroiditis: Serum anti TPO ab. very high
3) CBC: Usually macrocytic anemia, but may be microcytic
4) Hyponatremia
5) High CPK
6) High cholesterol & triglycerides
7) Radio I scan shows decreased uptake (but not done as a routine)
TREATMENT of HYPOTHYR.
- Levothyroxine tabs. (synthetic T4) is the main treatment
- Taken for ever
- Take in an empty stomach
- Start with a medium dose about 50 micrograms/d in young & otherwise healthy people. Increase as needed RR
- In elderly & in IHD, start 25 mcg (higher dose can cause arrhythmias)
- Levothyroxine is safe in preg. & should be continued RR
- Check TFTs 6 weeks after starting or any dose change (TSH takes some to normalise)
- Increase the dose gradually ( about 25mcg). Rapid hormone correction is dangerous (arrhythmias)
- Once TSH, T3 & T4 are normalised, maintain the dose. Later, routine TFTs once a year is enough
- Do not suppress the TSH to below normal - Improvement of S/S takes a few months
MED & SURGERY
- Primary:
- Hashimoto’s disease
- Post RAI for Grave’s disease
- Post thyroidectomy
- Sub-acute thyroiditis
- Iodine deficiency
- Goitrogens use- lithium, anti-thyroid drugs
- Inborn errors of thyroid hormone synthesis
- Secondary:
- Hypopituitarism
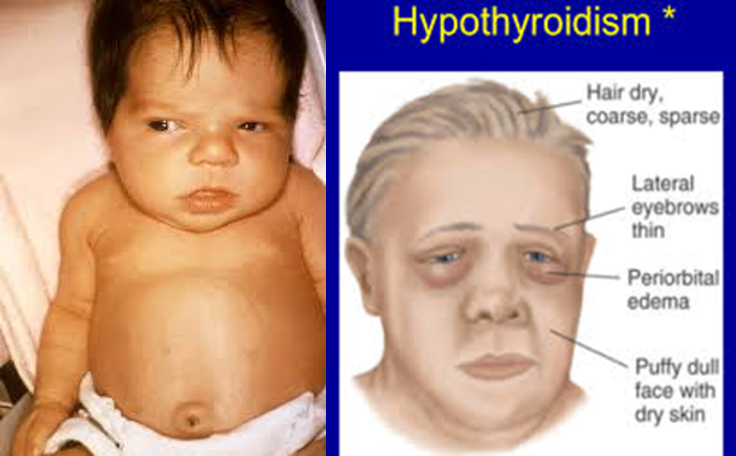
SIGNS OF HYPOTHYROIDISM
- Obese
- Dry inelastic skin
- Macroglossia
- Mask like facies
- Loss of hair in lateral eyebrow
- Hoarseness of voice
- Pseudomyotonic reflex (delayed ankle jerk); also called ‘hung up’ reflex
FM
Hypothyroidism is a condition in which the body lacks sufficient thyroid hormone.
- hypo = too little
thyroidism = disease of the thyroid
Thus, hypo-thyroidism = a disease of too little thyroid activity.
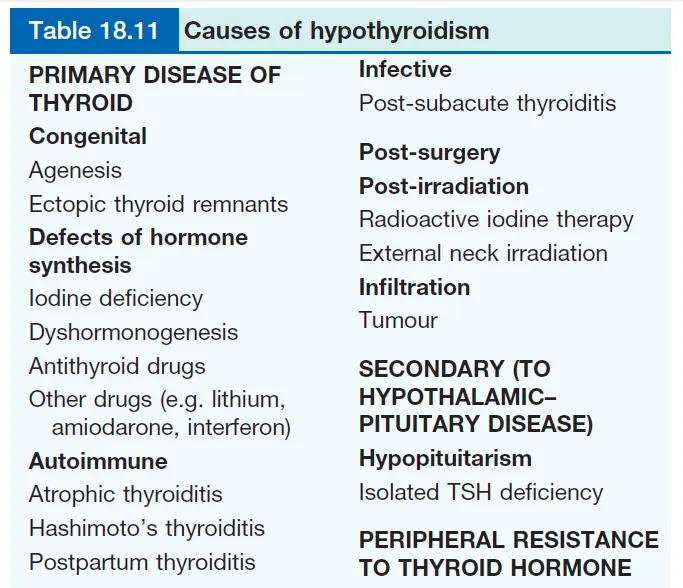
Table 18.11 Causes of Hypothyroidism
PRIMARY DISEASE OF THYROID
- Congenital
- Agensis
- Ectopic thyroid remnants
- Defects of hormone synthesis
- Iodine deficiency
- Dyshormonogenesis
- Antithyroid drugs
- Other drugs (e.g. lithium, amiodarone, interferon)
- Autoimmune
- Atrophic thyroiditis
- Hashimoto’s thyroiditis
- Postpartum thyroiditis
Infective
- Post-subacute thyroiditis
Post-surgery
Post-irradiation
- Radioactive iodine therapy
- External neck irradiation
Infiltration
- Tumour
SECONDARY (TO HYPOTHALAMIC–PITUITARY DISEASE)
- Hypopituitarism
- Isolated TSH deficiency
PERIPHERAL RESISTANCE TO THYROID HORMONE
Causes of Primary Hypothyroidism
Autoimmune:
Atrophic (autoimmune) hypothyroidism. This is the most common cause of hypothyroidism and is associated with antithyroid autoantibodies leading to lymphoid infiltration of the gland and eventual atrophy and fibrosis.
Hashimoto’s thyroiditis: This form of autoimmune thyroiditis produces atrophic changes with regeneration, leading to goitre formation.
TPO antibodies are present, often in very high titers (> 1000 IU/L). Patients may be hypothyroid or euthyroid.
Defects of Hormone Synthesis:
- Iodine deficiency (Dyshormonogenesis)
- Genetic defects in the synthesis of thyroid hormones
Hypothyroidism complications:
Myxedema Coma: A severe type of Hypothyroidism
- Is a rare but extremely severe manifestation of hypothyroidism.
- Mental status changes including lethargy, cognitive dysfunction, psychosis, and hypothermia are the hallmark features of myxedema coma.
- Hyponatremia, hypoventilation, and bradycardia can also occur.
- Endocrinology referral is recommended for all patients with suspected myxedema coma.
Sub-Clinical Hypothyroidism:
- Also known as mild thyroid failure.
- Diagnosed when peripheral thyroid hormone (T4) levels are within normal, but serum thyroid-stimulating hormone (TSH) levels are mildly elevated (usually 5-10 mU/L).
- Some patients may have some hypothyroid symptoms.
- Treatment is a dilemma.
- Patients should be treated with small doses of Levothyroxine if symptomatic.
Sub-Clinical - Treatment Treatment should be considered for patients with:
- Initial TSH levels greater than 10 mIU per L Z
- Patients with elevated thyroid peroxidase
- antibody titers,
- Patients with symptoms suggestive of
- hypothyroidism and
- TSH levels between 5 and 10 mIU per L, for
- patients who are pregnant or are attempting to conceive.
indication treatment with levothyroxine;
- symptomatic
- tsh >10
- pregnancy
- +ve TPO
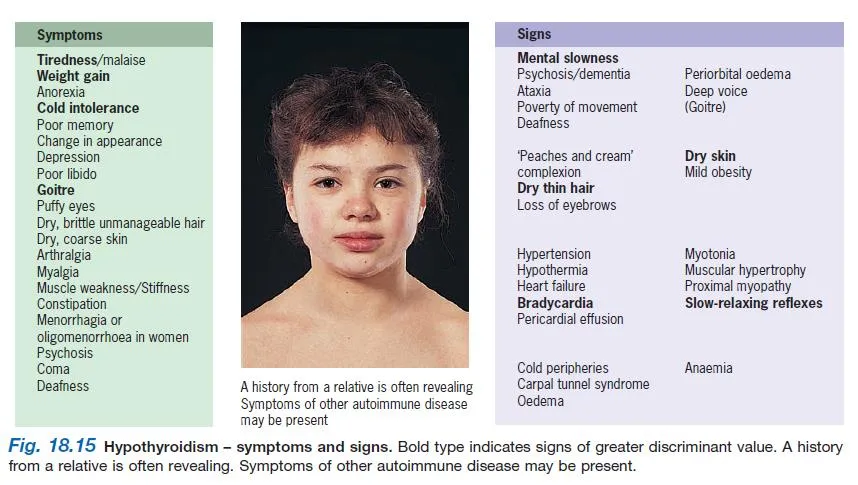
Fig. 18.15 Hypothyroidism – Symptoms and Signs Y
Bold type indicates signs of greater discriminant value. A history from a relative is often revealing. Symptoms of other autoimmune disease may be present.
Symptoms
- Tiredness/malaise
- Weight gain
- Anorexia
- Cold intolerance
- Poor memory
- Change in appearance
- Depression
- Poor libido
- Goitre
- Puffy eyes
- Dry, brittle unmanageable hair
- Dry, coarse skin
- Arthralgia
- Myalgia
- Muscle weakness/Stiffness
- Constipation
- Menorrhagia or oligomenorrhoea in women
- Psychosis
- Coma
- Deafness
Signs
- Mental slowness
- Psychosis/dementia
- Ataxia
- Poverty of movement
- Deafness
- ‘Peaches and cream’ complexion
- Dry thin hair
- Loss of eyebrows
- Dry skin
- Mild obesity
- Hypertension
- Hypothermia
- Heart failure
- Bradycardia
- Pericardial effusion
- Myotonia
- Muscular hypertrophy
- Proximal myopathy
- Slow-relaxing reflexes
- Cold peripheries
- Carpal tunnel syndrome
- Oedema
- Anaemia
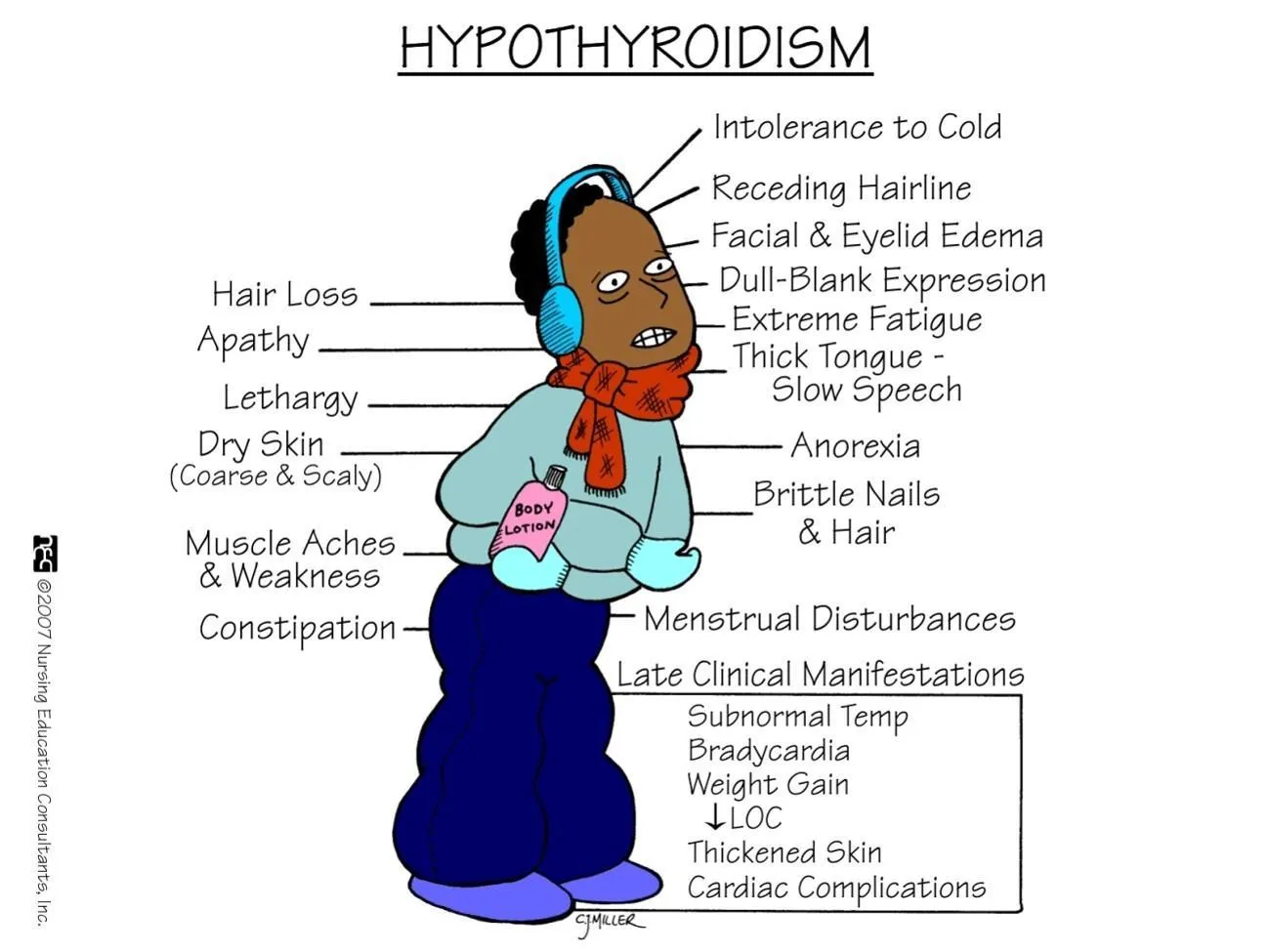
Late Clinical Manifestations Y
- Subnormal Temp
- Bradycardia
- Weight Gain
- LOC
- Thickened Skin
- Cardiac Complications
- Hair Loss
- Apathy
- Lethargy
- Dry Skin (Coarse & Scaly)
- Muscle Aches & Weakness
- Constipation
Diagnosis of Primary Hypothyroidism
The symptoms of hypothyroidism are very common.
- Thyroid Function Test (TFT) +
- Careful clinical assessment.
- The symptoms and/or signs alone are insufficient to make a diagnosis of hypothyroidism.
Investigations of Primary Hypothyroidism
- Serum TSH is the investigation of choice; a high TSH level
- A low free T4 level
- Antibody testing
Treatment
- Replacement therapy with levothyroxine (thyroxine, i.e. T4), taken daily, for life. adjusted to Body weight & Age

Untreated Hypothyroidism
Can contribute to:
- Hypertension
- Dyslipidemia
- Infertility
- Cognitive impairment
- Neuromuscular dysfunction.
Screening
May be considered in those with risk factors for hypothyroidism, such as: screen patients with Vitiligo
- History of autoimmune disease,
- History of head or neck irradiation,
- Previous radioactive iodine therapy,
- Presence of a goiter,
- Family history of thyroid disease,
- Treatment with drugs known to influence thyroid function.
Special Populations
Six populations deserve special consideration:
- Older patients;
- Known or suspected ischemic heart disease;
- Pregnant women;
- Patients with persistent symptoms of hypothyroidism despite taking adequate doses of levothyroxine;
- Patients with subclinical hypothyroidism;
- Patients suspected of having myxedema coma
OLDER PATIENTS & PATIENTS WITH IHD
- The initial dosage is generally 25 mcg or 50 mcg daily, with the dosage increased by 25 mcg every three to four weeks.
- Thyroid hormone increases heart rate and contractility, and therefore increases myocardial oxygen demand; arrhythmias
- Consequently, starting at higher doses may precipitate acute coronary syndrome or an arrhythmia.
Pregnancy Z
-
Thyroid hormone requirements increase during pregnancy.
-
A median increase of 47 percent in their thyroid hormone requirements.
-
It is recommended that women on fixed doses of levothyroxine take nine doses each week (one extra dose on two days of the week).
Patients with Persistent Symptoms
- Numerous medications can affect thyroid hormone levels in patients taking levothyroxine.
- Amiodarone
- Interleukin-2
- Interferon alfa
- Lithium
- Sulfonylurea
- Thalidomide
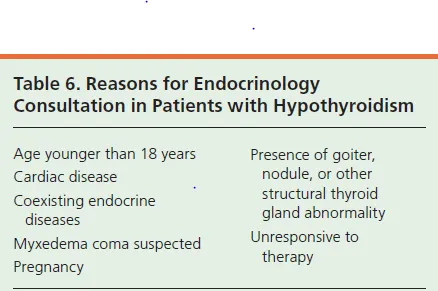
Table 6. Reasons for Endocrinology Consultation in Patients with Hypothyroidism Y
- Age younger than 18 years
- Cardiac disease
- Coexisting endocrine diseases
- Myxedema coma suspected
- Pregnancy
- Presence of goiter, nodule, or other structural thyroid gland abnormality
- Unresponsive to therapy
Complications of Hypothyroidism
What May Happen If the Disorder Is Untreated:
- Birth Defects
- Goiter
- Heart Problems
- Infertility
- Mental Health Issues
- Myxedema coma.
- HTN
- DLD
Thera
Defined as low free T4 level with a normal or high TSH.
Causes of hypothyroidism:
A- Primary: Thyroid gland dysfunction Most common:
- Congenital hypothyroidism (in neonates) = Cretinism
- Chronic lymphocytic thyroiditis (Hashimoto`s thyroiditis) Autoimmune disease of thyroid. Thyroid gland is enlarged
- Iodine deficiency +++
- Thyroid surgery (total thyroidectomy)
- Radioactive iodine treatment
B- Secondary: Pituitary hypofunction
(hypopitutarism due to radiation therapy or destruction of the pituitary)
Laboratory Investigation:
- Low plasma free T4…..
- Plasma TSH is normal or high in 1ry hypothyroidism &
- low in 2ry hypothyroidism
- Neonatal screening for congenital hypothyroidism = Cretinism (plasma TSH is elevated in affected neonates)
clinical manifestations of hypothyroidism:
Symptoms:
- Cold intolerance
- Depression
- Mental retardation (infants)
- Growth failure (children)
- Dry skin
- Constipation
- Dyspnea on exertion
Signs:
- Bradycardia
- Periorbital edema
- Slowed movement & speech
- Delayed relaxation phase of deep tendon reflex tendons
- Lab: Hypercholesterolemia