Objectives
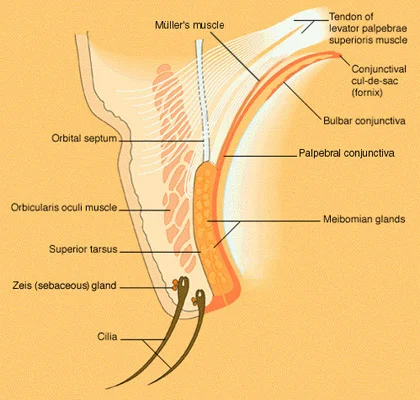
- Recognize the main anatomical landmarks of the eyelid and its cranial nerves’ supply.
- Identify eyelid and eyelash malposition and disorders.
- Distinguish between different causes of eyelid inflammation and infection.
- Recognize the most common lid tumors.
Anatomical Structure of the Eyelid
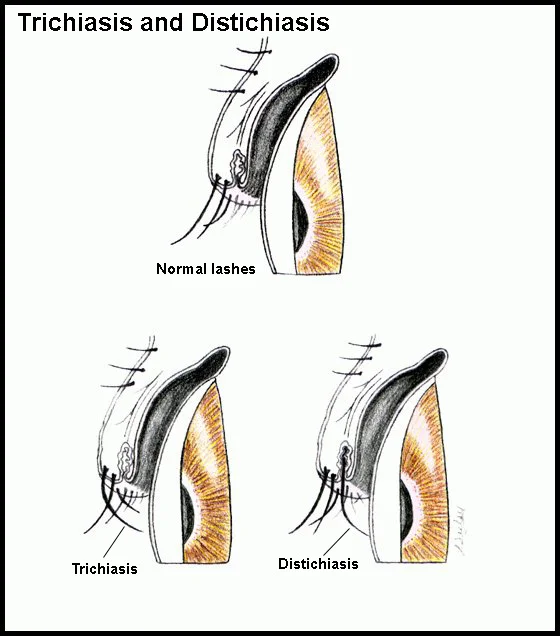
Lash Disorders
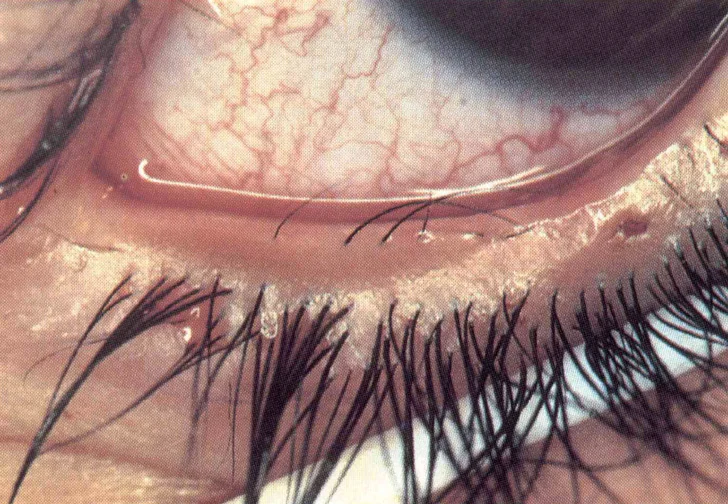
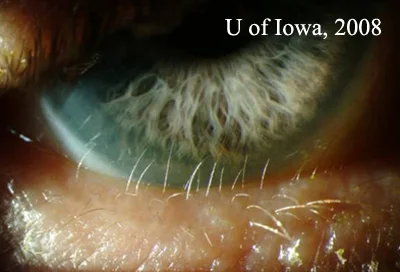
- Trichiasis: primary or secondary (entropion).
- Madarosis: local or systemic.
- Poliosis: Local (blepharitis) or systemic (VKH).
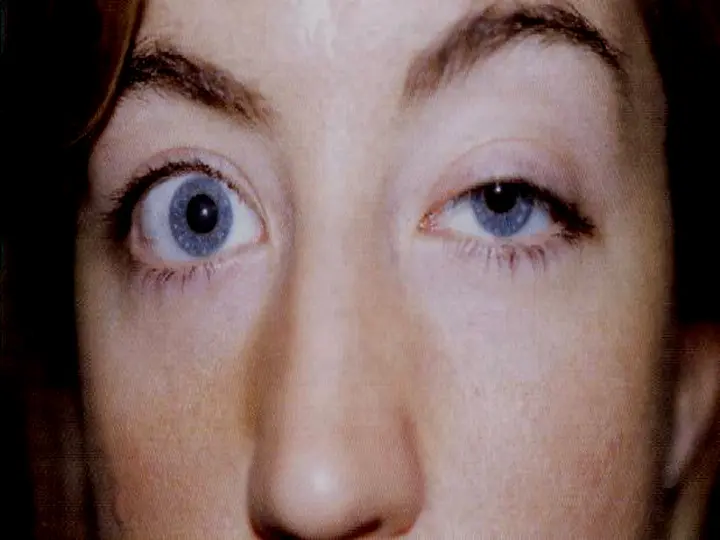
- Lid retraction: Thyroid eye disease.



Allergic Disorders
-
Acute allergic edema: insect bite or other allergens. Unilateral or bilateral painless pitting edema.
-
Contact dermatitis: Type 4 hypersensitivity reaction.
Topical medications, cosmetics.


Xanthelasma
- Elderly people or young’s with hyperlipidemia.
- Cholesterol and lipid form subcutaneous plaques.

Infections of the Eyelid
-
Blepharitis
-
Hordeolum:
- Externum (Stye)
- Internum
-
Trachoma
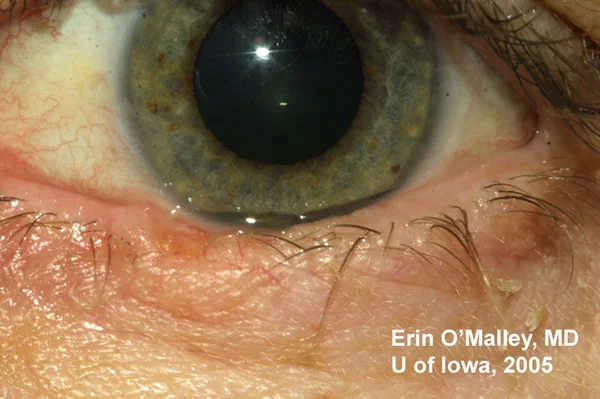
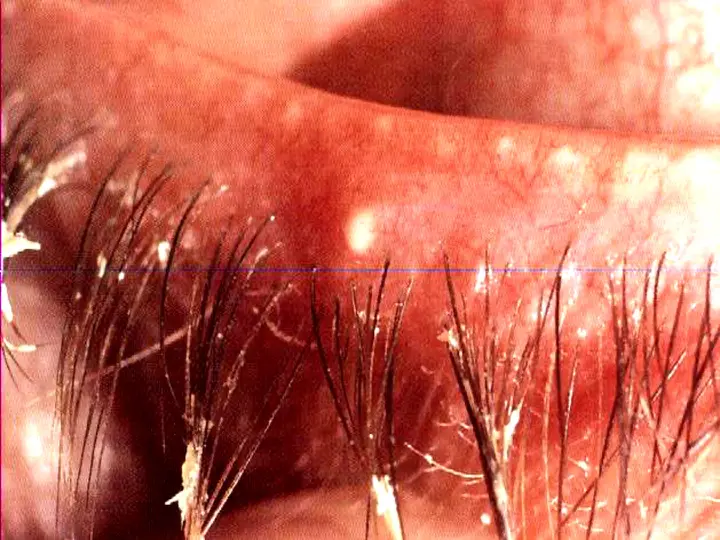
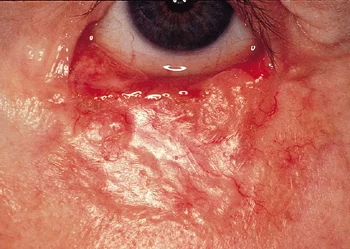
Blepharitis
-
Anterior, posterior, or mixed.
- Symptoms: burning, grittiness, mild photophobia, crusting, and redness of lid margin.
- Signs: lid margin (hyperemia, telangiectasia and tiny abscesses) scales and lashes (greasy and stuck together).
-
Complications: Stye, tear film instability, hypersensitivity to staph. toxins, trichiasis, madarosis, and poliosis.
-
Treatment:
- Lid hygiene.
- Lubricants.
- Antibiotic ointment.
- Weak topical steroid.
- Systemic tetracycline.
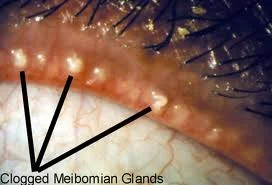
Clogged Meibomian Glands
- Clogged Meibomian Glands




External Hordeolum (Stye)
- Acute staph. infection of hair follicles and associated glands.
- Signs and symptoms
- Mild pre-septal cellulitis.
- Treatment: Hot compresses, epilation, topical antibiotics.
- Also control any blepharitis.

- Also control any blepharitis.
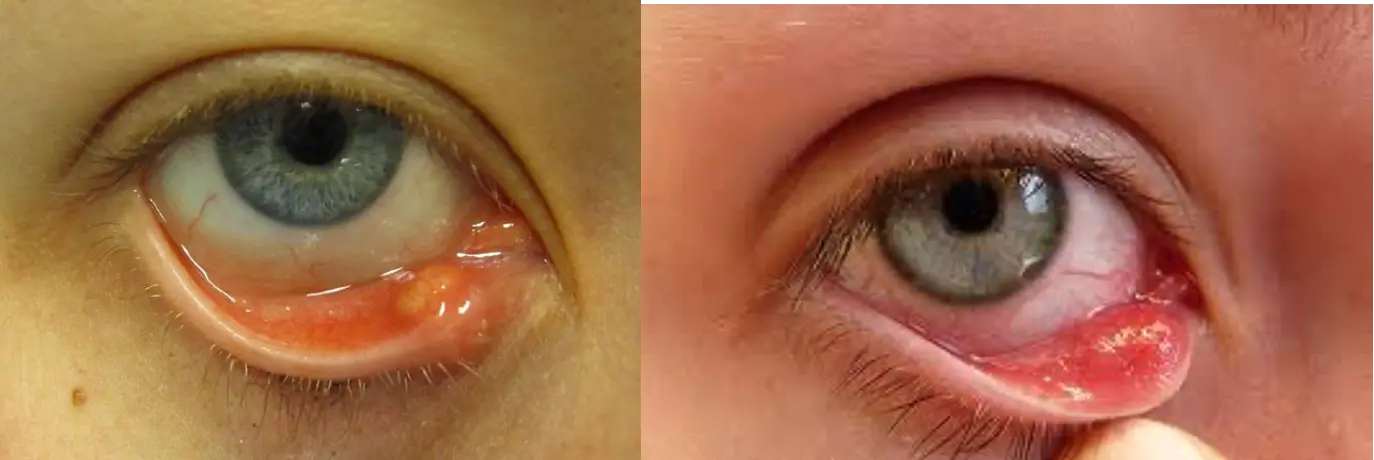
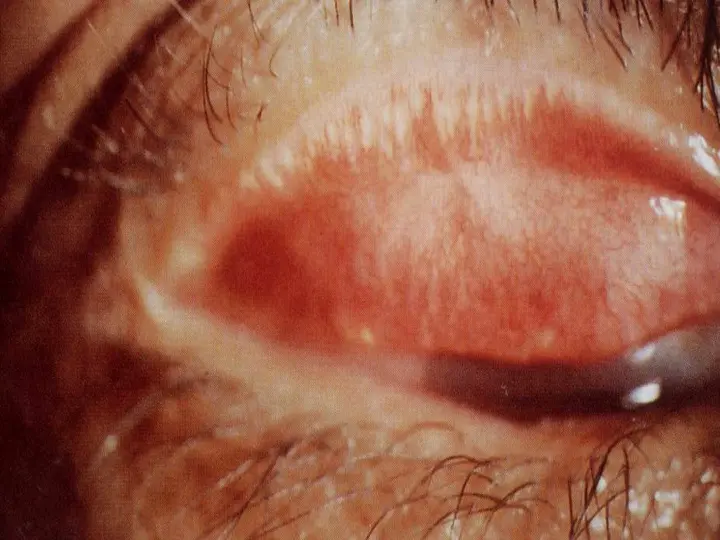
Internal Hordeolum
- Acute staph. infection of meibomian gland.
- Signs: tender inflamed swelling within the tarsal plate. It may discharge anteriorly through the skin or posteriorly through the conjunctiva.
- Treatment: Control of infection with hot compresses and topical abs.
Chalazion
(Meibomian cyst)
- Chronic lipogranulomatous inflammation caused by obstruction of the gland orifice.
- Most common lid mass.
- Symptoms
- Signs
- Treatment: control posterior blepharitis
- Hot compresses for 4 weeks
- Surgery (incision and curettage)
- Steroid injection

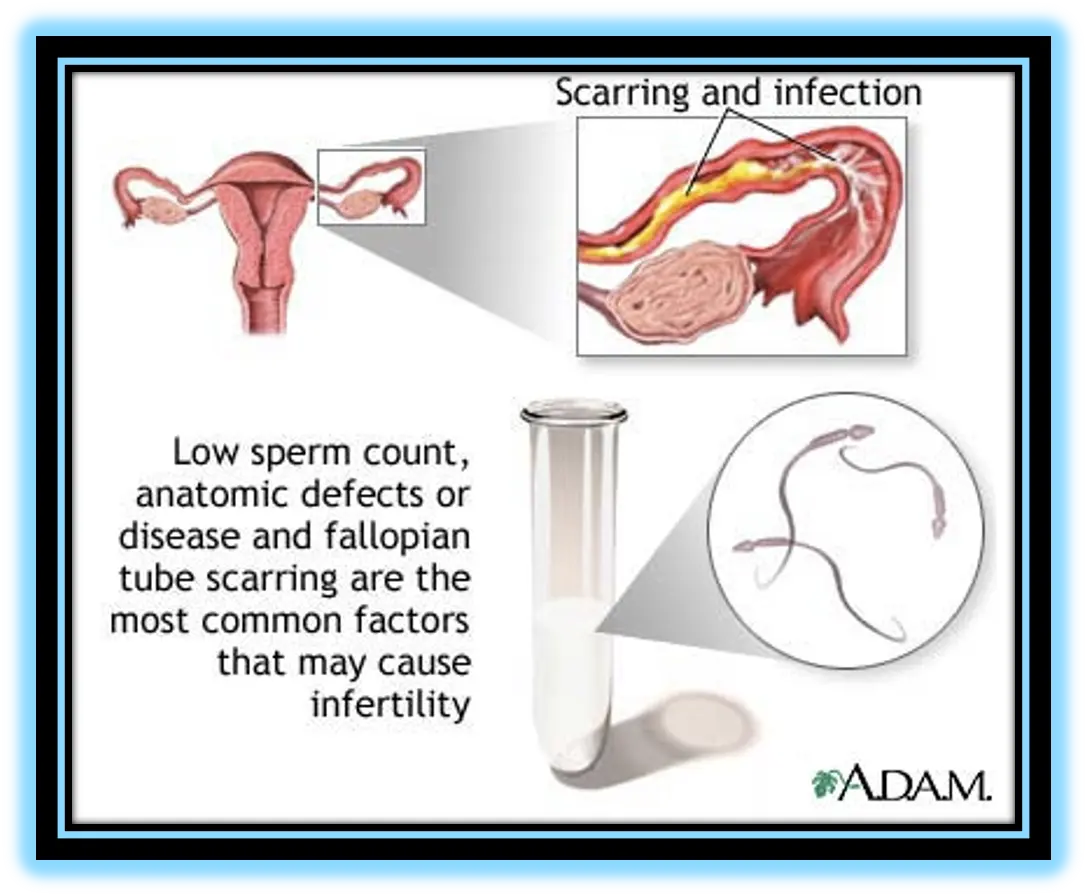
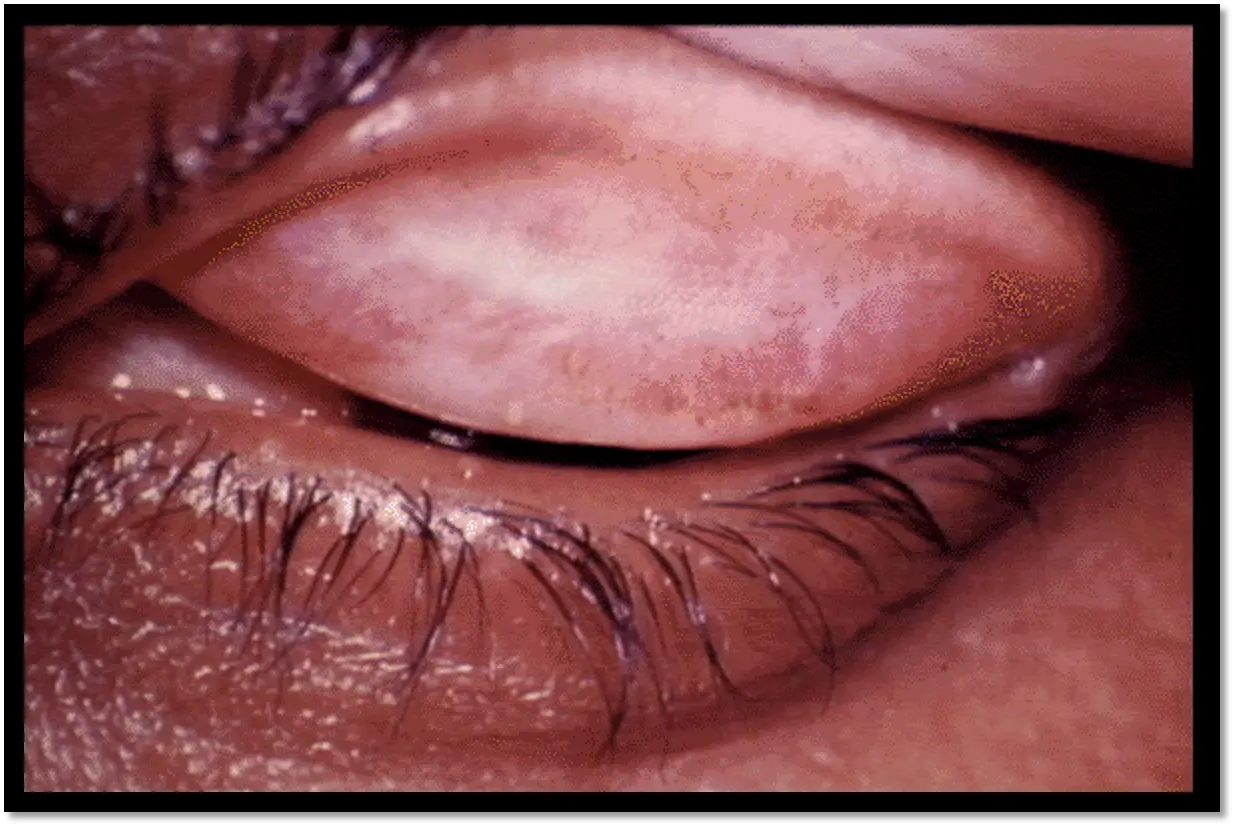
Chlamydial Conjunctivitis
- Adult Inclusion Conjunctivitis:
- Sexually transmitted disease (50% associated with genital infection) caused by serotypes D to K.
- Subacute onset, unilateral or bilateral mucopurulent discharge.
- Follicular conj. Reaction
- Non-tender lymphadenopathy.
- Treatment: Topical tetracycline plus systemic tetracycline, doxycycline, or recently azithromycin.
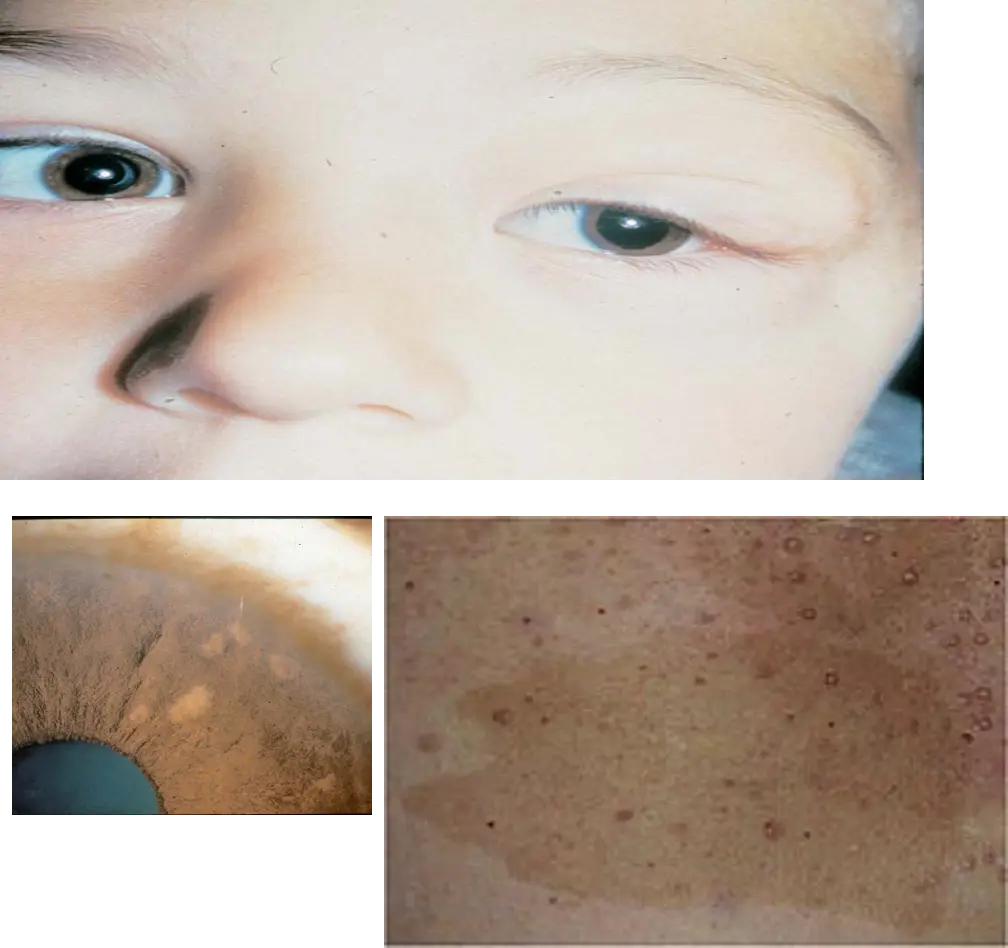
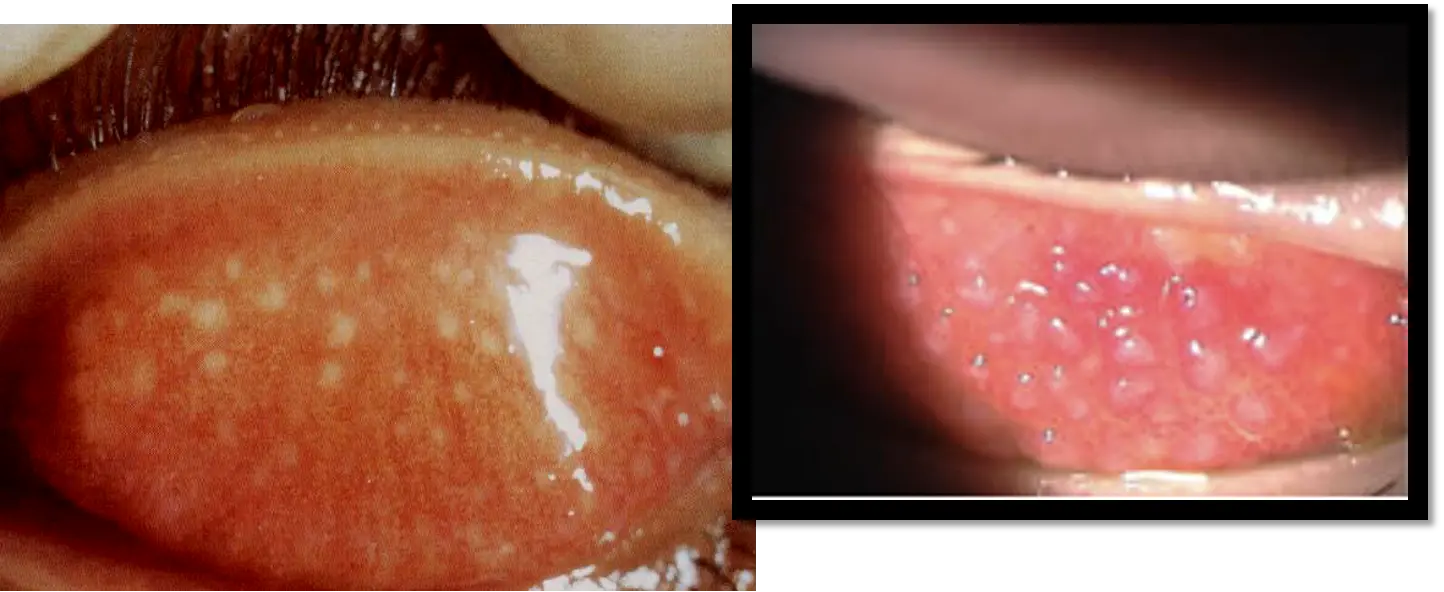
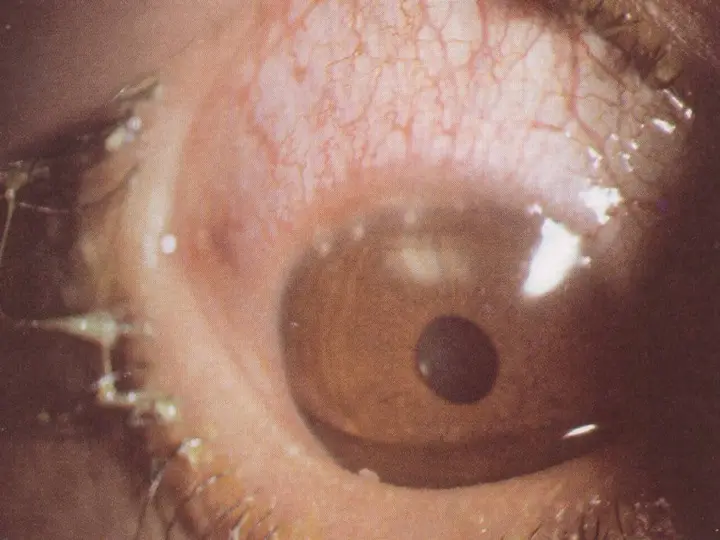
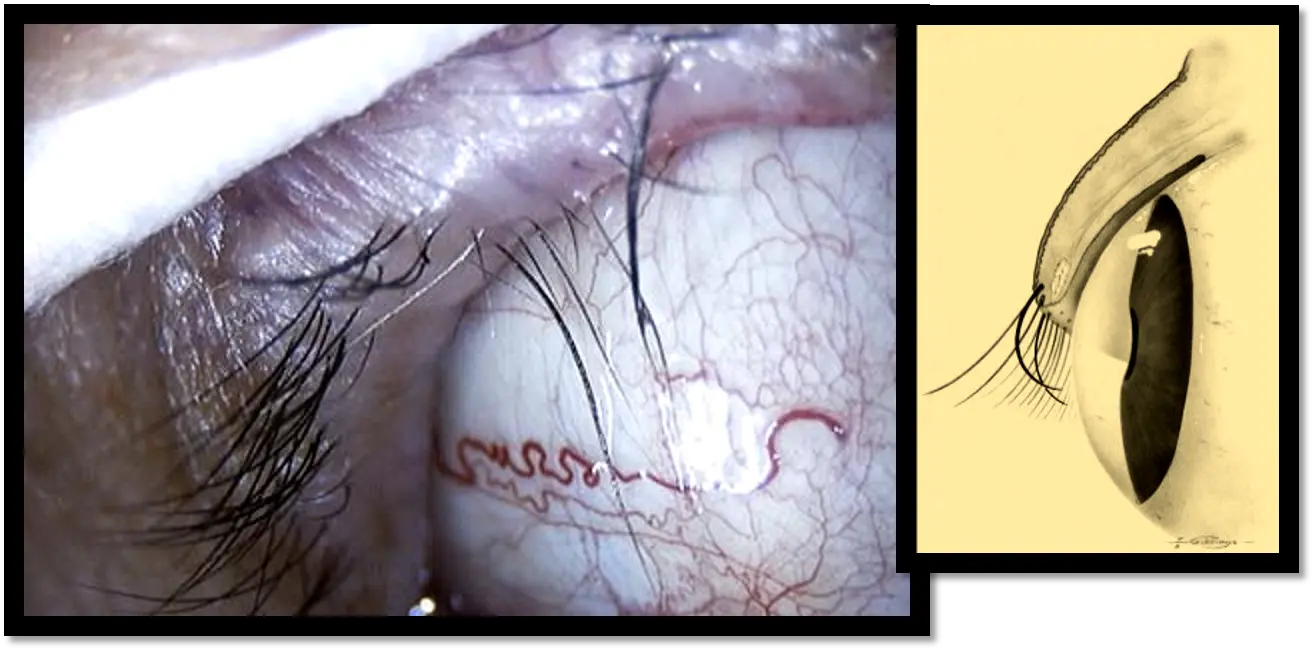
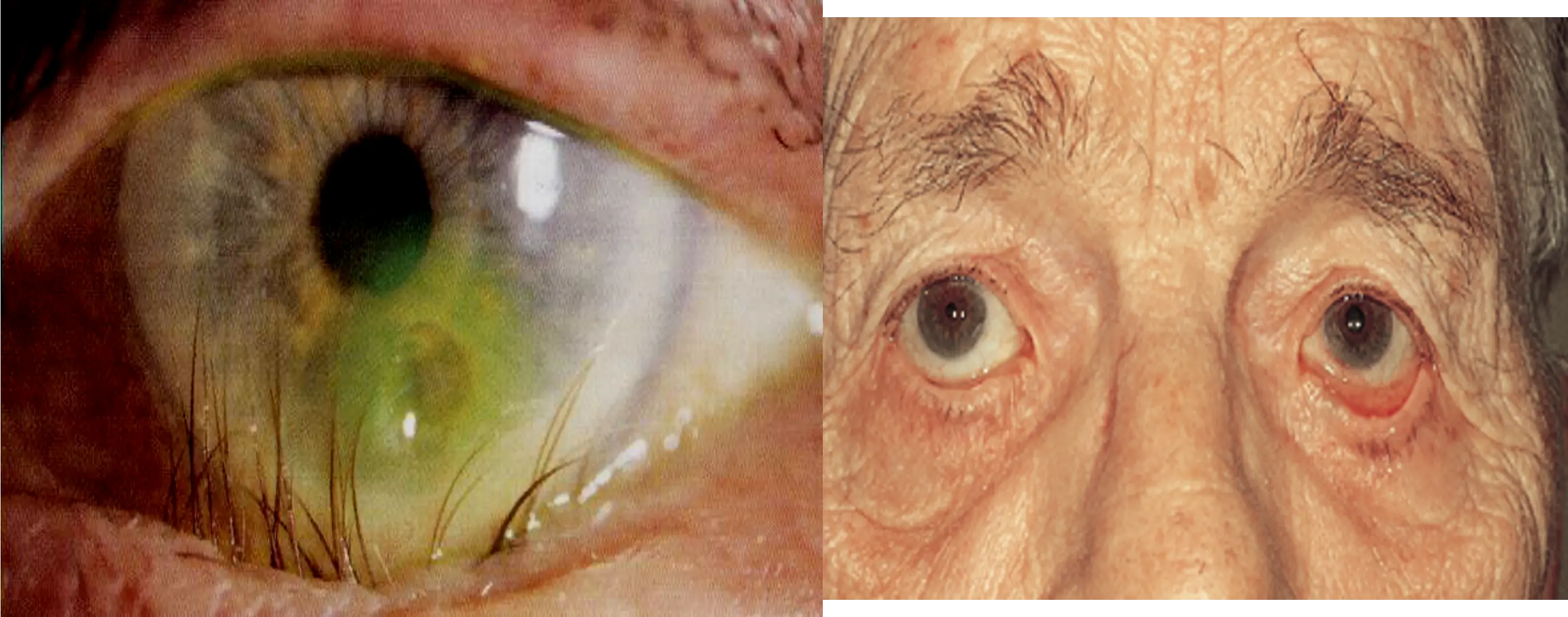
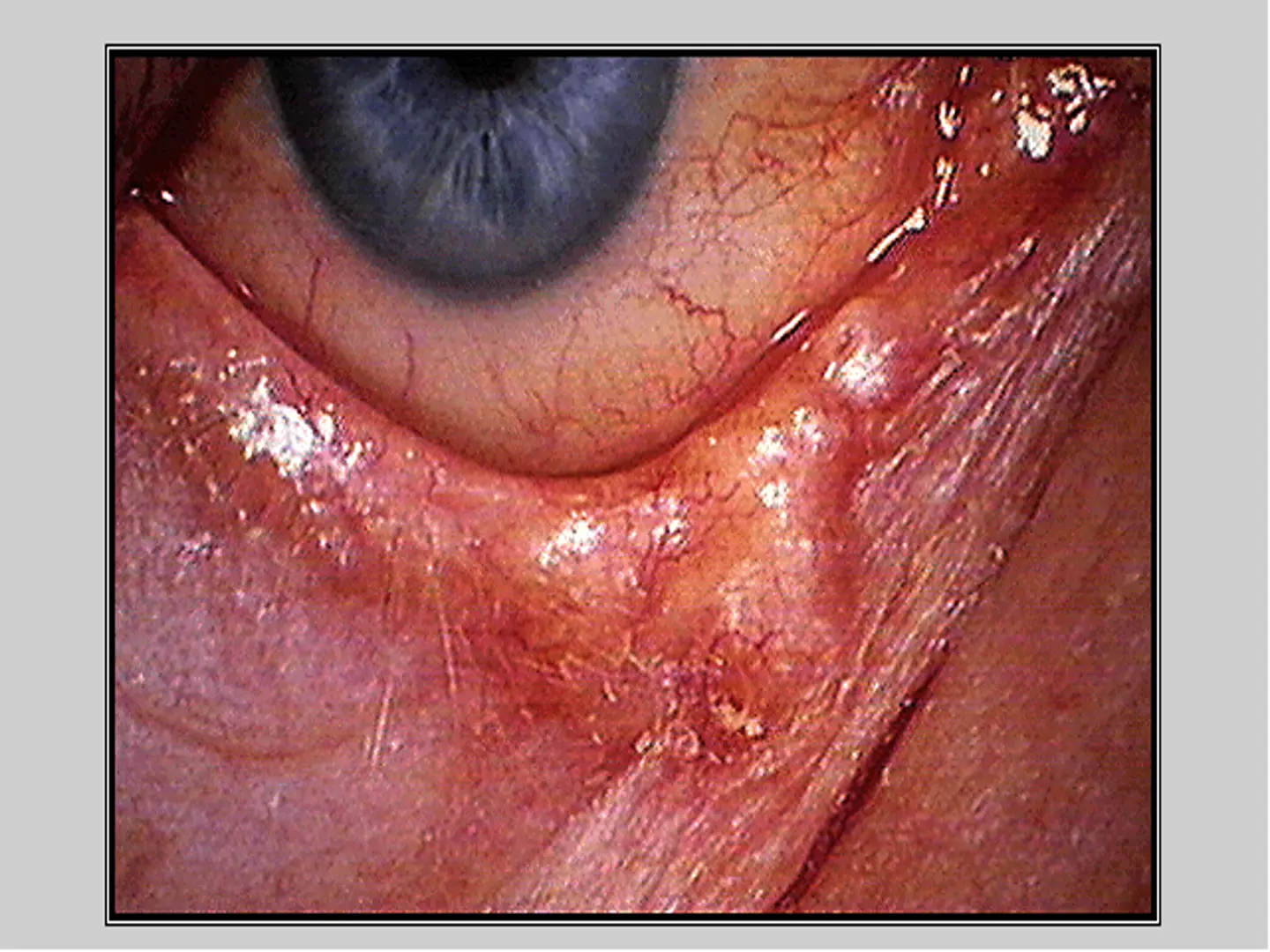
Trachoma
-
Infection caused by Chlamydia trachomatis (serotypes A, B, Ba & C).
-
Obligate intracellular bacteria.
-
The common fly is a major vector in the transmission of the disease.
-
It is the leading cause of preventable blindness all over the world.
-
Symptoms: During childhood with redness, and mucopurulent discharge.
-
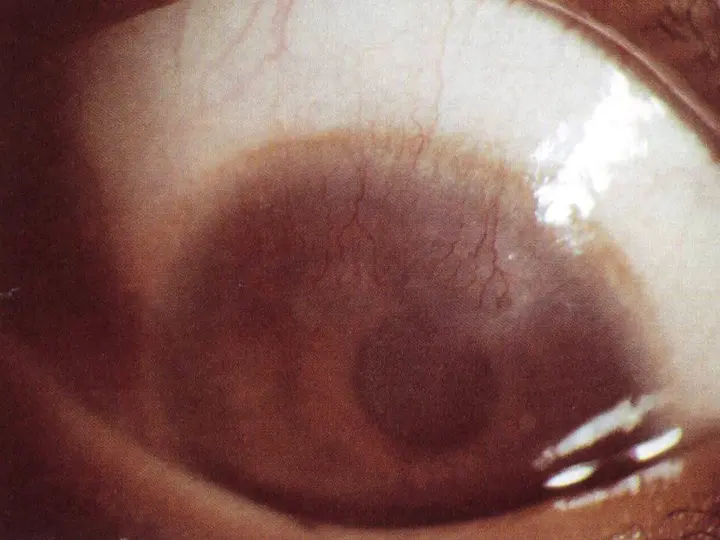
Signs: of active Trachoma
- follicular conjunctivitis.
- Limbal follicles.
- Keratitis.
-
Complications:
- Progressive conjunctival scaring (Arlt’s line, and entropion).
- Herbert pits.
- Corneal pannus.
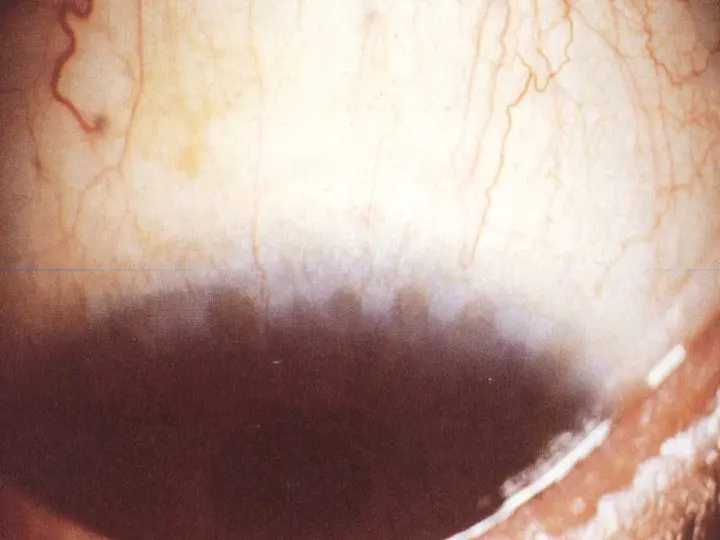
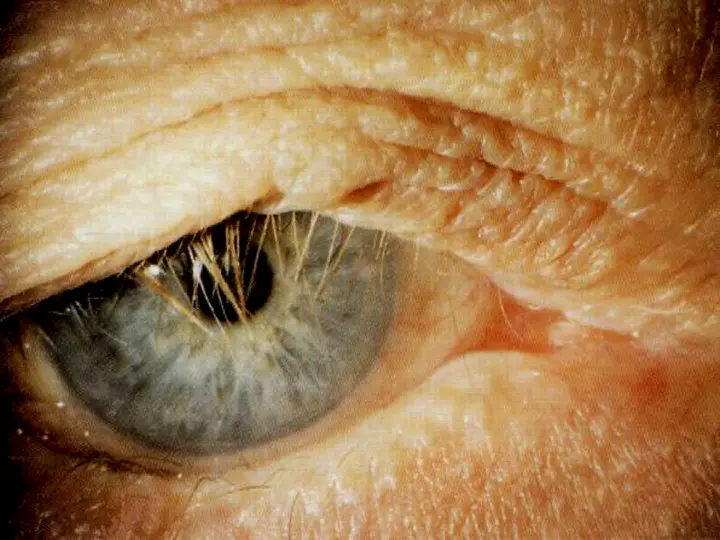
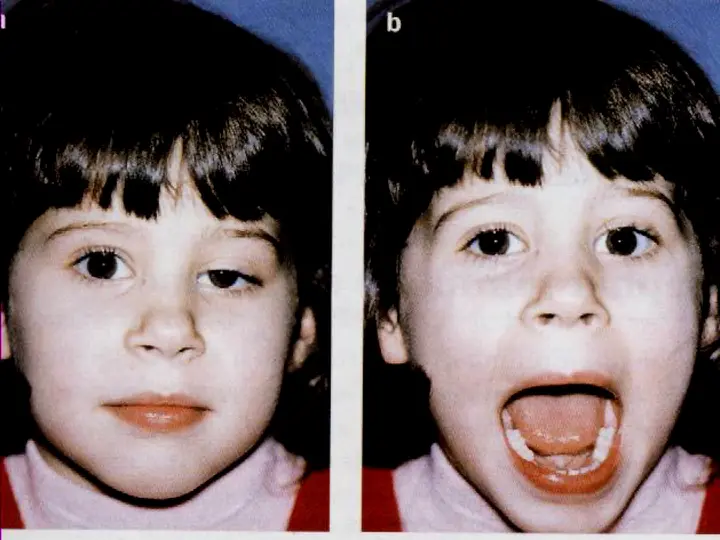
Entropion
- Inversion of the lid margin
- Types:
- Congenital
- Acute-spastic
- Involutional
- Cicatricial
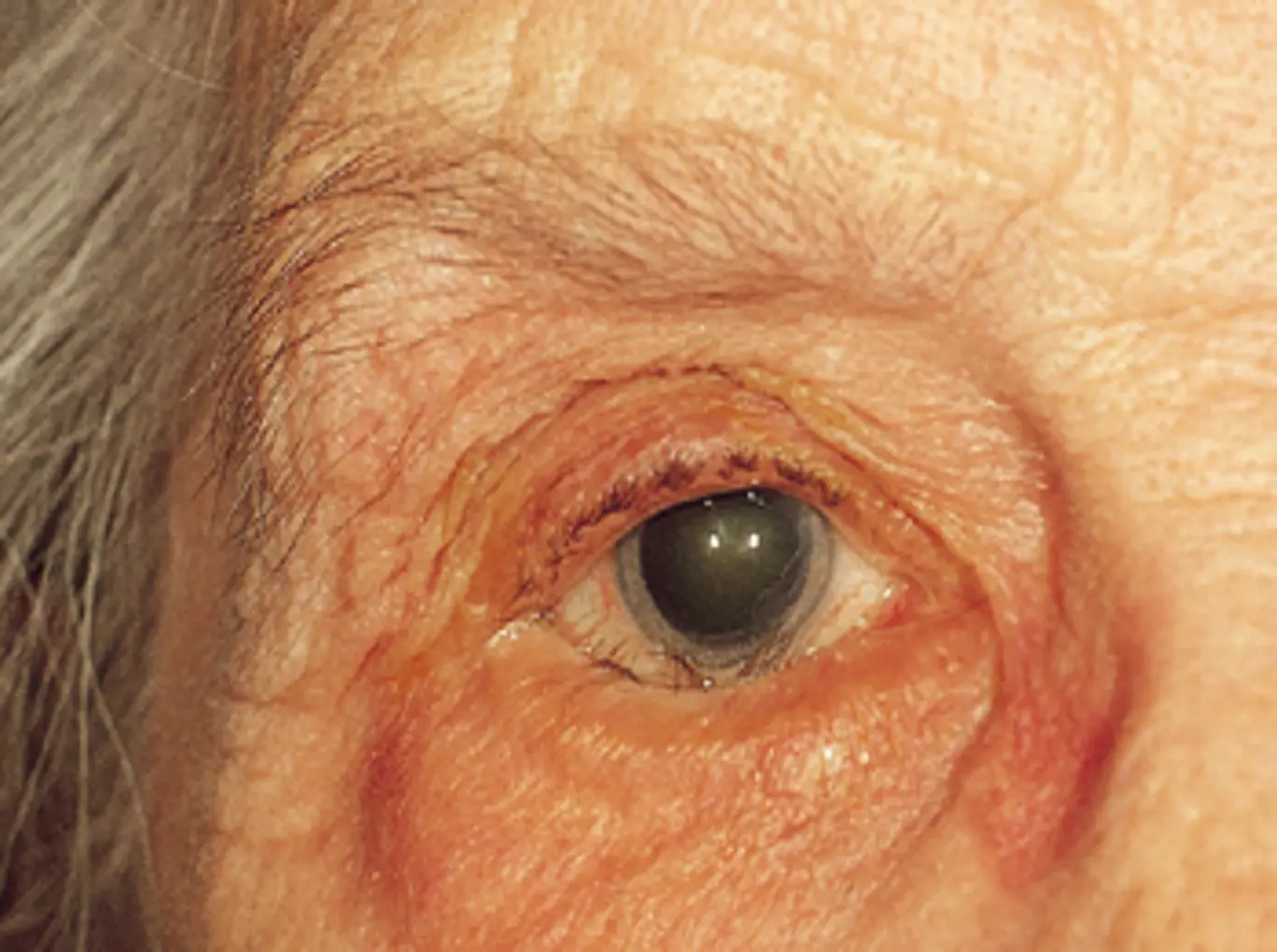
Ectropion
- Eversion (Outward turning) of lid margin
- Types:
- Congenital
- Involutional
- Paralytic
- Cicatricial
- Mechanical



Lid Tumors
- Benign:
- Naevus, Capillary haemangioma, Port-wine stain …etc
- Malignant:
- BCC, SCC, SGC, and Melanoma.

- BCC, SCC, SGC, and Melanoma.
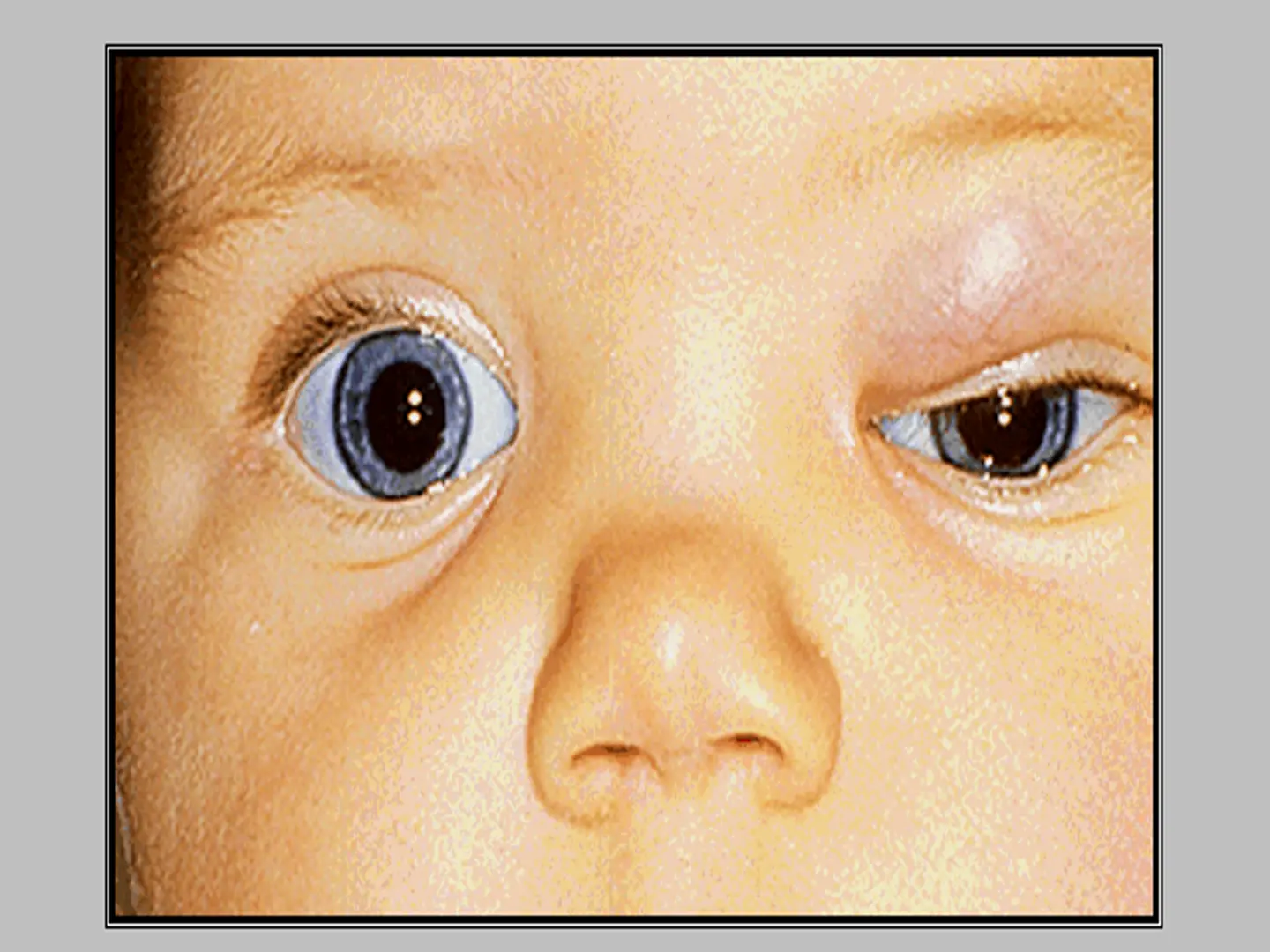
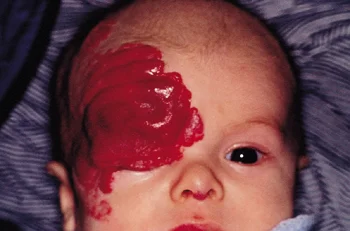
Port-wine Stain Hemangioma = Naevus Flammeus = Cavernous Hemangioma


Basal Cell
- 90-95% of malignant eyelid tumors
- Lower lid and medial canthal areas
- Medial canthal lesions can be problematic
- Mortality is less than 1%

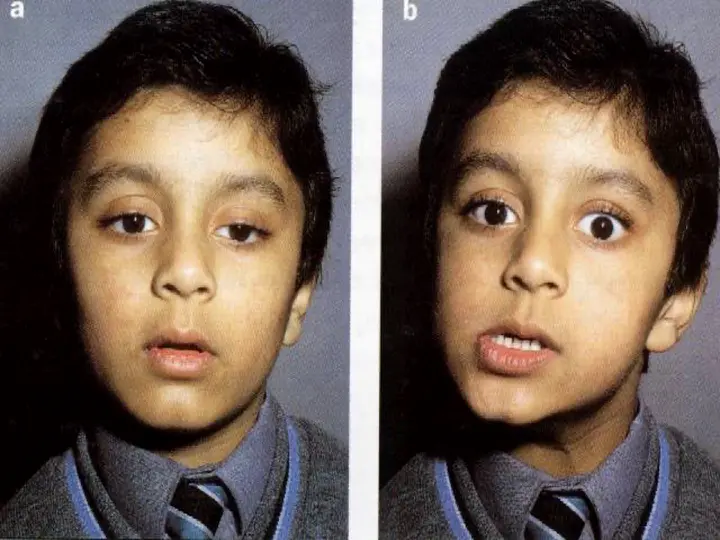
Ptosis
- Drooping of the upper lid.
- Pseudoptosis
- Classification:
- Congenital.
- Acquired:
- Neurogenic
- Myogenic
- Aponeurotic
- Mechanical
Clinical Evaluation
- History:
- Age of onset, Trauma, Previous surgery, and Diurnal variations.
- Exclusion of Pseudoptosis.
- Associated signs.
- EOM movements, pupil status, fatigability, and jaw-winking.
Management
- Risk of amblyopia in severe unilateral congenital ptosis.