IM
Stroke, or cerebrovascular accident (CVA), is a clinical term that describes a sudden loss of neurologic function persisting for more than 24 hours that is caused by an interruption of the blood supply to the brain.
- Stroke is the third leading cause of death worldwide, with considerable disability among survivors.
- Someone in the USA has a stroke every 40 seconds.
- Every 4 minutes, someone dies of stroke
- Stroke is a leading cause of serious long-term disability.
- Stroke reduces mobility in more than half of stroke survivors age 65 and over.
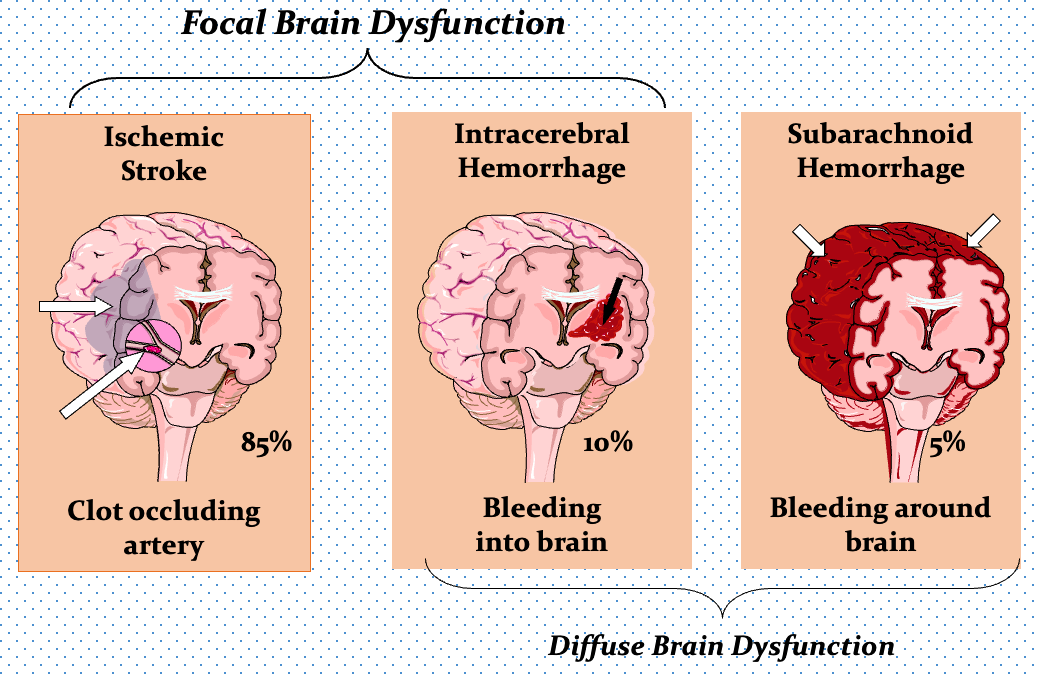
THREE STROKE TYPES
| Ischemic Stroke (85%) | Intracerebral Hemorrhage (10%) | Subarachnoid Hemorrhage (5%) |
|---|---|---|
| Clot occluding artery | Bleeding into brain | Bleeding around brain |
| Focal Brain Dysfunction | Diffuse Brain Dysfunction | Diffuse Brain Dysfunction |
| Thrombosis Embolism Hypoperfusion | Intracerebral Subarachnoid | Intracerebral Subarachnoid |
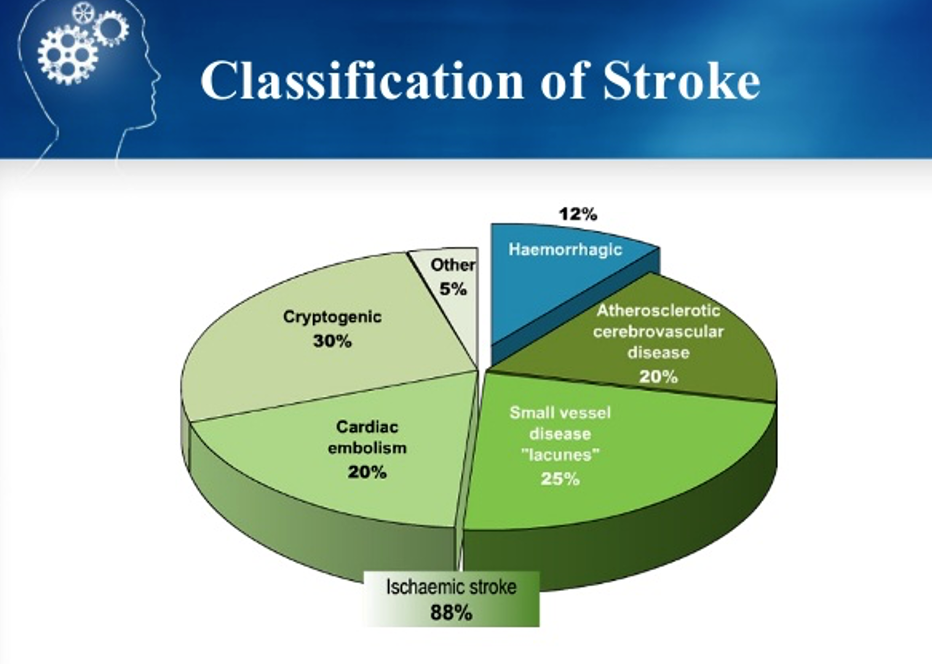
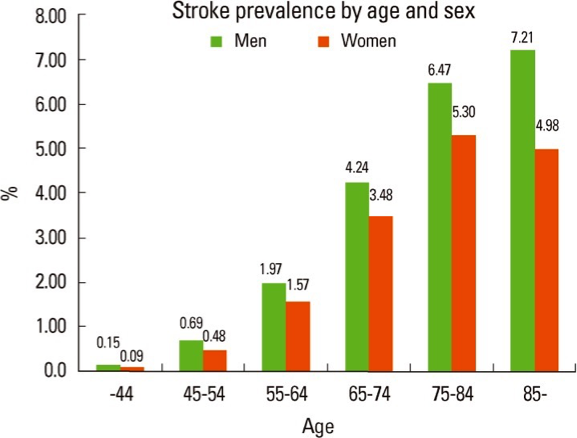
Stoke: Prevalence
Pathogenesis of Ischemic stroke
ISCHEMIC STROKE PATHOPHYSIOLOGY The First Few Hours
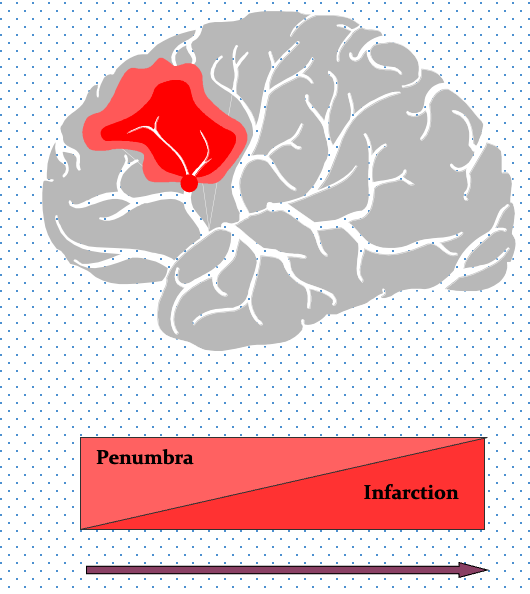
““TIME IS BRAIN: “SAVE THE PENUMBRA” Penumbra is zone of reversible ischemia around core of irreversible infarction—salvageable in first few hours after ischemic stroke onset
Penumbra damaged by:
- Hypoperfusion - fluids
- Hypoglycemia - give glucose
- Fever
- Seizure
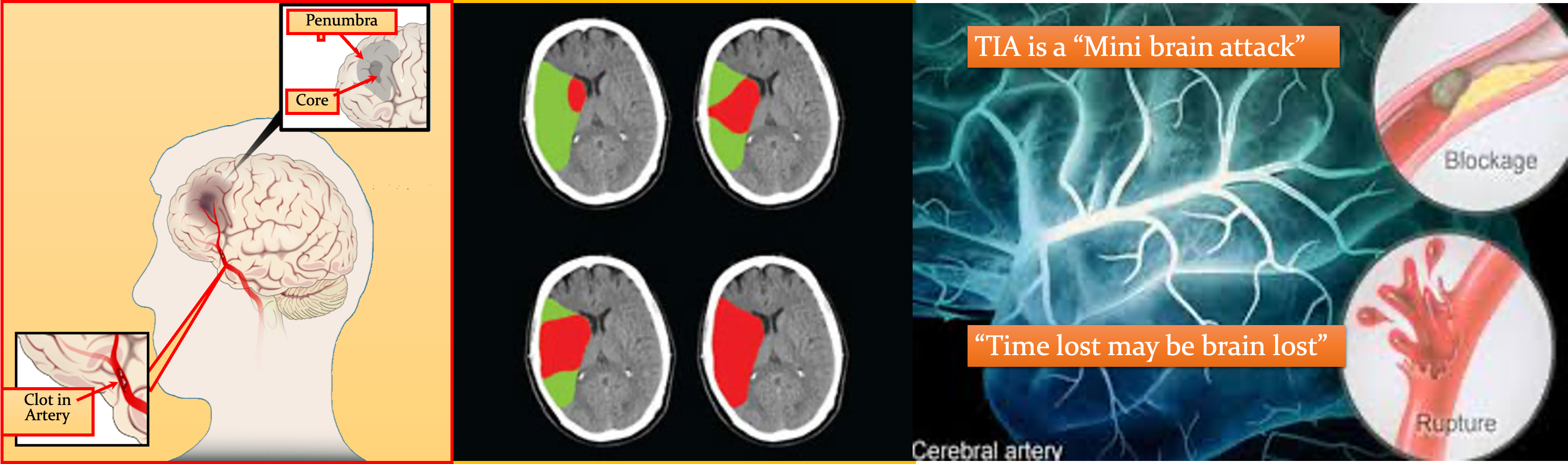
ISCHEMIC PENUMBRA
Immediately after an ischemic stroke (top left), a core of irreversibly damaged brain tissue (red) is surrounded by an area of viable but at-risk tissue called the penumbra (green). Unless blood flow is restored quickly, the tissue within the penumbra will be lost (bottom right).
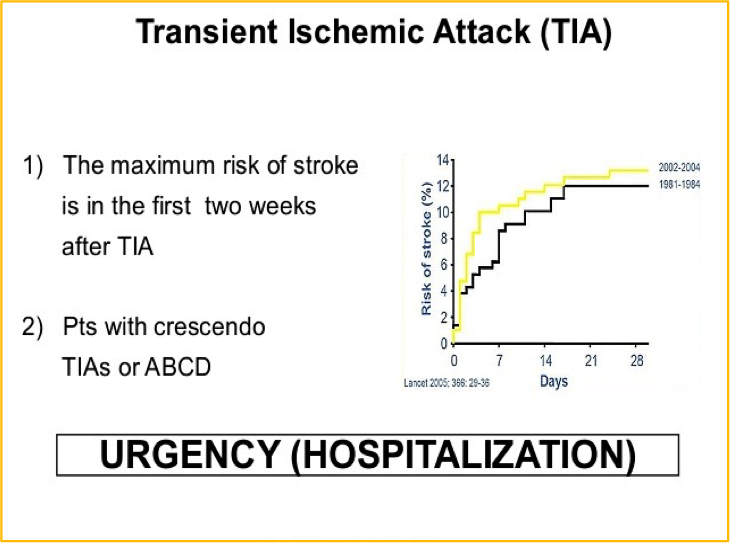
TIA: symptoms “Mini stroke”
A transient ischaemic is caused by a temporary disruption in the blood supply to part of the brain. - Warning sign for stroke - Brief localized ischemia
Common manifestations:
- Contralateral numbness
- Weakness of hand, forearm, corner of mouth
- Aphasia
- Visual disturbances- blurring
- Amaurosis fugax
Deficits last less than 24 hours (usually less than 1 or 2 hours)
Crescendo TIA’s
- Cerebral ischemia increasing in frequency, severity and duration
- Capsular warning syndrome: repeated weakness face, arm, leg
PLATELET AGGREGATION & THROMBUS FORMATION
Platelets (magnified here thousands of times) home to damaged areas of blood vessels and contribute to the formation of clots. Antiplatelet drugs can help reduce the risk of ischemic stroke.
CAUSES (ETIOLOGIES) OF ISCHEMIC STROKE: SIX MAIN CATEGORIES
| YOUNGER PATIENTS (< 55) | OLDER PATIENTS (> 55) | |
|---|---|---|
| Nonatherosclerotic vasculopathies | Large-artery atherosclerosis | |
| Hypercoagulable states | Small-artery disease | |
| Cardio-embolism | Cardio-embolism | |
| Hypotension | Hypotension |
Correct therapy depends on cause of stroke! “Cause” & “risk factor” are not synonymous—must Rx both!
ETIOLOGIC EVALUATION: IDENTIFY STROKE, FIND SOURCE OF CLOT
| NONINVASIVE (Day 1) | INVASIVE (Day 2) | |
|---|---|---|
| ARTERIES | MRI & intracranial MRA Carotid duplex (CD) | Catheter angiogram |
| HEART | ECG & monitor Cardiac biomarkers Transthoracic echo (TTE) | TEE |
| BLOOD | Hypercoagulable profile | in select patients |
Signs and symptoms
Consider stroke in any patient presenting with acute neurologic deficit or any alteration in level of consciousness.
- Abrupt onset of hemiparesis, monoparesis, or (rarely) quadriparesis
- Hemisensory deficits
- Monocular or binocular visual loss
- Visual field deficits
- Diplopia
- Dysarthria
- Facial droop
- Ataxia
- Vertigo (rarely in isolation)
- Nystagmus
- Aphasia
- Sudden decrease in level of consciousness
Examination
The goals of the neurologic examination include:
- Confirming the presence of stroke symptoms
- Distinguishing stroke mimics
- Neurologic baseline, to monitor progress
- Establishing stroke severity: (National Institutes of Health Stroke Scale [NIHSS]) to assist in prognosis and therapeutic selection
Essential components of the neurologic examination:
- Cranial nerves
- Motor function
- Sensory function
- Cerebellar function
- Gait
- Deep tendon reflexes
- Language (expressive and receptive capabilities)
- Mental status and level of consciousness
Cardio-embolic Sources
| High Risk | Medium Risk | Low / Unclear Risk |
|---|---|---|
| Atrial fibrillation | LV hypokinesia / aneurysm | Patent foramen ovale |
| Recent anterior MI | Bioprostetic valve | Atrial Septal Aneurysm |
| Mechanical valve | Congestive failure | Spontaneous Echo Contrast |
| Rheumatic mitral stenosis | Cardiomyopathy | |
| Thrombus / tumor | Myxomatous MVP | |
| Endocarditis |
Immediate Diagnostic Studies:
Evaluation of a Patient With Suspected Acute Ischemic Stroke All patients
- Non-contrast brain CT or MRI
- Blood glucose
- Oxygen saturation
- Serum electrolytes/renal function tests*
- Complete blood count, including platelet count*
- Markers of cardiac ischemia*
- Prothrombin time/INR*
- Activated partial thromboplastin time*
- ECG*
- Lumbar puncture (if SAH is suspected in CT –ve scan
- EEG (if SZ are suspected)
HYPERCOAGULABLE PROFILE PATIENTS < 55 YEARS OLD
- CBC
- PT/aPTT
- Fibrinogen
- Factor VIII
- Factor VII
- C-reactive protein
- Antithrombin III
- Protein C
- Protein S (total & free)
- Lipoprotein (a)
- Activated protein C resistance (APCR) (& Leiden factor V mutation if APCR -)
- Prothrombin G20210A mutation
- Antiphospholipid antibodies
- Methyltetrahydrofolatereductase (MTHFR) C677T & A1298C mutations
- Sickle cell screen
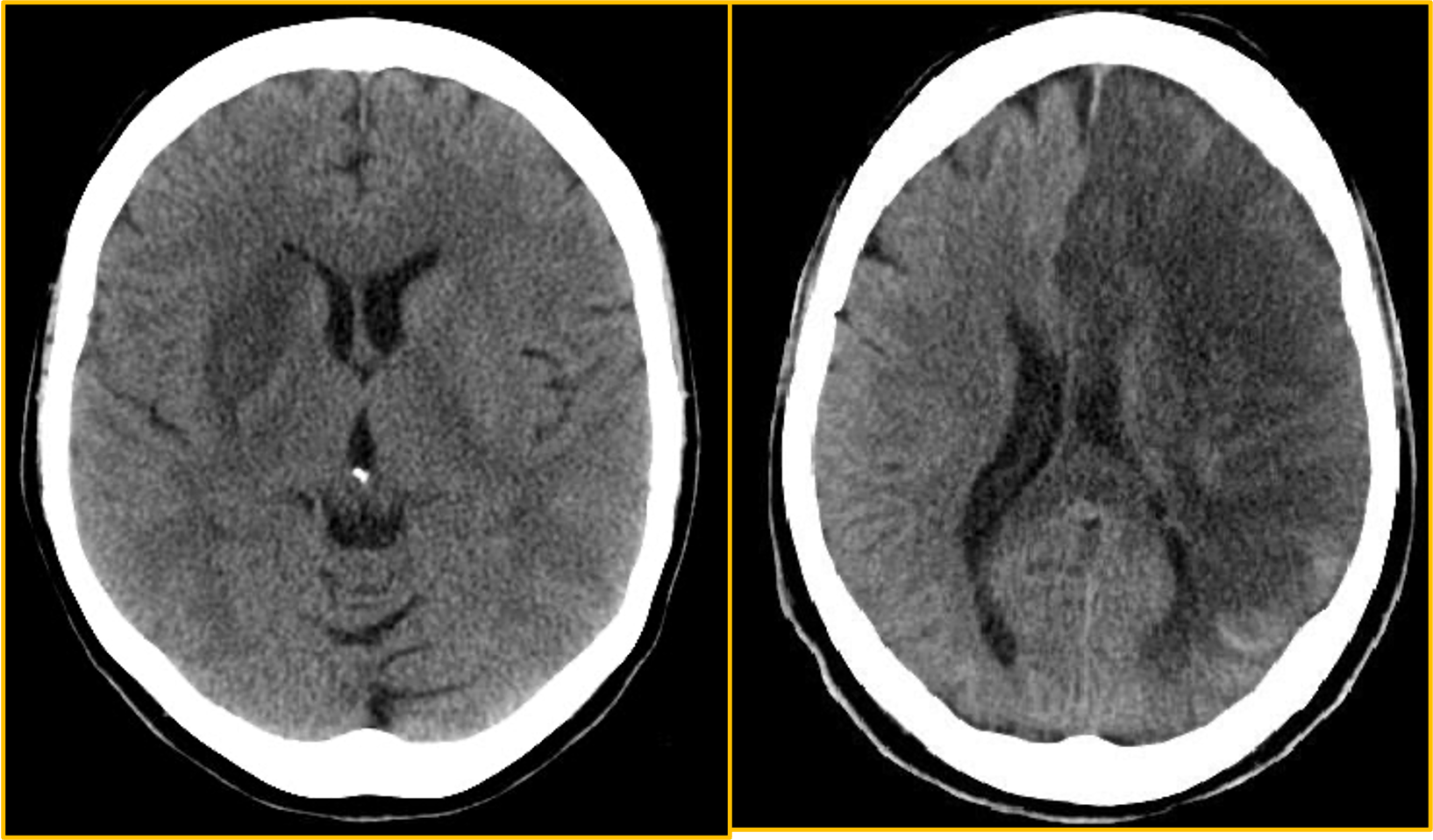
CT Examination
Axial non-contrast computed tomography (NCCT) scan demonstrates diffuse hypodensity in the right lentiform nucleus with mass effect upon the frontal horn of the right lateral ventricle in a 70-year-old woman with a history of left-sided weakness for several hours.
NCCT scan in a 52-year-old man with a history of worsening right-sided weakness and aphasia demonstrates diffuse hypodensity and sulcal effacement with mass effect involving the left anterior and middle cerebral artery territories consistent with acute infarction. There are scattered curvilinear areas of hyperdensity noted suggestive of developing petechial hemorrhage in this large area of infarction.
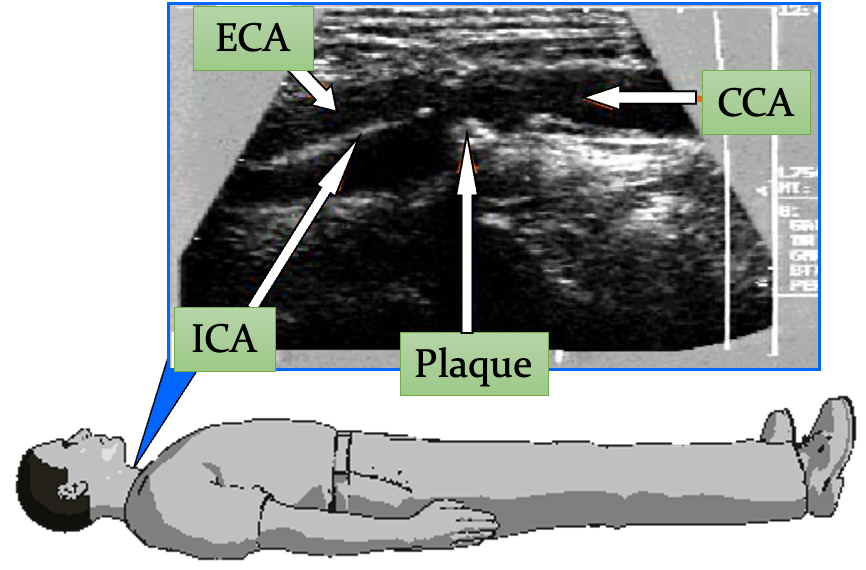
CAROTID DUPLEX
Evaluates carotid arteries in neck (operable area)
- Excellent screen in the right hands
- May not differentiate 99 vs. 100% stenosis
- Need contrast angiography for clinically relevant stenosis measurement
Carotid duplex =
- Doppler (velocities) +
- B-mode ultrasound (echo picture)
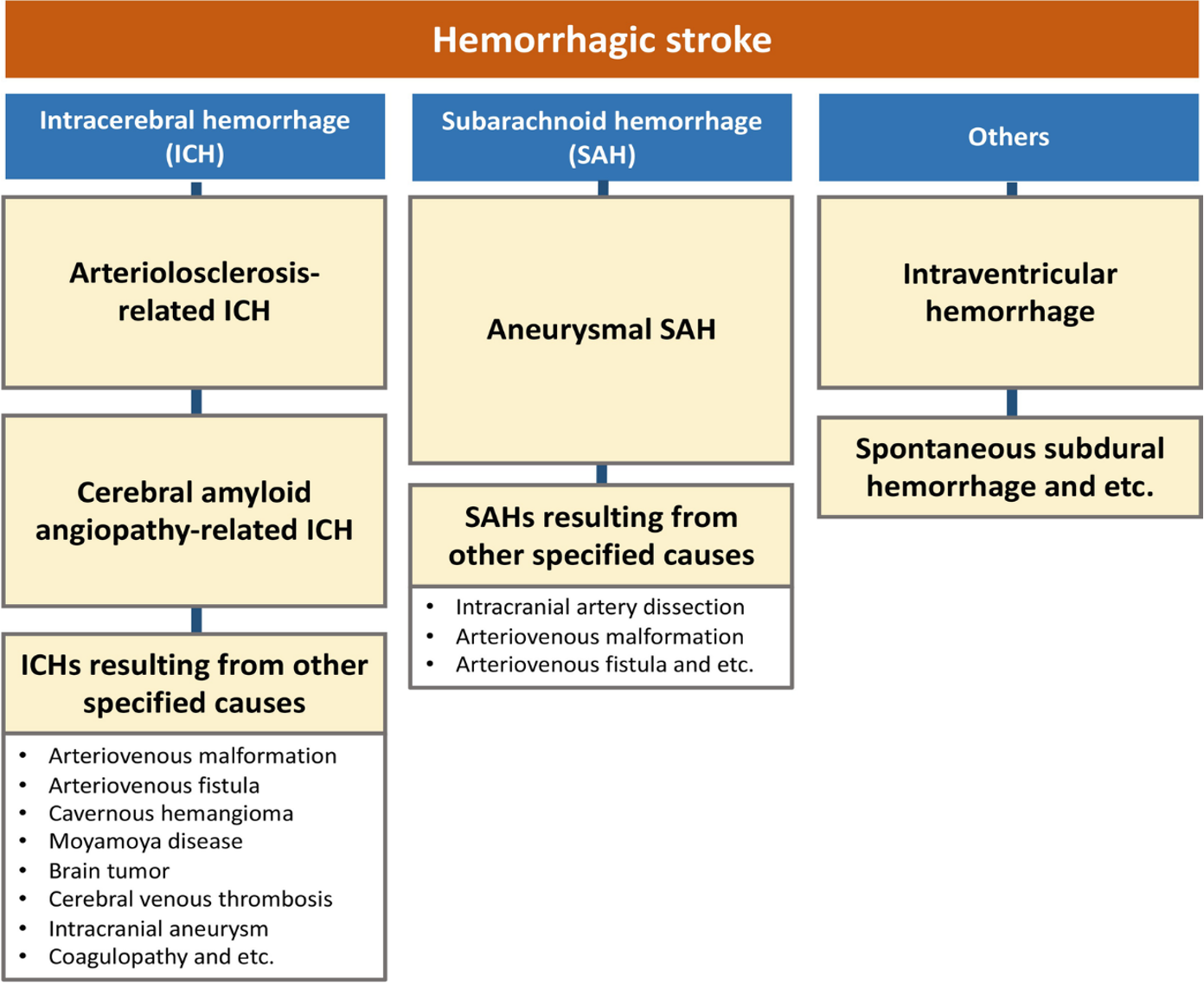
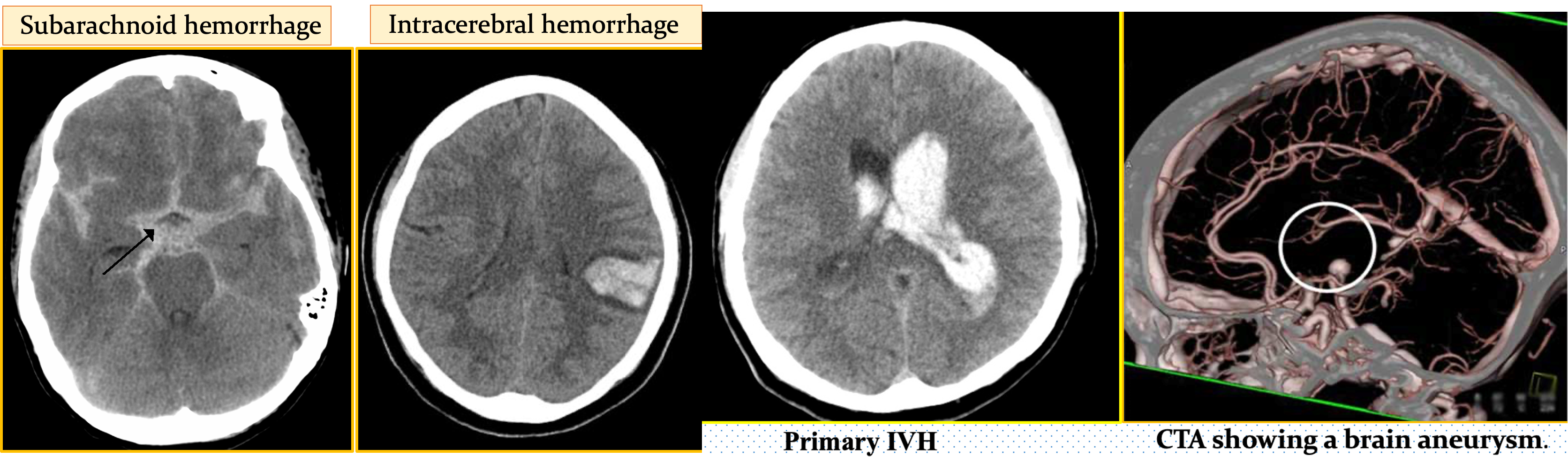
Hemorrhagic strokes
- Subarachnoid hemorrhage
- Intracerebral hemorrhage
Lacunar strokes
15 – 20% of ischemic strokes
- Small penetrating branches of circle of Willis, MCA, or vertebro-basilar artery
- Atherothrombotic or lipohyalinotic occlusion
- Infarct of deep brain structures
- Basal ganglia, cerebral white matter, thalamus, pons, and cerebellum
- From 3 mm to 2 cm
Clinical syndromes:
- Pure motor hemiparesis (with dysarthria)
- Pure sensory stroke (loss or paresthesia)
- Dysarthria-clumsy hand (with contralateral face and tongue weakness)
- Ataxia-hemiparesis (contralateral face and leg weakness)
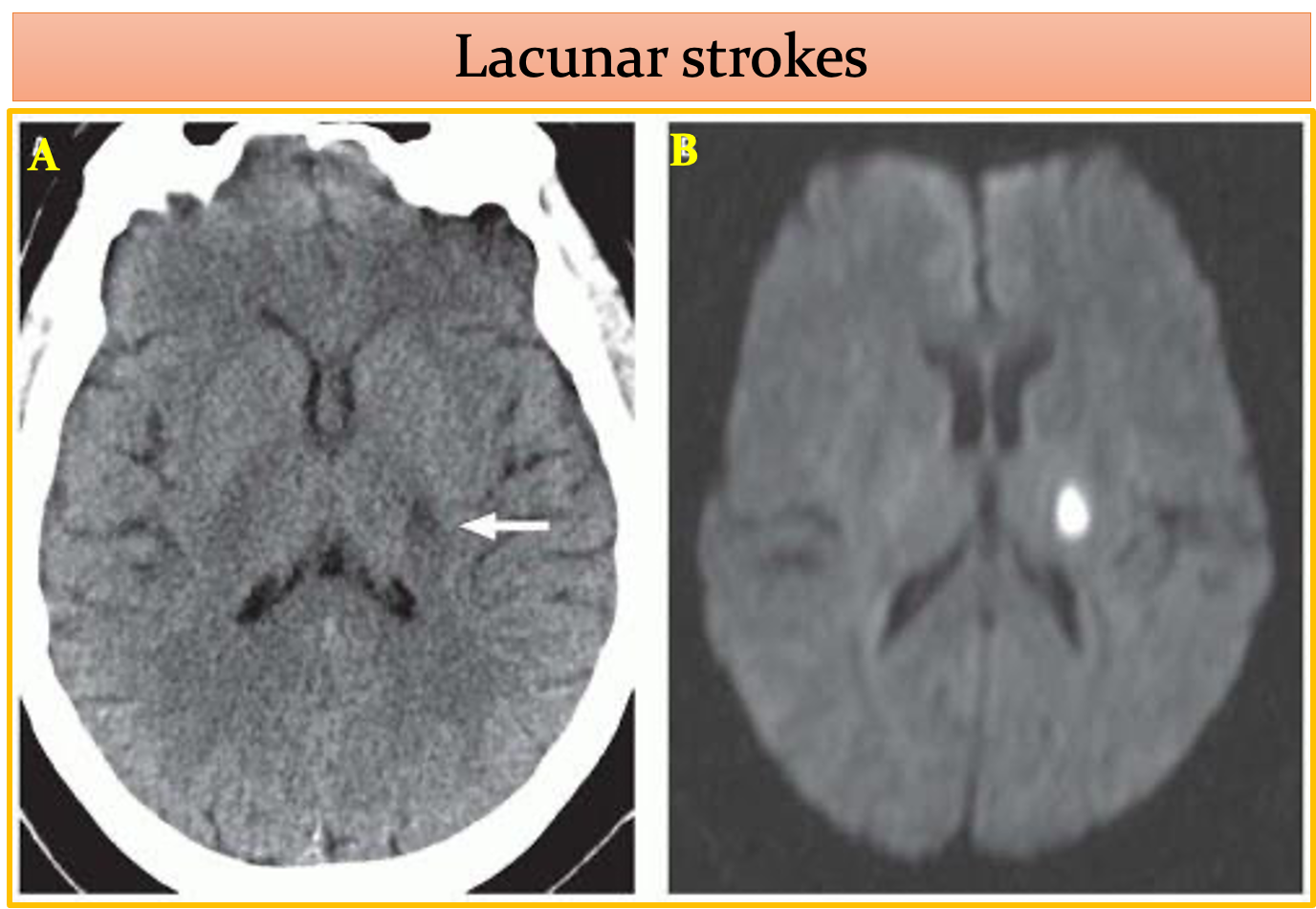 Acute lacunar infarct. A: Axial unenhanced CT image demonstrates an ovoid area of hypo density centered in the posterior limb of the left internal capsule. B: A corresponding DWI image demonstrates high-signal intensity, reflecting restricted diffusion in an acute lacunar infarct
Acute lacunar infarct. A: Axial unenhanced CT image demonstrates an ovoid area of hypo density centered in the posterior limb of the left internal capsule. B: A corresponding DWI image demonstrates high-signal intensity, reflecting restricted diffusion in an acute lacunar infarct
LACUNAR INFARCTS
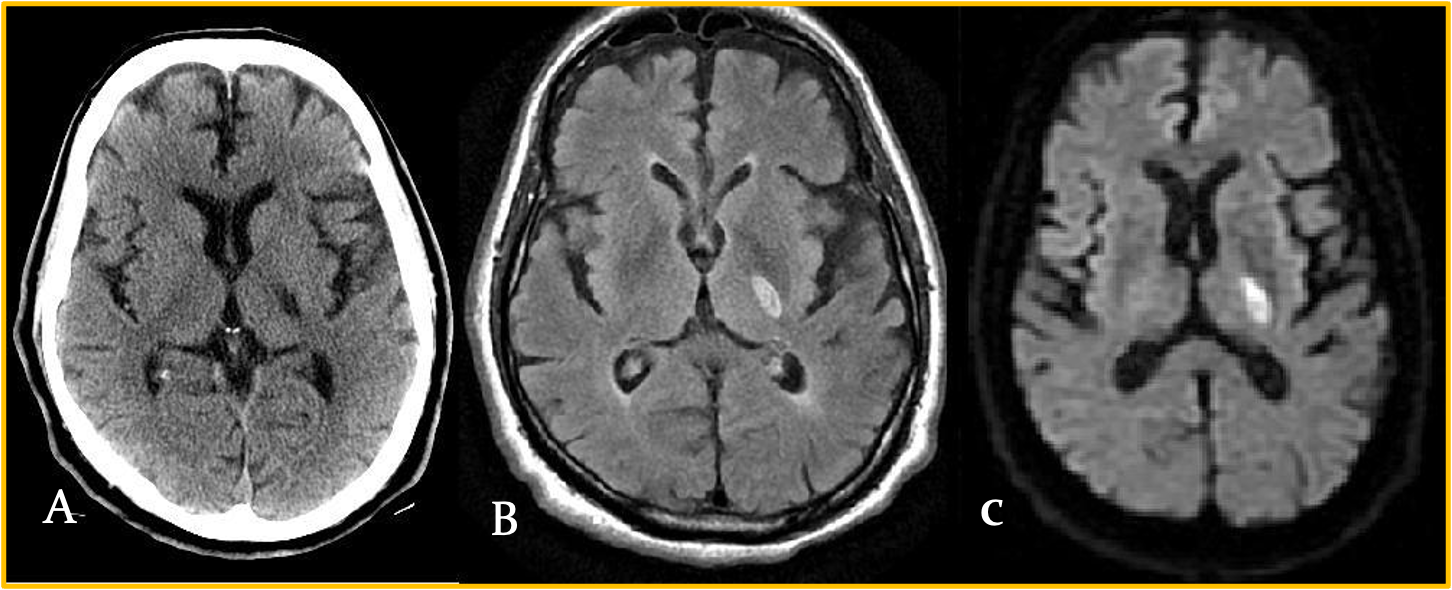
-
Axial NCCT scan: Demonstrates a focal area of hypodensity in the left posterior limb of the internal capsule in a 60-year-old man with acute onset of right-sided weakness.
-
High signal FLAIR sequence (middle image) and diffusion-weighted magnetic resonance imaging (MRI) scan (right image), with low signal on the apparent diffusion coefficient (ADC) maps indicating an acute lacunar infarction.
-
Lacunar infarcts are typically no more than 1.5 cm in size and can occur in the deep gray matter structures, corona radiata, brainstem, and cerebellum.
Deep border-zone, or watershed infarcts
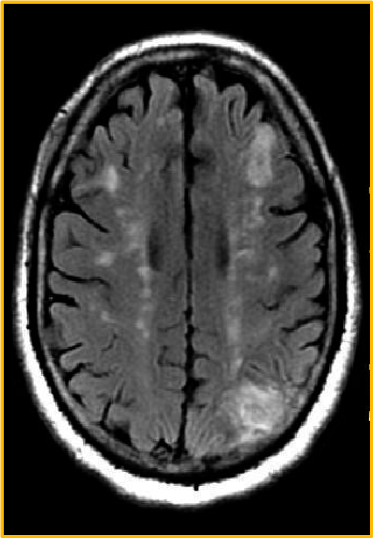
MRI scan of a 62-year-old man with HTN and diabetes and a history of transient episodes of right-sided weakness and aphasia. The FLAIR image demonstrates patchy areas of high signal arranged in a linear fashion in the deep white matter, bilaterally. This configuration is typical deep border-zone, or watershed infarction, in this case the anterior and posterior middle cerebral artery (MCA)
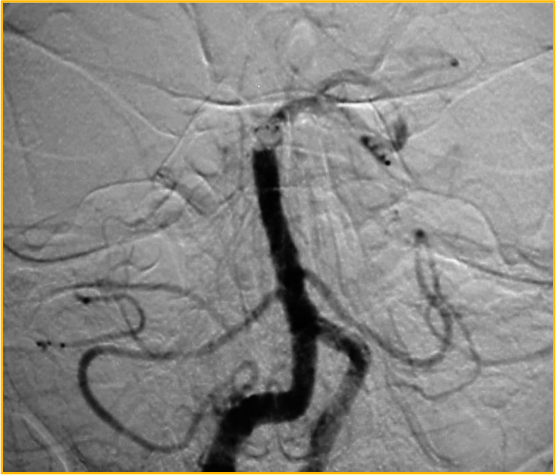
Cerebral angiogram showing basilar artery occlusion
Cerebral angiogram: performed approximately 4.5 hours after symptom onset in a 31-year-old man demonstrates an occlusion of the distal basilar artery.
MANAGEMENT: AIS
The goal for the management of stroke is to complete the following within 60 minutes or less of patient arrival:
- Assess airway, breathing, and circulation (ABCs) and stabilize the patient as necessary
- Complete the initial evaluation and assessment, including imaging and laboratory studies
- Initiate reperfusion therapy, if appropriate
- Critical treatment decisions focus on the following:
- The need for airway management
- Optimal blood pressure control
- Identifying potential reperfusion therapies (e.g., intravenous fibrinolysis with rt-PA (alteplase) or intra-arterial approaches)
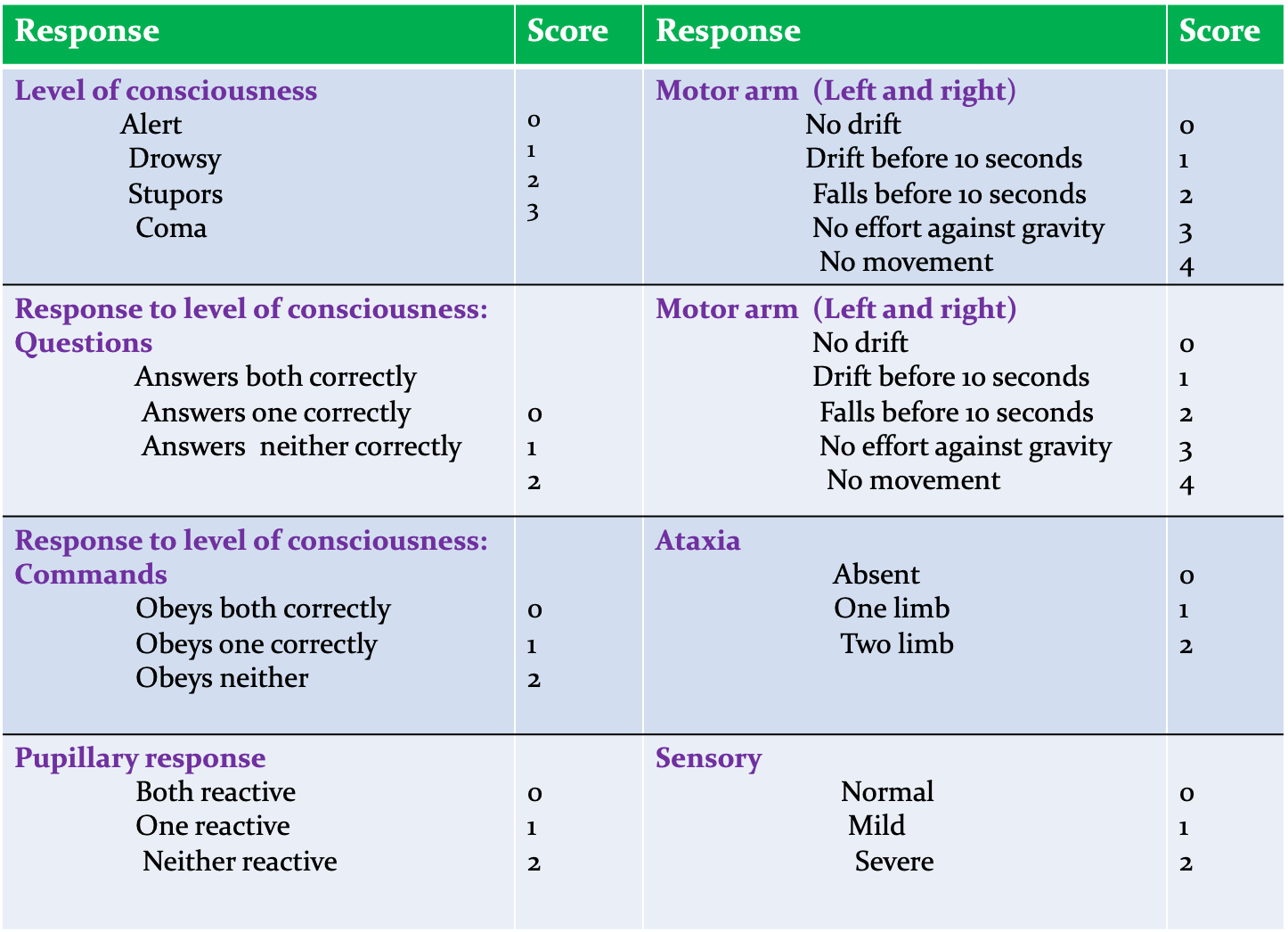
National Institutes of Health Stroke Max = 42
THE AIS-BP RELATIONSHIP
In AIS, high BP is a response not a cause – don’t lower it !
- BP increase is due to arterial occlusion (i.e., an effort to perfuse penumbra)
- Failure to re-canalize (w/or w/o thrombolytic therapy) results in high BP and poor neurological outcomes
- Lowering BP starves penumbra, worsens outcomes
Only definite indications to decrease BP emergently in AIS:
- AMI, CHF, Aortic dissection, ARF, or HTN encephalopathy
- Candidate for thrombolysis and BP > 185/110
Thrombolytic Therapy: Eligibility and Exclusion CriteriaX
IV tPA Indications: Within 3 hours of stroke symptom onset:
- AIS diagnosis with severe or mild but disabling stroke symptoms
- Symptom onset < 3 hours before starting treatment
- Age > 18 years
Between 3- 4.5 hours after stroke symptom onset:
- Age < 80 years
- No history of both DM and prior stroke
- NIHSS score < 25
- Not taking oral anticoagulants
- CT/MRI does not show involvement of > ⅓ of middle cerebral artery territory
If otherwise eligible and:
- BP is safely lowered to < 185/110 mm Hg.
- On antiplatelet drug therapy (aspirin or aspirin + clopidogrel) if benefit outweighs small risk of ICH
Contraindications for IV tPA: Z
- Symptom onset is unknown, > 4.5 hours, or if patient awoke with stroke
- Acute or previous ICH
- Imaging showing extensive regions of irreversible injury (hypo-attenuation)
- Prior ischemic stroke, severe head trauma, or intracranial/intra-spinal surgery within 3 months
- Symptoms of SAH
- GI malignancy or GI bleed within 21 days
- Coagulopathy: (Platelets < 100, 000/mm³, INR > 1.7, aPTT > 40 s, PT > 15 s)
- Treatment dose of low LMW heparin within 24 hours (does not apply to prophylactic doses to prevent VTE)
- Persistent elevated BP (systolic > 185 mm Hg or diastolic > 110 mm Hg)
Rt-PA Dosing:
- 0.9 mg/kg is total dose (Maximum total dose not exceed 90 mg)
- 10% given as bolus dose
- Remaining 90% as an infusion over one hour.
- Mix 50 ml of normal saline with 50 mg of rt-PA
- Mixture should be used within 6 hours.
Follow up of Patients Receiving rt-PA:
- Vital signs every 15 minutes/2 hrs: 30 minutes/ 6 hrs; hourly 24/ hrs until discharge.
- NIHSS assessment at 24 hours at day 7, 30 and 90.
- Ranking Scale and Barthel Index at 4 weeks and 3/12.
- Repeat CT Scan at 22-36 hours after start therapy.
- Physiotherapy and mobilization at 24 hours.
- Bloods at 24 hours day 30 or PRN: CBC, LFT, U/E’s, Blood Sugar, PT, PTT & INR
- Avoid (24 Hours) Invasive procedures, blood extraction, IM injections, NG tube, Folly’s cath.
THROMBOLYSIS COMPLICATIONS: SUSPECTD ICH
Prompted by :
- New headache
- Neurological deterioration
- Acute hypertension
- Nausea/Vomiting
Action:
- Discontinue rt-PA infusion
- Immediate CT Scan
- Blood: PT; PTT, INR, Platelet, Fibrinogen
- Give Fibrinogen 6-8 U & Cryoprecipitate with Factor VIII
- Prepare to give Platelets 6-8 U
No ICH on CT Scan:
- End algorithm
If ICH present on CT
- Evaluate Lab results: Fibrinogen, PT aPTT, INR
- Give fibrinogen or cryoprecipitate accordingly
- Alert Neurosurgeon
- Alert Hematologist
- Consider second CT Scan to assess size change
MANAGEMENT: AIS (Prevention)
Primary stroke prevention: refers to the Rx of individuals with no previous history of stroke. Measures may include use of the following:
- Platelet antiaggregants
- Statins
- Exercise
- Lifestyle interventions (e.g., smoking cessation, alcohol moderation)
Secondary prevention: refers to the Rx of individuals who have already had a stroke. Measures may include use of the following:
- Platelet antiaggregants
- Antihypertensives
- Statins
- Lifestyle interventions
MED
Cerebrovascular Accidents (Stroke)
Common presenting complaints – Weakness on one side of the body. Facial deviation or asymmetry. Loss of consciousness.
History of presenting illness –
- Start ((as my patient was apparently asymptomatic _ days back when he developed weakness on one side of the body.))
- The weakness was acute/insidious in onset and gradually progressive/static in nature.
- Activity Pt was involved in at the time when this weakness developed.
- PT fell down and hurt themselves as the attack occurred.
- What limb(s) or muscles affected; affected equally or not?
- First time or a previous similar condition had occurred.

Radio
Is defined as a sudden, focal neurological deterioration due to a disturbance in the blood supply to the brain.
Common causes: Cerebral infarction – Intracerebral haemorrhage - Subarachnoid haemorrhage.
Causes: Traumatic and none traumatic
- Hypertension
- Vascular malformations
- Coagulopathy
- Drug induced
- Tumor hemorrhage
- Trauma
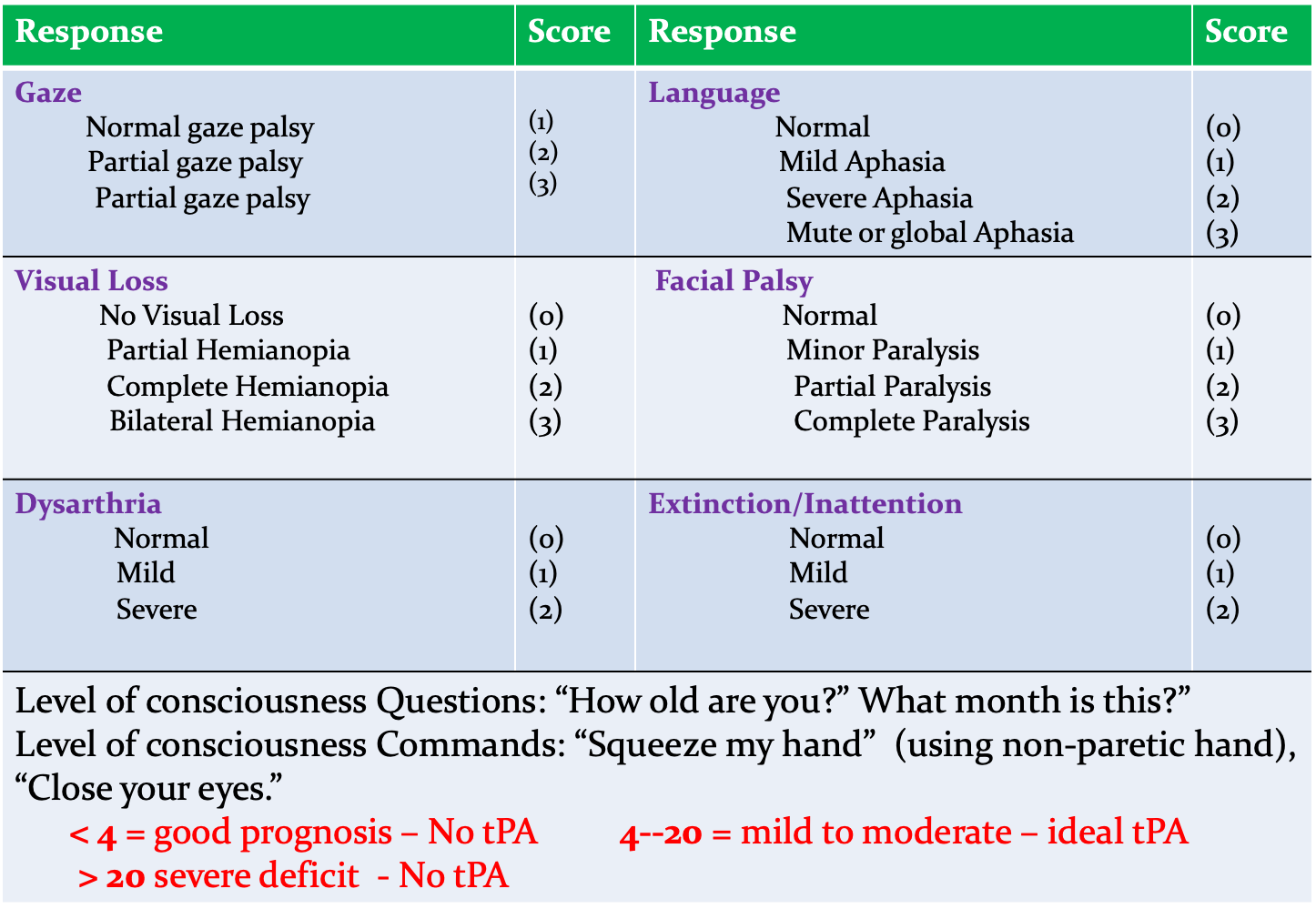
Initial imaging
CT without IV contrast
- Rapid
- Reliable to exclude hemorrhage
- High sensitivity for acute blood
- Acute blood appears bright (high attenuation) on CT relative to brain tissue.
- IV contrast only if suspicion of another etiology, e.g. tumor or AVM
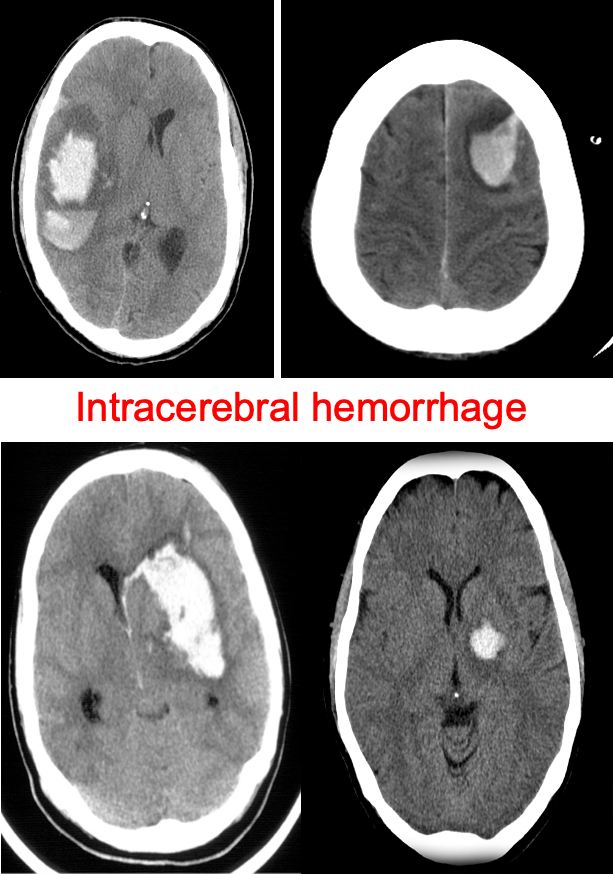 4th img----Pineal gland calcification - with intracerebral hemmorhage on left side of the brain
4th img----Pineal gland calcification - with intracerebral hemmorhage on left side of the brain