Reduction of Fractures
Methods of Reduction
-
Closed reduction:
- In most extra-articular fractures
- Simple metaphyseal / diaphyseal fractures
-
Open reduction
- In most intra-articular fractures
- Need perfect anatomical reduction
- Needs early mobilization (internal fixation better)
Reduction Techniques
-
Articular fractures:
- Need anatomical reduction: usually open (?? Closed)
- Needs early mobilization (internal fixation better)
-
Diaphyseal fractures: need functional reduction
- Restore: Length, Axis, and Rotation
- Exact a anatomical reduction of all fragments not necessary



Holding Reduction
Methods of Holding Reduction
- Methods of holding reduction
- Cast splint
- Internal fixation
- External fixation

Difference in Fracture Treatment
Intra-articular Fractures
- Need perfect anatomical reduction
- To avoid osteoarthritis
- Need early mobilization
- to maintain good range of motion and function
Extra-articular Fractures
- Need only functional alignment
- Of length, angulation, and rotation
- Can be immobilized longer
- with less risk of joint stiffness
Treatment of Fractures
Closed & Open fractures
Treatment of Closed Fractures
-
Emergency care (splinting)
- Splint them as they are (reduce major displacements)
- Adequate splinting is desirable
- Type of splints:
- Improvised
- Conventional
-
Definitive fracture treatment
- Reduce properly
- Hold reduction
-
Rehabilitation
- Muscle activity and
- Early weightbearing are encouraged
Conservative
-
Reduction (if displaced) – perform under general anesthesia; the sooner, the better.
-
Steps of reduction
- Traction
- Align the affected fragment(s)
- Reverse the mechanism of injury to restore anatomy
-
Immobilization – apply a POP (Plaster of Paris) cast, slab, or maintain traction.
-
Rehabilitation – commence once immobilization is secured.


Closed reduction 1. Traction in the line of the bone
-
Pressing fragment into reduced position
-
Disimpaction

Treatment of Open Fractures
- The four essentials are:
- Antibiotic prophylaxis
- Urgent wound and fracture debridement
- Stabilization of the fracture
- ? External Fixation
- Early definitive wound cover
Indications of Open Reduction Absolute
- Closed reduction fails
- Articular fragment requires accurate positioning
- Traction (avulsion) fractures with fragments held apart
Relative
- Multiple fractures
- Pathological fractures
- To promote early mobilization and prevent joint stiffness (e.g., diaphyseal fractures)


Types of Internal Fixation

| Type | Description | Images |
|---|---|---|
| Wires | • Simple, quick – Easy to apply – Easy to remove • Percutaneous • Not very stable – needs additional cast/splint • Mostly used in children | 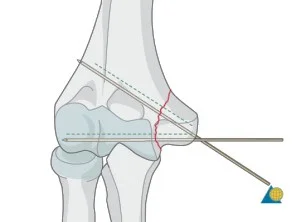 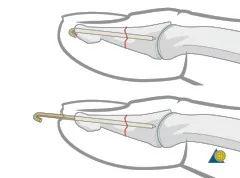  |
| Tension Band Wires | Special mechanics in – Patella – Olecranon – Malleolar fractures | 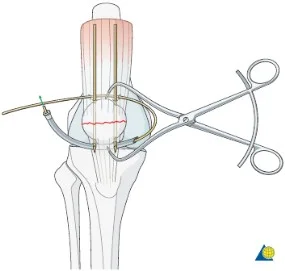   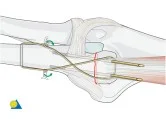 |
| Screws | Good fixation – stable – Can apply good inter‑fragmentary compression In simple fractures Can be applied percutaneous | 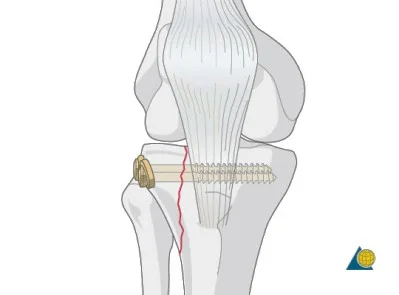 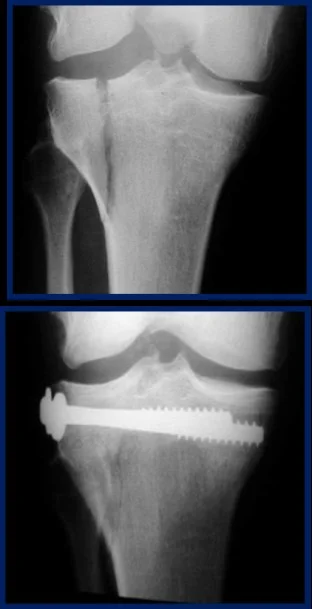  |
| Plates and Screws | Metaphyseal fractures Diaphyseal fractures Pelvis | 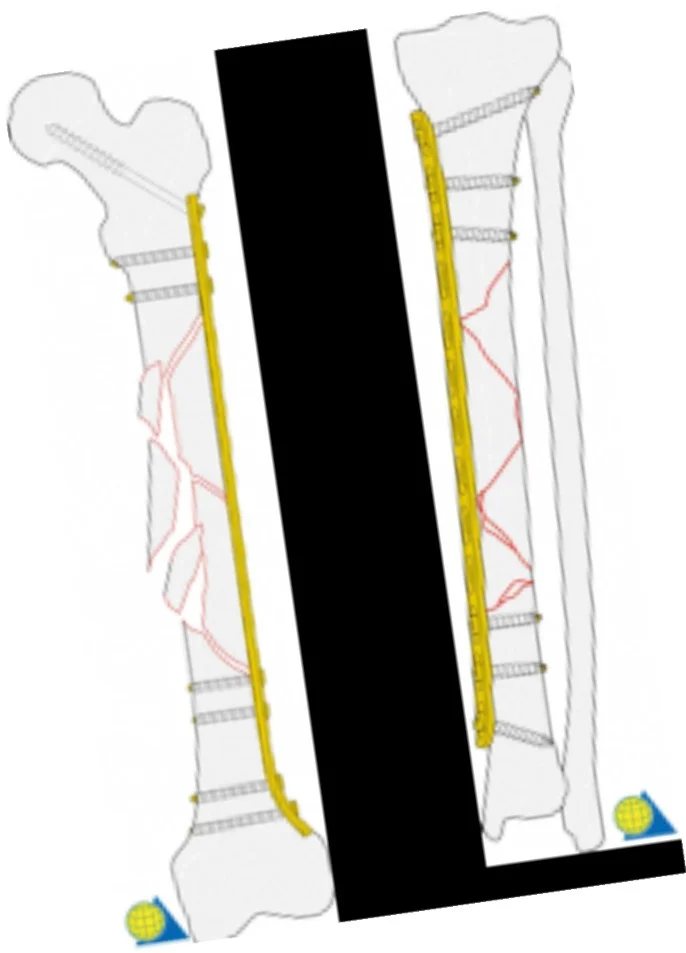  |
| Intramedullary Nails (IMN) | • Best fixation for diaphyseal long‑bone fractures – Femur, Tibia: preferred over plating • Locked IMN provide stable fixation |    |
Operative Vs. Non-operative Treatment
| Criteria | Operative | Non-operative |
|---|---|---|
| Risk of joint stiffness | Low | Present |
| Rehabilitation | Rapid | Slow |
| Risk of mal-union | Low | Present |
| Risk of non-union | Present | Present |
| Speed of healing | Slow | Rapid |
| Risk of infection | Present | Low |
| Cost | ? | ? |
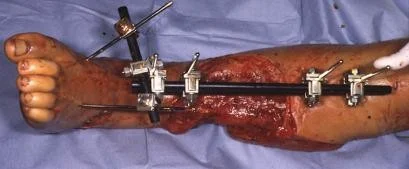
External Fixation
- Indications in acute trauma:
- Fractures associated with severe soft-tissue damage (including open fractures) or those that are contaminated
- Fractures around joints that are potentially suitable for internal fixation but the soft tissues are too swollen to allow safe surgery
- Patients with severe multiple injuries
Rehabilitation
-
Restore function of the
- injured parts and,
- patient as a whole
-
The objectives are:
- to reduce edema
- preserve joint movement
- restore muscle power
- guide the patient back to normal activity