MOA:
Binds with the 50s subunit Static The use of chloramphenicol, a broad-spectrum antibiotic, is restricted to life- threatening infections for which no alternatives exist. Chloramphenicol binds reversibly to the bacterial 50S ribosomal subunit and inhibits protein synthesis at the peptidyl transferase reaction . Due to some similarity of mammalian mitochondrial ribosomes to those of bacteria, protein and ATP synthesis in these organelles may be inhibited at high circulating chloramphenicol levels, producing bone marrow toxicity. Note: The oral formulation of chloramphenicol was removed from the US market due to this toxicity.
Spectrum:
Same as Tetracyclines Chloramphenicol is a broad-spectrum antibiotic. As with tetracyclines, it is effective against gram-positive and gram-negative bacteria, including Salmonella, Rickettsia, Mycoplasma and Chlamydia. Chloramphenicol is also effective against most anaerobic bacteria, including Bacteroides fragilis
Pharmacokinetics:
Absorption: Rapid and Fast (Less superinfection) • Chloramphenicol is rapidly and completely absorbed from the gastrointestinal tract and not affected by food ingestion or metal ions. Since absorption is rapid and complete after oral administration, there is less alteration of bacterial flora with less susceptability to superinfection
Distribution: - BBB: Passes with significant concentration • - Placenta: Passes (Grey Baby Syndrome) • - Excellent body fluids and tissues penetration. •
Excretion: needs healthy liver & kidney; otherwise adverse effects persist - Metabolites: Tubular secretion - Active Drug: Glomerular Filtration
Therapeutic uses:
Was the drug of choice in Typhoid (Now ciprofloxacin and Penicillens) (3rd) but now other safe and more effective drugs are used e.g. Ciprofloxacin and amoxycillin The serious and potentially fatal nature of chloramphenicol-induced bone marrow suppression restricts its use to a few life-threatening infections in which the benefits outweigh the risks.
- Topical Eye and Ear
- Others:
- 3rd choice Pyogenic Meningitis (After Penicillens & 3rd cephalosporins). immediate Lumber puncture + Empiric Therapy
- H.Influenzae (arthritis, Osteomylitis and epiglottitis)
- Severe anaerobic infections of brain caused by penicillin- resistant bacteria, such as B-fragilis
- Rickettsia (After Tetracycline and Macrolides); Chloramphenicol is an alternative to tetracycline
- Topical treatment of both ear and eye infections
Adverse effects:
- Toxic Bone Marrow depression:
- Dose dependent (Reversible)
- Anemia, thrombocytopenia, leucopenia, Sore throat • is recognized as anemia, thrombocytopenia or leukopenia (agranulocytosis). It is reversible on discontinuation of the chloramphenicol
Treatment: Stop the drug • Fresh Blood transfucion • Cortisone • Penicillin to eradicate strept in the throat • Bone marrow stimulants (Growth factor, vitamin B complex, adenine sulphate, pentose
-
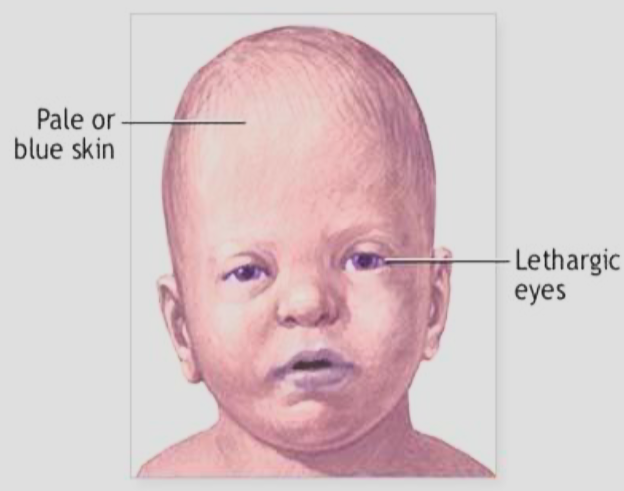
Grey Baby Syndrome: (40% Mortality) • If large doses are given to infants with immature hepatic conjugation. • Abdominal destention, vomiting, cyan; It occurs in newborn infants with large doses, especially those born prematurely. It is due to immature hepatic conjugating mechanism and in-adequate renal excretion which leads to high levels of chloramphenicol. This syndrome is characterized by abdominal distention, vomiting, progressive cyanosis, irregular respiration, hypothermia, flaccid paralysis and vasomotor collapse. Mortality is high (40%).
-
Others adverse effects:
- GIT Upset (nausea, vomiting, diarrhea and glossitis) •
- Superinfection (usually occurs after 5 –10 days) •
- Hypersensitivity (skin rashes, fever, angioedema (not frequent) •
- Optic Neurites and encephalopathy (Rare)
Drug Interactions:
Chloramphenicol inhibits the activity of the liver microsomal enzymes and thus enhances the activity of drugs, such as dicoumarol, diphenylhydantoin and tolbutamide which are normally degraded by these enzymes.