EM
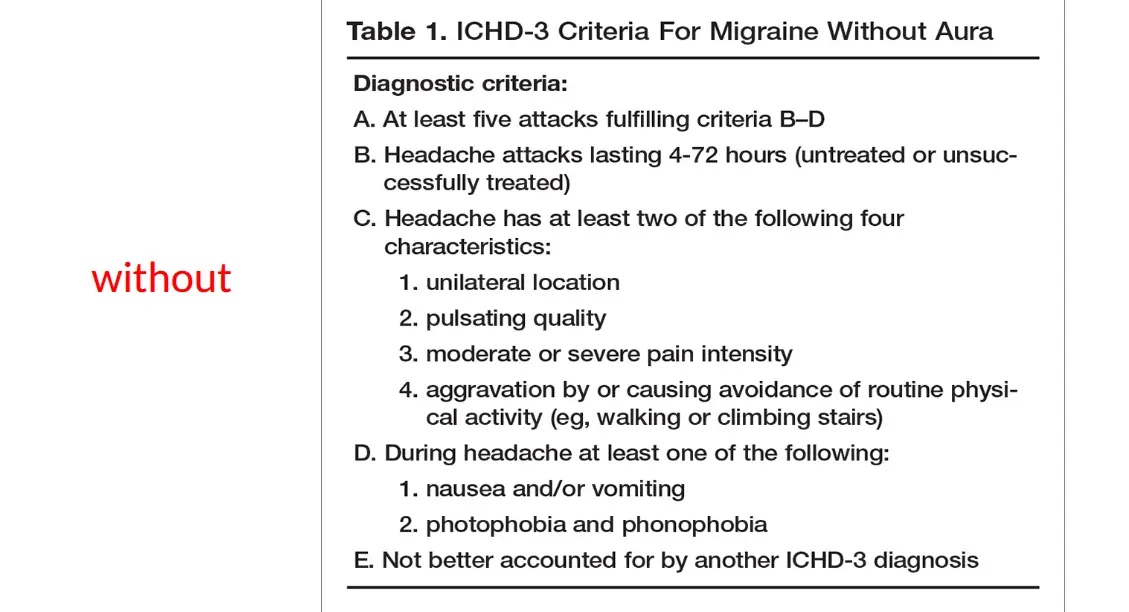
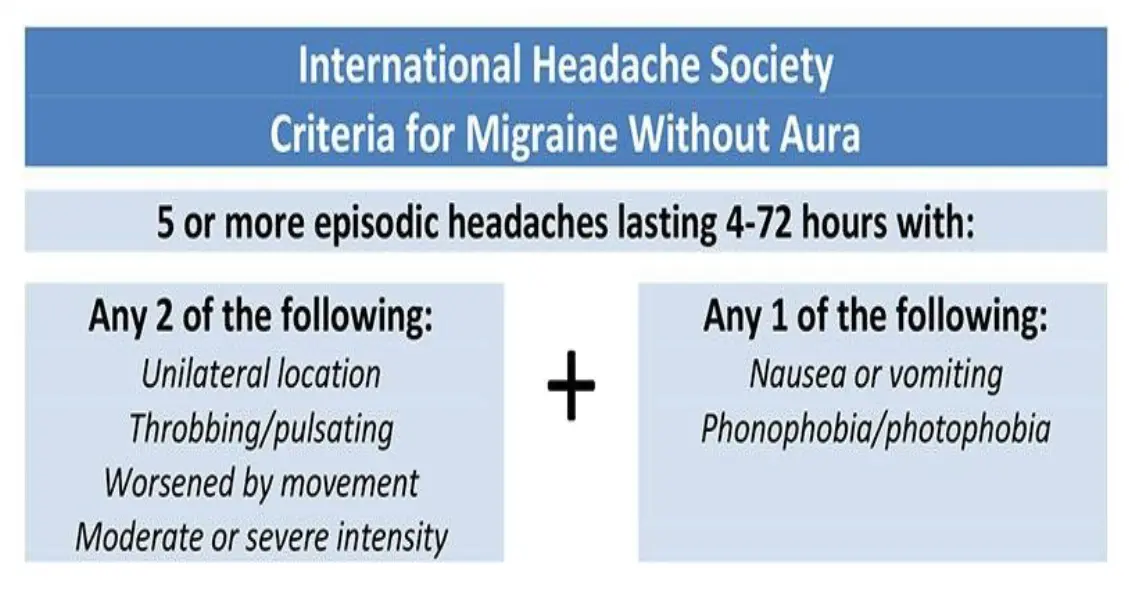
- Migraine is a primary headache disorder characterized by recurrent headaches that are moderate to severe
- most often unilateral with some cases associated with visual or sensory symptoms—collectively known as an aura
- more common in women and has a strong genetic component.
- Pain builds up over a period of 1-2 hours, progressing posteriorly and becoming diffuse
- Headache lasts 4-72 hours, however in young children frequently lasts less than 1 hour.
- Aggravates with movement or physical activity.
Pathophysiology
- The underlying causes of migraines are unknown. However, they are believed to be related to a mix of environmental and genetic factors
- Triggers include -psychological stress, hormonal changes (menarche, OCP, pregnancy, menstruation, menopause etc),dietary intake (MSG, chocolate, wine, tyramine etc),environmental(indoor air quality and lighting)
Continued pathophysiology
- Neurovascular theory--- neuronal hyperexcitability in cerebral cortex
Cortical spreading depression theory by Leao - explain the mechanism of migraine with aura - CSD is a well-defined wave of neuronal excitation in the cortical gray matter that spreads from its site of origin at the rate of 2-6 mm/min. This cellular depolarization causes the primary cortical phenomenon or aura phase; in turn, it activates trigeminal fibers, causing the headache phase
- Vasoactive substances and neurotransmitters-----
Perivascular nerve activity also results in release of substances such as 5-HT, substance P, neurokinin A, calcitonin gene-related peptide, and nitric oxide, which interact with the blood vessel wall to produce dilation, protein extravasation, and sterile inflammation. This stimulates the trigeminocervical complex
Signs and symptoms
- Throbbing or pulsatile headache, with moderate to severe pain that intensifies with movement or physical activity
- Unilateral and localized pain in the frontotemporal and ocular area, but the pain may be felt anywhere around the head or neck
- Nausea (80%) and vomiting (50%), anorexia, food intolerance, and light-headedness
- Sensitivity to light and sound Z
- Other neurologic symptoms----Hemiparesis (hemiplegic migraine), Aphasia, Confusion, Paresthesias or numbness
Phases
prodrome, which occurs hours or days before the headache— altered mood, irritability, depression or euphoria, fatigue, craving for certain food, stiff muscles (especially in the neck), constipation or diarrhea, and sensitivity to smells or noise
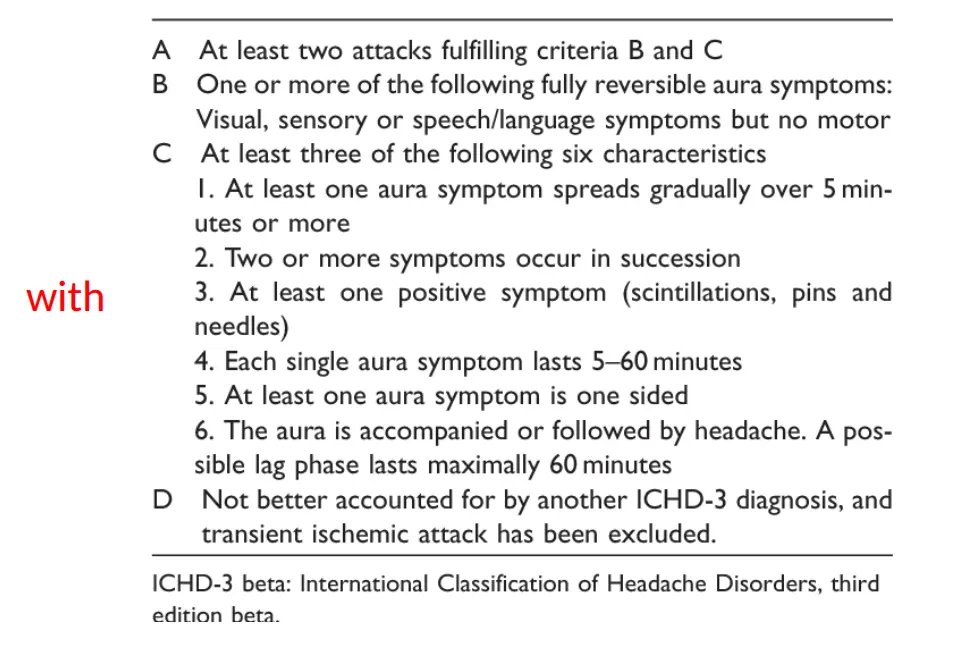
aura which immediately precedes the headache, and generally last less than 60 minutes---- Symptoms can be visual(scintillating scotoma),sensory(pins-and-needles,numbness ,loss of position sense),speech or language disturbances, motor (weakness)
Pain phase also known as headache phase
postdrome —the effects of migraine may persist for some time after the main headache has ended;(impaired thinking, general malaise ,GI symptoms, mood changes, weakness etc)

 Central scotoma
Central scotoma
 Scintillating scotoma
Scintillating scotoma
Differential diagnoses of migraines
- temporal arteritis
- cluster headaches
- acute glaucoma
- Meningitis
- subarachnoid hemorrhage
Management
KEY: avoid triggers
-
Analgesics (acetaminophen) NSAIDs (aspirin, ketorolac, ibuprofen, naproxen) and opioid analgesics (eg, oxycodone, morphine sulfate) — mild to moderate cases specific in migraine
-
5-hydroxytryptamine-1 (selective 5-HT1 agonists) (triptans) — eg: sumatriptan (oral/SC/nasal spray), rizatriptan, Zolmitriptan
-
ergot alkaloid (nonselective 5-HT1 agonists) eg: ergotamine, dihydroergotamine (DHE) [(alpha-adrenergic antagonist and serotonin antagonist effect)(iv/im/sc/intra nasal)]
-
Metoclopramide (IV or oral) (5HT3-receptor antagonist and a dopamine antagonist, prokinetic antiemetic)---enhances the analgesic effect with NSAIDS
-
5-HT 1B/1D agonists are contraindicated in individuals with a history of cardiovascular and cerebrovascular disease
-
Excessive use of abortive medication can lead to rebound headaches or either stop it
Management continued
Prophylaxis If attacks are frequent (more than 3–4 per month), prophylaxis should be considered
1st line: Beta blockers (atenolol or propranolol), Tricyclic antidepressants (amitriptyline), valproic acid (enhance GABA neurotransmission), Divalproex, Topiramate
2nd line: methysergide (ergot) flunarazine (calcium channel blocker), MAOIs (Phenelzine), gabapentin
- Botulinum toxin A—intractable, chronic migraine
- NSAID’S like naproxen
- TENS transcutaneous nerve stimulation device
other types
-
Status Migrainosus (an attack lasting over 72 hours) treated with steroids, iV valproate or ergotamine
-
Menstrual Migraine---perimenstrual use of preventive agents (e.g. triptan), perimenstrual estrogen treatment with estradiol (0.5 mg orally twice a day, or a 1-mg transdermal patch)
IM
Migraine
- Usually starts in adolescence or early adult life
- Family history often positive
- More common in females
Characteristics:
- Usually unilateral (may be generalized also)
- Throbbing (may be continuous dull ache also)
- Each episode lasts for 4-72 hours
- Pain aggravated with physical activity
- Often accompanied with nausea, vomiting, photophobia, phonophobia, visual blurring
- In some patients, “AURA” may occur just before the headache
Aura
Clinical features which occur 30 to 60 min. before the headache, warning the person that the headache is coming.
- Visual features: like visual field defects (scotomas), flickering lights, zig-zag lines, colored spots before the eyes etc.
- Neurological features: like Numbness, paresthesias, aphasia, weakness, dysarthria
Some Points about Aura
- Occurs only in about 30% of the migraine patients
- Some people get Aura but no headache (aura without headache). Can be confused with stroke/TIA
- Aura is not dangerous by itself
Pathogenesis of Migraine Z
Dysfunction of the neurons in the brain ⇒ leads to release of chemicals (neuropeptides) ⇒ act on the intracranial blood vessels ⇒ vasodilation ⇒ produces headache
Remember 1 important neuropeptide: Calcitonin Gene-Related Peptide (a peptide which is related to the calcitonin gene) CGRP
Things which can trigger a migraine attack
- Sleep disturbances: (less sleep, disturbed sleep pattern)
- Emotional & excess physical stress
- Menstruation
- Dehydration
- Excess exposure to TV / computer screens (so, no PS4)
- Foods: (Chocolate, Cheese, Coffee, alcohol, MSG found in Chinese foods)
- Bright & flickering lights
- Strong smells: (perfumes, benzene, chemicals, food smells)
- Oral contraceptives
Work up in a Migraine Patient
- Migraine is a clinical diagnosis, based on the history
- There is no blood test or imaging to “diagnose”
- Imaging like CT or MRI brain is done to rule out other intracranial pathology
Management of Migraine
- Avoid the triggering factors
- Healthy lifestyle (good sleep, no alcohol, exercise, no stress, avoid TV or mobile phone screens for long periods)
- Medicines to treat the acute attack
- Maintenance treatment (ALAATOOL) in some patients
Management of Acute Attack
- Lie down in a dark quiet room
- Avoid light and loud sounds
- Medicines (any of the following). Take at the start of the aura or headache.
A) Simple Analgesics (Panadol with caffeine, Panadol extra, NSAIDs). Don’t overuse (can lead to “medication overuse headache”)
B) Ergotamine Containing Meds e.g. Cafergot (ergotamine + caffeine). Avoid in pregnancy, CAD, HTN.
C) Triptans (expensive) ++ Cluster headaches not tension e.g. sumatriptan, zolmitriptan etc.
- Oral tabs, nasal sprays, subcutaneous injections
- Quick relief
- They are “serotonin receptor agonists”, & prevent the release of “migraine causing neuropeptides”
- Contraindicated in pregnancy, uncontrolled HTN, CAD, history of stroke
D) Blockers of (CGRP inhibitors) “Calcitonin Gene Related Peptides”
E) Antiemetics
- Metoclopramide, chlorpromazine, prochlorperazine
- Used along with analgesics to help the nausea/vomiting; symptomatic treatment
Narcotic analgesics are not used (why?) Risk of addiction, tolerance ++ Respiratory depression sedation constipation
Chronic Management of Migraine
Long term treatment given to people who have very frequent acute attacks (more than 3 times a month)
- Some antihypertension meds like propranolol, verapamil, & candesartan.
- Anti-epileptic meds like Topiramate, valproic acid
- Antidepressants like Amitryptyline; great for long run
- Some monoclonal antibodies (injections)
- Acupuncture
Rapid Fire Questions on Migraine
- Is it a primary or secondary headache? Primary
- Name some secondary headache syndromes? HTN, Eye disease, Intracranial hemorrhage, SOLs ; secondary(face diseases + HTN)
- Name 3 primary headaches? Migriane, tension, Cluster
- Usual location of migraine? Unilateral usually could be both sides
- Nature of migraine pain, throbbing or continuous? Throbbing
- Other symptoms associated with the attack? Neusea/Vomitting, Photophobia, Phonophobia, blurred vision
- What is an aura? before migraine attack
- Name some visual features of an aura? zig zag line, colored spots vision; numbness, hemiplegia
- Name some neurological features of an aura? 30%
- Is aura LAAZIM in all migraine patients? no
- Aura is dangerous, right or wrong? **
- Aura can occur without any headache, right or wrong? **
- Aura can be confused with what?
- Which chemicals are released in the brain to cause migraine? Name any 1? neuropeptides
- Which foods can trigger an attack? CCC ; C4, Chocolate, Caffiene CC
- Name some more triggering factors? sleep disturbance, menstural irregularities, perfumes, oral contraceptives, stress
- Diagnosis of migraine is based on what, CT or MRI? clinical diagnosis
- During an acute attack, what should the patient do, besides taking meds? sit in darkroom, avoid sound bright
- Name the 3 commonly used meds to treat an acute attack? panadol extra, analgesics, triptans
- Why not to use pain killers for a long time? Overuse results in headache
- Name any triptan? **
- Mode of action of triptans? serotonin receptors
- Name 3 contraindications to use triptans and ergotamine? pregnancy… constriction
- Name a newer drug to treat the acute attack? CGRP + Monoclonal
- What other symptomatic treatment along with analgesics? antimetics
- When to give chronic treatment? proponolol
- Name 3 meds used as chronic management? propanolol, amitriptyline, INR