RESP
History
Symptoms of Respiratory system
-
Cough; Persistent Cough in Adults and Chronic Cough in Children,may indicate B.A,GERD , or Cystic fibrosis
-
Dyspnoea (acute, progressive or paroxysmal)
-
Chest pain
-
Fever
-
Hoarseness
-
Night sweats, Sleepiness
-
Loss of appetite is a common feature whenever people are unwell it suggests that the disease is having a significant effect on well-being.
- Significant loss of weight may well be indicative of serious illness - eg, malignancy or tuberculosis.
- Upper gastrointestinal symptoms: gastro-oesophageal reflux is a common cause of chronic cough.
- Heart disease may cause respiratory symptoms. Establish whether there are any indications of heart failure or coronary heart disease.
- Severe anaemia may cause breathlessness.
- Rheumatoid arthritis and other connective tissue diseases may cause respiratory symptoms.
- Neuromuscular diseases may cause respiratory symptoms, particularly dyspnoea.
Past Hx
-
Use of inhalers (assess compliance and technique).
-
Use of steroids (some measure of severity in asthma).
- Other drugs which may have relevance in respiratory disease - eg, angiotensin-converting enzyme (ACE) inhibitors (cough).
- Allergies; Ask about all allergies including, for example, food, inhaled allergens and drugs.
Occupational/Social Hx
- An occupational history may be very important in respiratory disease. - Hobbies and pets may also be responsible for respiratory disease. - Lifestyle and alcohol consumption are also very relevant to respiratory diseases.
- Ask about illicit drugs. - Smoking history should detail, for example, the type and number of cigarettes smoked currently and in the past.
- Ask also about passive smoking. - Sexual history may be relevant to risk of HIV and AIDS.
Family Hx
- Respiratory diseases with a genetic component - -eg, cystic fibrosis, emphysema (alpha-1-antitrypsin deficiency). - Infectious diseases such as -tuberculosis (remember high-risk groups). - Atopic diseases such as -asthma, hay fever and eczema.
Main symptoms and signs in common respiratory diseases
- Chill
- Continued fever: 39-40ºC
- Chest pain
- Tachypnea
- Cough
- Rusty sputum
Examination
Inspection:
laying on back - bilateral implications lying on infected side giving space to healthy lung -
General Inspection:
- Evidence of respiratory distress at rest or when walking - eg, obvious breathlessness, talking in short phrases rather than full sentences, use of accessory muscles, exhalation with pursed lips. - Evidence of other respiratory symptoms - eg, cough, audible wheeze. - Note whether the patient appears to be pyrexial (check their temperature). - Note whether there are any indicators of recent weight loss - eg, sunken cheeks.
Hands:
- Finger clubbing. - Cyanosis. - Tobacco staining. - Radial pulse: tachycardia suggests significant respiratory difficulty or marked overuse of a beta agonist.
- Lung cancer can cause atrial fibrillation.
- A large pneumothorax or a tension pneumothorax can cause pulsus paradoxus. - A tremor may indicate carbon dioxide retention.
- Weakness of hand’s small muscles.
Wrist:
- Pulse: rate & character
- Flapping tremors (asterixis)

Neck:
- JVP: increase in corpulmonale & SVC obstruction. eg, cor pulmonale.
- LN: enlargement in CA bronchus or metastasis; Lymphadenopathy
- Goitre (any possible tracheal obstruction). - Evidence of superior vena cava obstruction (may be caused by lung cancer).
Face:
- General appearance - eg, Cushingoid as a result of long-term use of steroids. - Tongue: central cyanosis - Anaemia (conjunctivae). - Eye: Horner’s syndrome (possible apical lung cancer). in CA bronchus
- SVC obstruction: plethoric & cyanosed, injected
eyes.

Respiratory distress
- Can not complete sentence
- RR (14-20) per min (Tachypnea)
- Use of accessory muscles, paradox movement and intercostal drawing
- Cyanosis
- Lip breathing

Chest Inspection
1- Tracheal.
2- Chest wall deformities:
- Kyphosis - curvature of the spine - anterior-posterior
- Scoliosis - curvature of the spine - lateral
- Barrel chest - chest wall increased anterior-posterior diameter (normal in children) typical of hyperinflation
- Pectus excavatum
- Pectus carinatum
Overinflated (may indicate chronic obstructive pulmonary disease
(COPD)or severe acute asthma).
Asymmetry (the abnormality is on the side that moves less - eg,
pneumothorax, collapse, consolidation or effusion).
Other abnormalities include pigeon chest (pectus carinatum), funnel chest (pectus excavatum). Kyphosis and/ or scoliosis.


Abdomen and lower limbs: - Hepatomegaly may indicate right heart failure. - Swollen calf (possible deep vein thrombosis). - Peripheral oedema may be noted (lower legs if ambulant or sacral if bed-bound).
Respiration Inspection
Respiratory rate (normal for an adult is about in between 12-18 with an average14/minute). - Note any indication of respiratory distress.
Nature of breathing, including:
- Kussmaul’s breathing: deep and laboured breathing, often associated with severe metabolic acidosis.
- Cheyne-Stokes’ breathing: progressively deeper breathing followed by temporary apnoea, which may occur with heart failure, cerebrovascular disease, head injury, carbon monoxide poisoning or brain tumours, or be a normal variant during sleep or at high altitude.
- Respiratory movement
- Abdominal breathing: male adult and child
- Thoracic breathing: female adult.
- Symmetry: posteriorly and anteriorly looking for decrease or delayed chest movement during moderate respiration
- Respiratory rate: 16-18 b/min
- Tachypnea: >20 b/min
- Bradypnea: <12 b/min
- Shallow and fast
- respiratory muscular paralysis, elevated intraabdominal pressure, pneumonia, pleurisy
- Deep and fast
- Agitation, intension
- Deep and slow
- Severe metabolic acidosis (Kussmaul’s breathing)
-
Respiratory rhythm Cheyne-Stokes’ breathing
-
Inhibited breathing
- Sudden cessation of breathing due to chest pain
- Pleurisy, thoracic trauma
- Sighing breathing
- Depression, intension
- Scars:
- From previous operation or chest drains or cautery marks or radiotherapy markings.
- Paradoxical chest movement may indicate a fractured rib
- Prominent veins:
- in case of SVC obstruction
Palpation:
Trachea:
- Normally central, slight right displacement .
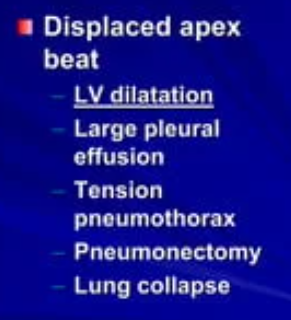
Apex beat & mediastinum:
- Check for displacement.
Chest expansion:
- Normal expansion ≥ 5cm All three areas front and back
Thoracic expansion:
- Massive hydrothorax, pneumonia, pleural thickening, atelectasis
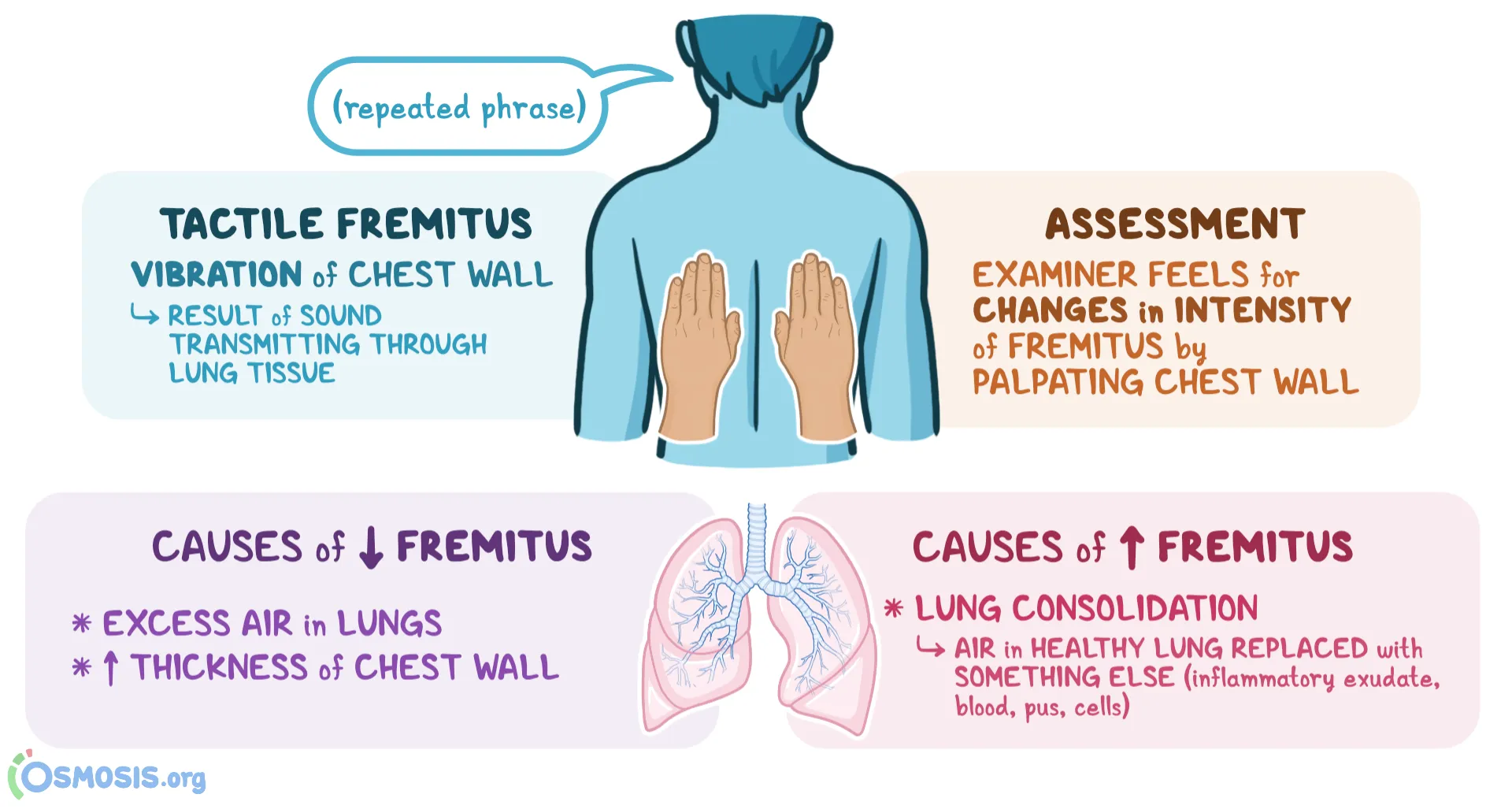
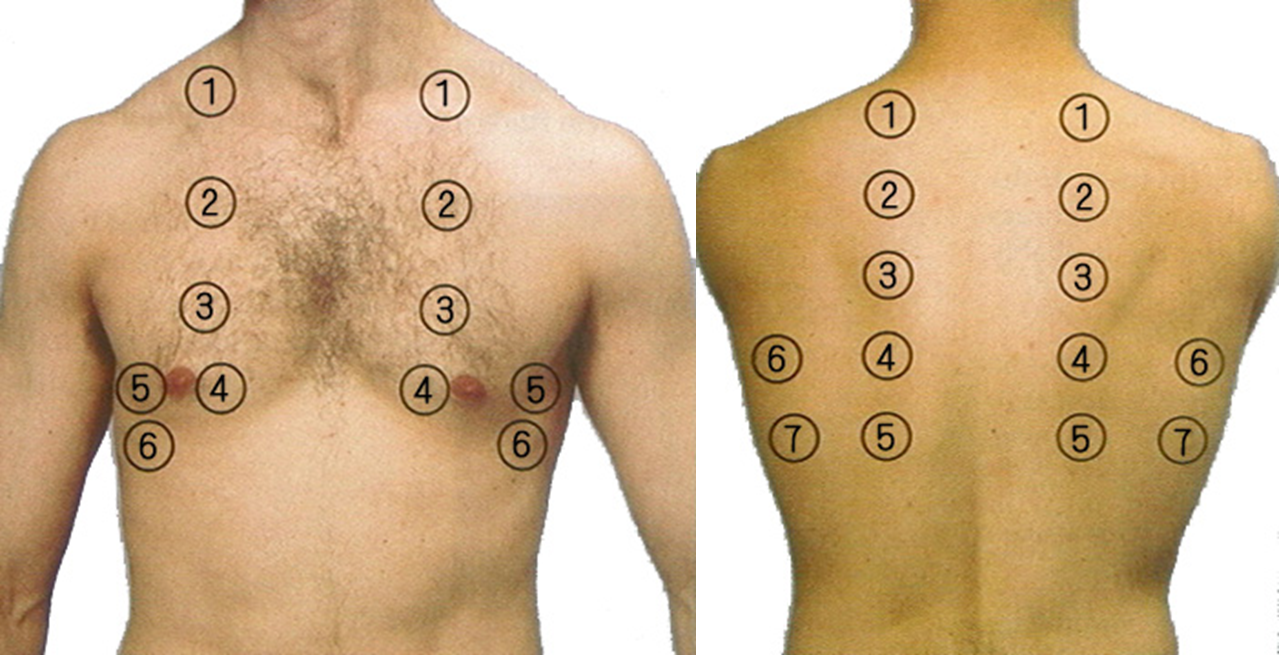
Vocal fremitus (tactile fremitus)
- Ask the patient to say “ninety-nine” several times in a normal voice.
- Palpate using the palm of your hand.
- You should feel the vibrations transmitted through the airways to the lung.
- Increased tactile fremitus suggests consolidation of the underlying lung tissues All three areas front and back
Assessing chest expansion in expiration (left) and inspiration (right).

Percussion:
- hyper ressonance - pneumothorax | Emphysema
- normal - ressonance
- Dullness - pneumonia | atelectasis
- Stony Dullness - Pleural effusion
- Tympany: Cavity or pneumothorax
Mediate
-
Pleximeter: distal inter-phalangeal joint of left middle finger
-
Plexor: right middle fingertip
-
Order: Up to down, anterior to posterior
- Should be done symmetrically and comparing the two sides.
- Supraclavicular area, then clavicles should be percussed directly to evaluate the upper lobes.
-
Liver dullness: of the upper edge starting at the 6th rib MCL, resonant note below this area indicates hyper-inflation (COPD and severe asthma)
-
Cardiac dullness: may be ↓ in hyperinflated chest.
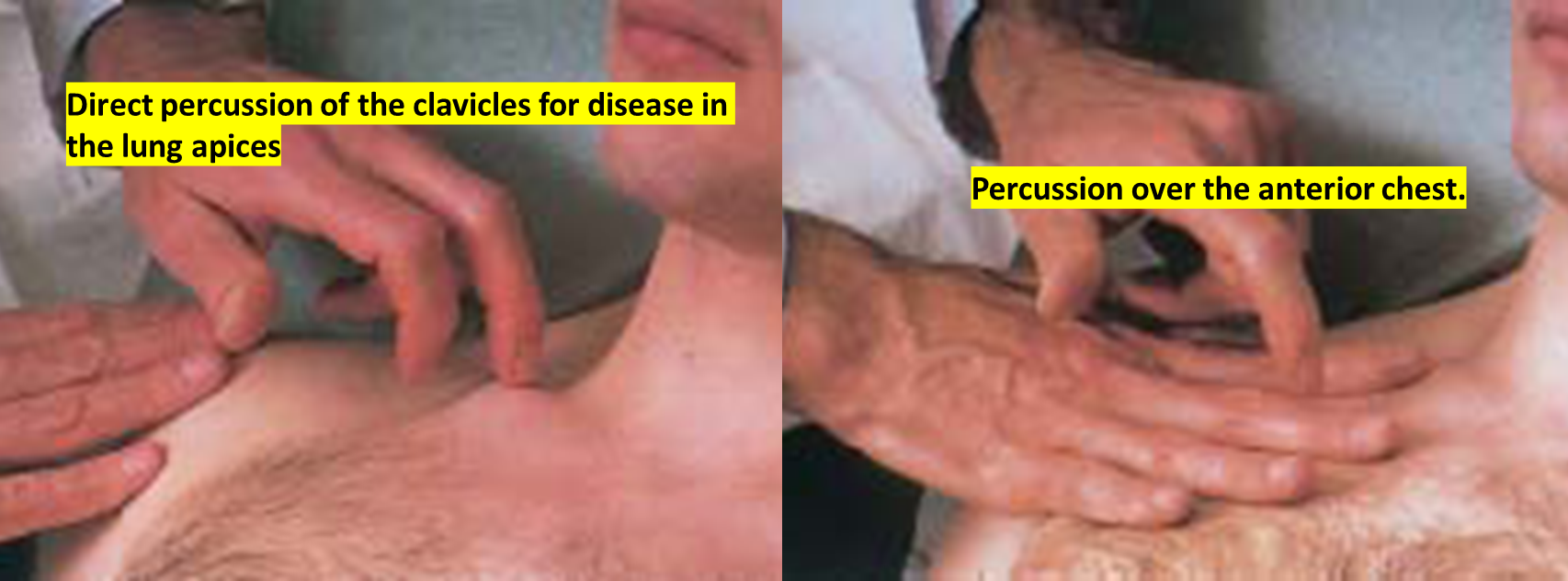
Percussion by - For percussion of the chest, it is usual to use the middle finger of the dominant hand to do this. - The clavicle is percussed directly, usually about a third of the way between the sternum and the acromium.
- The rest of the chest is percussed by placing the non-dominant hand on the chest and using the dominant middle finger to tap the other middle finger over the middle phalanx.
- Percuss over the lobes of the lung, front and back except that the middle lobe
- does not have surface anatomy on the back - Percuss over the heart, in hyperinflation of the chest, there is loss of cardiac dullness. - A hyper-resonant sound suggests hyperinflation or a pneumothorax. - A dull sound is easier to distinguish from normal, it may suggest collapse or consolidation, or a pleural effusion.
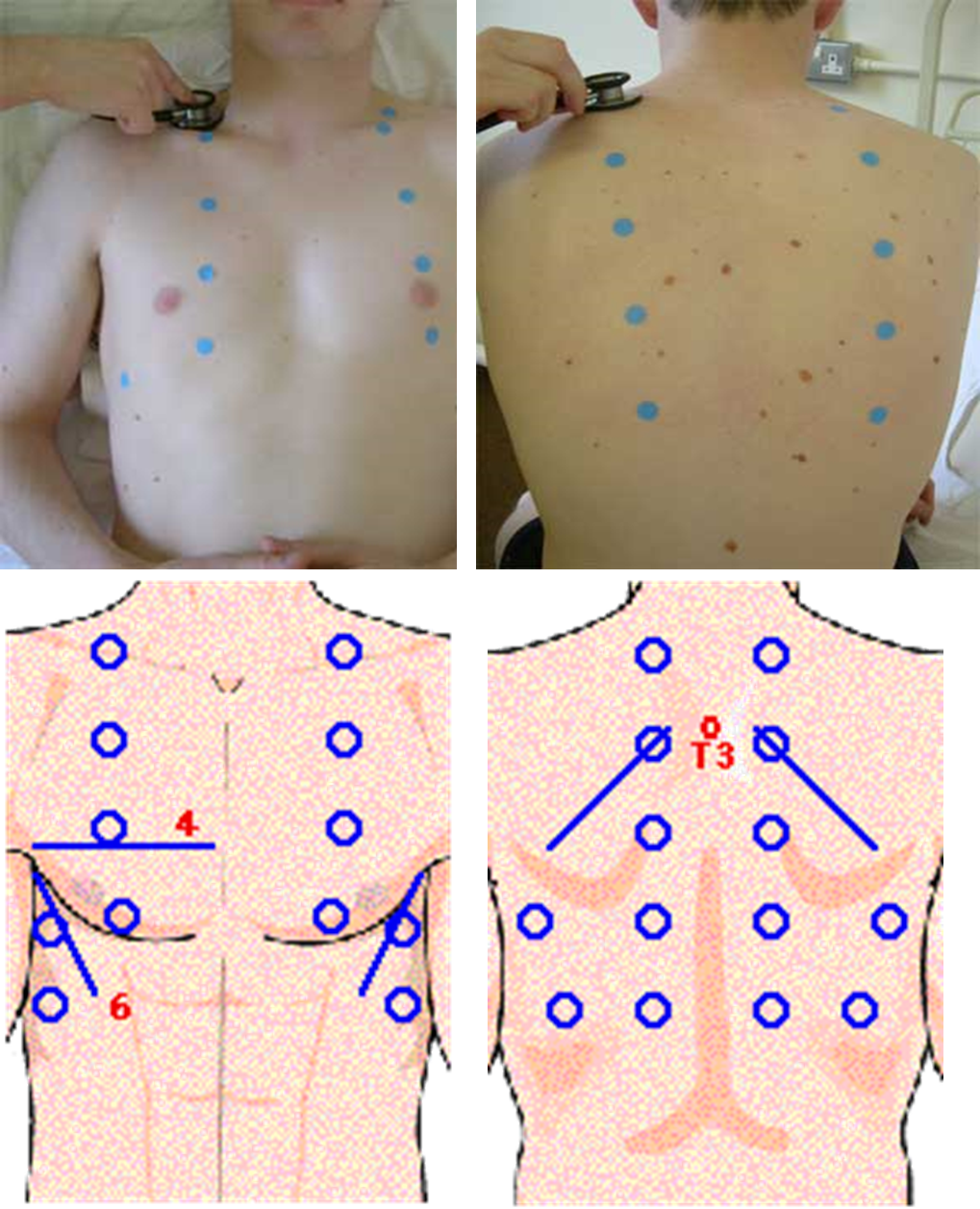
Auscultation:
auscultate back Pleural effusion
-
To assess breath sounds, ask the patient to breathe in and out slowly and deeply through the mouth.
-
Begin at the apex of each lung and zigzag downward between intercostal spaces. Listen with the diaphragm portion of the stethoscope.
-
Heart auscultation is mainly to detect heart abnormalities but severe lung disease may cause pulmonary hypertension and a loud P2
- Place the stethoscope over each of the five lobes of the lungs in turn, on the front and back of the chest. Ask the patient to take deep breaths in and out with their mouth open.
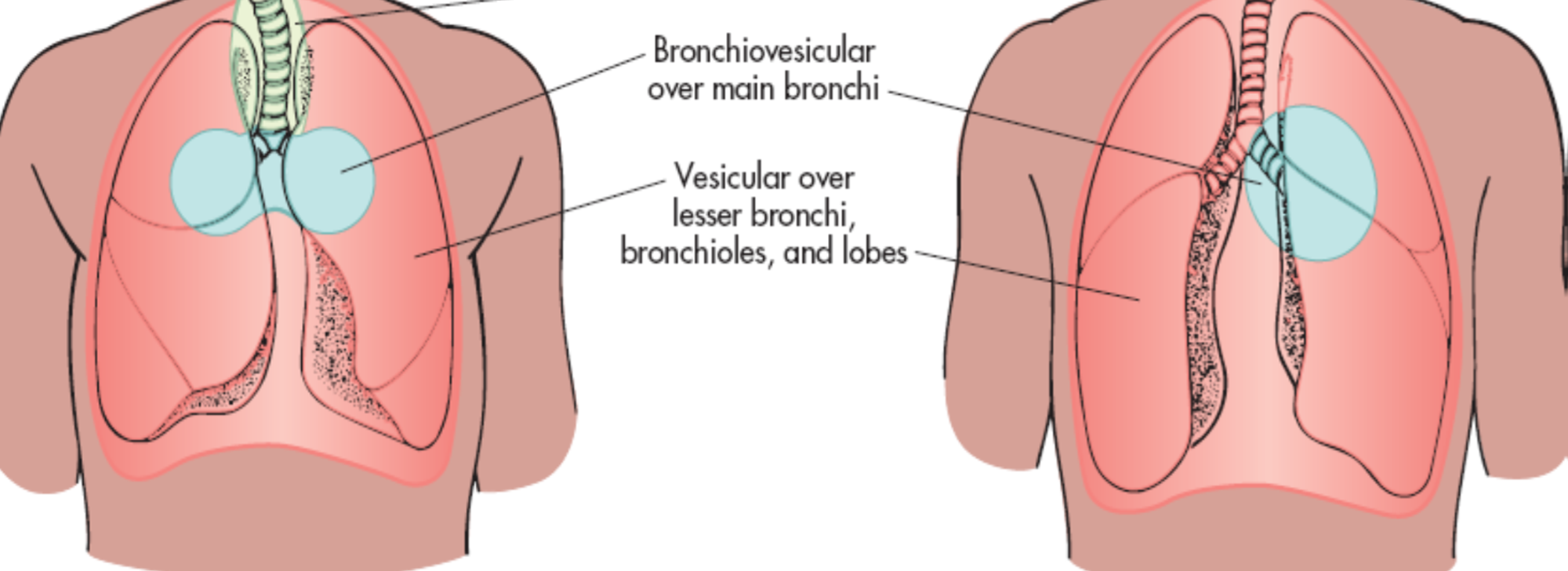
- Normal breath sounds are called vesicular. They are described as quiet and gentle. There is usually no gap between the inspiratory and expiratory phase sounds.
Process
- Using the diaphragm of a stethoscope & comment on the following:
- Breath sounds (BS)
- Intensity: Normal or ↓ as in (consolidation, collapse, pleural effusion, pneumothorax, lung fibrosis)
- Quality: Vesicular or bronchial
- Differentiation between vesicular & bronchial
- Vesicular: louder & longer on inspiration & has no gap between the 2 phases
- Bronchial: louder & longer on expiratory & has a gap between the 2 phases
Order of auscultation
1- Comment on Air Entry
Reduced in lung diseases, pulmonary collapse, pneumothorax
2- Comment on Breath sound
Bronchial:
Heard over the trachea and mainstay bronchi (2nd-4th intercostal spaces either side of the sternum anteriorly and 3rd-6th intercostal spaces along the vertebrae posteriorly). The sounds are described as tubular and harsh. Also known as tracheal breath sounds. 2nd / 3rd intercostal normal continuous
Broncho-vesicular:
Heard over the major bronchi below the clavicles in the upper of the chest anteriorly. Broncho- vesicular sounds heard over the peripheral lung denote pathology. The sounds are described as medium-pitched and continuous throughout inspiration and expiration. Inspiratory high pitch = Low pitch Expiration
Vesicular:
Heard over the peripheral lung. Described as soft and low- pitched. Best heard on inspiration. inspiration long, expiration short
Diminished:
Heard with shallow breathing; normal in obese patients with excessive adipose tissue and during pregnancy. Can also indicate an obstructed airway, partial or total lung collapse, or chronic lung disease.
Abnormal bronchial breath sound (tubular breath sound)
Bronchial breath sound appears in supposed vesicular breath sound area where expiration inspiration are mostly equal
- Consolidation: lobar pneumonia (consolidation stage)
- Large cavity: TB, lung abscess
- Compressed atelectasis: hydrothorax, pneumothorax
Added Sounds
- Stridor - Wheezes: are continuous musical polyphonic sound, heard louder on expiration & can be heard on inspiration which may imply severe airway narrowing. It indicates airway obstruction. - Ronchi
- Crackles: interrupted non-musical inspiratory sound - Crackles may be early, late or pan-inspiratory. - Fine, coarse or medium.
- Pleural Friction Rub
3- Comment Vocal resonance
It’s the ability to transmit sounds.
Ask patients to say 44 (Arabic) or 99 (English)
Bronchophony Consolidation
Pectoriloqny Massive consolidation
Egophony Upper area of hydrothorax
Other Notes
Cesarean; insidence of: asthma, fibrosis, autoimmunity Allergens; asphalt, dust, pollen Chest X-ray; R/O pneumothorax, cavities, effusions etc… Occupational; later presented at work, subsides later.
DM ⇒> Pain = Angina
ASTHMA
Symptom Expiratory dyspnea with wheezing
Signs
- Expiratory dyspnea with wheezing
- Orthopnea
- Cyanosis
- Severe sweat
- Decreased movement of respiration
- Decreased vocal fremitus
- Hyperresonance
- Rhonchi in full fields of lungs
COPD
2L - strong forceful cough - bounding pulse
Risk factors; Vape shisha, passive smoker, driver Consequence: Lung cancer - Sings: cyanosis, tar stain, pulsating, astrexis, wasting small muscles of hand, clubbing, high JVP, distance apple adam for smoker, pulmonary osteodystrophy, tenderness at wrist, tracheal tug
Plan do Hx again with no diagnosis keep patients until symptomps appear
Findings
- Expansion:
- Tactile Fremitus:
- Resonance:
pink puffers???
Pleural Effusion
Sequele of injury includes = secretions = swelling = fibrosis = calcification = coronary calcification
Which is most common on left vs right transudate / exudate?
Signs
- Tachypnea ⇒
- Limited movement of affected side ⇒
- Costal interspaces of affected side are wider ⇒
- Trachea shifts to opposite side ⇒
- Decreased vocal fremitus ⇒
- Stony Dullness ⇒
- Decreased or disappeared vesicular breath sound ⇒
- Pleural friction rub ⇒
- Abnormal bronchial breath sound in upper area of the fluid
Pneumonia
Wants to cough but cant - 6 L
Typical: ? sick, rigor, fever, central trachea, bronchial breathing; sign of consolidation
Atypical: ? TB, Legionella (shower), bullous microplasma (only lung infiltrates) parrots?, selenemous (horse?), toxoplasmosis (cat)
Findings: Tactile fremitus
General signs
- Acute facial features, blushing
- Nares flaring (dyspnea)
- Cyanosis
- Tachycardia
- Simple herpes around lips
Inspection
- Decreased respiratory movement
- Palpation
- Increased vocal resounce
Fibrosis - Scleroderma
- crepitations
- pincher nose?
- waxy skin???
Other notes
NYHA classification for dyspnea
- Class 1 - exercise
- Class 2 - Normal activity
- Class 3 - Slight movement
- Class 4 - At Rest
Cases
C1
80 year old saudi with known case of DM, HTN, Vitilligo presents to hospital with progressive 4D hx of SOB - patient is connected to Oxygen
- Dry hands
- Cyanosed
- 2L O
- Fungal infection on fingernails
- Diabetic nephropathy glove feet
- Loss of hair
- Bronchial breathing + (pleural sound)
- no cough
- no palpitation
- no chest pain
- no phelgm production
- no vomitting
- no diarhhea
O/E
- unilateral chest expansion,
- decreased expansion of chest on left side
- reduced tactile fremitus on right side
- dull on percussion
Investigations
- X-ray; pleural effusion on left lung, fibrosis on right lung CABG, Pacemaker,
C2
Male with pleural effusion, lung cancer taking 3rd dose of chemo