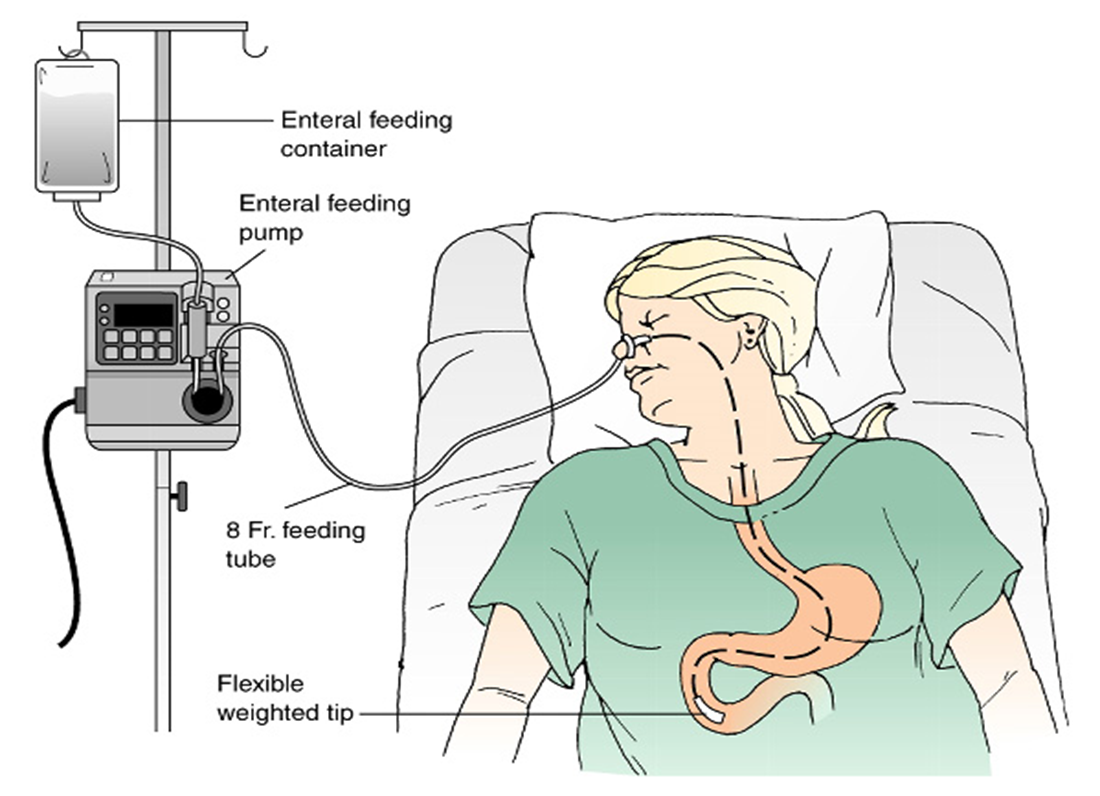
Gastrointestinal intubation is inserting of Polypropylene, Silicone or Latex (rubber) tube into the stomach , duodenum or intestinal
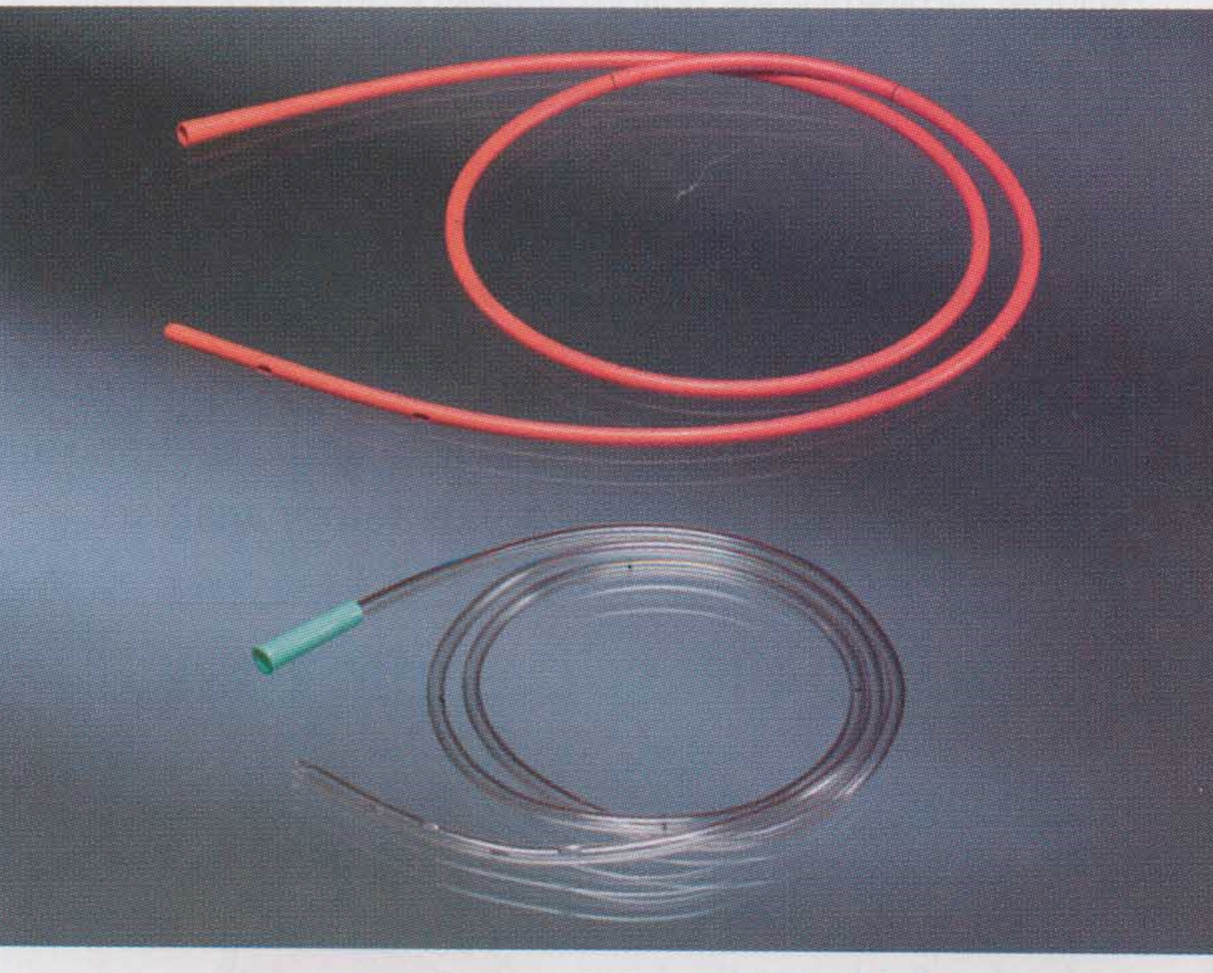
Nasogastric tubes come in various sizes (8, 10, 12, 14, 16 and 18 Fr).
Indications for GI Intubation
- To decompress the stomach and remove gas and fluid
- To lavage the stomach and remove ingested toxins
- To diagnose disorders of GI motility and other disorders
- To administer medications and feedings
- To treat an obstruction
- To compress a bleeding site
- To aspirate gastric contents for analysis
Intubating the patient with an NG tube
-
Assessment:
-
Who needs an NG:
- Surgical patients (bowel obstruction, Ileus, …)
- Ventilated patients
- Neuromuscular impairment .
- Patient with swallowing disorders (post CVA, …)
-
Assess patency of nares.
-
Assess patient medical history:
- Nosebleeds
- Nasal surgery
- Deviated septum
-
Anticoagulation therapy
-
Assess patients’ gag reflex.
-
Assess patient’s mental status.
-
Assess bowel sounds.
Technique
equipment:
-
14 0r 16 Fr NG tube
-
Lubricating jelly
-
PH test strips
-
Tongue blade
-
Flashlight
-
Emesis basin
-
syringe
-
1 inch wide tape or commercial fixation device
-
Suctioning available and ready
-
Explain procedure to client
-
Position the patient in a semi-sitting or high fowlers position. If comatose-semi fowlers.
-
Examine feeding tube for flaws.
-
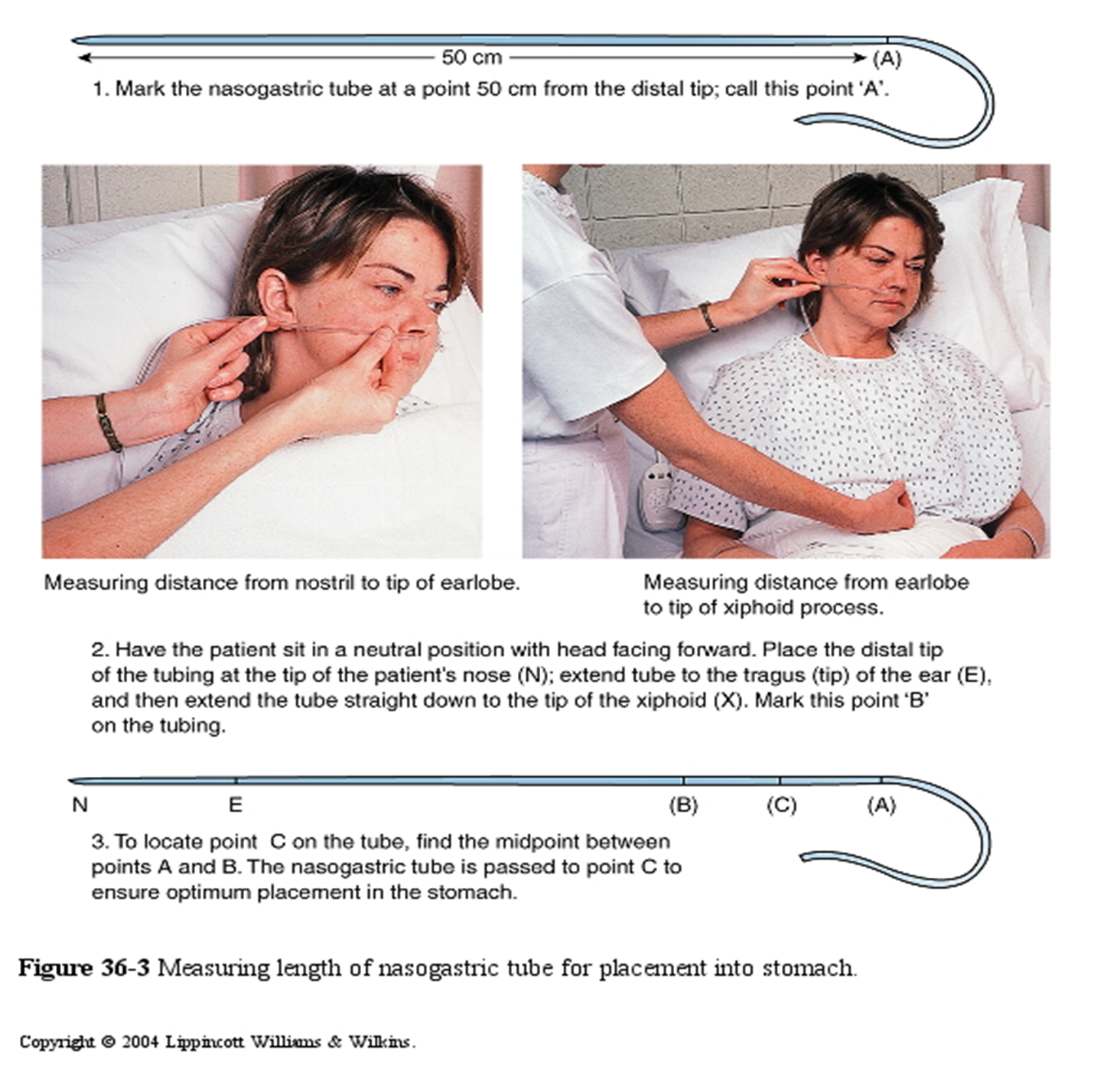
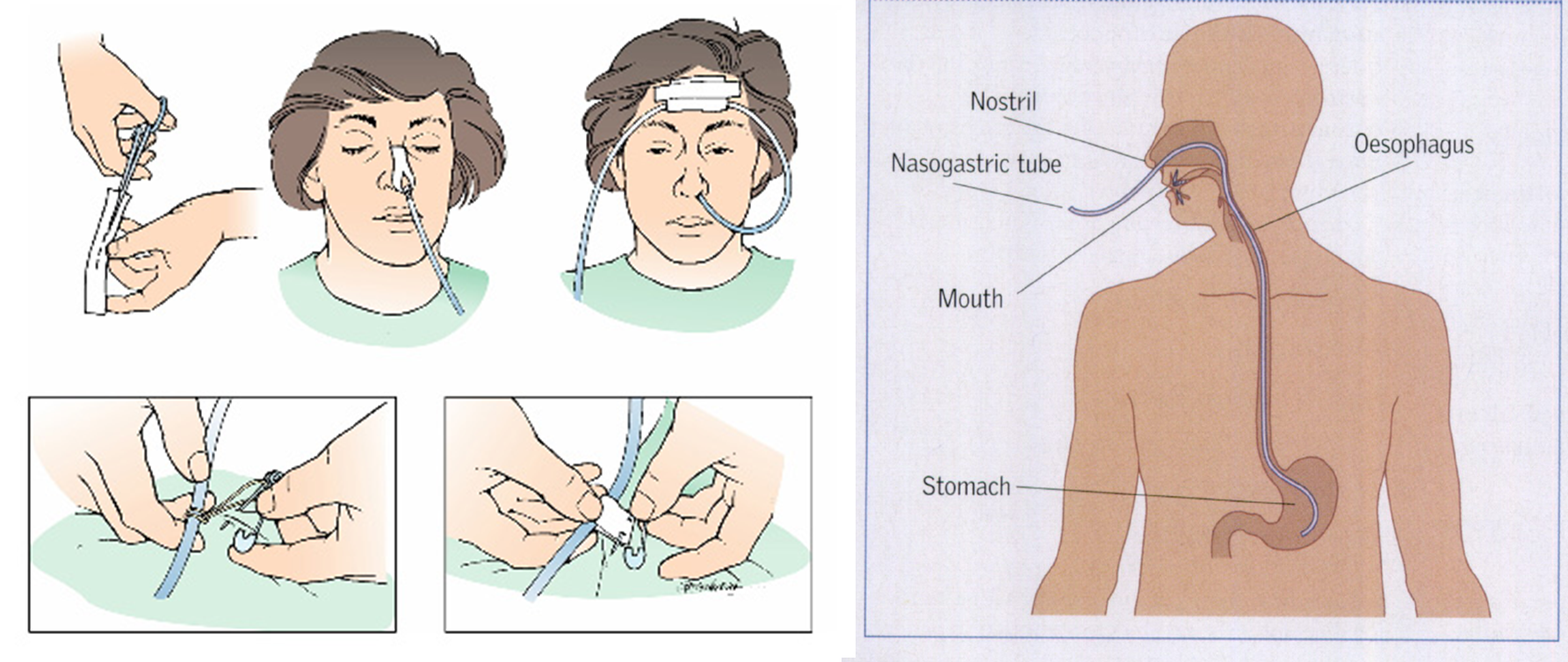
Determine the length of tube to be inserted.
-
Measure distance from the tip of the nose to the earlobe and to the xyphoid process of the sternum.
-
Prepare NG tube for insertion.
Fowler’s Position. Head rest is adjusted to desired height and bed is raised slightly under patient’s knees
Implementation
- Wash Hands
- Put on clean gloves
- Lubricate the tube
- Hand the client a glass of water
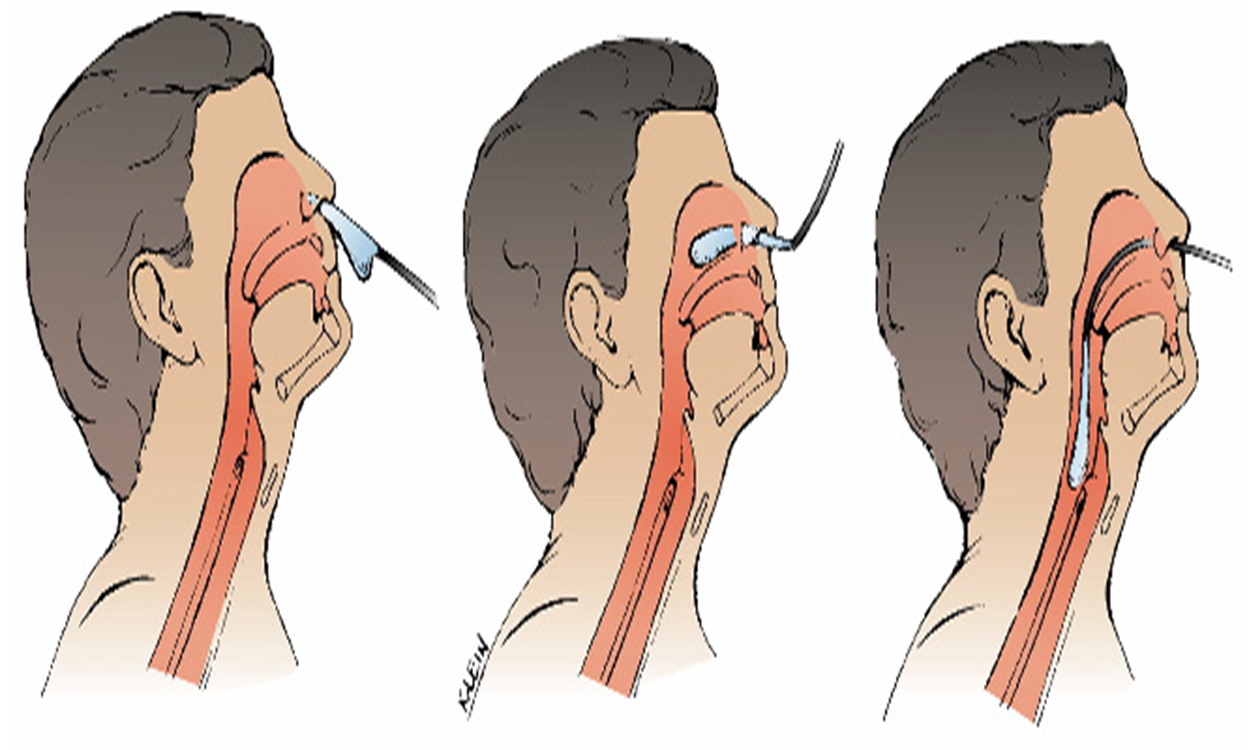
- Gently insert tube through nostril to back of throat (posterior naso pharynx). Have patient flex head toward chest after tube has passed through naso pharynx
-
Emphasize the need to mouth breathe and swallow during the procedure.
-
Swallowing facilitates the passage of the tube through the oropharynx.
-
Advance tube each time client swallows until desired length has been reached.
-
Do not force tube. If resistance is met or client starts to cough, choke or become cyanotic stop advancing the tube and pull back.
-
Check placement of the tube.
- X-ray confirmation
- Testing pH of aspirate
- Secure the tube with tape or commercial device
Evaluation
-
Observe client to determine response to procedure.
-
ALERTS!!! Persistent gagging – prolonged intubation and stimulation of the gag reflex can result in vomiting and aspiration
-
Coughing may indicate presence of tube in the airway.
-
Note location of external site marking on the tube
-
Documentation - Size of tube, which nostril and client’s response. - Record length of tube from the nostril to end of tube - Record aspirate pH and characteristics
Testing Placement (Confirmation)
- Use more than one method when in doubt because all methods of confirmation have some possibility of error
- Radiographic evaluation is the most definitive way
Methods: - Insufflation test: Insufflate air into NG tube and auscultate for rush of air over the stomach - Aspiration of stomach content - PH-tested of aspiration - If patient awake & cooprative, ask the patient to talk, if he/she can not speak, suspect respiratory placement - Chest X-ray.
Complications
- Clogged Tube- most common
- Oral mucosal breakdown
- Nasal irritation/ulceration
- Dumping Syndrome.
- Aspiration during feeding : ensure head of bed is elevated at least 30 degrees while feeds are being administered
- Dehydration- diarrhea is a common problem.
- Electrolyte imbalance: hyperkalemia and hypernatremia
- Gastric mucosa ulceration