Preterm Labor
Objective:
- Definition and Diagnosis
- Incidence
- Risk factor
- Management
- Prevention
Definition:
Delivery after 20 week and before 37 week
Criteria of Diagnosis:
With ruptured or intact membranes
- Documented uterine contractions (4 per 20 minutes or 8 per 60 minutes)
- Documented cervical change (cervical effacement of 80% or cervical dilation of 2 cm or more)
Incidence:
In the United States, approximately 12% of all live births occur before term. Preterm births account for approximately 70% of neonatal deaths and 36% of infant deaths as well as 25–50% of cases of long-term neurological impairment in children.
In SA, an overall preterm birth prevalence of 7.89 per 100 live births.
Risk Factors
Maternal Causes
- Prior preterm birth.
- Bacterial infection (cervical, vaginal, Urinary).
- Medical disease (DM, HTN, obesity).
- Black race.
- Stress.
- Lack of prenatal care.
- Smoking
Uterine Causes
- Uterine overdistention (multiple gestation, polyhydramnios)
- Uterine anomalies.
- Placental abruption.
- Cervical insufficiency
- PPROM
- IUGR
Proposed Mechanisms of Disease
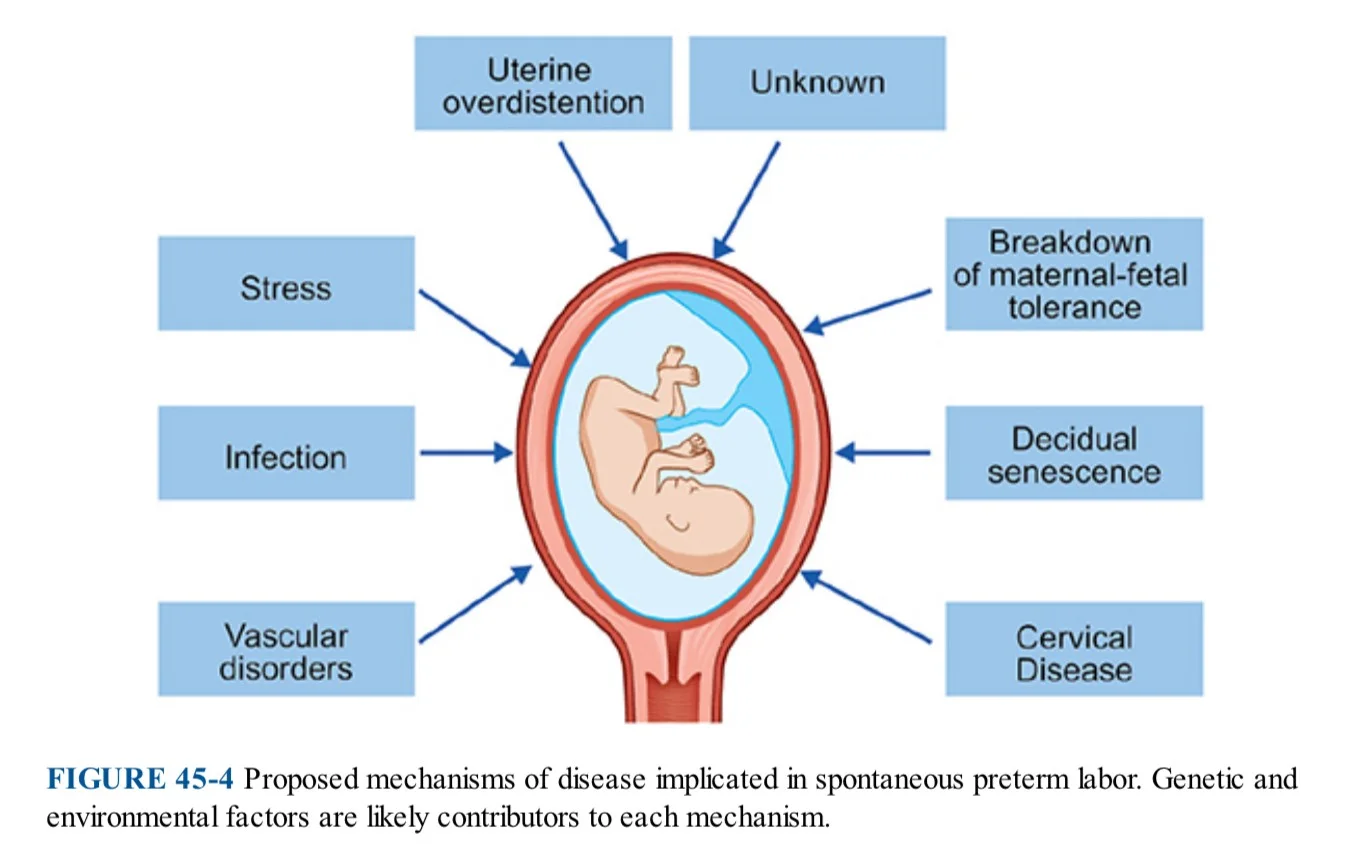
PRIMARY CAUSES OF PRETERM BIRTH AND THEIR ESTIMATED FREQUENCY
| Cause | Frequency (%) |
|---|---|
| Spontaneous preterm labor | 35-37 |
| Multiple gestations* | 12-15 |
| Preterm premature rupture of membranes (PPROM) | 12-15 |
| Late preterm births | 50-70 |
| Pregnancy-associated hypertension | 12-14 |
| Cervical incompetence/uterine anomalies | 12-14 |
| Antepartum hemorrhage | 5-6 |
| Intrauterine growth restriction (IUGR) | 4-6 |
*Increased proportion because of advancing maternal age and assisted reproductive technologies (ARTs). ART has increased the incidence of twinning by 50% with a very recent decline due to more elective single embryo transfers.
Management
Case Study
A 27-year-old lady, G3P2+0 at 34 weeks GA, unsure about her LMP, came to ER Z complaining of abdominal pain and vaginal discharge. No follow-up in the clinic. 2xSVD, medically and surgically free.
Physical Examination
- Vital signs: HR 115 bpm, BP 120/85, O2 sat 99% on room air, Temp: 37°C
- Abdominal and pelvic examination: Fully dilated, vertex zero station
After 30 minutes, the patient delivered NSVD with an intact perineum. Outcome: baby girl, weight 1650 gm, admitted to NICU due to respiratory distress. Mother stable, admitted to postnatal.
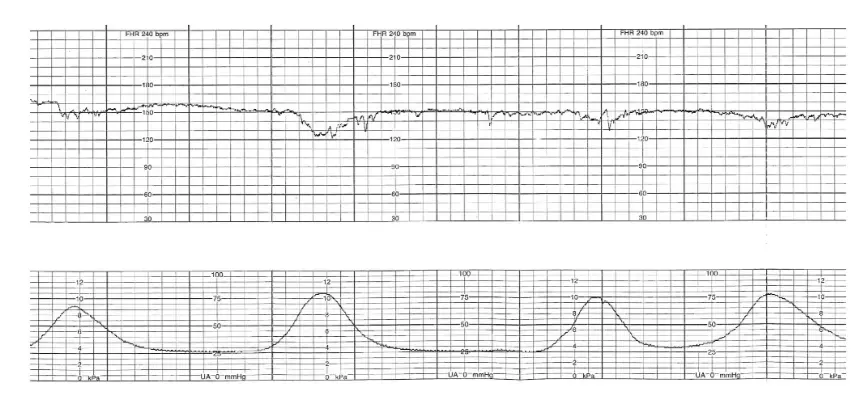 4 contractions in 20 min
4 contractions in 20 min
Treatment
Hydration
With adequate hydration and bed rest, uterine contractions cease in approximately 20% of patients.
Antibiotic
For patients who are not allergic to penicillin, a 7-day course of ampicillin and erythromycin may be given. Those allergic to penicillin may be given clindamycin.
Corticosteroid
-
Treatment consists of 2 doses of 12 mg of betamethasone, given intramuscularly 12 hours apart,
-
or 4 doses of 6 mg of dexamethasone given intramuscularly 12 hours apart.
- lung maturity CC
- ARDS?
- IPH?IBH>IVH
- NEC>
Tocolytic Agents
- Calcium channel blocker (nifedipine)
- Beta agonist (terbutaline)
- Magnesium sulphate (1-preterm labor, 2- 3- prevent cerebral an. esp if. <32wk not >32)
- NSAID (indomethacin)
- Oxytocin antagonist (atosiban)
Mainly for dex
Contraindications to Tocolysis
- Intrauterine fetal demise
- Lethal fetal anomaly
- Nonreassuring fetal status
- Severe preeclampsia or eclampsia
- Maternal bleeding with hemodynamic instability
- Chorioamnionitis
- Maternal contraindications to tocolysis (agent specific)
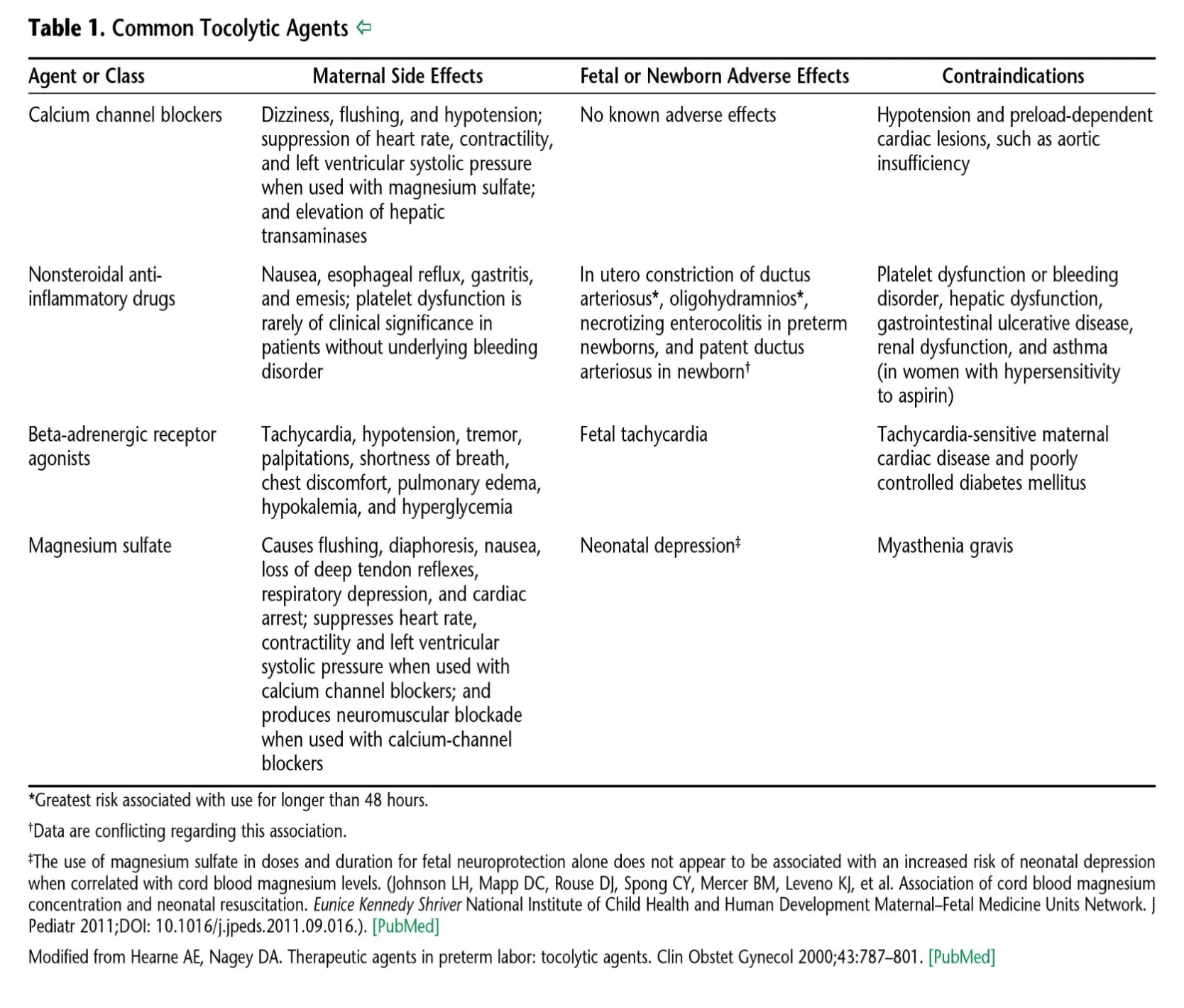
Common Tocolytic Agents
| Agent or Class | Maternal Side Effects | Fetal or Newborn Adverse Effects | Contraindications Z |
|---|---|---|---|
| Calcium channel blockers | Dizziness, flushing, and hypotension; suppression of heart rate, contractility, and left ventricular systolic pressure when used with magnesium sulfate; and elevation of hepatic transaminases | No known adverse effects | Hypotension and preload-dependent cardiac lesions, such as aortic insufficiency |
| Nonsteroidal anti-inflammatory drugs | Nausea, esophageal reflux, gastritis, and emesis; platelet dysfunction is rarely of clinical significance in patients without underlying bleeding disorder | In utero constriction of ductus arteriosus*, oligohydramnios*, necrotizing enterocolitis in preterm newborns, and patent ductus arteriosus in newborn† | Hepatic issues, asthma Platelet dysfunction or bleeding disorder, hepatic dysfunction, gastrointestinal ulcerative disease, renal dysfunction, and asthma (in women with hypersensitivity to aspirin) |
| Beta-adrenergic receptor agonists | Tachycardia, hypotension, tremor, palpitations, shortness of breath, chest discomfort, pulmonary edema, hypokalemia, and hyperglycemia | Fetal tachycardia | Tachycardia-sensitive maternal cardiac disease and poorly controlled diabetes mellitus |
| Magnesium sulfate | Causes flushing, diaphoresis, nausea, loss of deep tendon reflexes, respiratory depression, and cardiac arrest; suppresses heart rate, contractility and left ventricular systolic pressure when used with calcium channel blockers; and produces neuromuscular blockade when used with calcium-channel blockers | Neonatal depression‡ | Myasthenia gravis |
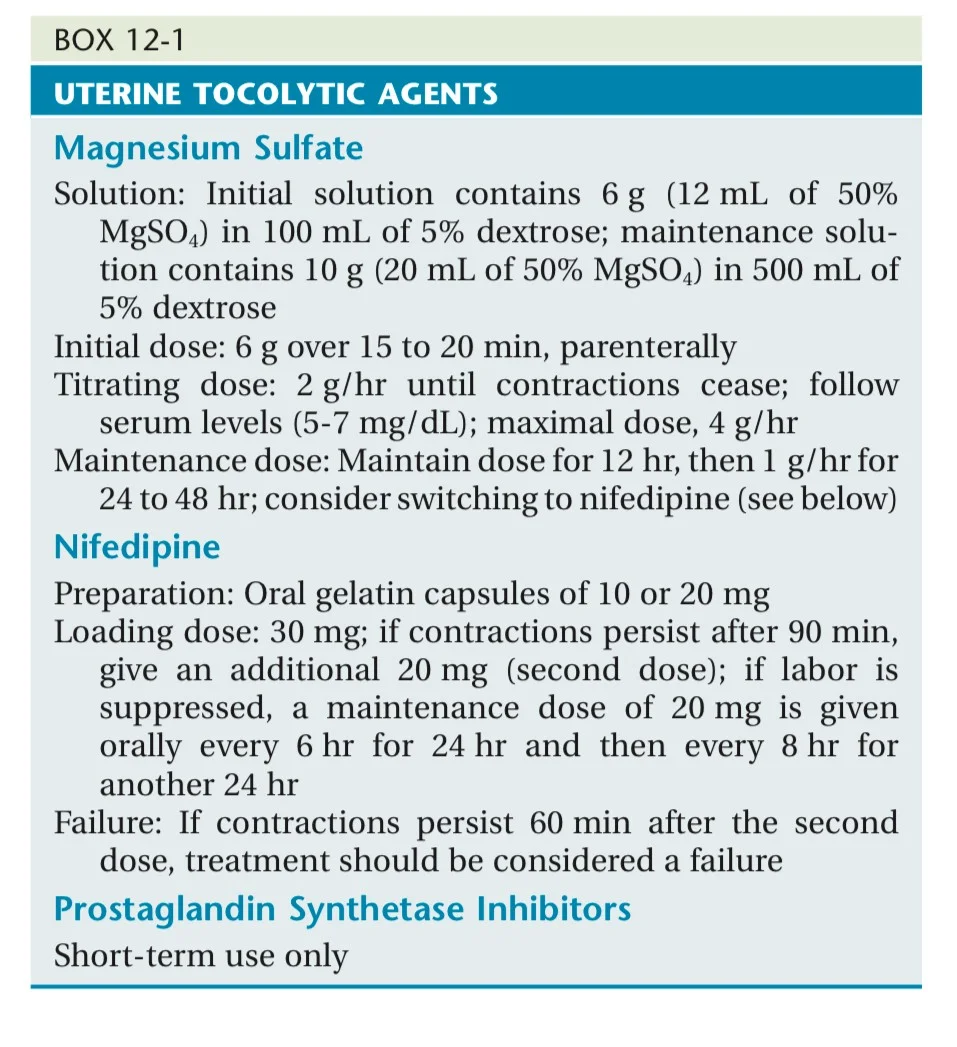
Uterine Tocolytic Agents
Magnesium Sulfate
Solution: Initial solution contains 6 g (12 mL of 50% MgSO4) in 100 mL of 5% dextrose; maintenance solution contains 10 g (20 mL of 50% MgSO4) in 500 mL of 5% dextrose
- Initial dose: 6 g over 15 to 20 min, parenterally
- Titrating dose: 2 g/hr until contractions cease; follow serum levels (5-7 mg/dL); maximal dose, 4 g/hr
- Maintenance dose: Maintain dose for 12 hr, then 1 g/hr for 24 to 48 hr; consider switching to nifedipine
Nifedipine
Preparation: Oral gelatin capsules of 10 or 20 mg
- Loading dose: 30 mg; if contractions persist after 90 min, give an additional 20 mg (second dose); if labor is suppressed, a maintenance dose of 20 mg is given orally every 6 hr for 24 hr and then every 8 hr for another 24 hr
- Failure: If contractions persist 60 min after the second dose, treatment should be considered a failure
Prostaglandin Synthetase Inhibitors
Short-term use only
Labor and Delivery of Preterm Infant
-
Delivery at tertiary Hospital, NICU available
-
The lower limit of potential viability is 24 weeks or 500 g, although the limits vary with the expertise of the neonatal intensive care unit.
-
Continuous fetal heart monitoring and prompt attention to abnormal fetal heart rate patterns are extremely important
Delivery Considerations
-
Vertex presentation vaginal delivery is preferred.
-
For the breech fetus estimated at less than 1500 g Z, neonatal outcome is improved by cesarean delivery.
Complications
- Hypothermia
- Respiratory: (RDS, apnea of prematurity, BPD)
- Cardiac: PDA, shock, low BP
- IVH
- NEC
- Bacterial and fungal infection
- Anemia of prematurity.
- Retinopathy of prematurity
Prevention
- Serial cervical length measurement at 16-24 weeks.
- 17-OH progesterone.
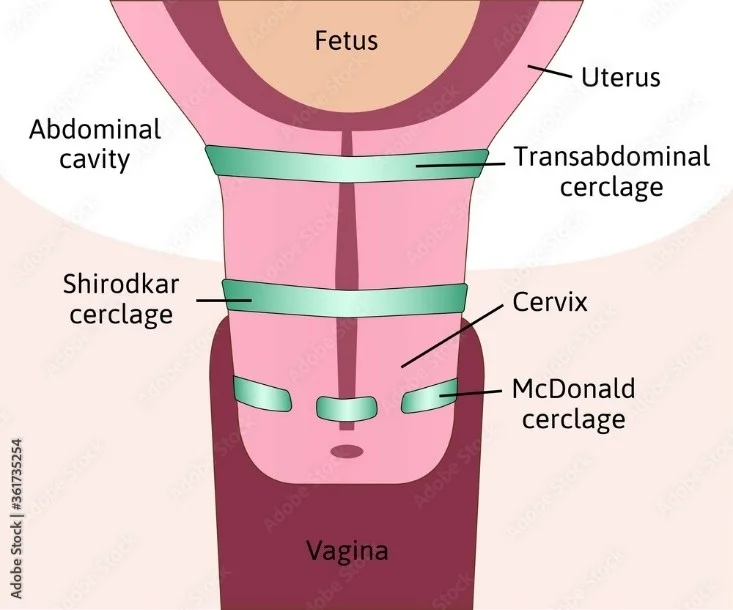
- Cervical cerclage.
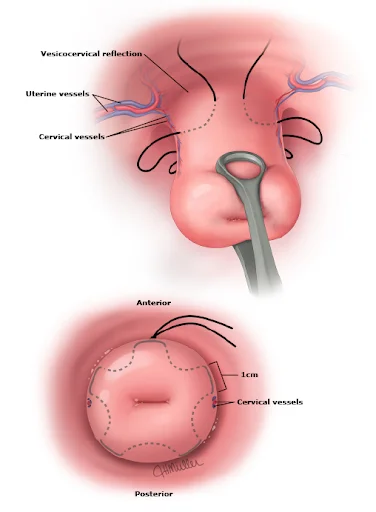
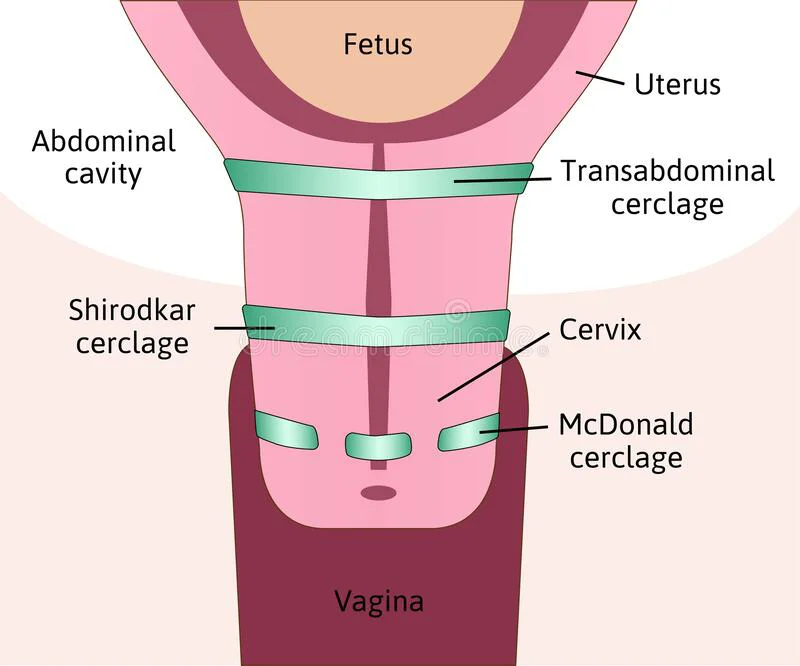
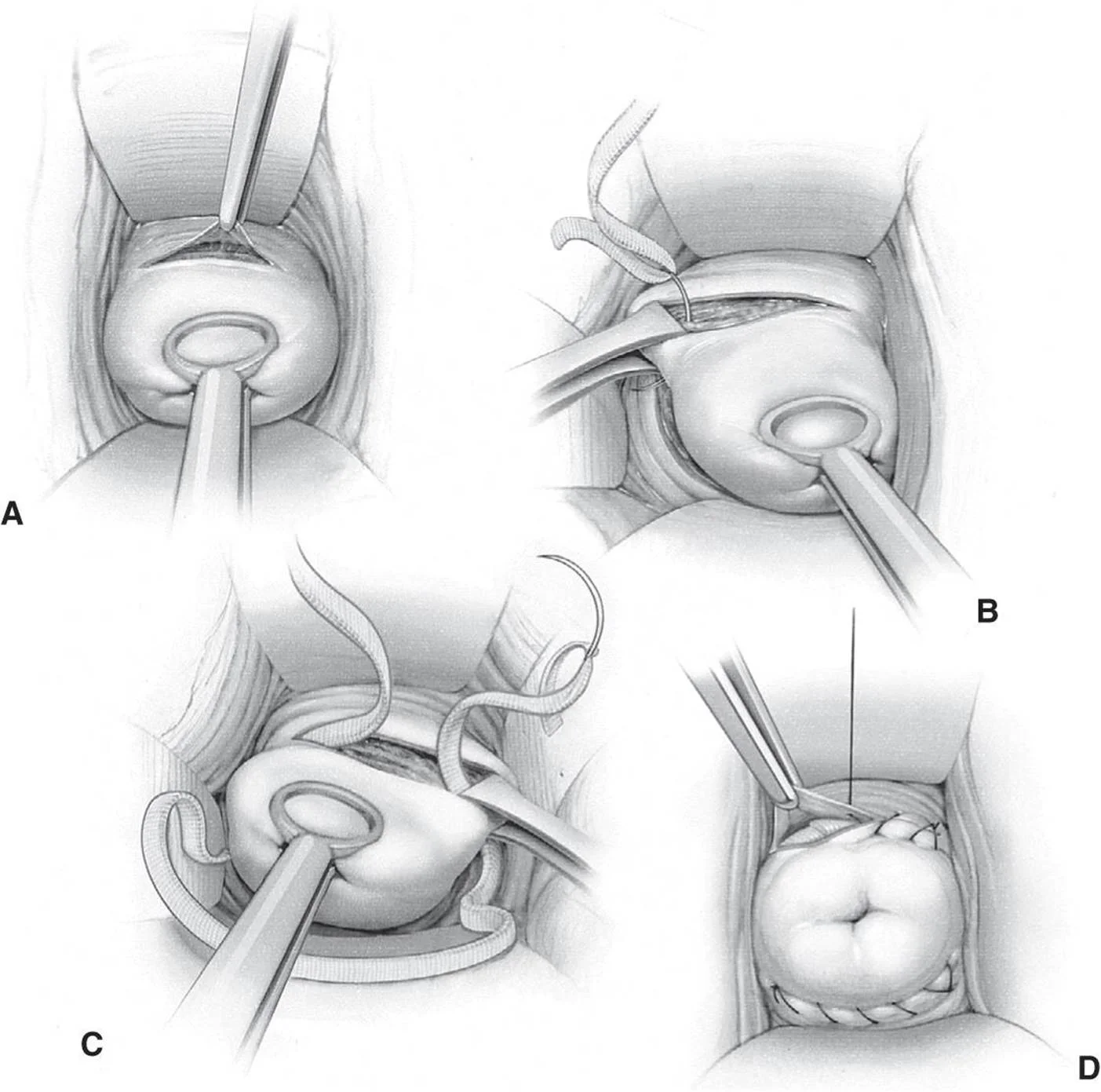
Cervical Cerclage Diagram
Case Scenarios
Scenario 1
A 24-year-old G1P0 patient at 26 weeks’ gestation presents for a routine obstetric (OB) visit. She has had regular prenatal care, and her pregnancy has been uncomplicated. Her fundal height measures 40 cm, prompting an ultrasound which demonstrates polyhydramnios. How should the patient be counseled about the risks of this condition?
Answer
A: She has an increased risk of preterm delivery.
Scenario 2
A 30-year-old G1P0 patient with a twin pregnancy at 28 weeks’ gestation presents to labor and delivery with light vaginal bleeding and uterine contractions. She does not report leaking fluid. A bedside ultrasound examination demonstrates normal amniotic fluid and anterior placentas and no evidence of placenta previa. The fetal heart rate tracing is Category I for both twins, and external monitor shows uterine contractions every 2 to 3 minutes. Examination demonstrates that the cervix is 2 cm dilated and 50% effaced, and the presenting part is at -3 station. Tocolysis with magnesium sulfate is initiated and intravenous antibiotics are started for group B streptococcus (GBS) prophylaxis. Betamethasone, a corticosteroid, is also administered. How should this patient be counseled about the benefits of betamethasone in this situation?
Answer
C: Betamethasone promotes fetal lung maturity and decreases the risk of respiratory distress syndrome.
Preterm Labor
DR. ROUA ALI

Definition
Preterm labor (PTL) is defined as the onset of labor after viability i.e., 24 weeks, and before 37 completed weeks of pregnancy.
Risk Factors
1. Maternal Risk Factors:
- Maternal age <18 years or >40 years.
- Preterm premature rupture of the membranes
- Maternal complications (medical or obstetric).
- Lack of prenatal care.
2. Uterine Causes:
- Myomata (particularly submucosal)
- Uterine septum.
- Bicornuate uterus.
- Cervical incompetence
- Multiple gestation
- Polyhydroamnios
3. Placental Causes:
- Abnormal placentation
4. Infectious Factors:
- Genital:
- Bacterial vaginosis, Chlamydia, GBS, Mycoplasmas
- Intra-uterine:
- Ascending (from genital tract)
- Transplacental (blood-borne)
- Extra-uterine:
- Pyelonephritis.
- Malaria.
- Typhoid fever.
- Pneumonia
- Listeria.
- Asymptomatic bacteriuria
Pathogenesis
Diagnosis
- Regular uterine contractions with or without pain (at least 4 in every 20 min or 8 in 60 min).
- Dilatation (> 2 cm) and effacement (80%) of cervix.
- Pelvic pressure and backpain
Length of cervix (measured by TVS) < 2.5 cm and funneling of internal os. TVS should be done and cervical length measured. Besides this fetal fibronectin.

Management
Tocolytics:
- Prostaglandin synthetase inhibitors (indomethacin, sulindac)
- Calcium channel blocker (nifedipine)
- Oxytocin antagonist, i.e., atosiban
- Diazoxide
- Magnesium sulfate
- Nitric oxide donor (glyceryltrinitrate)
- Betamimetics (ritodrine, terbutaline, salbutamol and isoxsuprine HCl)
Other Management Strategies:
- Dexamethasone
- Progesterone
- Rescue cerclage
- Cervical pessary

Prevention
Cerclage
- McDonald cerclage - vaginal delivery, removed at 35 week
- Shirodkar cerclage - C/S
- Transabdominal cerclage - C/S