CVS
Congestive Heart Failure Coronary Artery Diseases Acute Coronary Syndrome Aortic Valvular Heart Diseases
History
- Patient’s demographic data:
- Age: Coronary artery disease & peripheralvascular disease more common in old people
- Nationality
- Occupation: Ask if sitting or physical exertion at work. Any stress at work? (Physical exertion precipitates angina. Stress also can worsen angina)
- Housing: Ground floor or above (climbing stairs precipitates angina)
COMMON CVS DISEASES
- Coronary artery disease (angina, Myocardial infarction)
- Congestive heart failure
- Arrhythmias (atrial fibrillation)
- Pericarditis
- Endocarditis
- Peripheral vascular disease
S/S Cardio vascular diseases can present with the following:
- History of Chest Pain (coronary artery disease, pericarditis sometimes arrhythmias)
- Dizziness/ Syncope (heart failure, aortic valve diseases, Hypotension, Ischemic Heart Disease)
- Dyspnea (angina/MI, heart failure)
- Palpitations’ due rapid HR (angina, MI, arrhythmias, hypertension)
- Fatigue (heart failure)
- Orthopnea: *Supine position produces dyspnea. Occurs in HF
- Nausea/sweating (anginal attack, MI)
- Claudication: peripheral vascular disease
- Fever Occurs in endocarditis (infection of the heart valves)
SUMMARY OF FEATURES
- Angina/MI:
- Causes chest pain - Usually in adults
- Pain may radiate to the neck, jaw, left arm
- Risk factors are: fam. Hist, smoking, DM, HTN high cholesterol
- Precipitated by exertion, relieved by rest
- Sharp, pressure like
- Pain comes and goes in angina
- Often associated with sweating, palpitations, nausea, dizziness
- Pericarditis:
- Pain not very severe * Persistent
- Worse while supine, better by leaning
- No radiation * Occurs gradually
- Pricking pain
-
Valve problems: Can lead to dizziness, syncope, palpitations, dyspnea
-
Hypertension: Can be asymptomatic or produce headache, general body pain, dizziness
-
Heart failure:
- No chest pain
- dyspnea
- fatigue
- Orthopnea
- Pedal edema
-
Arrhythmias: Produce palpitations, dizziness, syncope, can be asymptomatic
-
Peripheral vascular disease: pain on walking
-
Endocarditis: No chest pain. Fever present
Presenting complaint (PC)
- •Chest pain
- •Breathlessness (dyspnoea)
- •Palpitation
- •Dizziness
- •Blackouts (syncope)
- •Lower limb swelling
- •Intermittent claudication
History of presenting complaint (HPC) As with any pain history, the mnemonic SOCRATES can help develop your differential diagnosis:
- Site: where exactly is the pain?
- Onset and progression: when did the pain start and how has it changed or evolved?
- Character: what type of pain is it (dull, sharp, or crushing)?
- Radiation: does the pain move anywhere (into the jaw, arm, or back)?
- Associated S&S: ask about sweating, N and V, SOB, cough, haemoptysis, dizziness, & palpitations
- Timing and duration: does the pain occur at particular times of the day? How long does each episode last?
- Exacerbating and alleviating factors: what make the pain better or worse (exercise, movement, deep breathing, coughing, cold air, large or spicy meals, alcohol, rest, GTN, sitting up in bed)?
- Severity: “How would you rate the pain on a scale of 1 to 10, & effect on everyday life.
Past medical history (PMH)
- Current, past, and childhood illnesses.
- Stroke or transient ischaemic attack (TIA),
- Renal impairment,
- rheumatic fever, heart murmur
- Peripheral vascular disease
- Systemic disorders (pericarditis and Raynaud’s
- Marfan’s syndrome (aortic dissection)
- myotonic dystrophy (atrioventricular block).
- Operations, hospital clinic attendances
Social history
- Effect of the chest pain on the patient’s life:
- Employment.
- Housing.
- Hobbies.
- Smoking
- Alcohol
- Recreational drugs such as cocaine and amphetamines
General Examination
- Chest shape
- Shortness of breath (@ rest or walking)
- Sitting upright? Able to speak?
- Visible impulse on chest wall from vigorously contracting ventricle (rare)
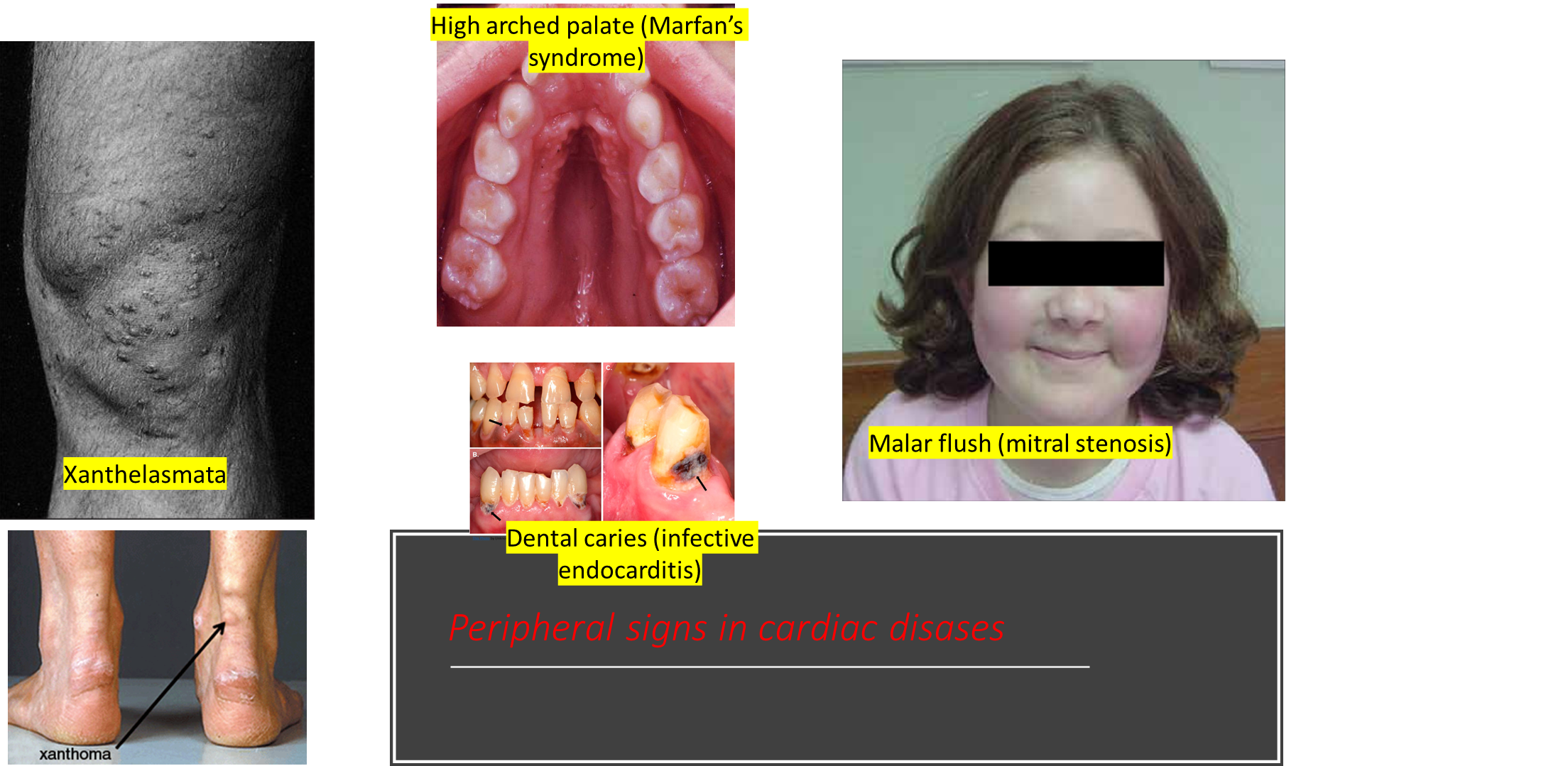
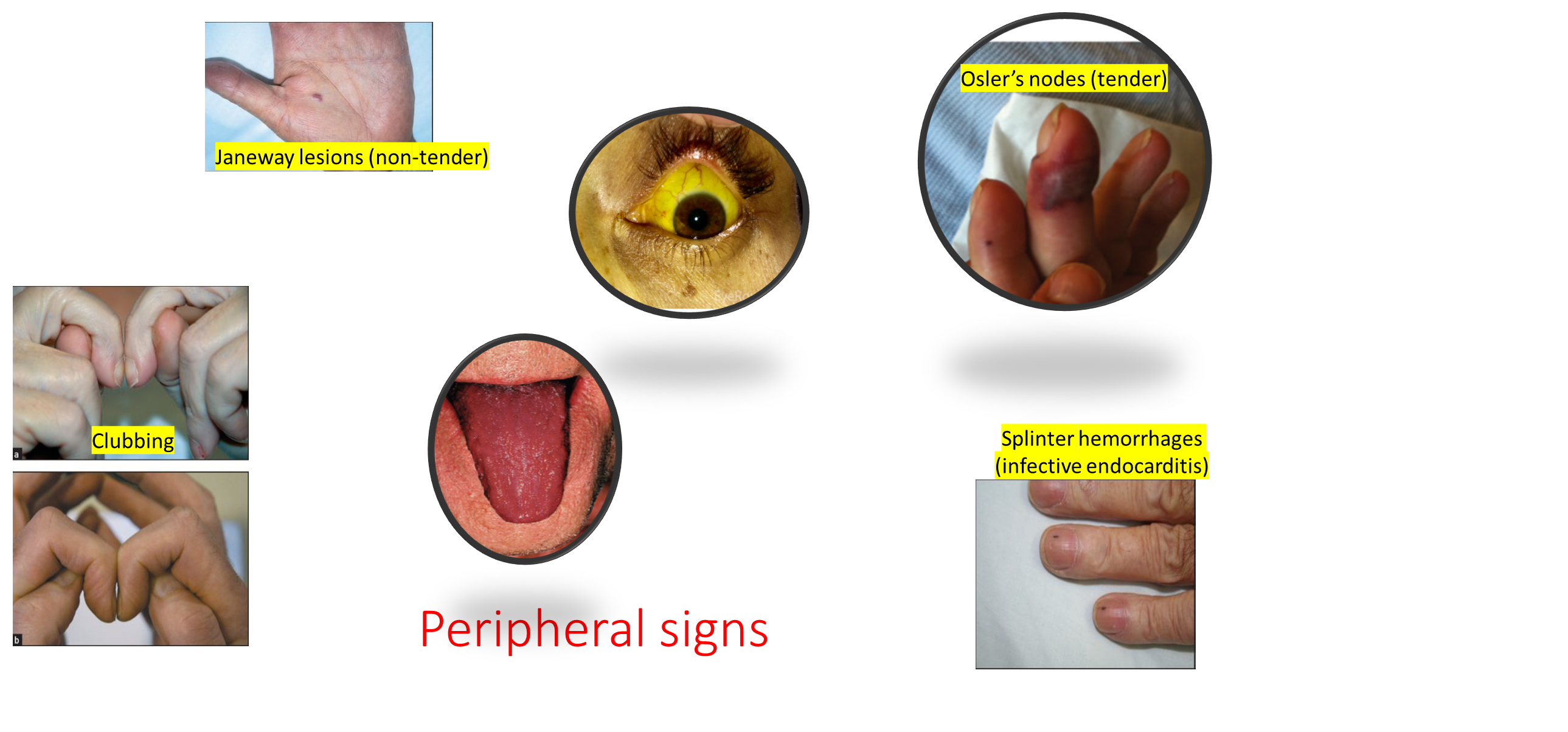
- Hands - Temperature, peripheral cyanosis, splinter haemorrhages, tar staining, xanthomata
- Radial pulse - Rate, rhythm, collapsing
- Arm - Blood pressure, brachial pulse waveform
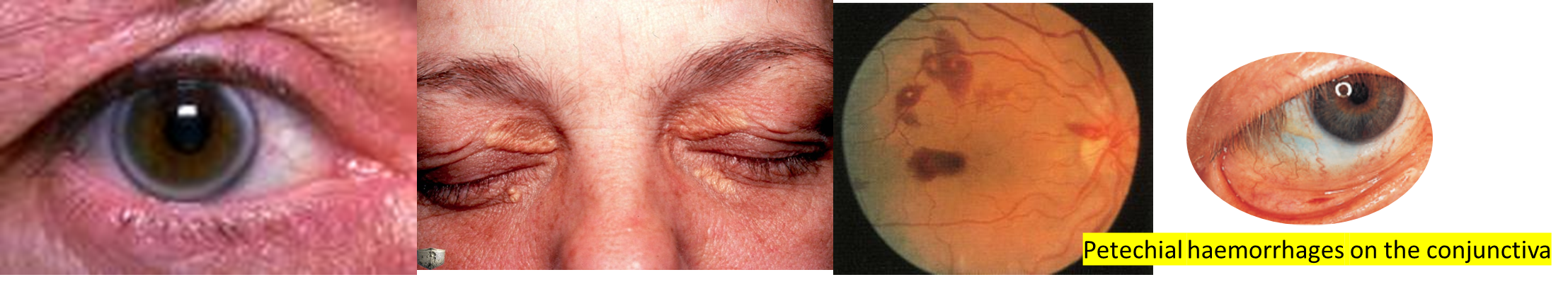
- Eyes - Arcus, xanthelasma, anaemia
- Face - Malar flush
- Lips and tongue - Central cyanosis
- Neck - JVP, carotid pulse
- Chest-Inspection - Scars, pulsations Palpation - Apex, thrils, heaves-Auscultation - Heart sounds, added sounds, murmurs, carotid bruits, basal crepitations
Examination
Inspection:
To check Respiration/Pulse time in Resp 30s & cardio 15s
Upper Limb
- Splinter Haemorrhage; hard labour, Infective endocarditis
- Peripheral Cyanosis- Tetralogy of Fallot, VSD, ASD (VSD & ASD complicated with ezinminger syndrome, Tetralogy of Fallot)
- Clubbing - may be complicated by Tetralogy of fallot
- Osler Nodules; painful
- Janeway lesion; painless
- Arachnodactyly - Marfan's syndrome relation to regurgitation of aorta
- Aortic reaggregation; check axilla for Ehlers-Danlos syndrome (EDS) - elastic falling down from axilla
Clubbing grading 1-4
-
Fluctuation Test (Grade 1) - Press down on the nail and observe the opposite side for fluctuation, which indicates increased sponginess of the nail bed.
-
Window Test (Grade 2) - By placing the nails of the same fingers against each other, a small diamond-shaped window appears if there is no clubbing. The absence or reduction of this window indicates the presence of clubbing.
-
Increased Anteroposterior Curvature (Grade 3) - The nails show increased curvature both longitudinally and transversely, which is more pronounced and visible.
-
Drumstick Appearance (Grade 4) - The terminal phalanges of the fingers enlarge, and the nails curve around the fingertips, resembling drumsticks.
Face & Neck
- Jaundice could happen due RHF
- Malar flush (Mitral Stenosis)
- Lips and tongue - Central cyanosis
- Dental Caries (Infective Endocarditis)
- High Arched Palate (Marfan’s Syndrome)
- Neck - JVP, carotid pulse
- Thoracicectomy scars
- Down Syndrome
- Obesity, Cachexia
- Eyes; Exomphalos, XANTHELASMATA, CORNEAL ARCUS, Roth spot, Petechial Haemorrhage on the conjunctiva, Jaundice
JVP
- 45 degrees - don’t touch the patient
- Tell patient to look away from your side to his left
- Between two heads of sternocleidomastoid, and arise till lobe of the ear
- 2-3cm then its normal JVP
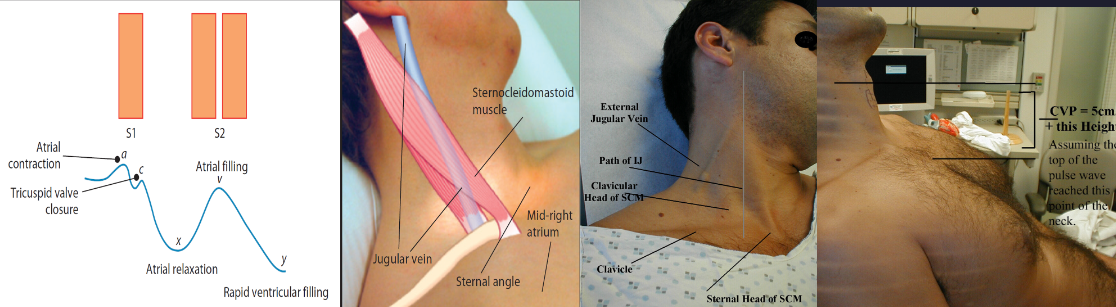
Observe the level of the jugular venous pulse in the neck.
A positive abdominojugular reflux test suggests elevated central venous pressure, which can be due to right heart failure or constrictive pericarditis, among other conditions.
Watch the jugular vein as you apply pressure. A positive test is indicated by a sustained rise in the JVP of more than 3 cm that persists as long as pressure is applied and then quickly returns to normal when the pressure is released.
Locate the Sternal Angle (Angle of Louis): This is the bony prominence at the junction between the manubrium and the body of the sternum. It’s typically in line with the second rib and is a key landmark for assessing JVP.
Identify the highest point of the distended jugular vein pulsation. In cases of high venous pressure, this might be visible above this angle.
Place a ruler vertically on the sternal angle. Then use another ruler or straight edge to form a right angle with the first ruler at the level of the highest visible pulsation. This second ruler will help you measure the vertical distance from the sternal angle to the top of the JVP.
Calculating CVP:
-
Measure the vertical height of the JVP above the sternal angle in centimeters. This height is added to a baseline pressure assumed to be approximately 5 cm H₂O, which is the vertical distance from the right atrium to the sternal angle when the patient is lying at 45 degrees
-
For example, if the JVP is observed 3 cm above the sternal angle, the estimated CVP would be 3 cm (height of JVP above the sternal angle) + 5 cm (baseline pressure) = 8 cm H₂O.
Timing and Observation:
- The ‘A’ wave occurs after the P wave of the ECG and just before the carotid pulse.
- The ‘V’ wave occurs later in the cardiac cycle and peaks after the carotid pulse.
Causes for raised JVP
- Right sided heart failure
- Constrictive Pericarditis
- Restrictive cardiopathy
- Mitral Regurgitation; ---- A / V Wave
- Bronchogenic Carcinoma; without any waves - rest on this list has waves
JVP
- Visible but not palpable
- Two pulses - A and V
- hepatojugular reflux
- Change in respiration
- Between two heads of sternocleidomastoid, and arise till lobe of the ear
Carotid
- V + D, One pulse systemic
- Palpable, may be visible in some pathologies
- No hepatojugular reflex
- No Change in respiration
- medial to sternocleidomastoid - lateral to trachea
Chest
- Gynecomastia,
- spider nivea,
- hair distribution,
- surgical scars,
- chest buldging, Clear Deformity; pect excv- others
- cvs diseso?,
- visible palpation.
- Check for scars on chest for (ICD-valve replacement-transplant-CHD if it’s young- CABG check his legs and hand) -Mediastinotomy Scar: This is a scar on the chest, typically vertical, resulting from a mediastinotomy, which is a surgical procedure to access the mediastinum (the central compartment of the thoracic cavity). -Valve Replacement/CABG Scar: For patients who have undergone valve replacement or CABG (often referred to colloquially as “cabbage”), expect to find a sternotomy scar, which is a vertical scar down the middle of the chest. - though they are very rare
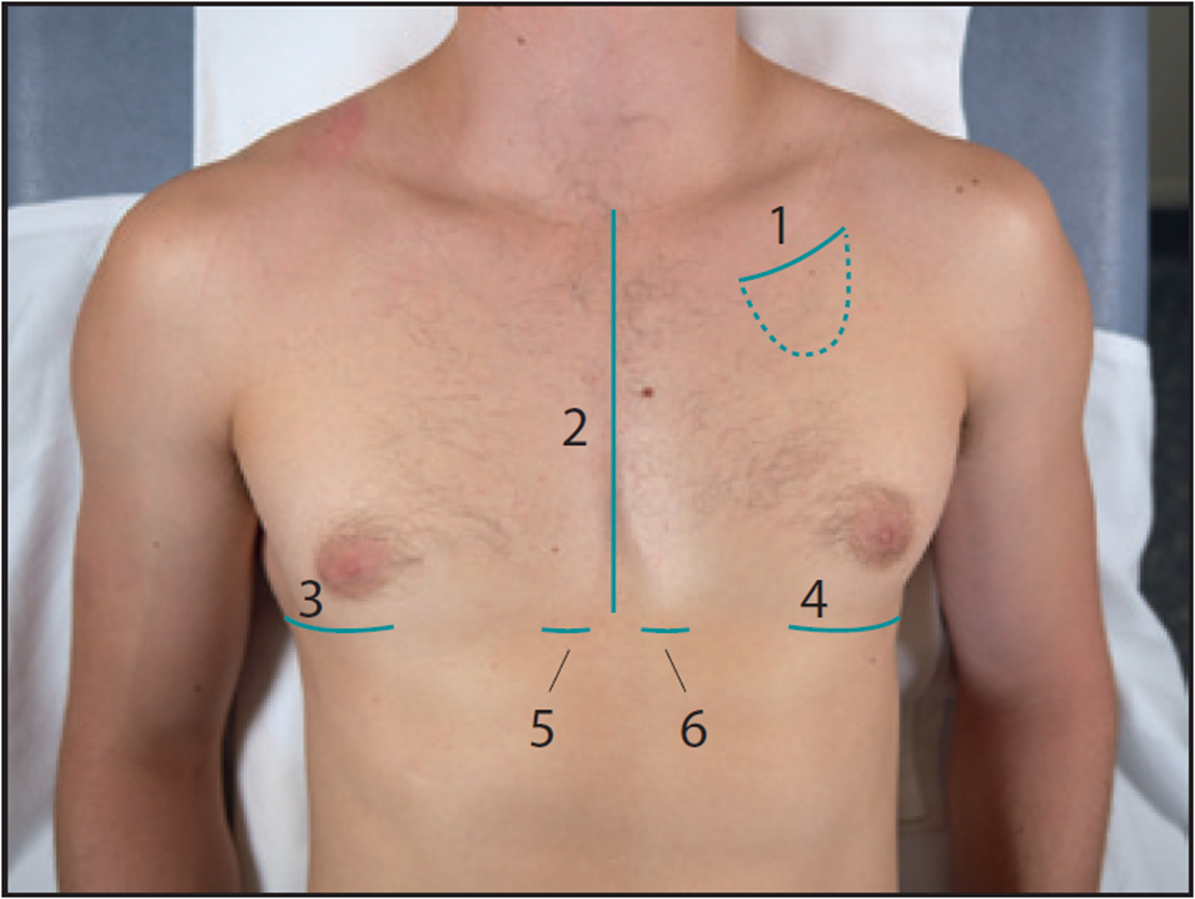
- 1 = pacemaker scar
- 2 = median sternotomy scar
- ==3 + 4 = right and left lateral thoractomy scars,==
- 5 + 6 = surgical drain scars
Lower Limb
- Unilateral Cyanosis - DVT
- Bilateral Cyanosis - Cortication of AORTA -
- If unilateral hairless, painful, Cyanosed - Ischemia PAD
- Hoof-mans Sign; DVT; though not highly specific
- Edema gradings
- Search for scar saphenous vein graft - -Saphenous Vein Graft Scar: This scar results from harvesting the saphenous vein in procedures like coronary artery bypass grafting (CABG). Look for a linear scar along the inner thigh or leg where the vein was removed.
Signs to look out for
Palpation:
I- Peripheral Pulses Examination
Rate, rhythm, volume, character, synchronization
A- Rate: placing three fingers without moving patient arm upon bony prominence of radial artery - times 30 seconds multiply by two counted, have watch in your pocket
B- Rhythm:
- Irregular; Mitral Stenosis
C- Volume
- Large; Pulse on superficial touch, collapsing pulse - Aortic/Mitral Regurgitation
- Small; Aortic Stenosis, Mitral Stenosis, anemia, (peripheral artery???) - not necessary to do
- Normal;
D- Character
Grading per finger - 1st normal - 2nd bounding pulse - 3rd +ve collapsing pulse - 4th water hammer pulse severe aortic regurgitation
Bounding pulse -
- normally in preganancy
- anemia, thyrotoxicosis,
Collapsing Pulse Large pulse (aortic regurgitation); will feel when you raise patient hand tje pulas higher than before and the radio will be lower - Ask if theres pain on shoulders - collapsing pulse; press four fingers against brachioradialis - normal if arm is above head
Pulsus alternans
- (left ventricular failure)
Pulse deficit
- (atrial fibrillation)
Pulsus Paradoxus Cardiac Tamponade, PE, Asthma, Emphysema, Constrictive pericarditis
Pulsus Bisferiens digitalis toxicity, Aortic regurgitation & or stenosis
E- synchronization
- Radio Radial, Radio femoral delay
- all cardiovascular exam mostly 45 degree
Sync Radio Radial refers to a difference in the timing of the pulse between the two radial arteries. This can be indicative of subclavian artery stenosis & Aortic cortication
- Trauma is the most common
- Recurrent Arterial blood gasses testings; DM, Atherosclerosis
- Takayasu disease - This is a rare form of vasculitis that predominantly affects Asian women and can involve the subclavian and aortic arch arteries. It leads to narrowing, occlusion, or aneurysms of the affected arteries.
Sync Radio femoral delay
patient should stand, test for femoral artery
Mid inginual point; typically located from the anterior superior iliac spine (ASIS) to the pubic symphysis.
- Cortication of descending aorta
D- Arterial Examination Points of Lower Limb
-
Dorsalis Pedis Artery:
- Origin: This artery originates from the anterior tibial artery. It is located on the dorsum (top) of the foot.
- Location for Palpation: It can typically be felt by palpating the foot just lateral to the extensor tendon of the big toe.
-
Peroneal Artery (possibly meant by “Perinoeum”):
- This artery, also known as the fibular artery, runs along the lateral aspect of the lower leg and supplies blood to the lateral compartment of the leg.
- It does not travel below the feet but can be challenging to palpate as it lies deep between the muscles of the lower leg.
-
Anterior Tibial Artery:
- This artery passes down the front of the leg. It originates from the popliteal artery and travels down to become the dorsalis pedis artery at the ankle.
-
Posterior Tibial Artery:
- Location for Palpation: This artery can be palpated behind (posterior to) the medial malleolus, which is the bony prominence on the inner aspect of the ankle.
- It does not specifically involve the calcaneum (heel bone), but it runs down the inner aspect of the ankle close to the medial malleolus.
-
Popliteal Artery:
- This artery is found at the back of the knee and is the continuation of the femoral artery. It is best palpated with the knee slightly flexed and relaxed.
-
Common Femoral Artery:
- Location for Palpation: This artery is palpated in the groin at the mid-inguinal point, which is halfway between the anterior superior iliac spine and the pubic symphysis.
-
Aorta:
- Palpating the aorta itself through the abdominal wall is challenging and usually only possible in thin individuals or when an abdominal aortic aneurysm is present.
- Bruit: If there is aortic stenosis or an aneurysm, a “bruit” can often be heard using a stethoscope. A bruit is a whooshing sound made by turbulent blood flow.
- Other Sounds: In the case of other vascular closures or narrowing, similar bruits can be heard at different sites along the arteries, depending on the location of the narrowing.
II- Assess the character Apex Beat:
localized apex beat, count from mid axillary after angle of loui 2nd ICS innermost outermost. Areas of maximum pulsation - Typically located in the left fifth intercostal space at the midclavicular line.
Technique: Place your flat of your hand gently in this area to feel the pulsation. If the pulsation is not palpable, ask the patient to lean forward or turn to their left side, which may make the apex beat more apparent.
- Normal
- Tapping – in mitral stenosis
- Heaving (when pressure overload) – aortic stenosis, hypertension
- Thrusting (when volume overload) – Aortic/Mitral Regurgitation
- Impalpable
- Obesity
- COPD
- pericardial effusion
- Emphysema
- Apex is Under the Rib
- Shifted apex to the axilla; due Dilated Cardiomyopathy/Mitral Regurgitation
- Pericardial effusion = Pericarditis // Friction rub sounds
- Dextrocardia
III- Parasternal Heave:
Location: lateral to the sternum. 3-5th ICS
Technique: Lightly place your hand over the left parasternal area to feel for any heaving motions.
Positive test Indicates
- Right ventricular hypertrophy; typically due to conditions like pulmonary hypertension or tricuspid regurgitation
IV- Thrill:
Check thrill on all 5 areas of the heart diastolic thrill, apex you hear mitral - thrill = palpable murmur after grade 3
- Palpable second heart sound - Pulmonary HTN
Systemic HTN - RT side thrill??
V- Lower Limb edema test
-
Greet patient - take consent -
-
Before proceeding with the physical examination, ask the patient if they are currently experiencing any pain in their limbs. This can help differentiate between edema due to fluid overload and edema due to inflammation or injury
-
Using your thumb, apply firm pressure to the soft tissue of the area. Press down until the pressure of your finger causes a noticeable indentation.
-
Maintain the pressure for about 10 seconds before releasing. This duration allows adequate time to displace the fluid and create a visible indentation if edema is present.
Grade the pitting edema if present:
- 1+ Mild pitting, slight indentation, no perceptible swelling of the limb
- 2+ Moderate pitting, indentation subsides rapidly
- 3+ Deep pitting, indentation remains for a short time, leg looks swollen
- 4+ Very deep pitting, indentation lasts a long time, leg is very swollen
Ectopic pulse; Irregular Sinus Rhythm; skipped heart beat, may be due stressors, caffiene, alcohol etc..
Abdominal Palpation
- Patient lying with one pillow (if tolerated)
- Tender hepatomegaly
- Pulsatile liver (tricuspid regurgitation) Z
- Ascites
- Splenomegaly
- Abdominal aortic aneurysm
Percussion:
used in specific cases, not routine
Auscultation:
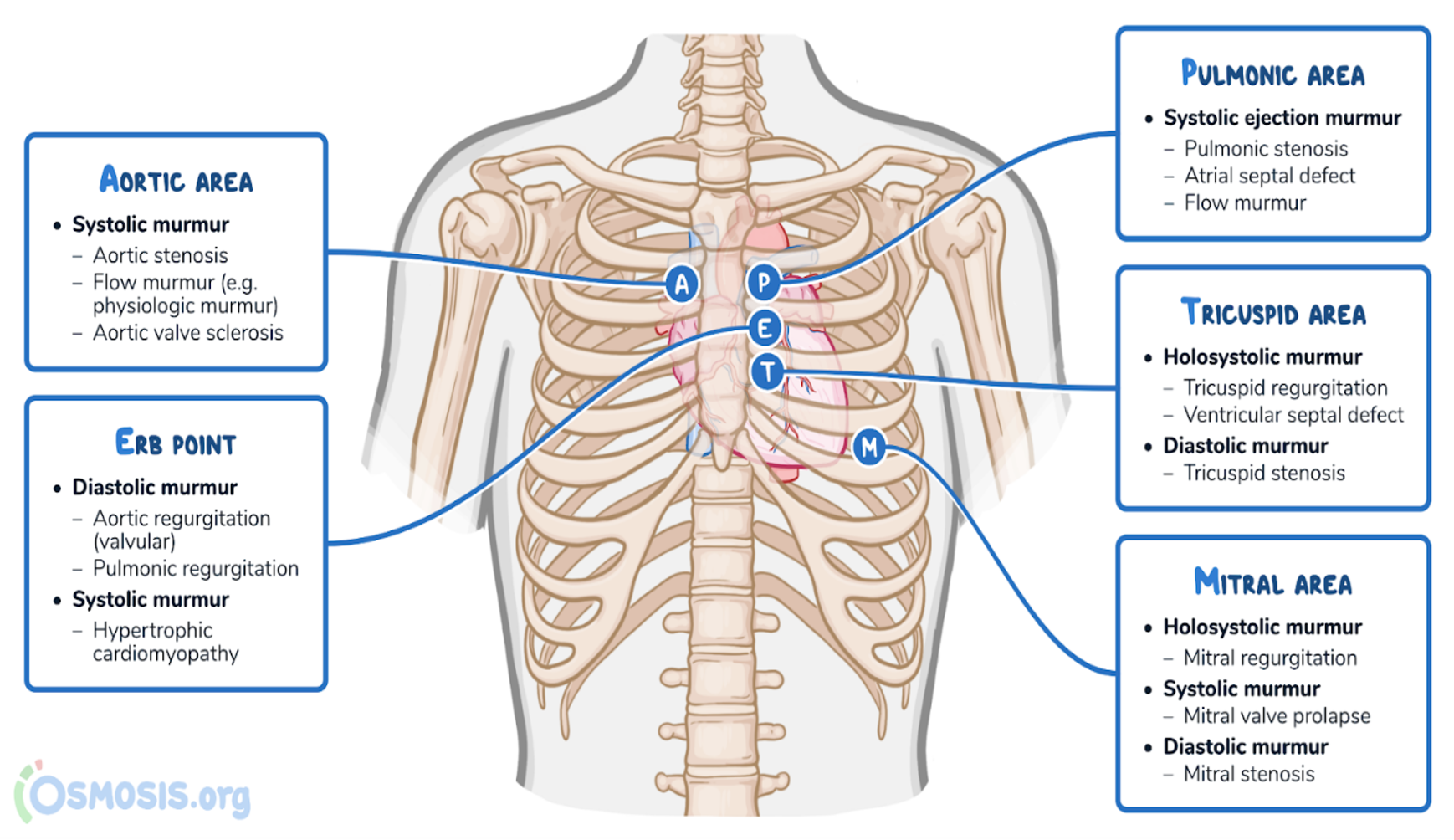
S1 -(Systolic)- S2 —> (Diastolic) —> S3,S4 —> S1 heard after S1 is systolic, after S2 is diastolic
Points of auscultation Mitral + Tricuspid + ERB’s point + Aortic + Pulmonary
Abnormal Heart Sounds
- Systolic; MR,TR, AS, PS.
- Diastolic; MS,TS, AR, PR.
- Continuous; Patient Ductus Arteriosus (PDA)
Signs of cardiac failure:
- Elevation of the JVP.
- Gallop rhythm (tachycardia and 3rd HS).
- Basal crepitations. ?
- Hepatomegaly.
- Dependent pitting oedema.
SIgns of pericarditis - Scratchy - Grating - Tri-phasic friction rub on auscultation - Comprises ventricular systole - Early diastolic ventricular filling - Late diastolic atrial systole.
| Systolic Murmurs - aorta open | Diastolic Murmurs/Sounds |
|---|---|
| (crescendo-decrescendo) AS = aortic stenosis & PS = pulmonary stenosis HCM = hypertrophic cardiomyopathy | (Early Diastolic/Decrescendo) AR = aortic regurgitation PR = pulmonary regurgitation |
| (Holosystolic/Pansystolic) MR = mitral regurgitation TR = tricuspid regurgitation VSD = ventricular septal defect | (Mid-late Diastolic/ decrescendo- crescendo) MS = mitral stenosis TR = tricuspid stenosis |
| I = innocent murmur | S3 = third heart sound |
| PDA = patent ductus arteriosus (continuous murmur) |
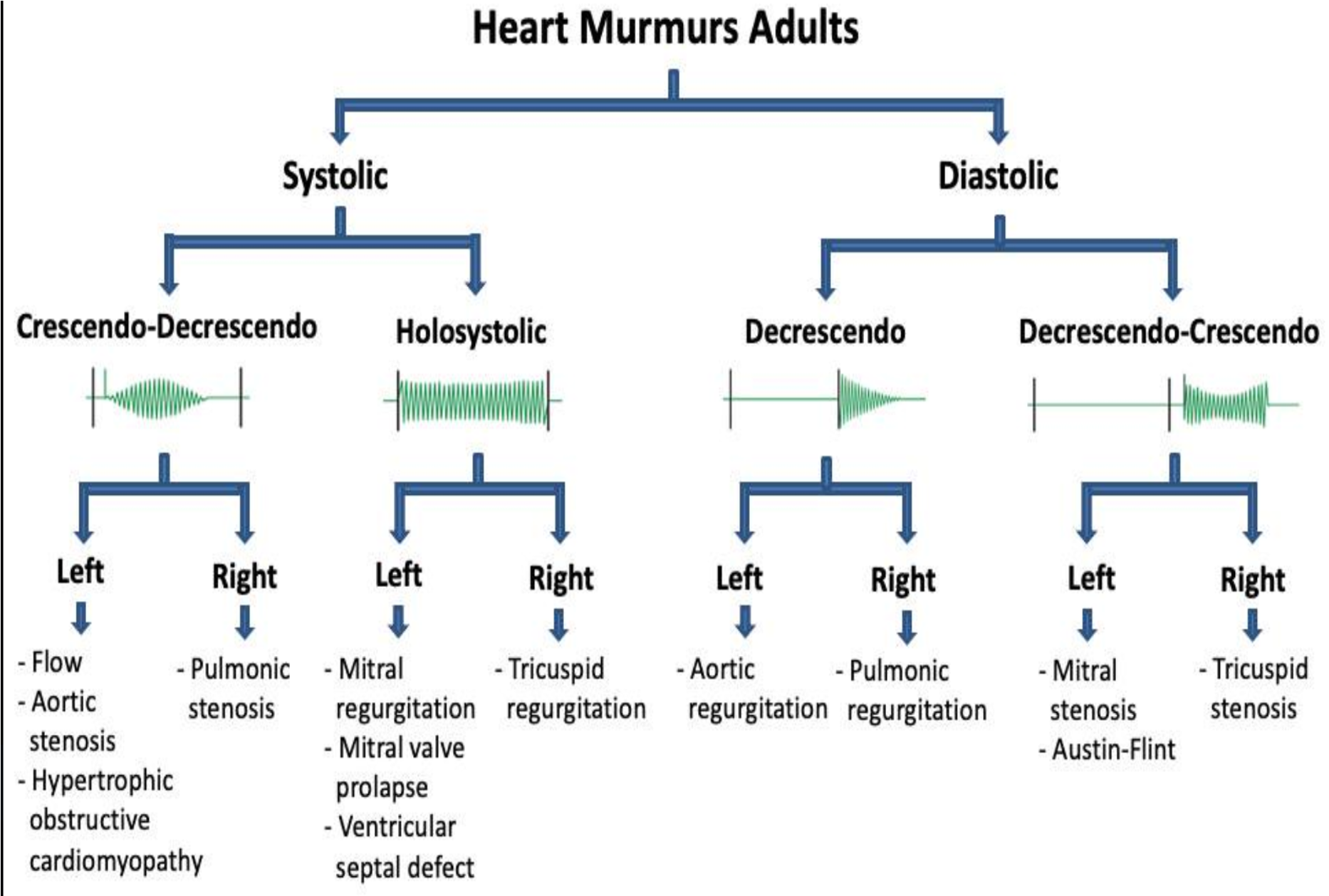
Radiation
-
Aortic stenosis; Typically causes a systolic murmur that can radiate to the carotid arteries. The presence of aortic calcification, which can be associated with aortic stenosis, does not necessarily cause pain but can contribute to the severity of the stenosis detectable via imaging or echocardiography.
-
Mitral regurgitation; have pansystolic murmur that radiates to the axilla. The murmur starts with S1 and extends up to S2, indicating the backward flow of blood from the left ventricle to the left atrium throughout systole.
Sound Differentiation
- Tricuspid Regurgitation - swoosh dub murmur - RT. V. Hypertrophy
- Mitral Stenosis - LUB dub -
- Regurgitation صوت قبيح
- Stenosis صوت جميل
Localization of Heart Sounds
Mitral Stenosis: This condition is best evaluated by listening over the mitral area, which is generally found over the apex of the heart, toward the left side of the chest.
Austin Flint Murmur of Aortic Regurgitation: S1 (first heart sound) is typically best heard in the aortic area, which is the right second intercostal space near the sternum. It is best felt in the pulmonary area, which refers to the left second intercostal space adjacent to the sternum.
Tricuspid Stenosis: This is best heard over the tricuspid area, located at the lower left sternal border of the chest.
Left Atrial Myxoma: Suspected when a tumor in the left atrium causes a sound, which can often be best detected near the heart’s apex.
Diastolic Murmurs: These murmurs are generally quiet and can be challenging to hear. It is advisable for the patient to sit forward and hold their breath after exhaling to enhance the audibility of these murmurs.
Other Notes
-
Puts stethoscope in pocket whilst examining if finished with it
-
To assess rate (bring your watch and put it in the pocket)
-
Regurg not palpable
-
Move Z with heart exam
-
Heart with bell; low pitch for diastolic murmurs
-
Hearing a turbulence blood flow (Bruits) narrow artery; athero
-
Aortic stenosis ⇒ Carotid
-
Pansystolic Murmur is heart murmur that occurs throughout the entire systole S1 to S2
-
Mitral regurgitation sound radiates to axilla
-
RHF —> inspiration — pulmonary/Tricuspid
-
kussmaul’s sign - increased JVP in inspiration paradoxical
-
LHF—> Expiration — Aortic/Mitral
180/100 tolerable BP if high BP >220/110 decrease gradually to 180/100
- ACE inhibitors
- ARBs
- CCBs
timing of conditions most commonly presented in ER 3 AM; CVA, DM, Stroke 4 AM; Bronchial Tree Constriction 5 AM; IM + Angina
- Mitral stenosis = varicosed?
- Mcburdy point auscultation?
- examine abdomen = IPPA of abdomen it self
- Examine GIT = peripheral + IPPA
Right Sided Heart Failure
- SVC; Raised JVP
- IVC; Tender hepatomegaly + acities + bilateral pitting edema
Left sided heart failure
- Bi-basal crackles; indicate pulmonary edema
- Pulmonary edema
- Audible S3,S4 Gallop Rhythm - usually not heard until heart strain
corpus spongiosum?? Pyroni disease?? Acantnosis nigricans?? radial brachial pulsation thrill mass like?? carotid to sync
dyspnea ask about paroxysmal orthopnea, cough, wheeze, lower limb edema, fever
pneumonia, CRF, infective endocafrditis, SLE, stroke,
Cases
C1
20 year old male presented to clinic with ankle edema, raised jvp, and ascites
C2
77 years old male sudanese he came to ER complaining of chest pain for 9 days, diffused tightness gradual tightness exacberating by exertion, relieving by rest, associated with cough with clear phlegm, severe sob 1-2h before presentation to ER- no palpitation, no syncopal attack, no b symptoms
diffused gradual chest pain
C3
Ali 62y yemeni presented with chronic exacerbation 1wk hx of progressive continuous SOB, relieved by sitting, exarcebated by slight movement.
sleep with pillow? Allergen - perfumes, dust, smokes? comes in specific time? slight exercise?
associated with cough + white viscous phlegm (simple; if green ask amount and smell),
No Syncope No Runny nose No Orthopnea? no chest pain, No palpitation - khafagan No diziness wheezing Lower limb swelling
Diagnosed inititial lung disease?? + + HF??
NYHA classification for dyspnea
- Class 1 - exercise
- Class 2 - Normal activity
- Class 3 - Slight movement
- Class 4 - At Rest
C4
20 year old male presented to clinic with ankle edema, raised jvp, and ascites