Post Infection Glomerulonephritis
Post-Infectious Glomerulonephritis
Presenter
Dr. Mansour Alqurashi
Learning Objectives
- Background
- Pathophysiology
- Histologic Findings
- Clinical
- History
- Physical
- Lab
- Differential Diagnosis
- Treatment
- Follow Up
Background
- Glomerulonephritis: Inflammation of the glomerulus, manifested by proliferation of cellular elements, secondary to an immunologic mechanism.
- Most cases are associated with a post-infectious state.
- Common in children aged 4-12 years, with a peak at 5-6 years.
- Male to female ratio: 1.7-2:1.
- Prognosis is generally good.
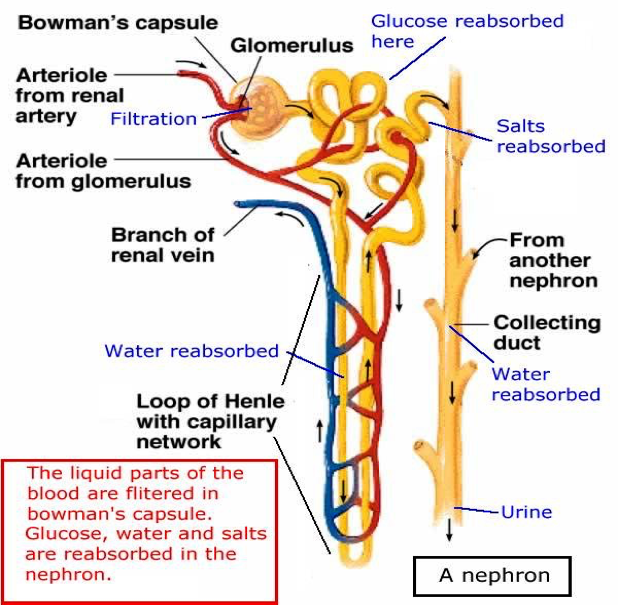
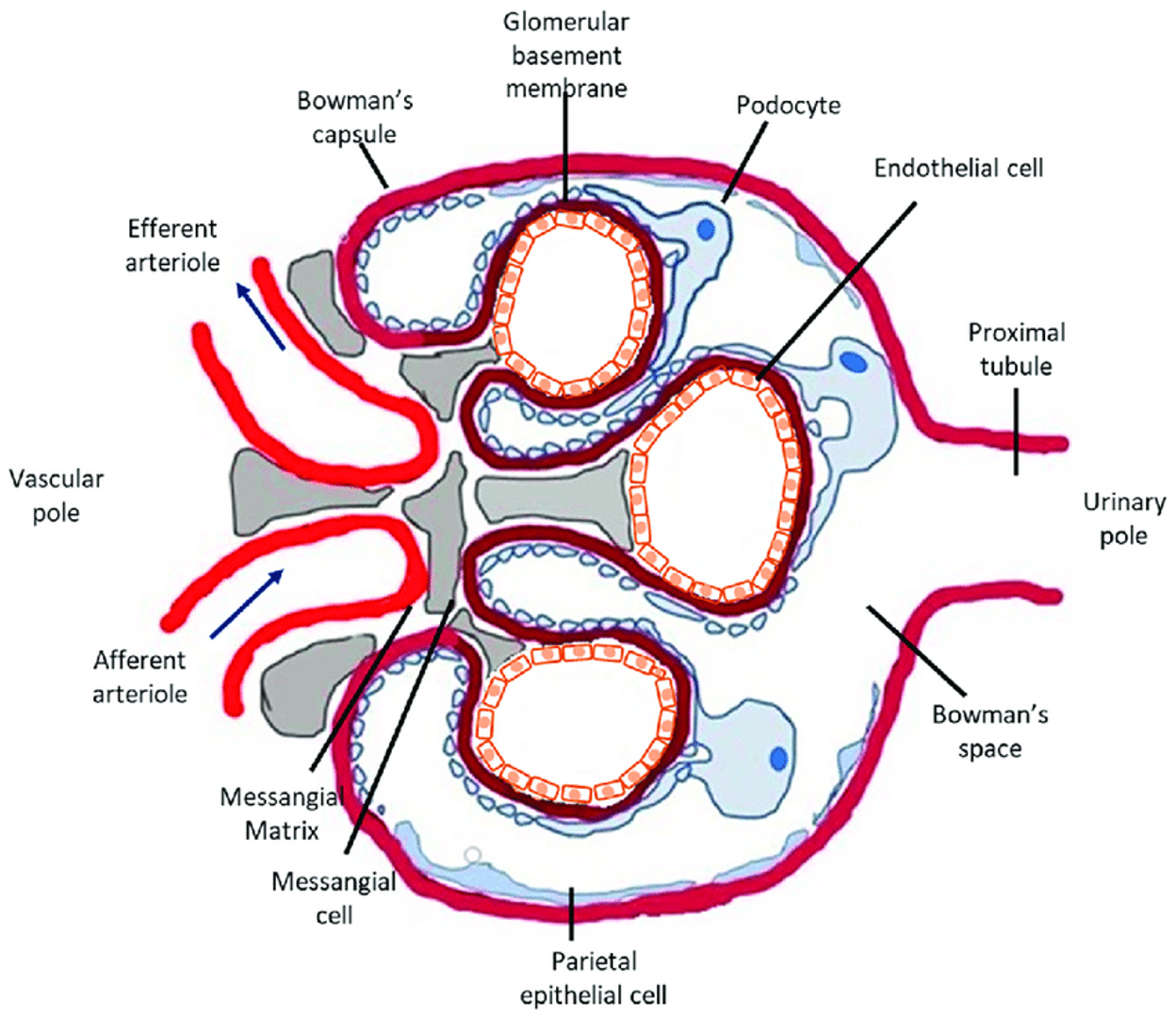
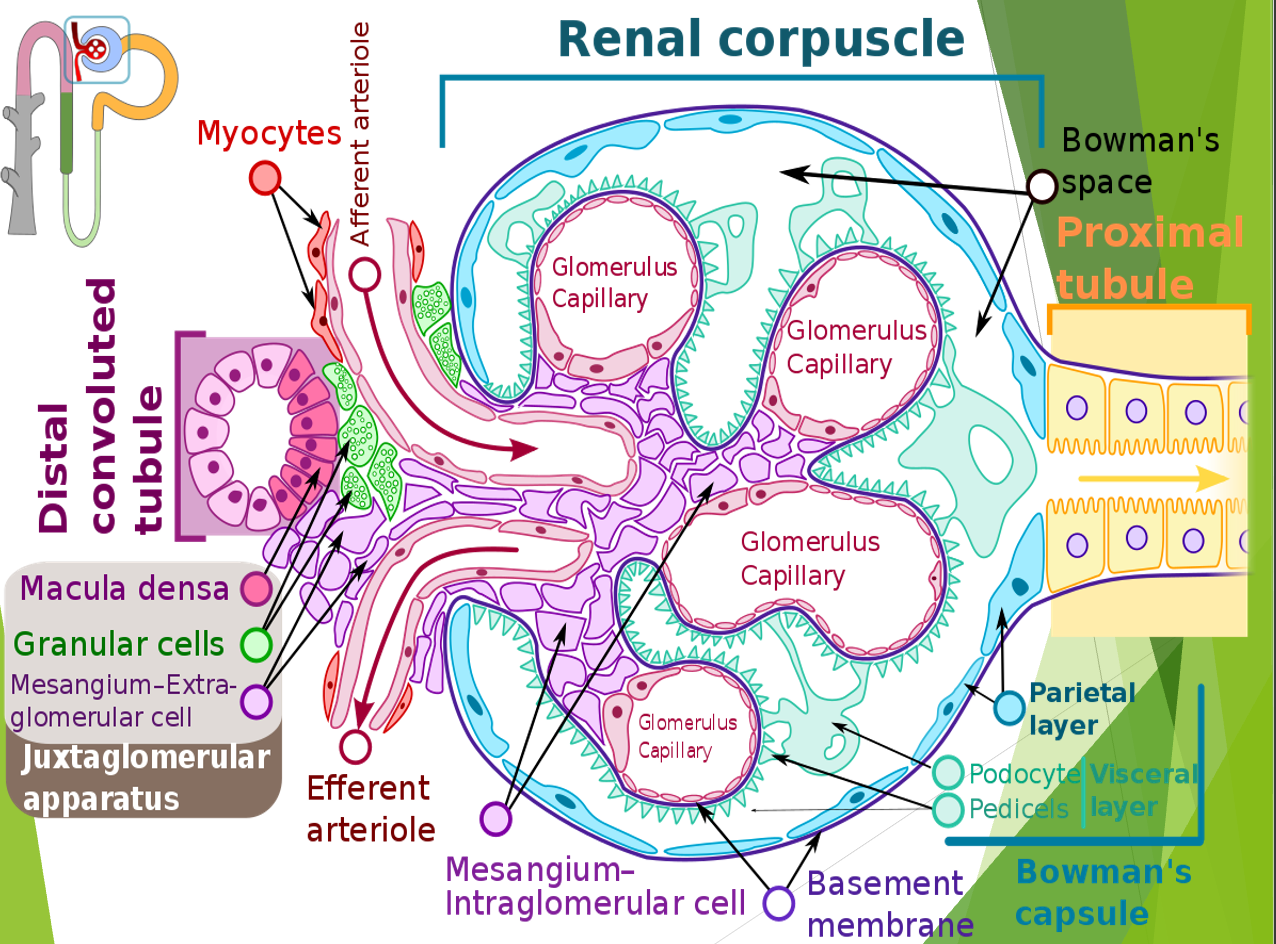
Filtration Barrier at the Glomerulus
- Three Layers:
- Capillary endothelium of glomerulus
- Basement membrane of glomerulus
- Visceral epithelium of Bowman’s capsule (podocytes with foot processes)
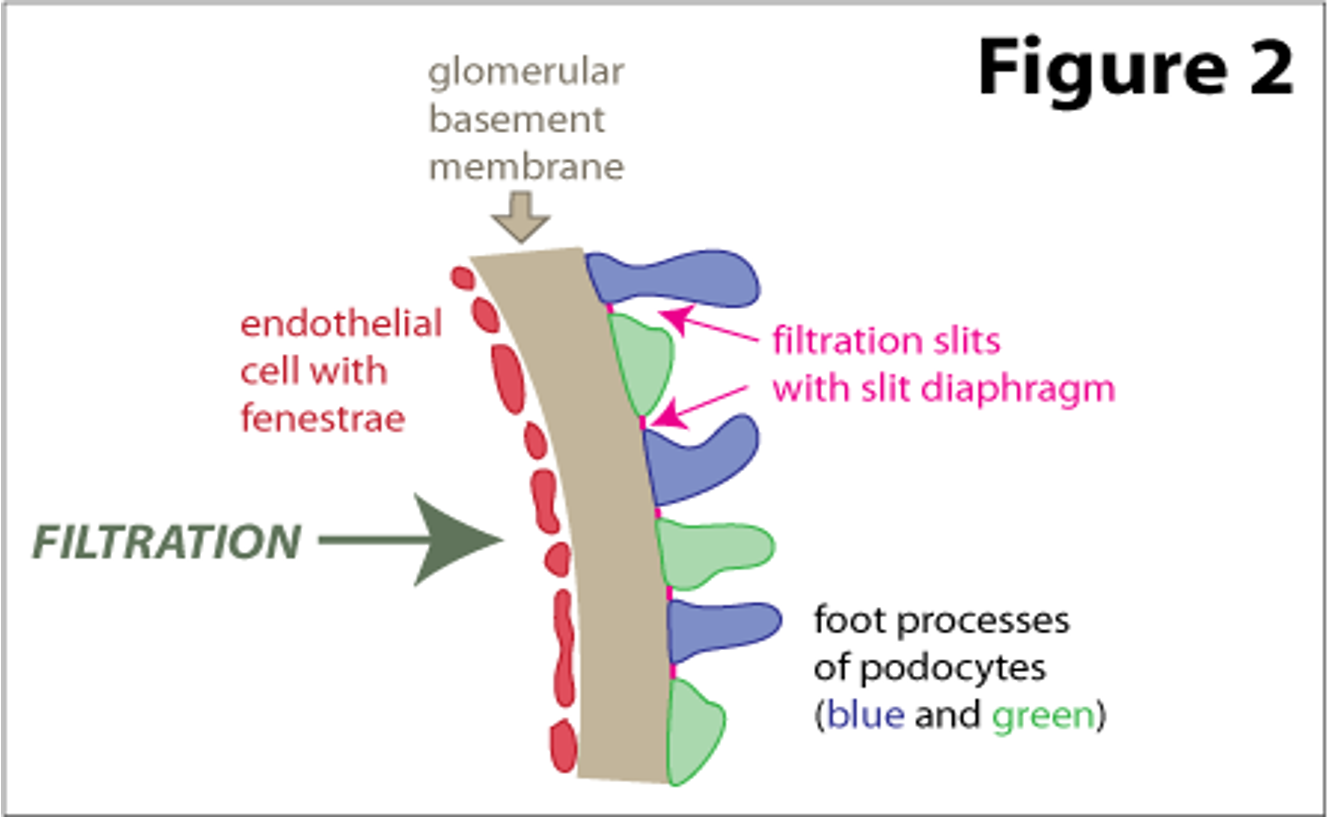
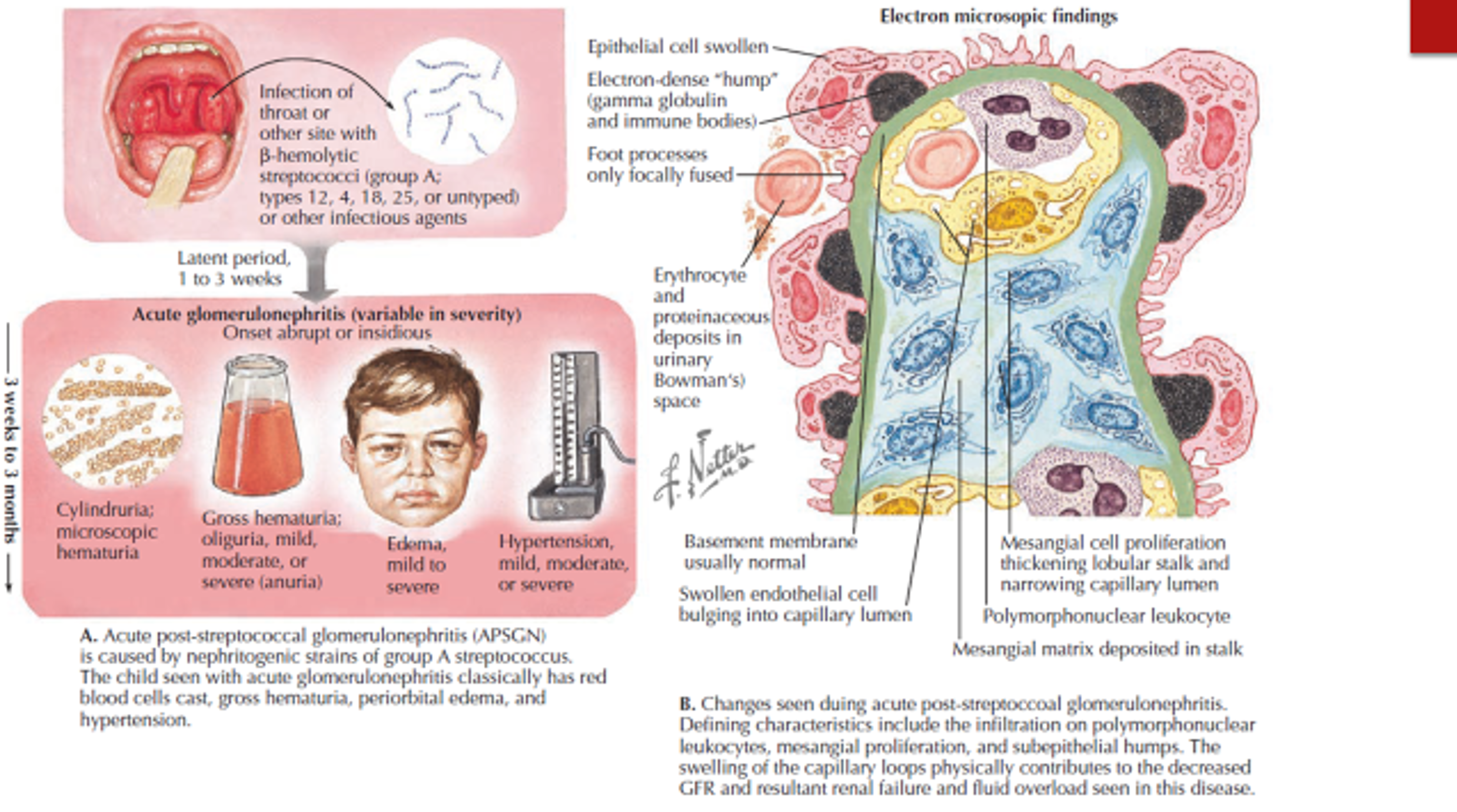
Pathogenesis
- Strep Antigens: Trigger antibodies that cross-react with glomeruli.
- Immune Complexes: Filtered by glomerulus and get stuck, activating complement.
- Damage: Diffuse and generalized damage to glomeruli.
- GFR and RBF: Decreased GFR due to inflammation; RBF decreases proportionally, maintaining normal filtration fraction.
- Tubular Function: Preserved.
- Plasma Renin and Aldosterone: Normal.
Incidence and Spectrum
epidemic form Decline in industrialized countries.
- Post-Streptococcal Glomerulonephritis: 28-47%
- Staph Aureus (Epidermidis): 12-24%
- Gram-Negative Bacteria: 10-22%
- Other Conditions: Bacterial endocarditis, shunt infections, atypical PIGN.
uacute endocapillary glomerulonephritis with mesangial and capillary granular immune deposition
General Symptoms
- Fever, Headache, Malaise
- Anorexia, Nausea, Vomiting
- Pallor: Due to edema and/or anemia.
- Confusion, Lethargy
- Enlargement of the Liver
Signs and Symptoms
- Gross Hematuria: 25-33%, dark brown or smoky urine.
- Oliguria: Urine output < 400 ml/day.
- Edema: 85%, starts in eyelids and face, then limbs, becomes generalized.; - Hypertensive encephalopathy, heart failure and acute pulmonary edema may occur in severe cases
- Hypertension: 60-80%, mild to moderate.
- CNS Symptoms: Seizures in 10%.
- Nephrotic Syndrome: Rare.
- ARF/Acute Renal Necrosis: Not uncommon, due to capillary injury or thrombosis.
Clinical Features - Examination
- State of Patient:
- Routine observations (temperature, HR, SBP, RR, SaO2).
- Core-peripheral temperature
- Serial plot of weights, heights
- Hydration: Peripheral perfusion, JVP, edema.
- Signs of Cardiac Failure
- Multi-System Disease Clues: Rash, arthropathy, arthritis, oral lesions.
- Palpable Kidneys or Masses
Mixed Nephritic and Nephrotic Syndromes
-
Nephritic Syndrome: Hematuria, proteinuria, oliguria, hypertension. Common Cause: PIGN/PSGN (Post-Infectious Glomerulonephritis
-
Nephrotic Syndrome:
- Proteinuria > 40mg/m2/hour | > 1g/m2/day
- hypoalbuminemia,
- edema,
- hyperlipidemia. Common Cause: MCNS (Minimal Change Nephrotic Syndrome).
-
Mixed Syndrome: Commonly caused by post-infectious GN.
Investigations
- Blood Tests: Full blood count, ESR, coagulation screen, serum electrolytes.
- Complement Assays: C3, C4, C3 nephritic factor. (C3: Decreased for few weeks.)
- Serum electrolytes
- U&Es, Cl, CO2, urea, creatinine, glucose
- LFTs, CK, urate, bone profile
- Ca, Mg, PO4, ALP, albumin
- Immunoglobulins: Including IgA, (ASOT, antiDNAase B. (Measured at 2-3 weak intervals))
- Autoimmune Profile: ANA, dsDNA, qDNA, ENA, ANCA, ACIgM/G.
- Culture: From pharynx and skin.
Urine Tests
- Urinalysis
- Urine M,C&S
- Urine Electrolytes
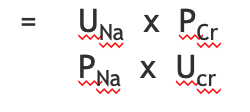
- Fractional Excretion of Sodium (FENa): For evaluation of acute kidney failure .
Note that microscopic haematuria can persist for years following the acute episode.
Imaging and Biopsy
Renal ultrasound scan
- bilateral echogenic kidneys
Percutaneous renal biopsy
- confirm PIGN
- exclude MPGN
- consider crescentic GN.
The indications for renal biopsy are:
- severe renal dysfunction at presentation
- rapidly progressive acute renal failure
- atypical presentation
- delayed recovery
- macroscopic haematuria for >1 month
- low C3 levels for >6 months
- heavy proteinuria for > 6 months
Differential Diagnosis
Hypocomplementemia
- PIGN
- Bacteria (GAS, S. viridans, pneumococcus, S. aureus, S. epi, atypical mycobacterium, meningococcus, Brucella, Leptospirosis, Propionibacterium)
- Viruses (VZV, EBV, CMV, rubeola)
- Parasites (Toxo, Trich, Riskettsia)
- Membranoproliferative GN
- SLE
- Cryoglobulinemia
- Bacterial Endocarditis
- Shunt nephritis
Normal complement
Treatment
Treatment of Underlying Infections in Acute GN
Antimicrobial Therapy
- Antibiotics (e.g., penicillin) are used to control local symptoms and to prevent the spread of infection to close contacts.
- Antimicrobial therapy does not appear to prevent the development of GN, except if given within the first 36 hours.
Loop Diuretic Therapy
- Loop diuretics may be required in patients who are edematous and hypertensive in order to remove excess fluid and to correct hypertension.
- Relieves edema and controls volume, thereby helping to control volume-related elevation in BP.
- Vasodilator drugs (e.g., nitroprusside, nifedipine, hydralazine, diazoxide) may be used if severe hypertension or encephalopathy is present.
Diet
- Sodium and fluid restriction
- Protein restriction for azotemic patients
Activity
- Recommend bed rest until signs of glomerular inflammation and circulatory congestion subside.
Follow Up
-
Prognosis: Usually excellent.
-
Mortality: 0.5% due to pulmonary edema or pneumonia.
-
Progression to CKD Stage 5: <1%.
-
Monitoring: Ensure control of hypertension, resolution of edema, hematuria, proteinuria, and normalization of creatinine.
-
Gross hematuria resolves within 2 weeks
-
Complement low for 6-8 weeks
-
Proteinuria remains upto 6 months
-
Hematuria remains upto 2 years