Jaundice appearing during 1st 24 hours, hemolytic disease of the newborn should be suspected until proved otherwise.
Rhesus hemolytic disease
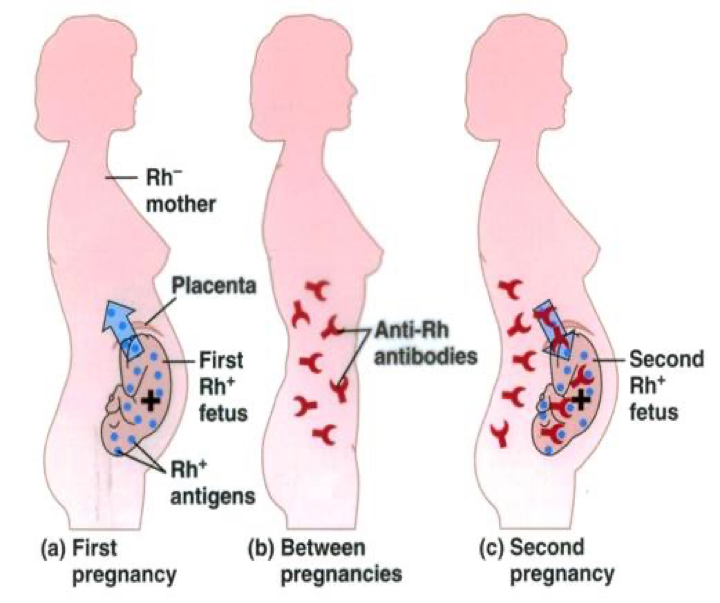
- Rh incompatibility that develops between Rh-negative mother previously sensitized to the Rh D antigen and her Rh positive fetus.
- Initial exposure of the mother to the Rh antigen occurs during birth, abortion, or ectopic pregnancy.
- Re-exposure to the Rh antigen will cause elevation of maternal specific IgG-Rh antibody.
- These antibodies pass through the placenta and attach to fetal erythrocyte causing extravascular hemolysis.
- Affected infants are usually identified antenatally and monitored and treated if necessary.
- Antibodies may develop to rhesus antigens other than D and to the Kell and Duffy blood groups, but hemolysis is usually less severe.
- Rho(D) immune globulin (RhoGAM) immunoprophylaxis at 28 weeks gestation in the absence of sensitization or within 72 h of suspected Rh antigen exposure or both will reduce the risk of sensitization to < 1 %.
ABO incompatibility
- This is now more common than rhesus hemolytic disease.
- Most ABO antibodies are IgM and do not cross the placenta, but some group O women have an IgG anti-A-haemolysin in their blood, which can cross the placenta and haemolyse the red cells of a group A infant.
- Occasionally, group B infants are affected by anti-B haemolysins. Hemolysis can cause severe jaundice but it is usually less severe than in rhesus disease.
- The infant’s haemoglobin level is usually normal or only slightly reduced.
- The direct antibody test (Coombs’ test), which demonstrates antibody on the surface of red cells, is positive.
- The jaundice usually peaks in the first 12 hours to 72 hours.
Diagnosis
- Blood type and Rh factor in the mother and infant
- Reticulocyte count
- Direct Coombs’ test
- Blood smear
- Bilirubin level (fractionated and total)
other hemolytic causes of unconjugated hyperbilirubinemia:
Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- X-linked recessive disorder.
- Those affected tend to be Mediterranean or Middle or Far Eastern or African in origin.
- Low levels of glucose-6-phosphate dehydrogenase.
- They may develop hemolytic anemia in response to a number of stressors, e.g. infection, certain medications, fava beans when older.
- It is diagnosed by measuring G6PD activity in red blood cells.
Spherocytosis
- This is considerably less common than G6PD deficiency.
- There is often, but not always, a family history.
- The disorder can be identified by recognizing spherocytes on the blood film.