Eye Lid

Dermatochalasis
Cause: Aging, loss of orbital fatty support - psuedoptosis

tarsal cyst

Poliosis


Chalazion
- Shape: Chalazoin
- Pathology: Inflammatory granuloma of myopyopoin gland
- Site: Mypoypoian glands

 Incision of chalazion (extensional biopsy)
if recurrent, do excision to exclude malignancy
Incision of chalazion (extensional biopsy)
if recurrent, do excision to exclude malignancy
 Chalazion forceps used in Chalazion surgery (excision)
Chalazion forceps used in Chalazion surgery (excision)
Infected Chalazion (internal hordeolum) Y


Madarosis
loss of eye lashes / brow




Stye (External hordeolum)
- Cause: Staphylococcus infection of Zeis glands
- Treatment: Remove affected eyelashes

Xanthelasma
- Cause: Due hyperlipidemia
- Treatment: Cosmetic (Blephroplasty)

Dermoid Cyst



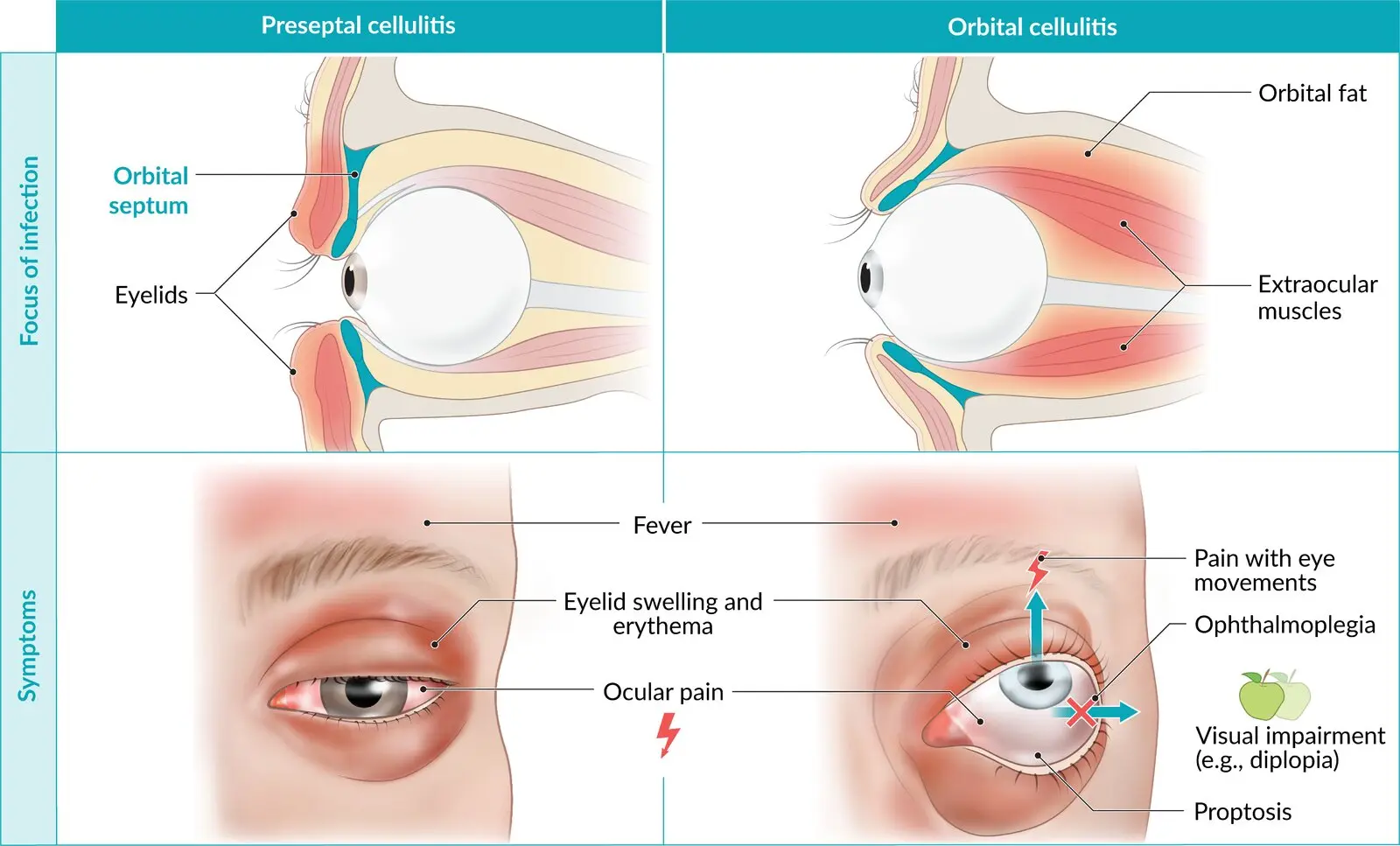
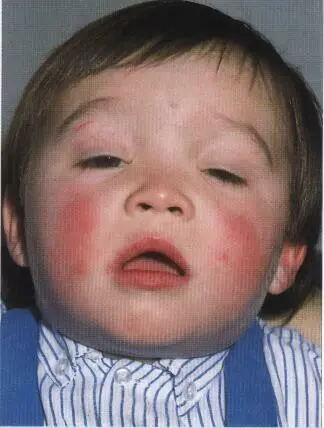
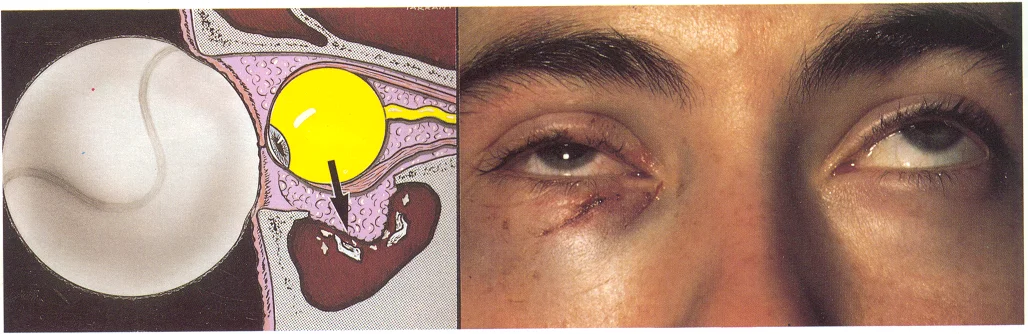
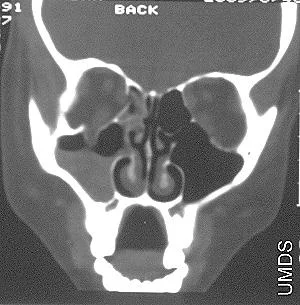
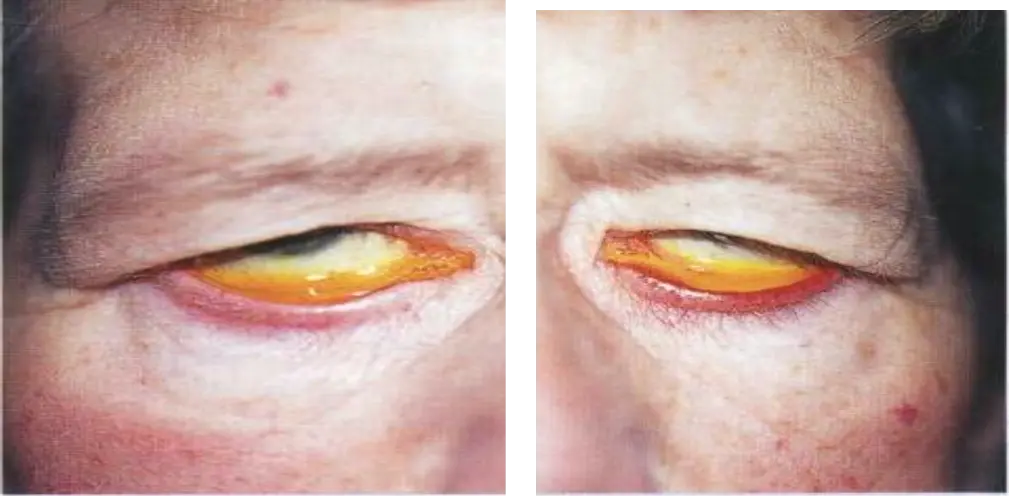
Left/Right Orbital Cellulitis
Can be from Paranasal sinusitis
Common cause:
- Sinusitis
Complications:
- Brain Abscess
- Infection spread to brain
- Cavernous Sinus Thrombosis
- vision loss
- Subperiosteal or Orbital Abscess
Investigations: (to exclude orbital causes - tumors, abscess…)
- CT with contrast
-
- MRI (may be used if CT is inconclusive, or to better evaluate soft tissues/brain involvement).
Treatment:
- Admission
- Systemic intravenous antibiotic + topical antibiotic
| Feature | Preseptal Cellulitis | Orbital Cellulitis |
|---|---|---|
| Location | Infection of eyelid/anterior eyelid tissues, anterior to the orbital septum | Infection of orbital fat and ocular muscles, posterior to the septum |
| Eyelid swelling/erythema | Yes | Yes |
| Tenderness | Mild–moderate | Moderate–severe |
| Ocular pain | Often, but no pain with eye movement | Worse on eye movement |
| Eye movements (motility) | Full range | Restricted |
| Proptosis | No | Yes |
| Vision changes | No | May have ↓ visual acuity / RAPD |
| Systemic signs | May have low-grade fever | Frequently fever, malaise |
| Skin warmth | May feel warm | Often hot to touch |


- Preseptal Cellulitis:
 2. Orbital Cellulitis (Postseptal Cellulitis):
2. Orbital Cellulitis (Postseptal Cellulitis):

Lid retraction
Cause: Thyroid eye disease
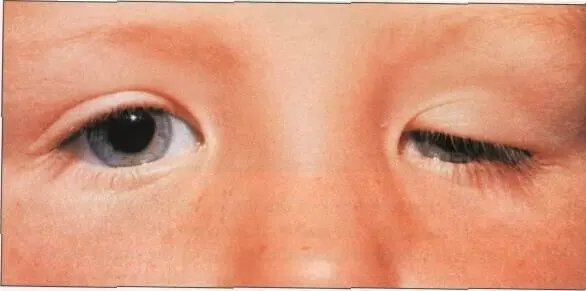

Ptosis
- Simple congenital ptosis:
- Divergent/Exotropia Ptosis: 3rd nerve palsy
- Sign: Ptosis with myosis;
- Diagnosis: horners syndrome -
- Affected muscle: Müller’s muscle

Marcus Gunn phenomenon
Misdirection between 3rd and 5th nerves
-
Marcus Gunn Jaw-Winking Phenomenon
-
This is a form of congenital ptosis characterized by synkinesis: an abnormal neurological connection between the Trigeminal Nerve (CN V), specifically branches innervating the pterygoid muscles (jaw movement), and the branch of the Oculomotor Nerve (CN III) innervating the Levator Palpebrae Superioris muscle.
-
The ptotic eyelid retracts (lifts up) when the patient moves their jaw (e.g., chewing, sucking, opening mouth, moving jaw side-to-side).
Muscles (MS) Elevating Upper Eyelid:
-
Levator Palpebrae Superioris: Innervated by the Oculomotor Nerve (CN III). This is the primary elevator of the upper eyelid.
-
Müller’s muscle (Superior Tarsal Muscle): Innervated by the Sympathetic nervous system. This provides minor (approx. 1-2 mm) eyelid elevation. - Correction: Spelling is Müller’s.
-
Frontalis muscle: Innervated by the Facial Nerve (CN VII). This muscle primarily raises the eyebrows. Raising the eyebrows indirectly helps lift the eyelids, especially when compensating for ptosis. It is considered an accessory muscle for eyelid elevation, not a direct elevator like the Levator or Müller’s muscle.

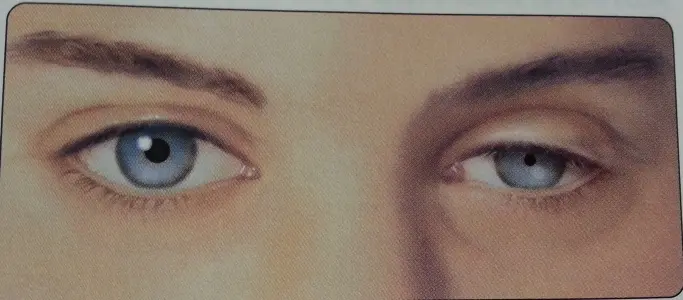
Anisocoria – Horner’s Syndrome Acquired

Anisocoria – Horner’s Syndrome Congenital
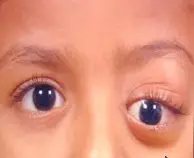
Ptosis, chin elevation - Bilateral severe ptosis


Bilateral Ptosis of myasthenia gravis
appears more severe at end of day, normal when waking up
Finding: ptosis both eyes
Complications squint, diplopia, eye fatigue
betablockers make em worse

Partial ptosis

Total Ptosis
MR affected - 3rd nerve palsy
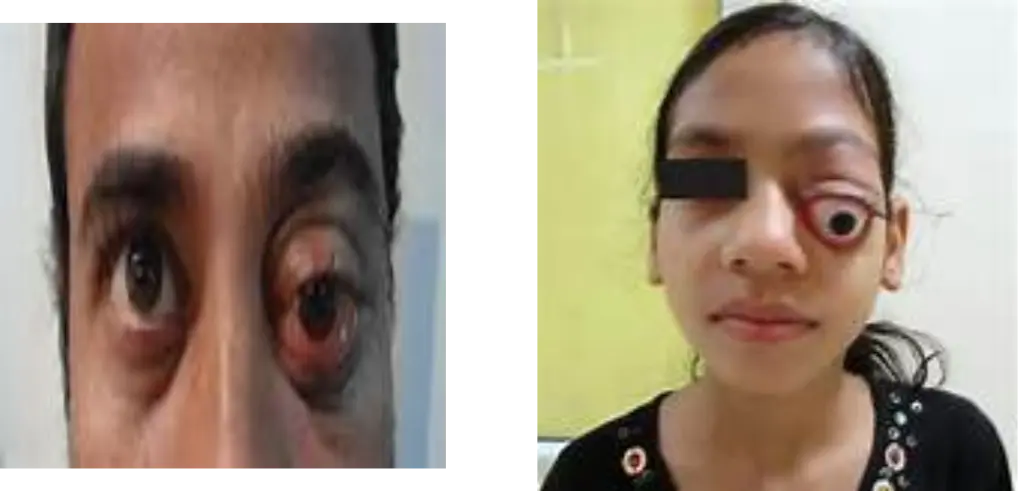
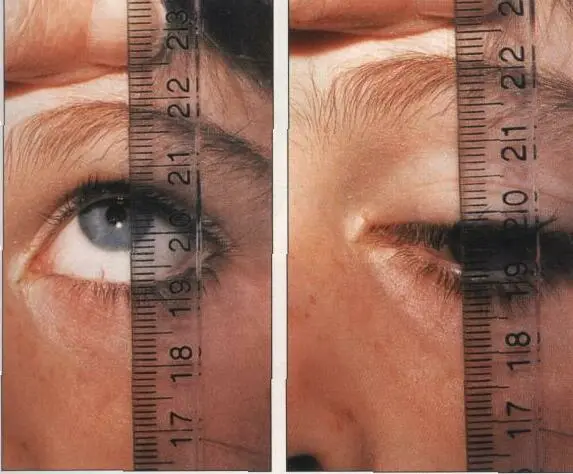
Proptosis
Cause:
- Thyroid eye disease common in adults
- Orbital Cellulitis & Benign Cystic Lesions in children
Investigation: (to exclude orbital tumor)
- CT
- MRI
Differential diagnosis
-
Trauma (retrobulbar hemorrhage)
-
Orbital inflammatory pseudotumor
-
Orbital infectious cellulitis
-
Orbital tumors (benign or malignant)
-
Lacrimal gland tumors
-
Carotid-cavernous fistula
-
Orbital varix
-
Orbital pseudotumor, orbital cellulitis, cavernous sinus thrombosis, intraorbital neoplasm
For Orbital Tumours most common Retinoblastoma never cause proptosis in children. In children, proptosis can be due to rhabdomyosarcoma (malignant), benign orbital cellulitis. In adults, causes include thyroid eye disease and cavernous hemangioma. Z

Exophthalmos
Proptosis + Lid retraction First sign is lid retraction
Floor Fractures


Orbital Fractures
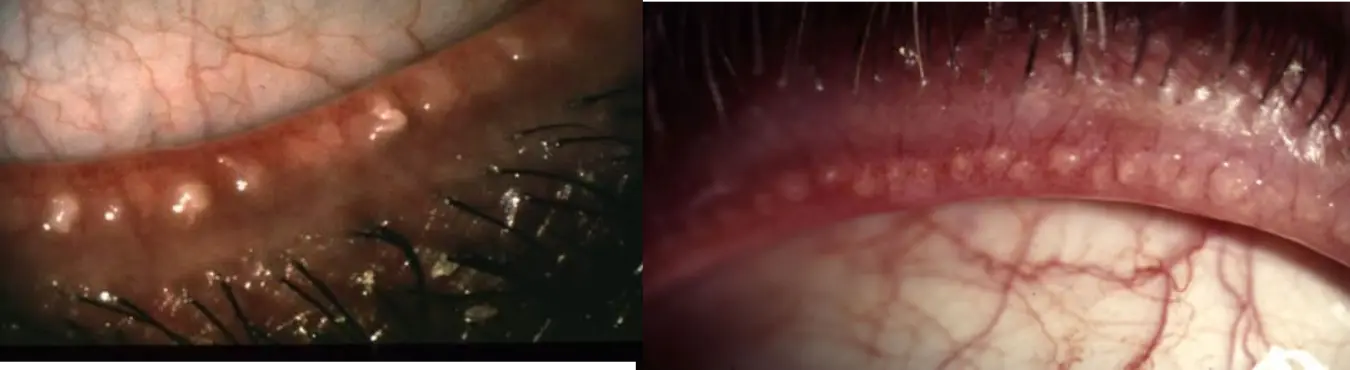
Molluscum contagiosum. Y
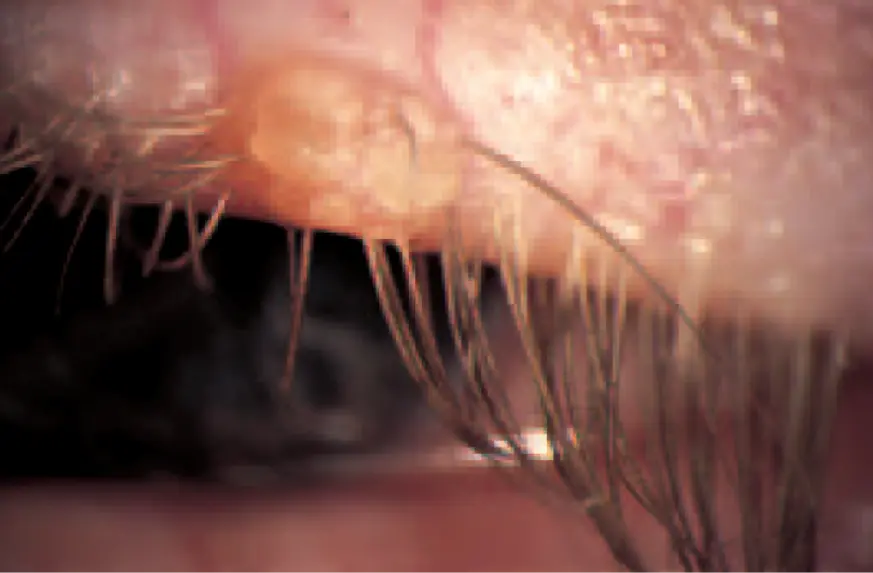 #Y
#Y

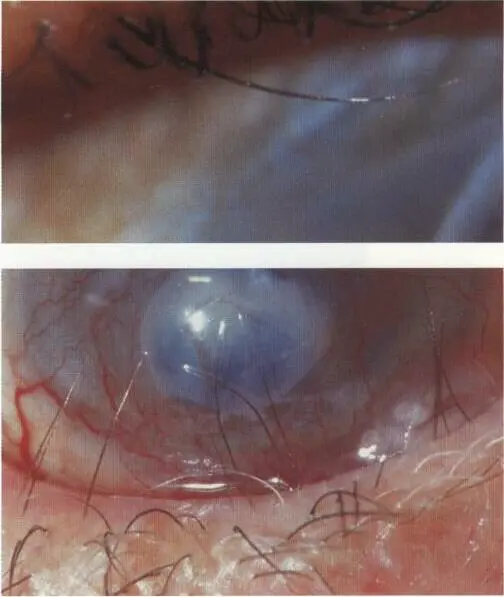
Herpes zoster ophthalmicus
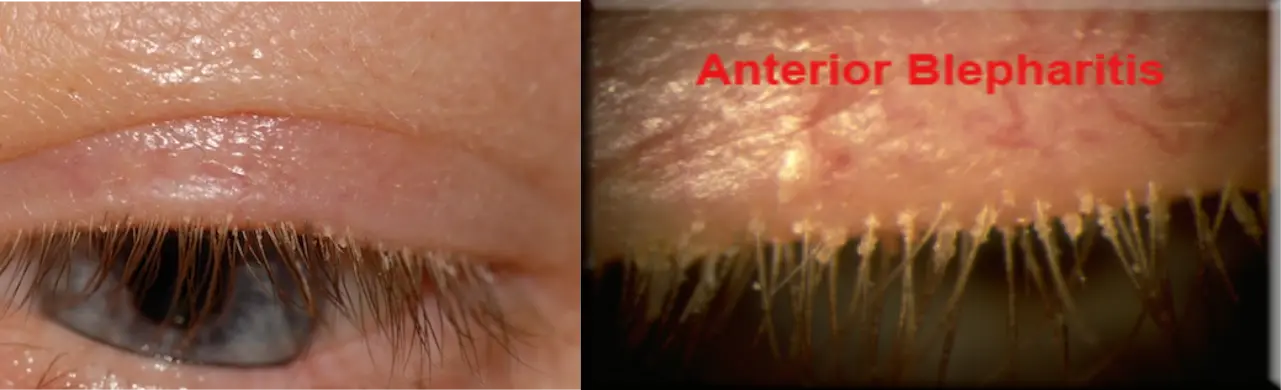
Anterior Blepharitis (infection of lid margin)
Causative Organism Staphylococcus
Posterior Blepharitis (infection of lid margin)
Name the condition: Posterior or anterior Blepharitis What organism: Staphylcoccus aureus Treatment:
-
Lid Hygiene: (Cornerstone)
- Warm compresses
- Lid massage
- Lid cleaning/scrubs
-
*Topical Medications:
- Antibiotics (to reduce bacteria)
- Steroids (short-term, for inflammation)
- Artificial tears (especially lipid-based)
-
*Oral Medications: (For persistent/severe cases)
- Tetracyclines (e.g., Doxycycline) or Azithromycin (anti-inflammatory effects)
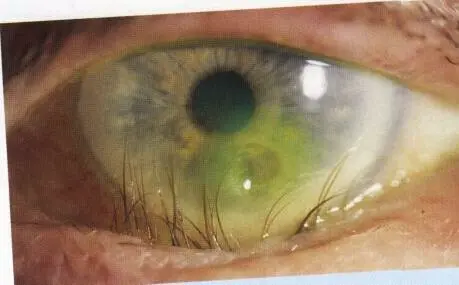
Squamous cell carcinoma Y

Disease of Lashes

Trichiasis
- Rubbing lashes
- Complication: Corneal irritation, Corneal ulcers
- Treatment: 1- simple removal (however recurrent) 2- cryo or laser therapies 3- surgery in some selective cases


Senile ectropion
- Complications: Dryness
Paralytic ectropion

Cicatricial ectropion
Most Common Complication Severe dryness
Senile entropion

Cicatricial entropion
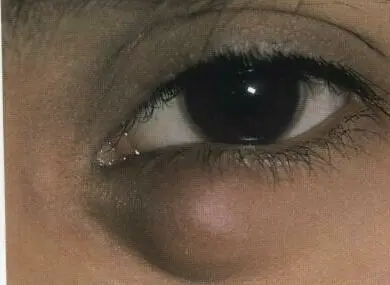
Lacrimal Presentation

Dacryocystitis
located Away from eyelid margin what’s the appropriate treatment? DCR
Nasolacrimal Duct System
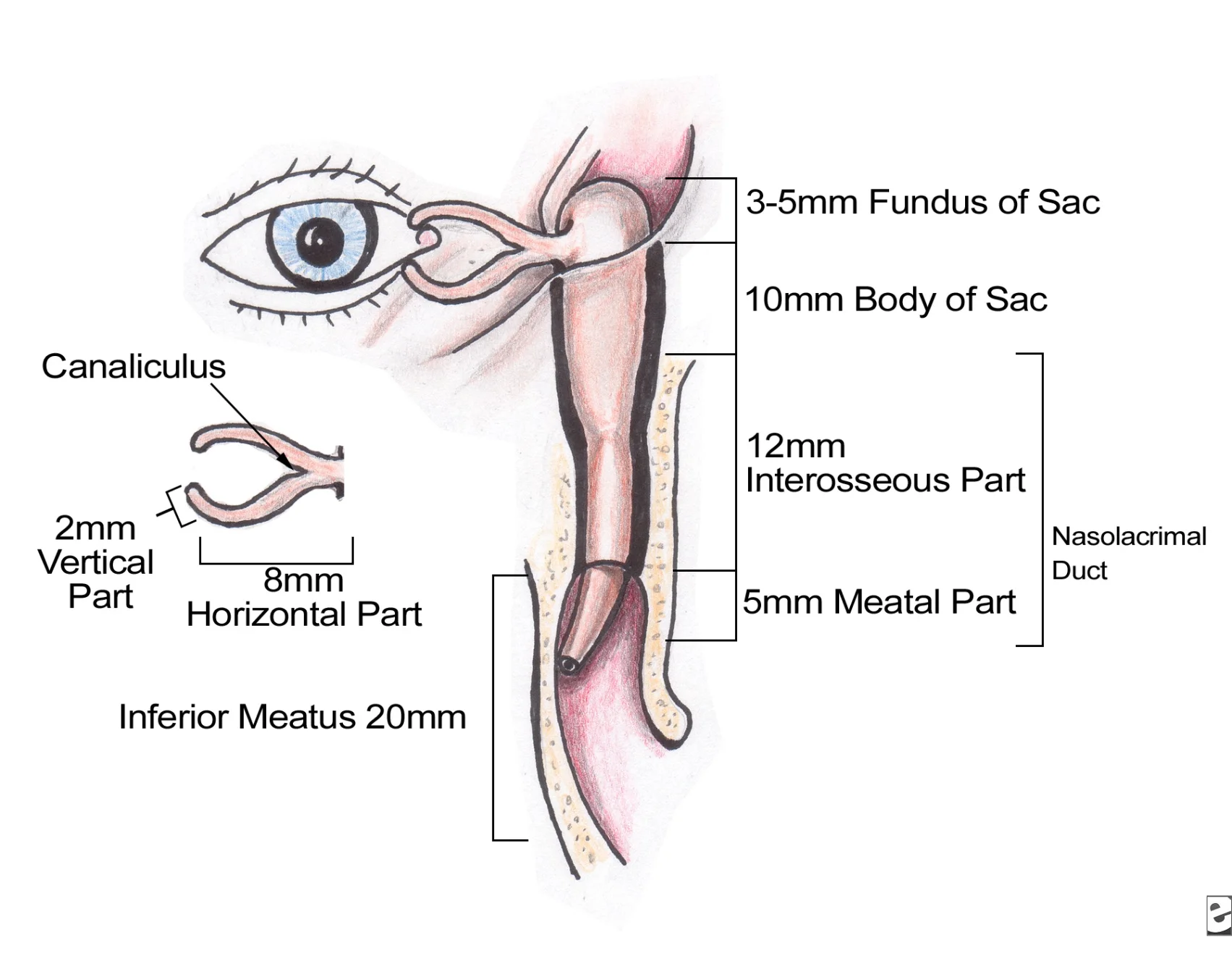
Classification of Nasolacrimal Duct Obstruction
- Congenital NLD obstruction.
- Acquired NLD obstruction.
Examination of Lacrimal System
- The eyelids contour and position.
- The dynamics of eyelid closure.
- The puncta size and position.
- The lacrimal sac swelling and presence of regurgitation on pressing on the sac.
- Irrigation of the NLS.

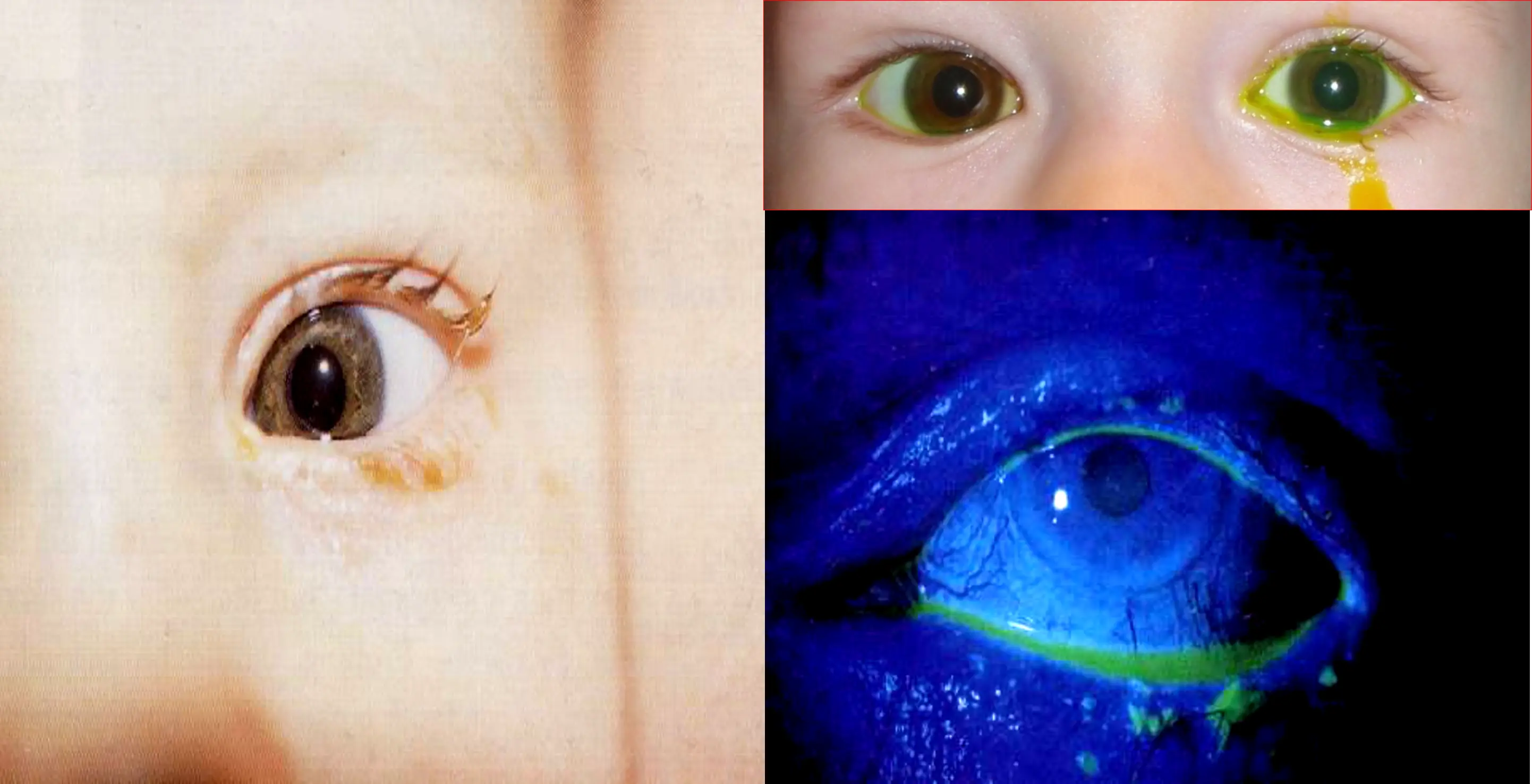
Congenital Nasolacrimal Duct Obstruction
- Symptoms
- Signs
- Dye Disappearance Test.
- Management:
- Massage of the lacrimal sac.
- Topical antibiotics.
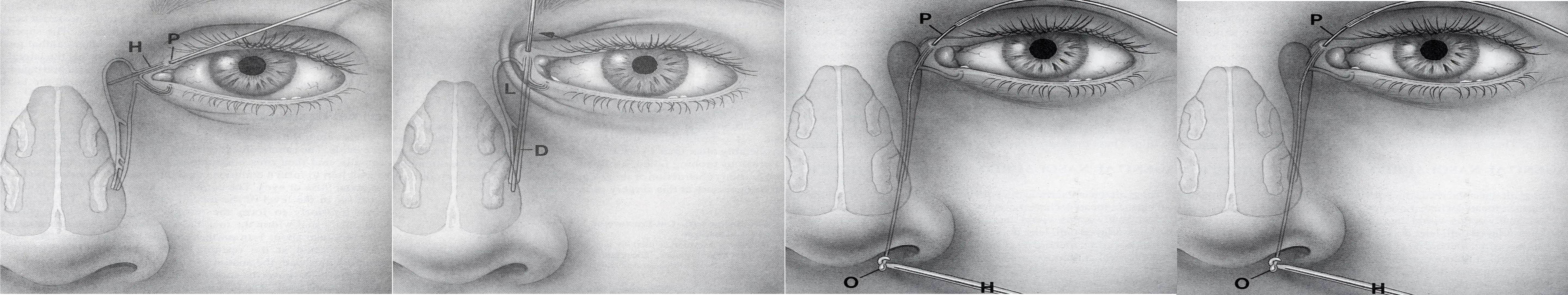
- Probing and syringing ± stenting after the age of 1 year.
 Obstruction in the nasolacrimal system
Dacryocystorhinostomy
Obstruction in the nasolacrimal system
Dacryocystorhinostomy
Eyelid Trauma
-
Types
- Blunt
- Sharp/penetrating
-
Classification
- Lid margin
- Not involved
- Involved*
- Canthal involved*
- Canalicula involved*
- Lid margin
Call ophthalmology
Globe Rupture or Laceration
- Stop examination.
- Keep NPO.
- Shield the eye.
- Give tetanus prophylaxis.
- Refer immediately to Ophthalmologist.
Lid Margin Sparing
- Skin and orbicularis only → skin sutures
- Fat protrusion = septum violated
- Make sure the levator muscle and globe are not involved.