Dr. Nada Abdelrahman
3,7 - extrinsic 12, 11, 9, 8 - Intrinsic 10 - Common Pathway
Learning Outcomes
- Explain the normal physiology of Blood haemostasias.
- Classify bleeding disorders
- Outline the aetiology of Haemophilias, their presentations, and management
- Outline the aetiology of VWF, its presentations and management
- Outline the aetiology of ITP, its presentations, and management
Stages of Blood Haemostasis
-
Primary Hemostasis Primary hemostasis formation of the weak platelet plug ⇒ vessel defects & Platelet disorders
- Triggered by injury.
- Involves the vessel wall + platelets.
- Results in the formation of P platelet plug.
-
Secondary Hemostasis Strong fibrin clot activation of the coagulation pathway (intrinsic, extrinsic and common) ⇒ Coagulation factor: deficiency or inhibitors
- Involves the activation of plasma coagulation factors.
- Leads to the formation of a stable fibrin clot.
- Fibrinolysis eventually dissolves the fibrin clot.
What Causes Bleeding Disorders?
Classification of Bleeding Disorders
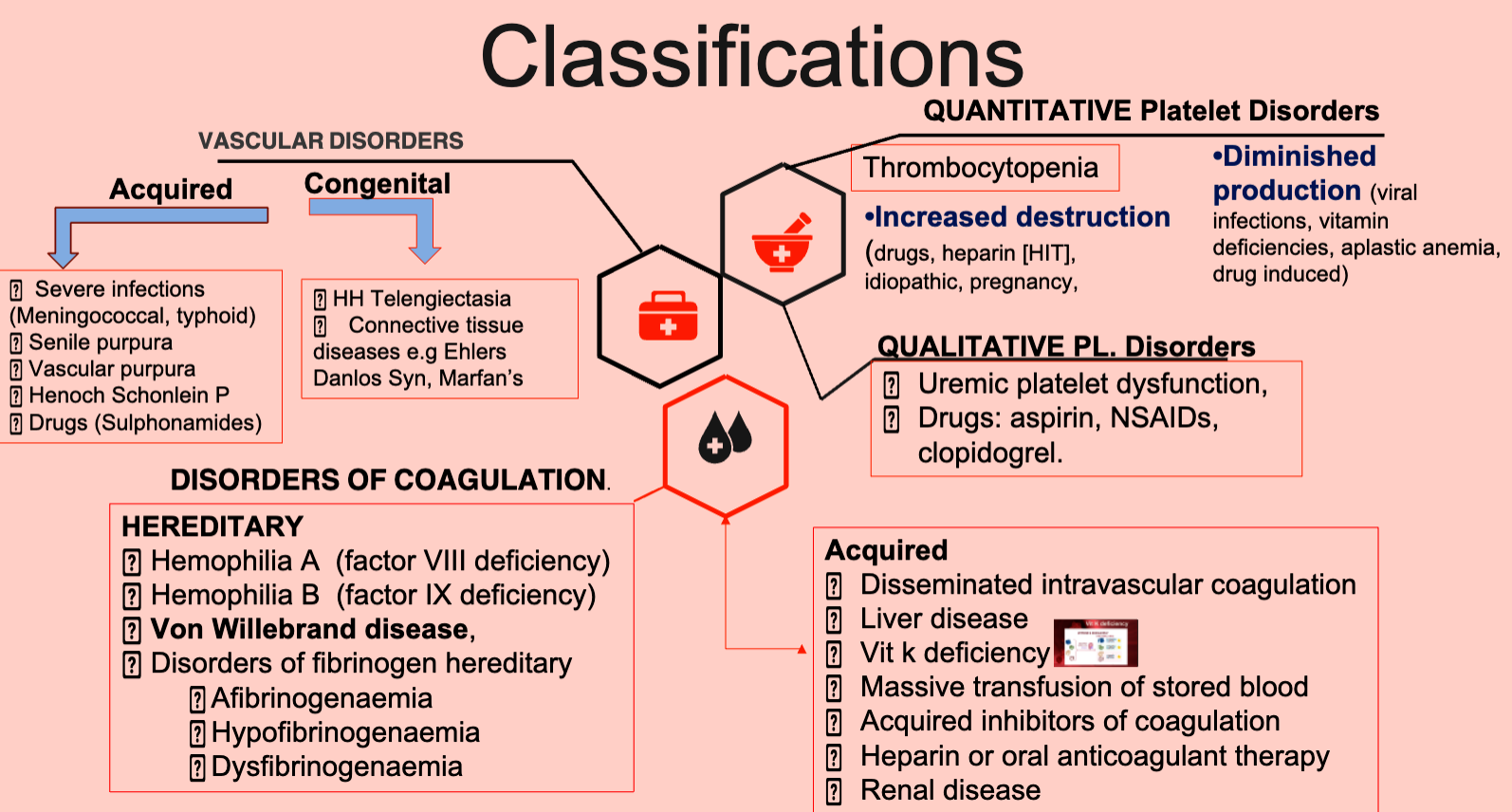
Bleeding disorders can be broadly classified into:
- Vessel Defects
- Platelet Disorders
- Quantitative: Thrombocytopenia (increased destruction or diminished production)
- Qualitative: Uremic platelet dysfunction, drug-induced (aspirin, NSAIDs, clopidogrel)
- Coagulation Factor Deficiencies or Inhibitors
- Mixed Platelet and Coagulation Disorders; Von Willebrand’s Disease
Vascular Disorders
-
Acquired:
- Severe infections (meningococcal, typhoid)
- Senile purpura
- Vascular purpura
- Henoch-Schönlein purpura
- Drugs (sulfonamides)
-
Congenital:
- Hereditary hemorrhagic telangiectasia
- Connective tissue diseases (e.g., Ehlers-Danlos syndrome, Marfan’s syndrome)
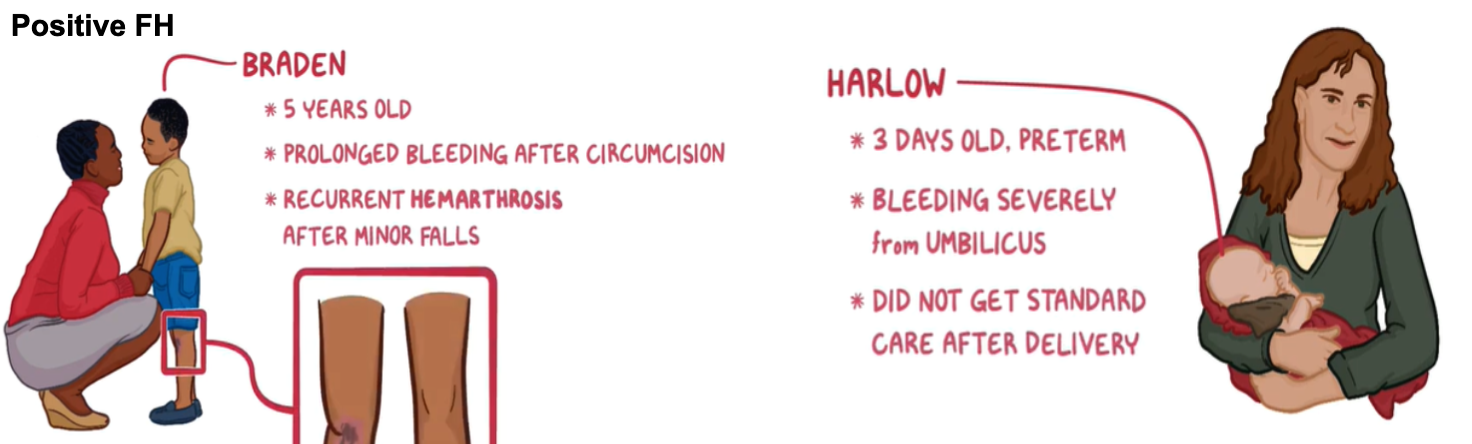
APPROACH TO A PATIENT OF BLEEDING DISORDERS
CLINICAL EVALUATION (H & E)
- HISTORY: Age of first manifestation
- FH: maternal relative with a bleeding Dis
- Bleeding spontaneous or after trauma; circumcision, or from dental procedures or cephalohematoma
- Time of manifestation after injury
- Ease with which bleeding is controlled
- Drug history
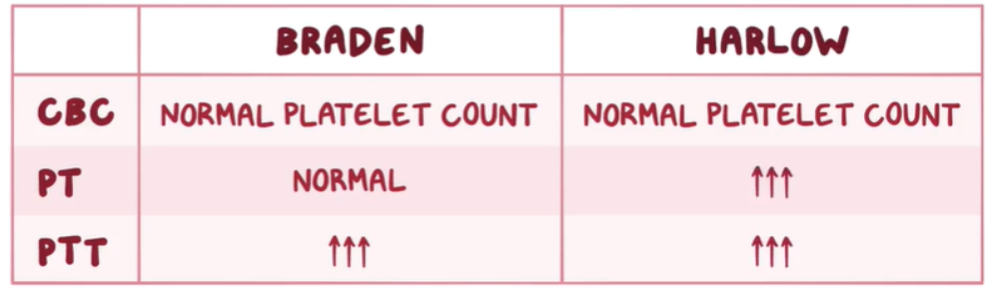
Laboratory Approach
- First line screening tests.
- Second line specific tests
Coagulation Disorders
Hereditary:
- Hemophilia
- Hemophilia A (factor VIII deficiency)
- Hemophilia B (factor IX deficiency)
- Von Willebrand’s Disease
- Disorders of fibrinogen (afibrinogenemia, hypofibrinogenemia, dysfibrinogenemia)
- Acquired:
- Disseminated intravascular coagulation
- Liver disease
- Vitamin K deficiency
- Massive transfusion of stored blood
- Acquired inhibitors of coagulation
- Heparin or oral anticoagulant therapy
- Renal disease
Question on aPTT
PT = extrinsic sys ⇒ common
Activated partial thromboplastin time measures the intrinsic system and the final common pathway
Question on Hemophilia Inheritance
A 24-year-old woman, gravida 1, para 0, at 12 weeks’ gestation comes to the office for her monthly antenatal visit. She says that her father died soon after she was born due to excessive bleeding from head trauma. Her father’s maternal grandfather also had bleeding problems. She is concerned that her unborn child may have the same medical problem and wants a genetic test. She does not have any past or current medical conditions. Her husband also has no past or current medical conditions but reports a family history of hypertension. Which of the following illustrates the risk of the patient’s unborn child being affected by the disorder?
A. 0% chance regardless of the sex
B. 100% chance if the fetus is a male
C. 50% chance if the fetus is a male
D. 25% chance if the fetus is a male
E. 25% chance if the fetus is a female