Multiple Pregnancy
Key Facts
- About 1 in 80 pregnancies at term
- incidence is rising with increasing maternal age and assisted conception.
- The second twin is at greater risk of intrapartum compromise.
- Vaginal birth is usually safely achievable where the presenting twin is in a cephalic vertex presentation.
- Caesarean section performed If the first twin presents by the breech or transverse.
Associated Complications
- abnormal fetal growth
- malpresentation
- CTG abnormalities
- cord prolapse
- need for emergency caesarean section in labour
- PPH.

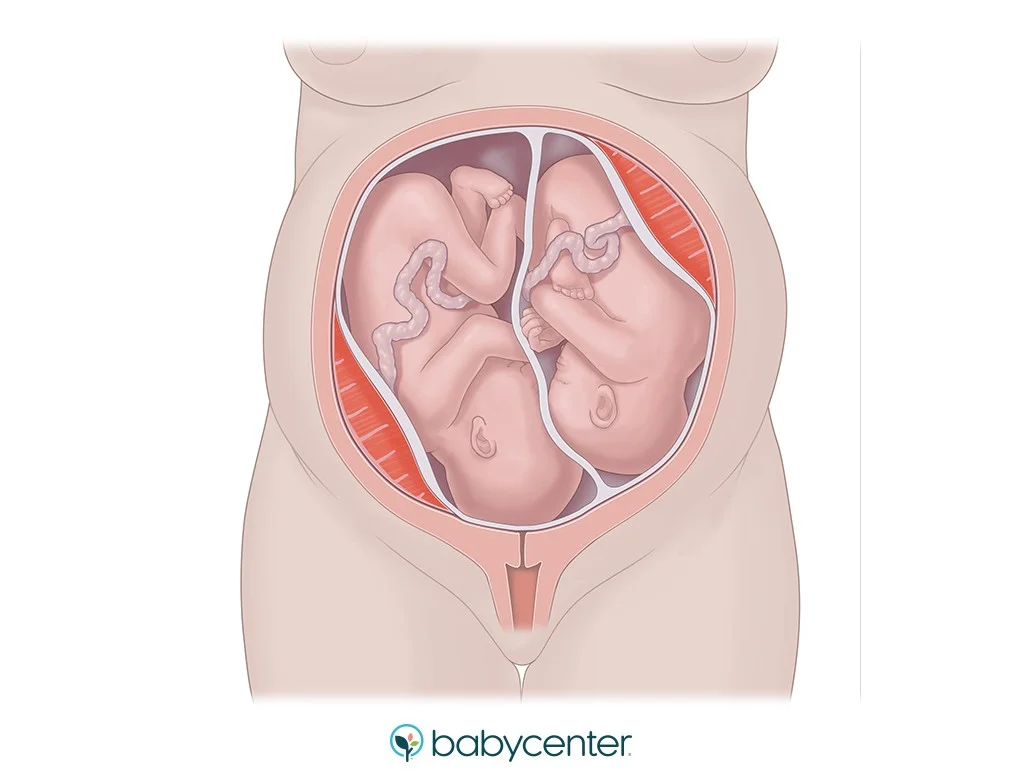
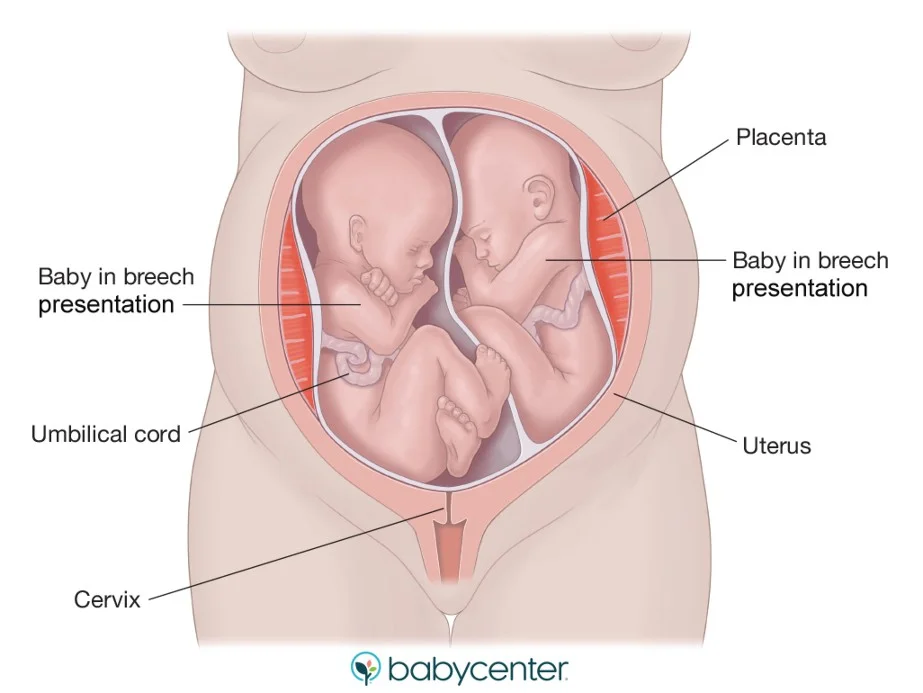
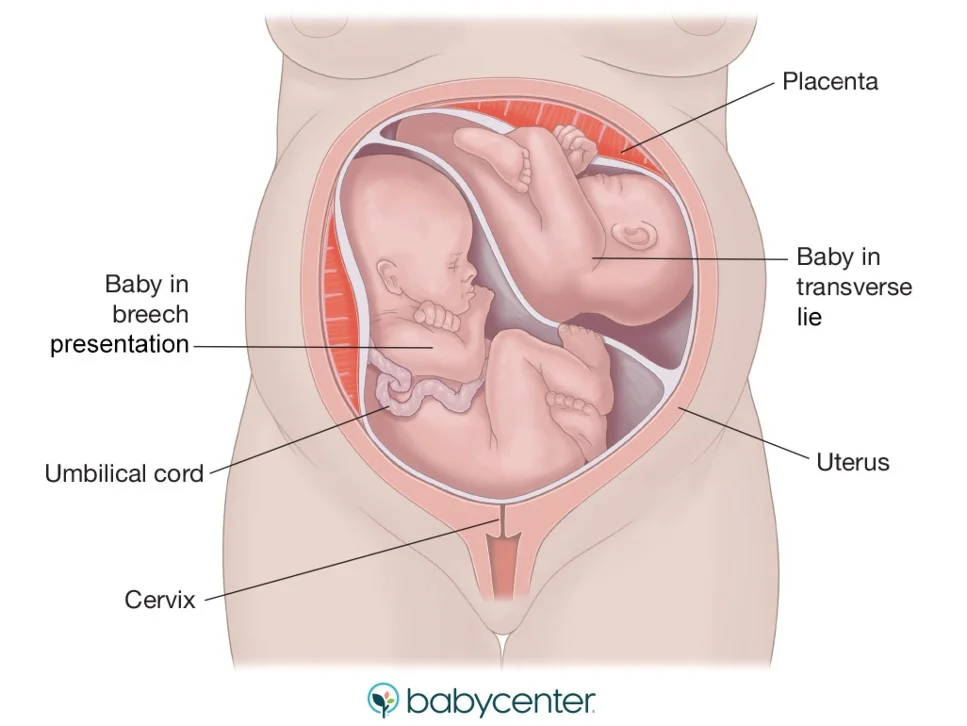
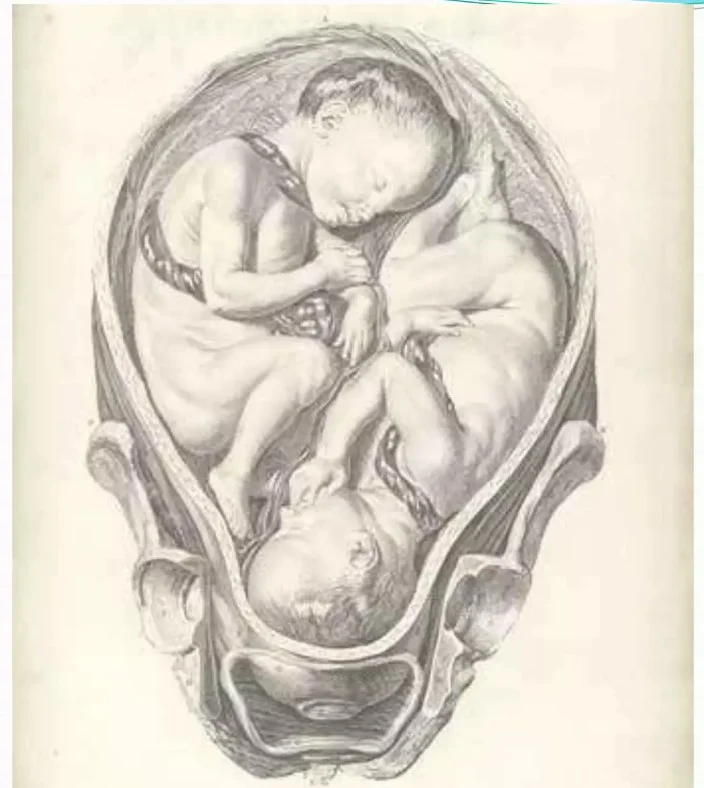
Twins in Different Positions
Scenarios
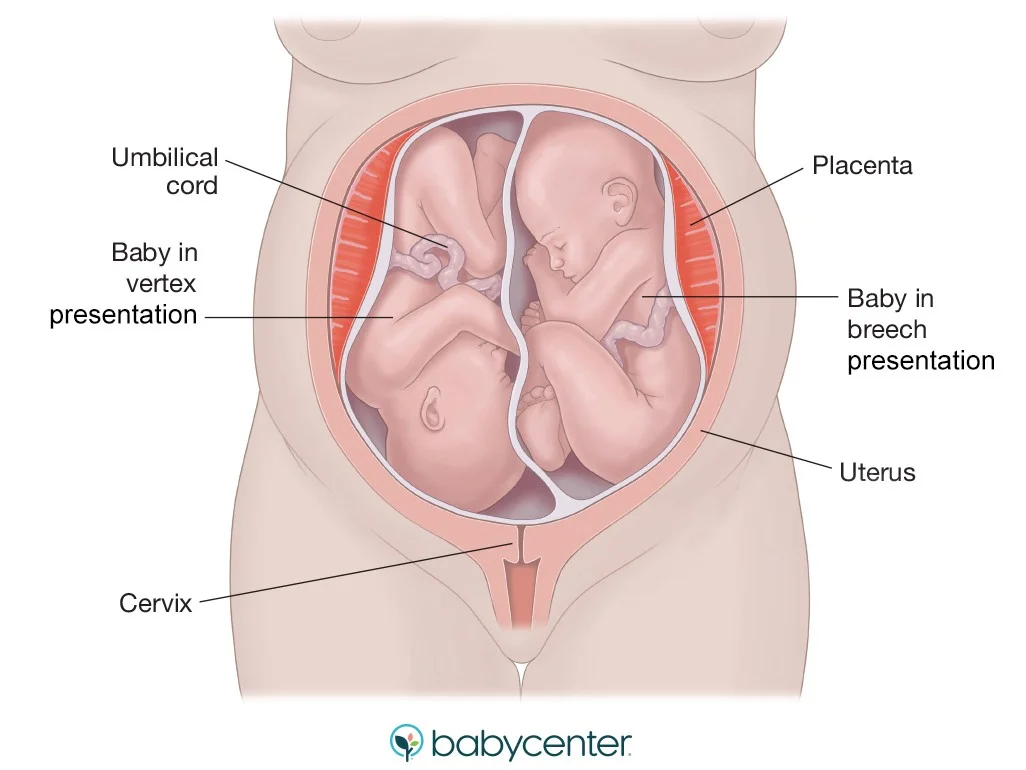
Delivery of Twins
Steps
- Vaginal birth if the first twin is in a cephalic (vertex) presentation.
- Caesarean section performed If the first twin presents by the breech or transverse.(not cephalic)
- Delivery of the 2nd twin:
- After the delivery of the 1st twin:
- ✔ clamp the cord.
- ✔ Determine the position of the 2nd twin.
- ✔ Bring the nearest pole (breech or cephalic).
- ✔ Do ARM & give oxytocin iv.
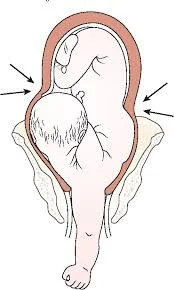
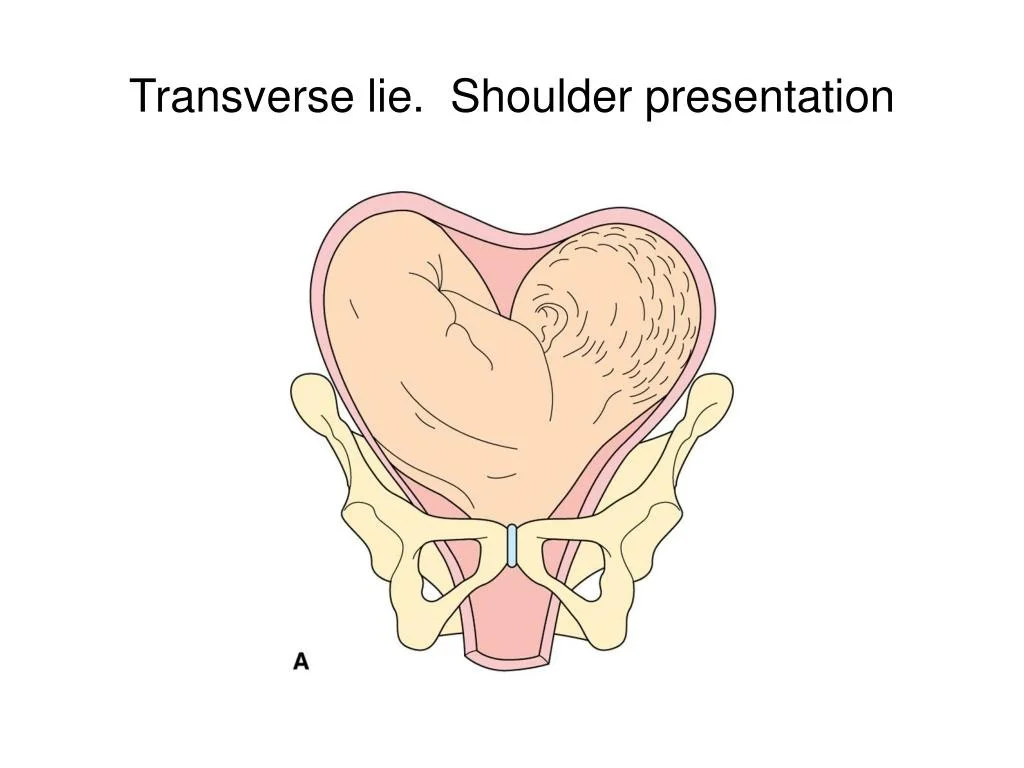
Shoulder Presentation
Causes and Management
- Shoulder presentation occurs as the result of a transverse or oblique lie of the fetus.
- Causes include:
- placenta praevia.
- high parity.
- pelvic tumour.
- uterine anomaly.
- Delivery should be by caesarean section.
- Delay:
- cord prolapse.
- uterine rupture.
Multiple Pregnancy
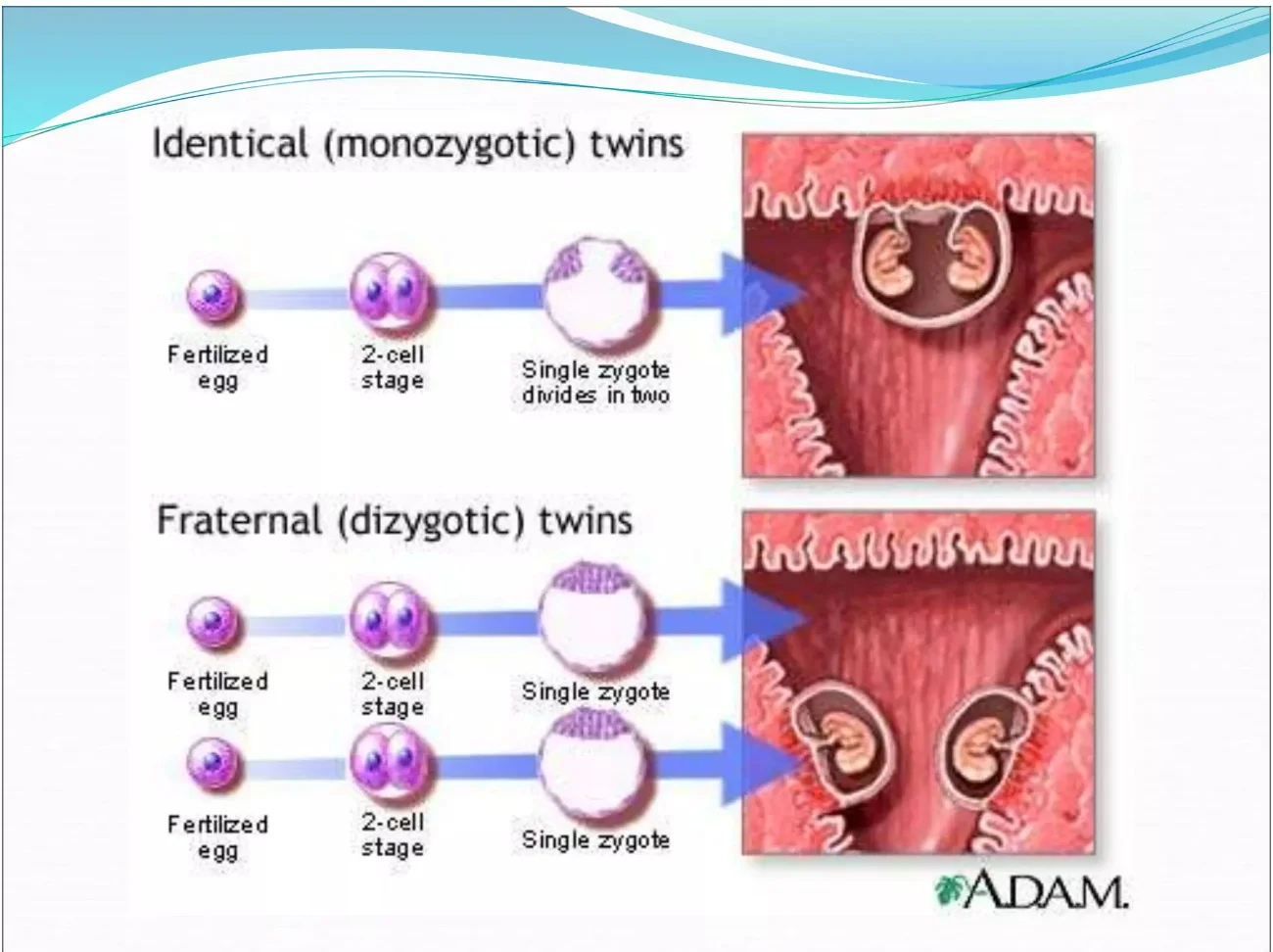
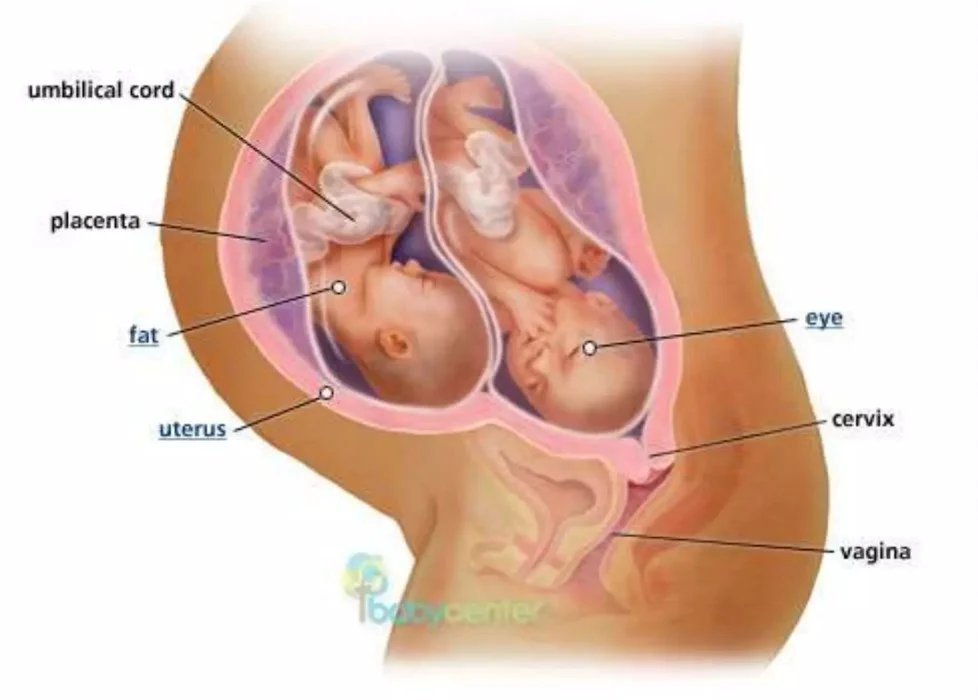
DIZYGOTIC TWINS
- Most common represents 2/3 of cases.
- Fertilization of more than one egg by more than one sperm.
- Non identical may be of different sex.
- Two chorion and two amnion.
- Placenta may be separate or fused.
Factors Affecting Dizygotic Twins Incidence
Factors
- Induction of ovulation, 10% with clomide and 30% with gonadotrophins.
- Increase maternal age? Due to increase gonadotrophins production.
- Increases with parity.
- Heredity usually on maternal side.
- Race; Nigeria 1:22 North America 1:90.
MONOZYGOTIC TWINS
- Constant incidence of 1:250 births.
- Not affected by heredity.
- Not related to induction of ovulation.
- Constitutes 1/3 of twins.
Identical (Monozygotic) Twins vs Fraternal (Dizygotic) Twins
Identical (Monozygotic) Twins
- Fertilized egg
- 2-cell stage
- Single zygote divides in two
Fraternal (Dizygotic) Twins
- Two separate fertilized eggs
- Two separate zygotes
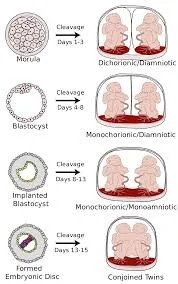
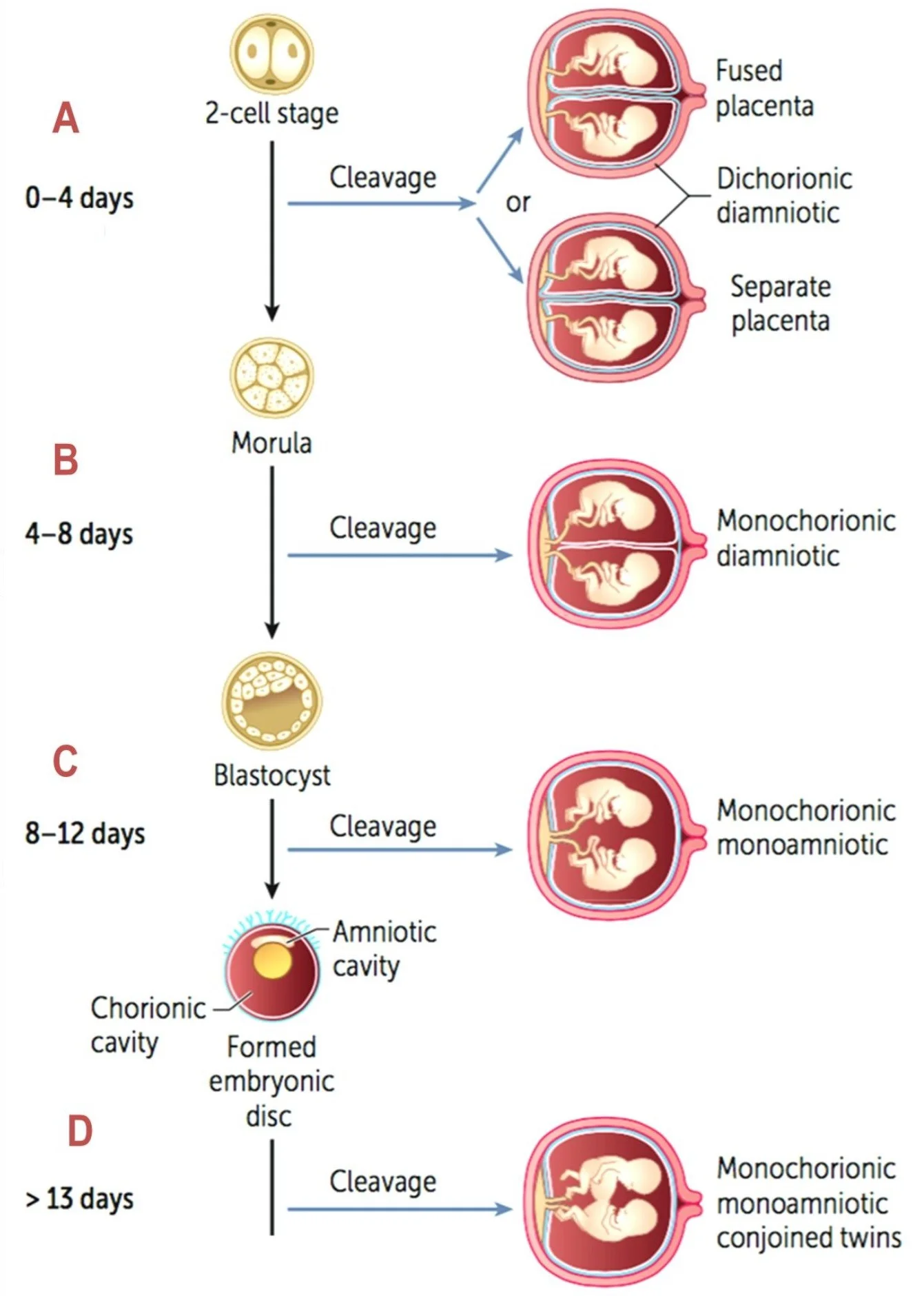
Twinning Cleavage Stages
Stages
- 0-4 days
- 2-cell stage
- Cleavage results in:
- Dichorionic diamniotic with Fused placenta or Separate placenta
- 4-8 days
- Morula
- Cleavage results in:
- Monochorionic diamniotic
- 8-12 days
- Blastocyst
- Components:
- Chorionic cavity
- Amniotic cavity
- Formed embryonic disc
- Components:
- Cleavage results in:
- Monochorionic monoamniotic
- Blastocyst
- > 13 days
- Cleavage results in:
- Monochorionic monoamniotic conjoined twins
- Cleavage results in:
Monochorionic Twins
- 70% are diamniotic monochorionic.
- 30% are diamniotic dichorionic
Diagnosis of Zygosity


Determining Zygosity
- Different sex indicates dizygotic twins.
- Separate placenta indicate dizygotic twins.
Determination of Zygosity After Birth
- By examination of the MEMBRANE, PLACENTA, SEX, BLOOD GROUP.
- Examination of the newborn DNA and HLA may be needed in few cases.
Complications of Multiple Pregnancy
Maternal Complications
- Anemia
- Hydramnios
- Preeclampsia
- Preterm labour
- Postpartum hemorrhage
- Cesarean delivery
Fetal Complications
- Malpresentation
- Placenta previa
- Abruptio placenta
- Premature rupture of the membranes
- Prematurity
- Umbilical cord prolapse
- Intrauterine growth restriction
- Congenital anomalies
- TTTS
Monochorionic Complications
TWIN-TWIN Transfusion Syndrome (TTTS)
- Results from vascular anastomoses between twins vessels at the placenta.
- Usually arterial (donor) venous (recipient).
- Occurs in 10% of monochorionic twins.
- Chronic shunt occurs, the donor bleeds into the recipient so one is pale with oligohydramnios while the other is polycythemia with hydramnios.
- If not treated death occurs in 80-100% of cases.
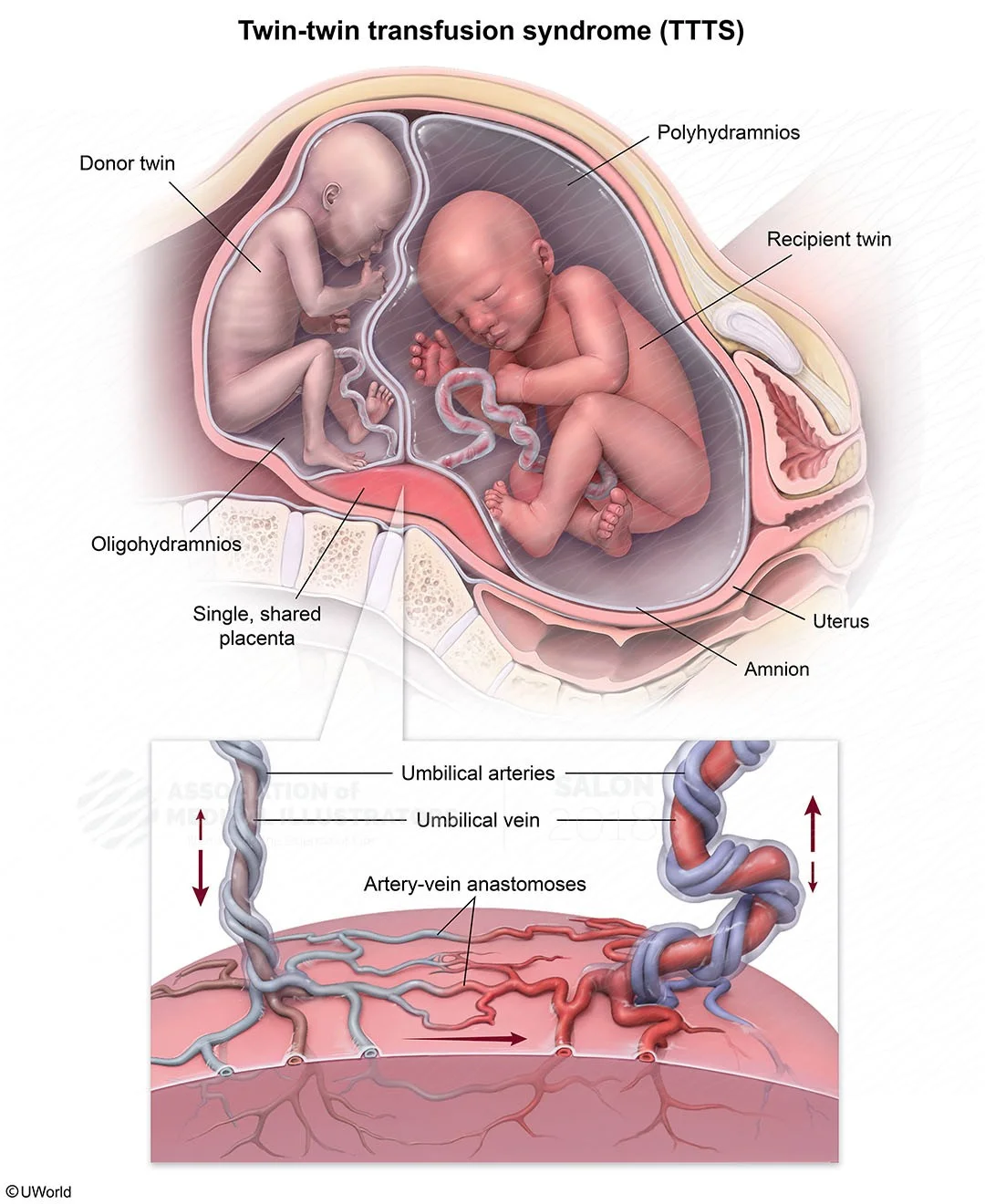
Possible Methods of Treatment for TTTS
- Repeated amniocentesis from recipient.
- Indomethacin.
- Fetoscopy and laser ablation of communicating vessels.

Severity Staging System for TTTSY
- The bladder is still visible in the donor twin.
- The bladder is no longer visible in the donor.
- Critically abnormal Doppler in either twin: absent-reverse diastolic flow in the donor or recipient umbilical artery and/or absent/reverse flow in the ductus venosus or pulsatile flow in the umbilical vein of the recipient.
- Hydrops in either fetus.
- Demise of one or both twins.
All Doppler measurements need to be done. A case cannot be staged unless umbilical artery, umbilical vein, and ductus venosus Dopplers have been performed.
Other Complications in Monochorionic Twins
- Congenital malformation. Twice that of singleton.
- Umbilical cord anomalies. In 3 - 4 %.
- Conjoined twins. Rare 1:70000 deliveries. The majority are thoracopagus.
- PNMR of monochorionic is 5 times that of dichorionic twins (120 vs 24/1000 births)
Diagnosis
- History
- Examination
- Ultrasound
Antenatal Care
Fetal Surveillance
- Monthly USS from 24 weeks to assess fetal growth and weight.
- A discordant weight difference of >25% is abnormal (IUGR).
- Weekly CTG from 36 weeks.
Methods of Delivery
Vertex-Vertex (50%)
- Vaginal delivery
Vertex-Breech (20%)
- Vaginal delivery by senior
Breech-Vertex (20%)
- CS is safer to avoid interlocking twins.
Breech-Breech (10%)
- Usually CS
- For Monochorionic twins
- CS
Perinatal Outcome Complications
- Perinatal mortality is 5 times more than singleton.
- RDS 50% more
- Incidence of stillbirth is twice that of singleton
- Anomaly
- Cerebral hemorrhage and asphyxia
- Cerebral palsy 4 times that of singleton.
Higher-Order Multiple Pregnancies
Triplets Quadruplets
