Haemostasis, & blood transfusion
Moneer Almadani
Objectives
- Introduction
- Coagulation pathway
- Blood disorders
- Surgical haemorrhage
- Blood transfusion
- Indication
- Complications
- Massive blood transfusion
Introduction
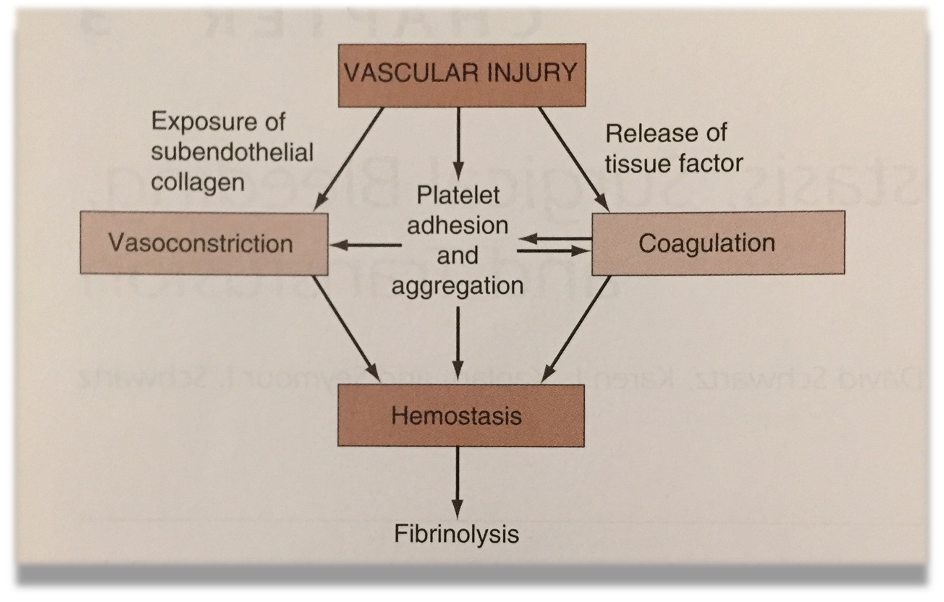 Haemostasis is a complex process that prevents or terminates blood loss from a disrupted intravascular space
Haemostasis is a complex process that prevents or terminates blood loss from a disrupted intravascular space
Stages:
-
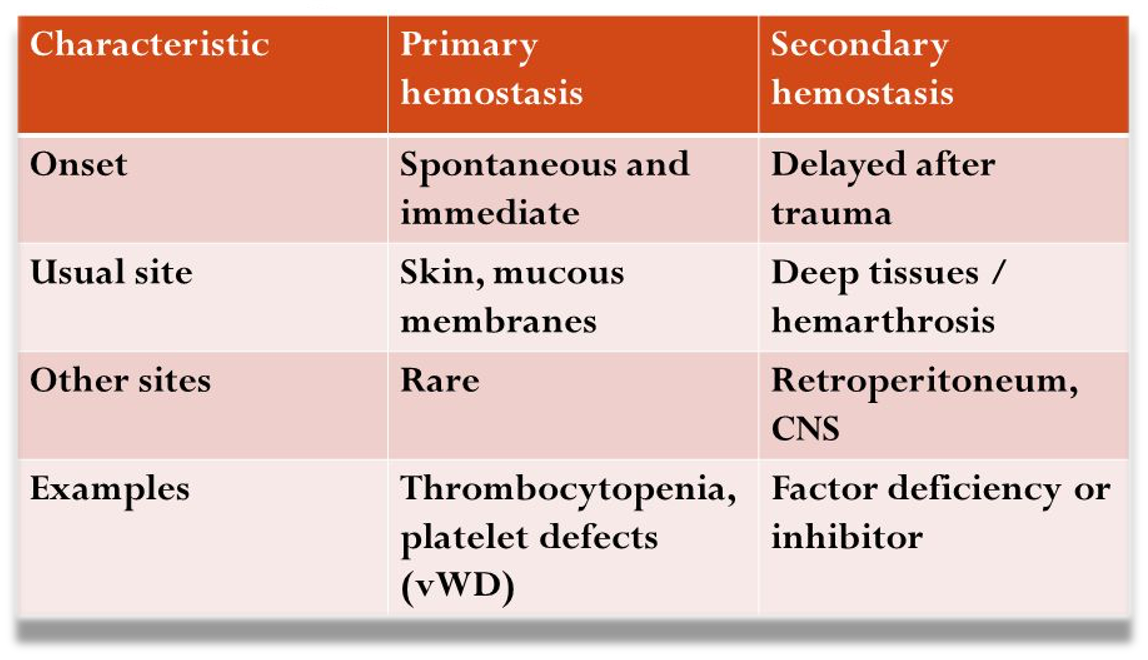
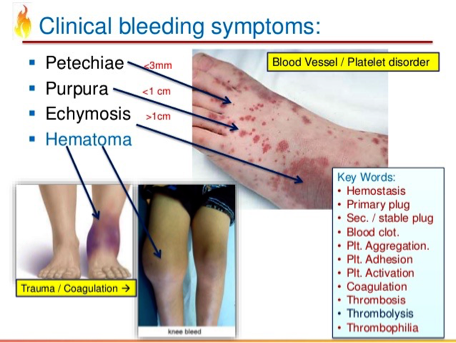
Primary haemostasis:
- Vasoconstriction
- Platelet plug formation
-
Secondary haemostasis: 3) Blood clotting -coagulation- (fibrin formation) 4) Fibrinolysis
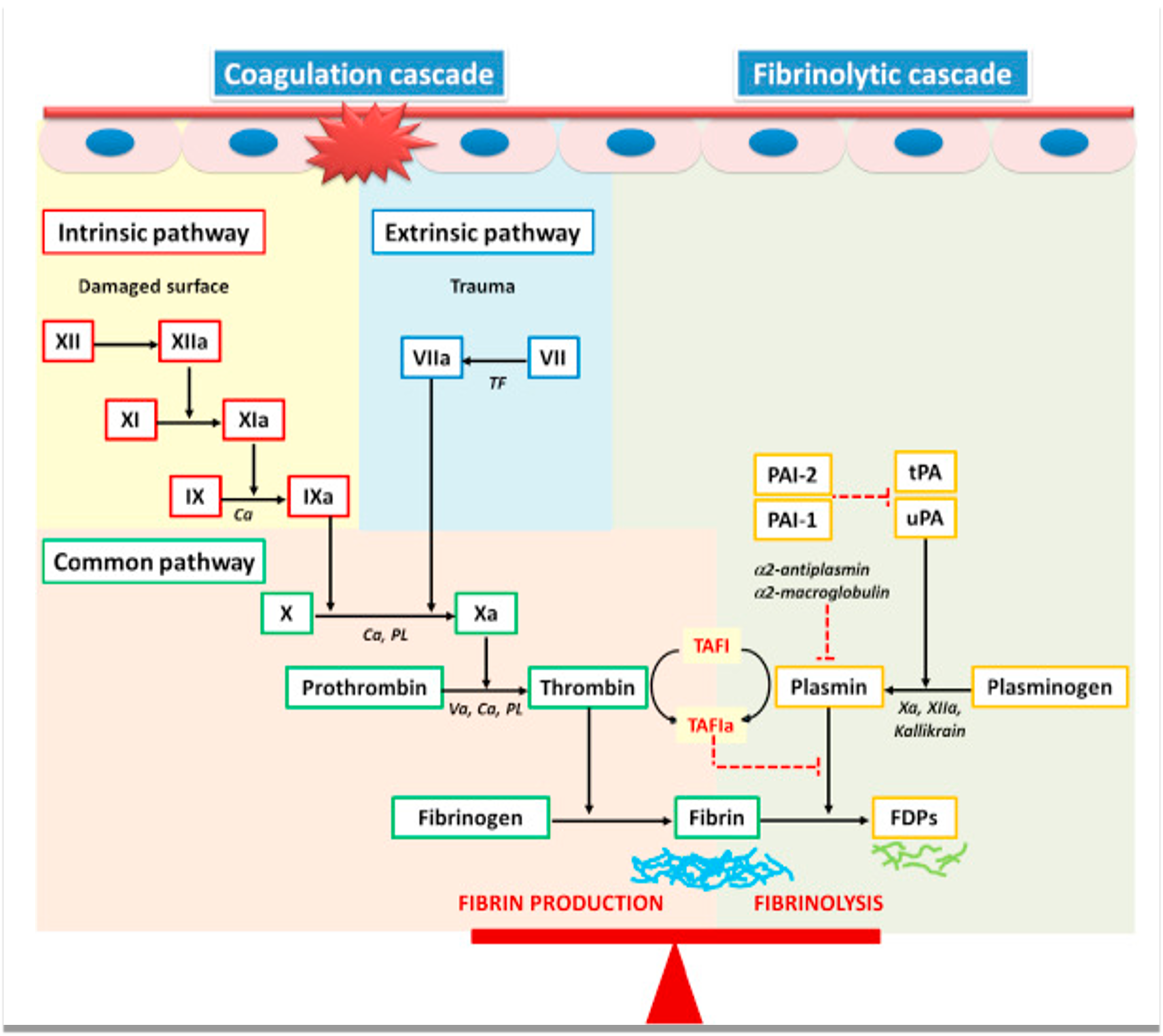
Coagulation pathway
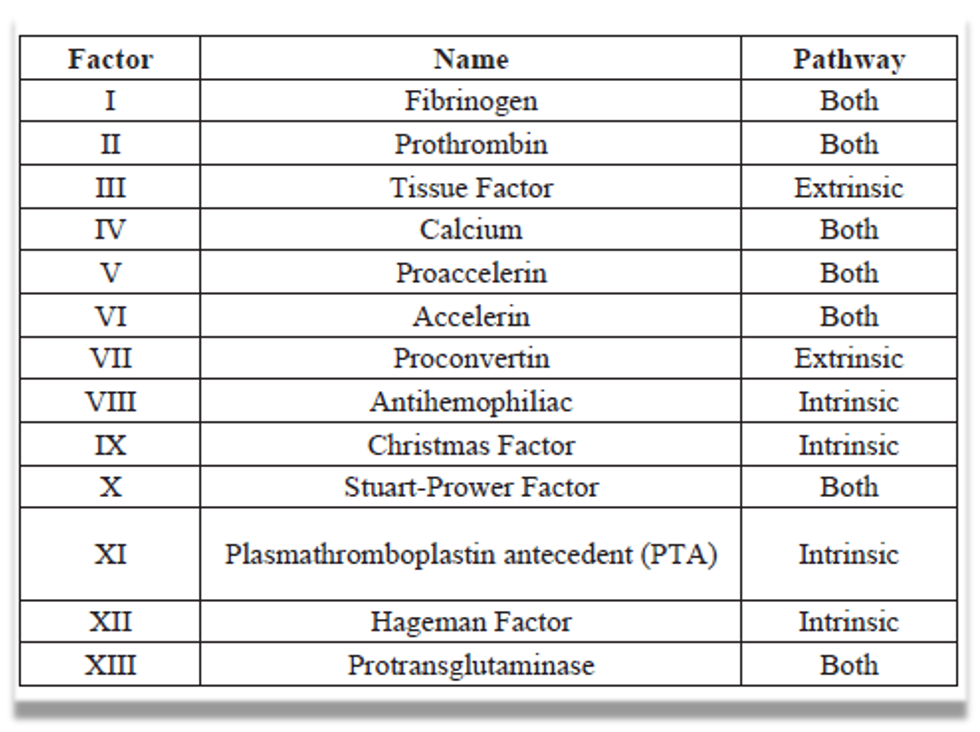
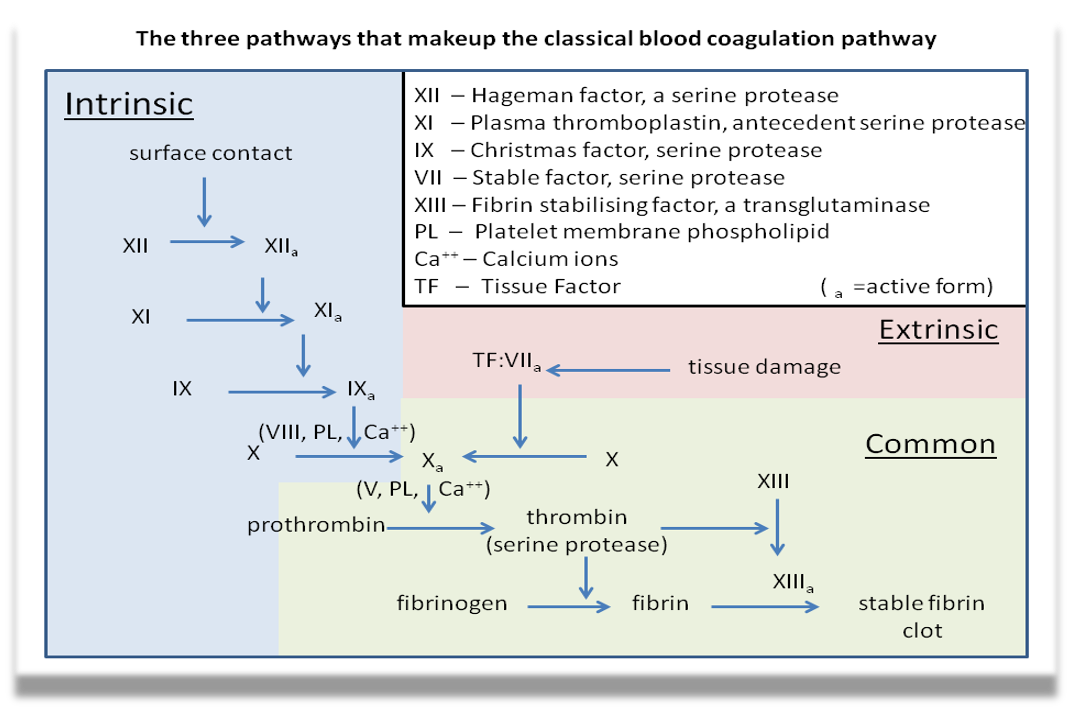 Intrinsic Factor
Surface contact XII-IX a = X (VIII, PL< Ca++) ⇒ X a
Intrinsic Factor
Surface contact XII-IX a = X (VIII, PL< Ca++) ⇒ X a
Intrinsic Factor Tissue Damage TF: VII a ⇒ X = X a
Common Pathway X a + (V, PL, Ca++) + Prothrombin ⇒ Thrombin ⇒ XIII ⇒ XIII a | v Fibronogen ⇒ Fibrin ⇒ XIIa = Stable fibrin clot
- PT is reported with the international normalized ratio (INR).
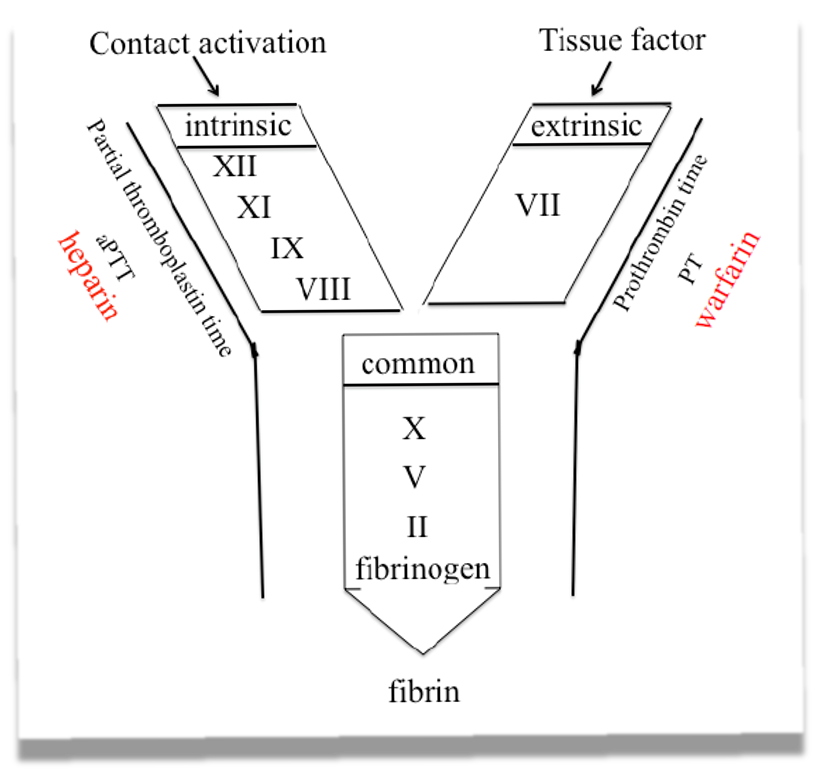 Extrinsic Pathway monitored by INR - affected by warfarin
Intrinsic Pathway monitored by aPTT - affected by Heparin
Extrinsic Pathway monitored by INR - affected by warfarin
Intrinsic Pathway monitored by aPTT - affected by Heparin
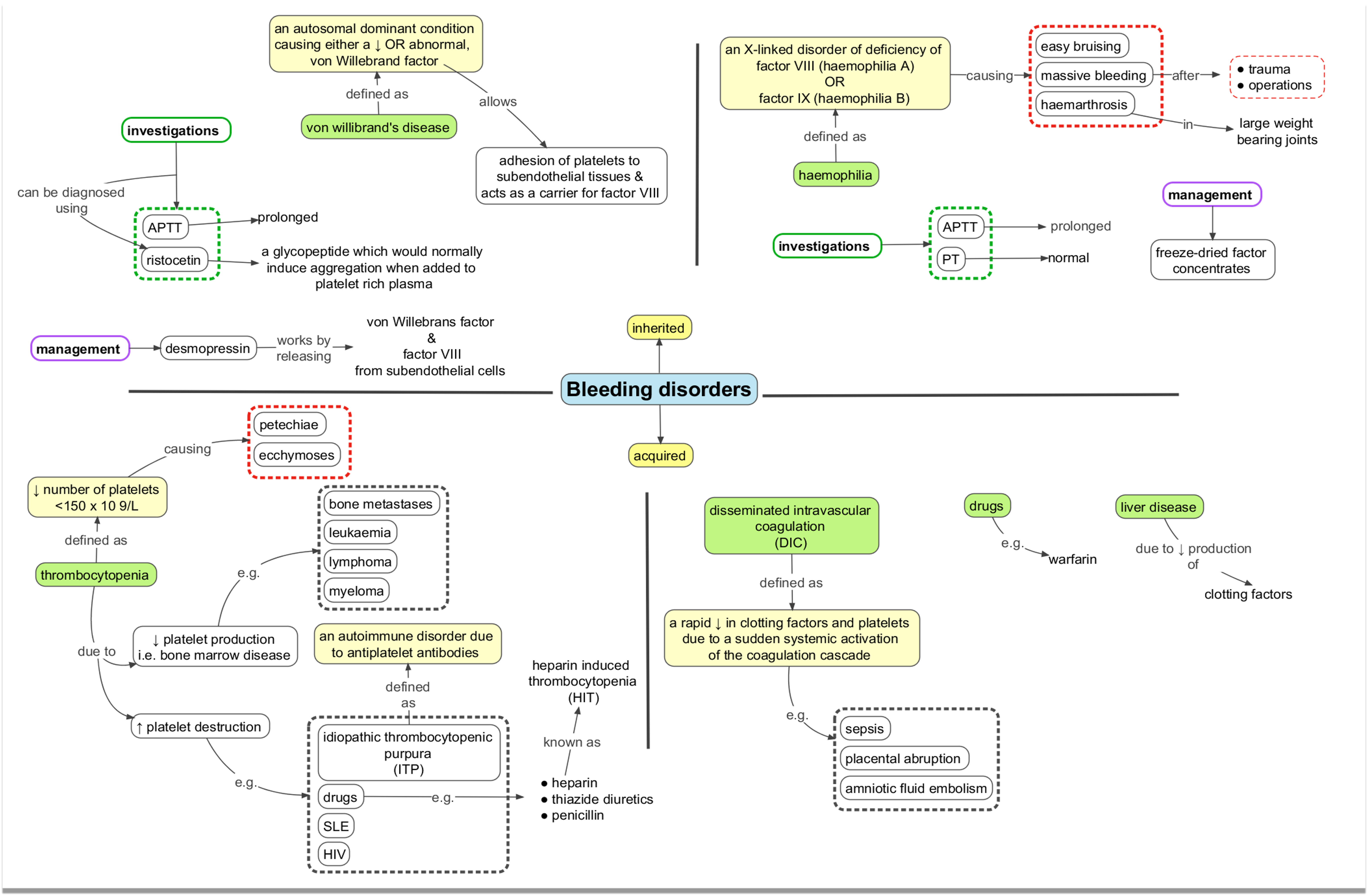
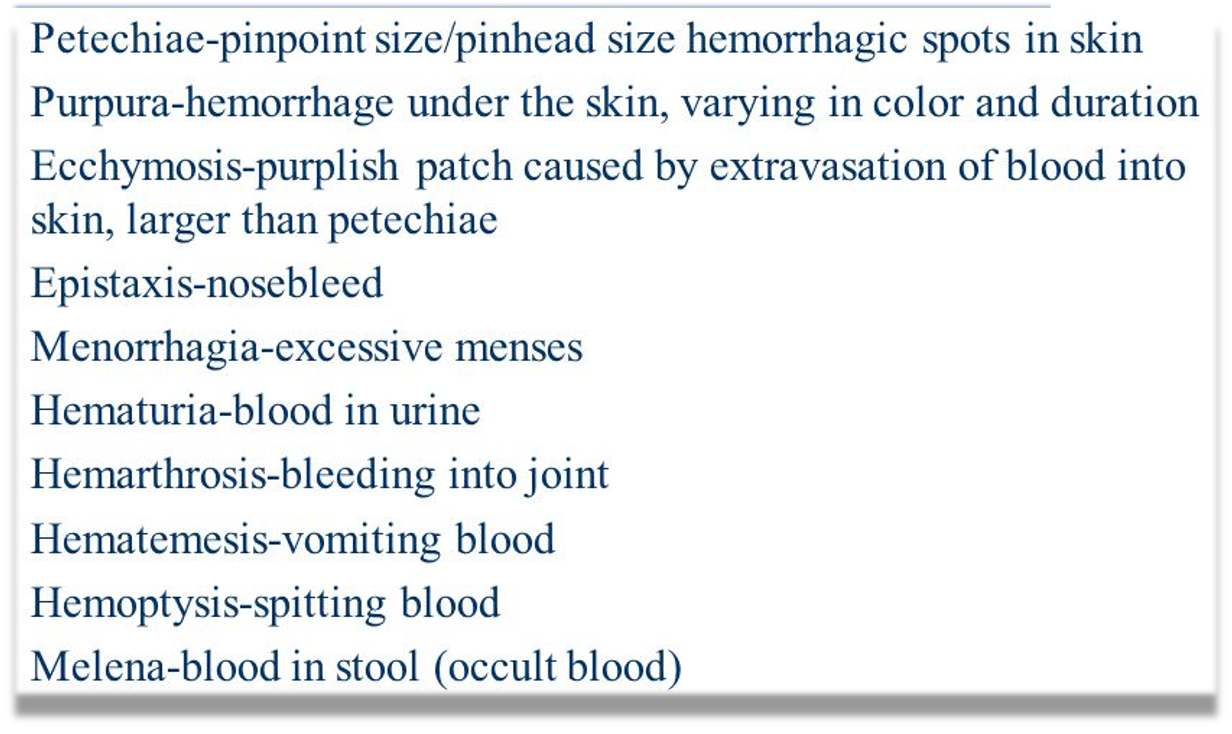
Blood disorders
Surgical haemorrhage
Primary: At the time of injury or surgery
Intermediate/ Reactionary: Within 24 h of injury or surgery
- Postop high BP, sneezing, coughing
Secondary: 48-72 h after injury or surgery
- Infection/ Sepsis
Blood transfusion
- 1 unit of PRBC has 300 ml, raise Hb around 1 gm
- PRBC could be stored up to 6 weeks
- Type and screen Vs type and cross match
- Thrombocytopenia
- Stop aspirin to restore Platelets function
- PLT should be at least 50,000 before surgery, less than 20,000 associated with bleeding
Fresh frozen plasma FFP:
- Replaces clotting factors
- No RBC, No PLT
Cryoprecipitate:
- Replaces fibrinogen
- VWF
- Some clotting factors
Studies have shown an association between anemia and increased mortality, It is not clear that correction of anemia will improve mortality. - Clear risk of postoperative death when the Hg fell below 7 g/dL

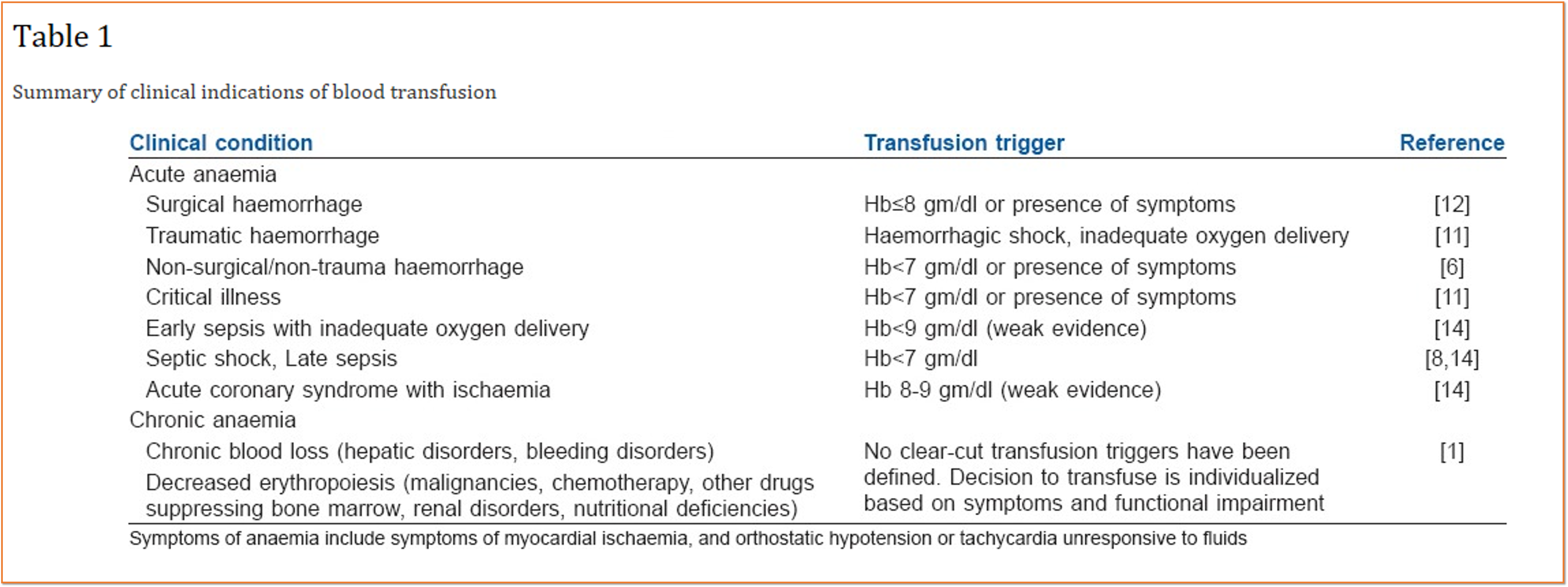
Indications of blood transfusion
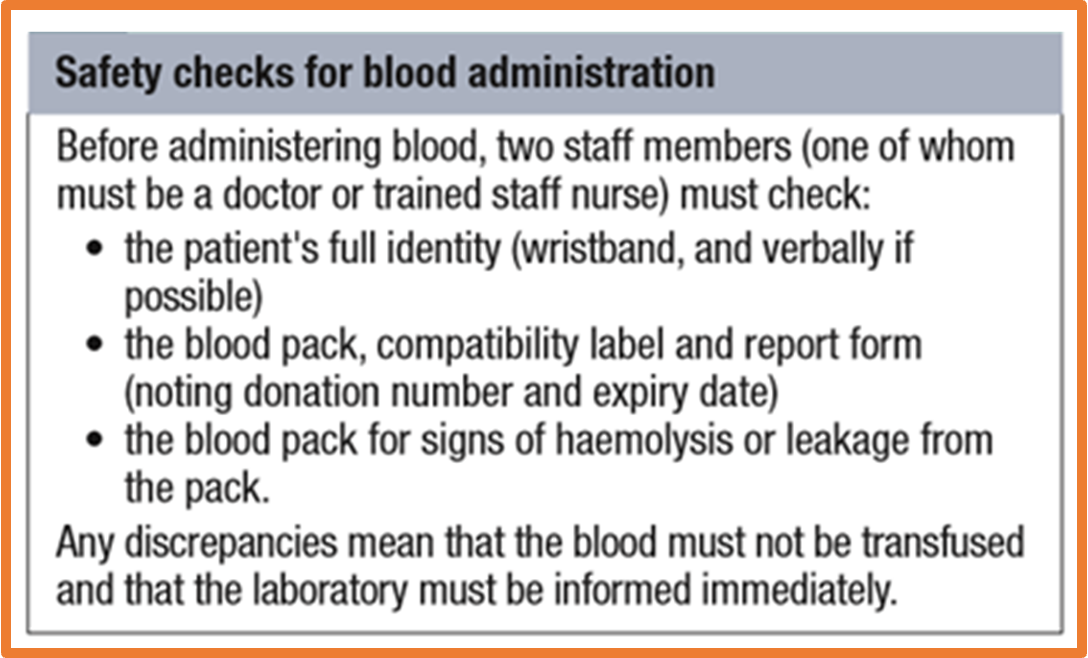
Steps prior to blood transfusion
Complications of blood Tx
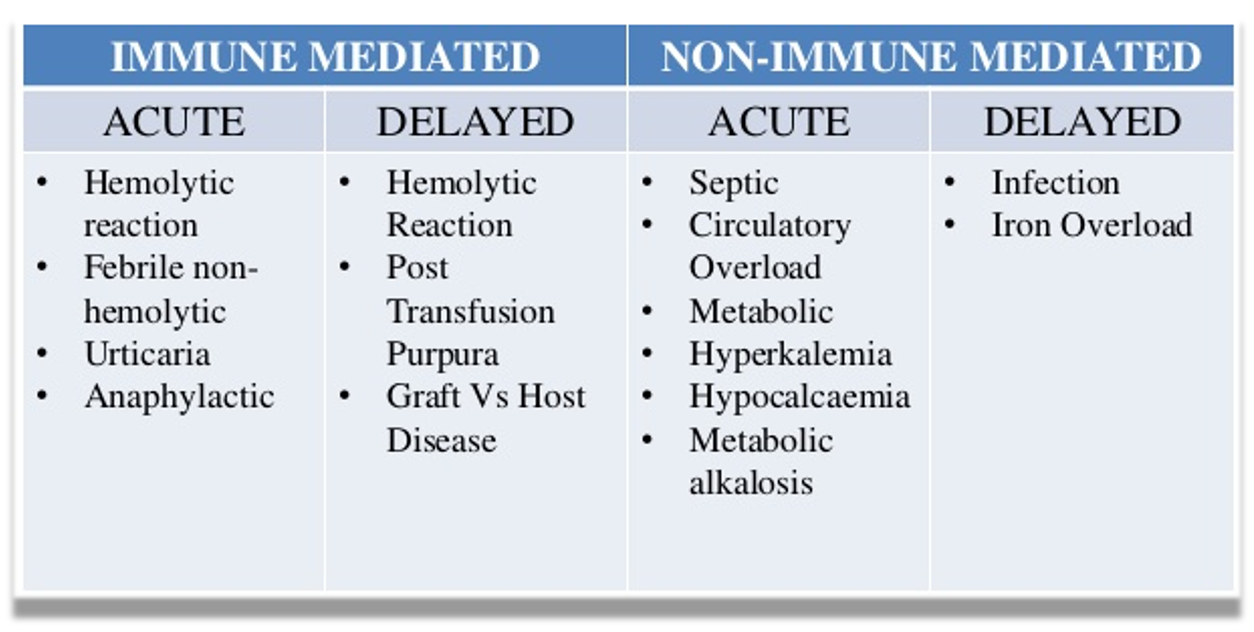
- Acute: fever due to WBC of donor
- Urticaria: recipient’s preformed-antibodies
- Hyperkalemia from potassium released from RBCs during blood bank storage
- Late: hemolytic reaction: Immune sensitization (Rh D antigen)
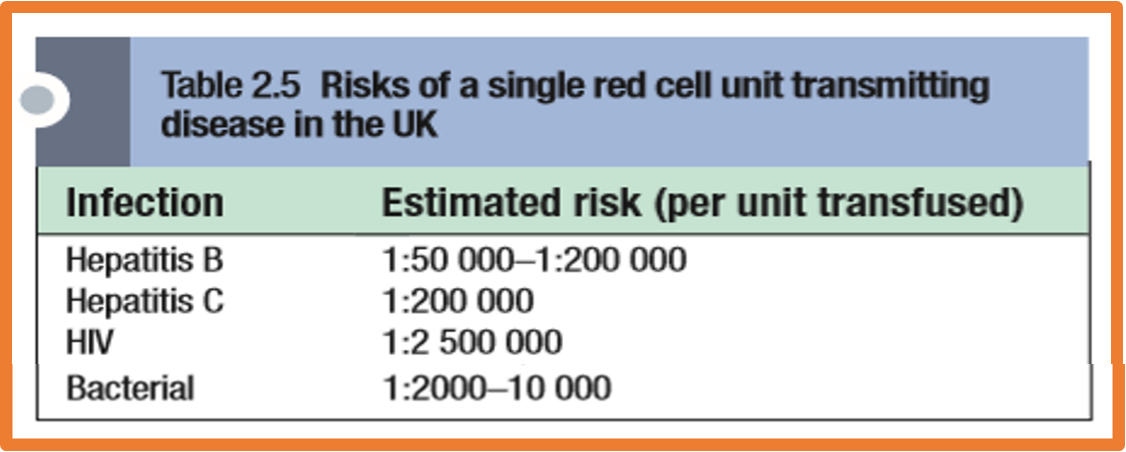
Risks of infection in blood Tx
Complications of blood Tx
Symptoms of transfusion reaction:
- Fever
- Chills
- Nausea
- Low BP
- Lumber pain
- Chest pain
- Abnormal bleeding
What to do? MBT
Massive Blood Transfusion MBT
- Different definitions
- Replacement of 10 units of PRBC in 24 hours,
- 3 units over one hour are more sensitive
- Replacement of 50% of total blood volume (TBV) within 3 h
- Hemostatic and metabolic complications
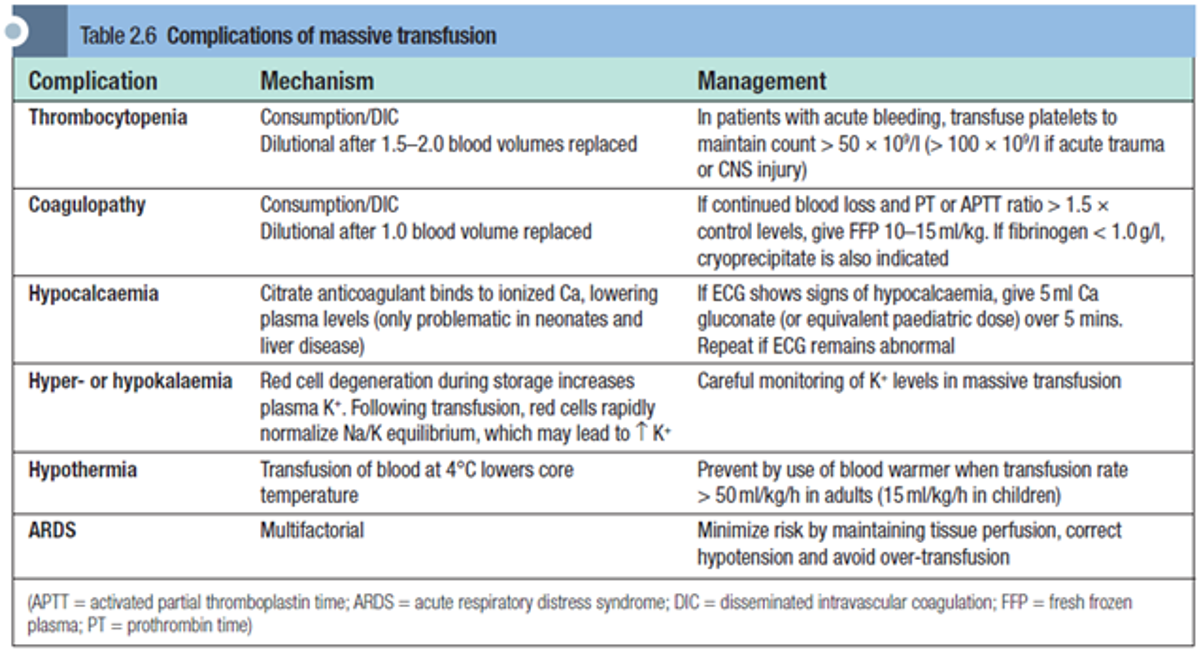
Complications of MBT
References
Principles and Practice of Surgery Pg 27-37