WIPER
Exposure | Position | Privacy | Ask for Vitals
- Wash hands (before and after examination)
- Introduce yourself to the patient and obtain consent both parties
- Position the patient appropriately
- Expose the patient as necessary (e.g.,Please take off your shirt if that is all right.)
- Right side of the bed
- Growth parameters & Vitals
I have already washed my hands and asked the parents to examine the child. Positioning and exposure are important, although positioning may not be as critical in pediatrics. I will stand to the right of the patient.
It is flexible for position, more important in exposure. Position: 45° exposure: upper trunk to the umblicus ideally to midthigh
General Appearance
ABCDEFG The patient appears to have an average body build, lying comfortable in bed, not connected to any devices, conscious and alert, but I would like to measure height, weight, and head circumference to assess growth parameters against a growth chart.
- Body build
- Dysmorphic features
- Signs of stress
- Connected devices
- Circulation / pallor / tachypnic
- Height
- Weight
- Head circumference
- Vital signs + Blood pressure on four limbs
General Examination
-
Clubbing (window test), (Fluctuation method) +
-
koilonychias (iron deficiency/white spots)
-
one line in palm down syndrome (flattened broad face esapically the bridge of the nose, almond shaped eyes and slanting eyes, epicanthic eyefold.)
-
Capillary refill time - 2s - important in GI also for dehydration. not necessarily done in CVS
-
Palmar erythema
-
Leukonychia
-
Osler or Janeway lesions
-
Cyanosis
-
Dysmorphic features
-
Dental hygiene, mucosa
-
central cyanosis (Under Tongue)
-
Pallor, Jaundice, Periorbital edema
stigmata of infective endocarditis.
Precordium Examination
Inspection
Before commenting on the following findings, check the axilla and back. Sit beside the patient to observe any bulging.
- Is the patient distressed? (e.g., tachypnea, use of accessory muscles)
- Scars:
- Mid-sternotomy scar (indicating open-heart surgery)
- Anterolateral thoracatomy
- posterior lateral thoractomy
- PDA, coarctation, or lobectomy scars
- Deformities (pectus)
- Pericardial bulge (indicative of cardiomegaly or pacemaker presence)
- Visible pulsations
- Visible tracheal deviation
Jugular venous distension (JVD) is not significant.
Palpation
-
Localize the apex beat: Locate it at the mid-clavicular line below the nipple. If dextrocardia is suspected, examine the opposite side. The apex beat should be palpable localized at first at the 4th-5th intercostal space midclavicular line and should have a normal character (heaving; volume overload or tapping; pressure overload). count from angle of louis and determine its location.
-
Thrill in all heart areas: Use the palm of your hand to check for vibrations, which may indicate murmurs or septal defects VSD, MS, AS. A thrill is typically absent in grades 1-3 murmurs and present/palpable in grades 4-6.
-
Palpable second heart sound: palpable second heart sound may suggest pulmonary hypertension. Use two fingers for palpation.
-
Parasternal Heave: right ventricular hypertrophy.
-
Hepatomegaly: May indicate right ventricular failure. (Mention only)
-
Lower limb/sacral edema: Complete the examination.
Peripheral Pulse Examination
Compare both sides
-
Rate: Place three fingers on the bony prominence of the radial artery without moving the patient’s arm. If the pulse is not localized in the radial artery, use a stethoscope to measure it. - (normal, tachycardia, bradycardia) | Age | Pulse Rate Range (BPM) | | ------------------------- | --------------------- | | Newborn baby (0
3 months) | 100150 | | Infants (36 months) | 90120 | | Infants (612 months) | 80120 | | Children (110 year) | 70130 | -
Rhythm: An irregular rhythm may indicate mitral stenosis. 1. (regular regular Normally) 2. (Irregular regular e.g: Sinus arrhythmia, Second degree Artioventricular block, Ectopic beat) 3. (Irregular irregular e.g: Atrial fibrillation, Multiple ectopics)
-
Volume:
- Large: A pulse that is easily felt on superficial touch, indicative of a collapsing pulse (aortic/mitral regurgitation).
- Small: May indicate aortic stenosis or mitral stenosis (not necessary to assess). - weak and thready pulse in shock, severe peripheral atrial disease
- Normal:
-
Character:
- Collapsing Pulse: Assess by pressing four fingers against the brachioradialis. If not palpable, raise the arm after asking the patient if there is any shoulder pain.
- Bounding Pulse: Commonly seen in pregnancy.
- Grading per finger:
- 1st: Normal
- 2nd: Bounding pulse (anemia, thyrotoxicosis)
- 3rd: Positive collapsing pulse
- 4th: Water-hammer pulse (severe aortic regurgitation)
- Grading per finger:
-
Synchronization:
- Assess for radio-radial and radio-femoral delays. if delayed most likely Aortic coarctation
- Radio-Radial Synchronization:
- Trauma is the most common cause.
- Recurrent arterial blood gas testing may indicate diabetes mellitus or atherosclerosis.
- Takayasu disease is a rare form of vasculitis that predominantly affects Asian women, leading to narrowing, occlusion, or aneurysms of the affected arteries.
- Radio-Femoral Synchronization:
- Assess at the mid-inguinal point, typically located from the anterior superior iliac spine (ASIS) to the pubic symphysis. The patient should stand to test the femoral artery.
- Consider coarctation of the descending aorta.
- Radio-Radial Synchronization:
- Assess for radio-radial and radio-femoral delays. if delayed most likely Aortic coarctation
Mention that you would take BP on all four limbs
Auscultation
Use the bell for diastolic murmurs or pericardial rubs in adults; however, using the diaphragm is generally sufficient in pediatrics.
Heart Sounds
- S1 (systolic) is known with the radial pulse; S2 (diastolic) follows.
- Auscultate S3 and S4 after S2.
- Use both the diaphragm and bell to auscultate all areas.
Auscultation Areas:
- Mitral (4th-5th midcl)
- Tricuspid
- Lower left sternal edge
- Pulmonary
- Aortic
- Below left clavicle
- Carotid
Listen to the opposite side to exclude dextrocardia before continuing. palpate radial while auscultating
Normal s1 & s2 no added sound. ss3, s4 gallop rhythm if present.
Murmur Assessment
Maximum intensity which part of pericordium murmur heard loudest, mitral? Tricuspid?
Grading
- If thrill is present automatically - 6
- if heard only - 3
Timing
- A murmur heard after S1 is systolic (pansystolic below areas/ejection above areas).
- A murmur heard after S2 is diastolic (rare; e.g., mitral regurgitation).
- A continuous murmur may indicate patent ductus arteriosus (PDA), which typically closes at birth.
If no murmur is present, palpate the first and second heart sounds without added sounds.
Radiation of Murmurs Is there any radiation of the murmur?
- Axillary radiation: May indicate mitral regurgitation.
- Ventricular septal defect (VSD): Global pericardial radiation.
- Pulmonary stenosis: Radiation to the back; scapula.
- Aortic stenosis: Ejection systolic murmur radiating to the neck or carotid.
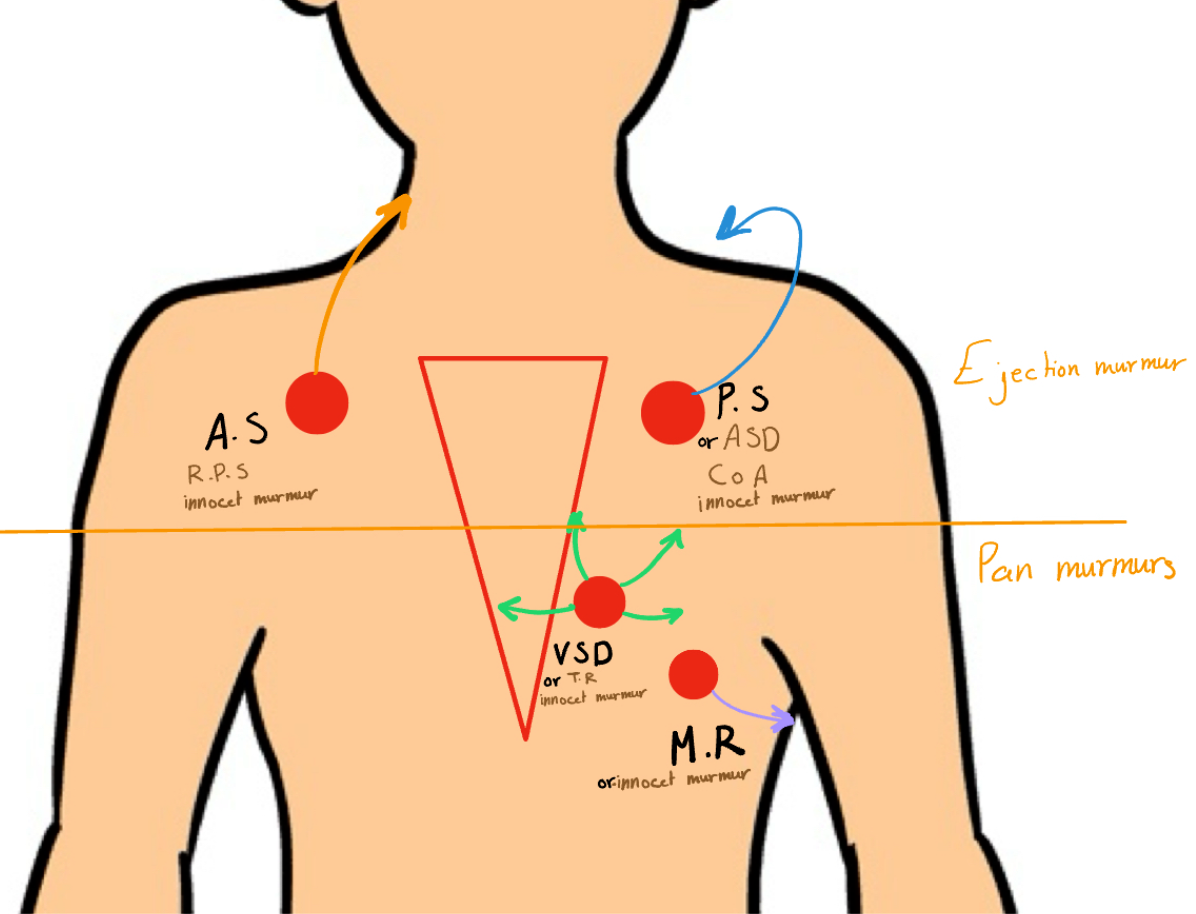
Second Heart Sound: - Normal: Mention “normal S1, S2, no added S3, S4.” - Increased: Indicates pulmonary hypertension. - Decreased: Indicates pulmonary stenosis. - Splitting: Suggests atrial septal defect (ASD).
make sure to auscultate all these areas to other than aforementioned areas of chest.
Basal Lung Auscultation (mention) back lung from lower lobe, Crepitation
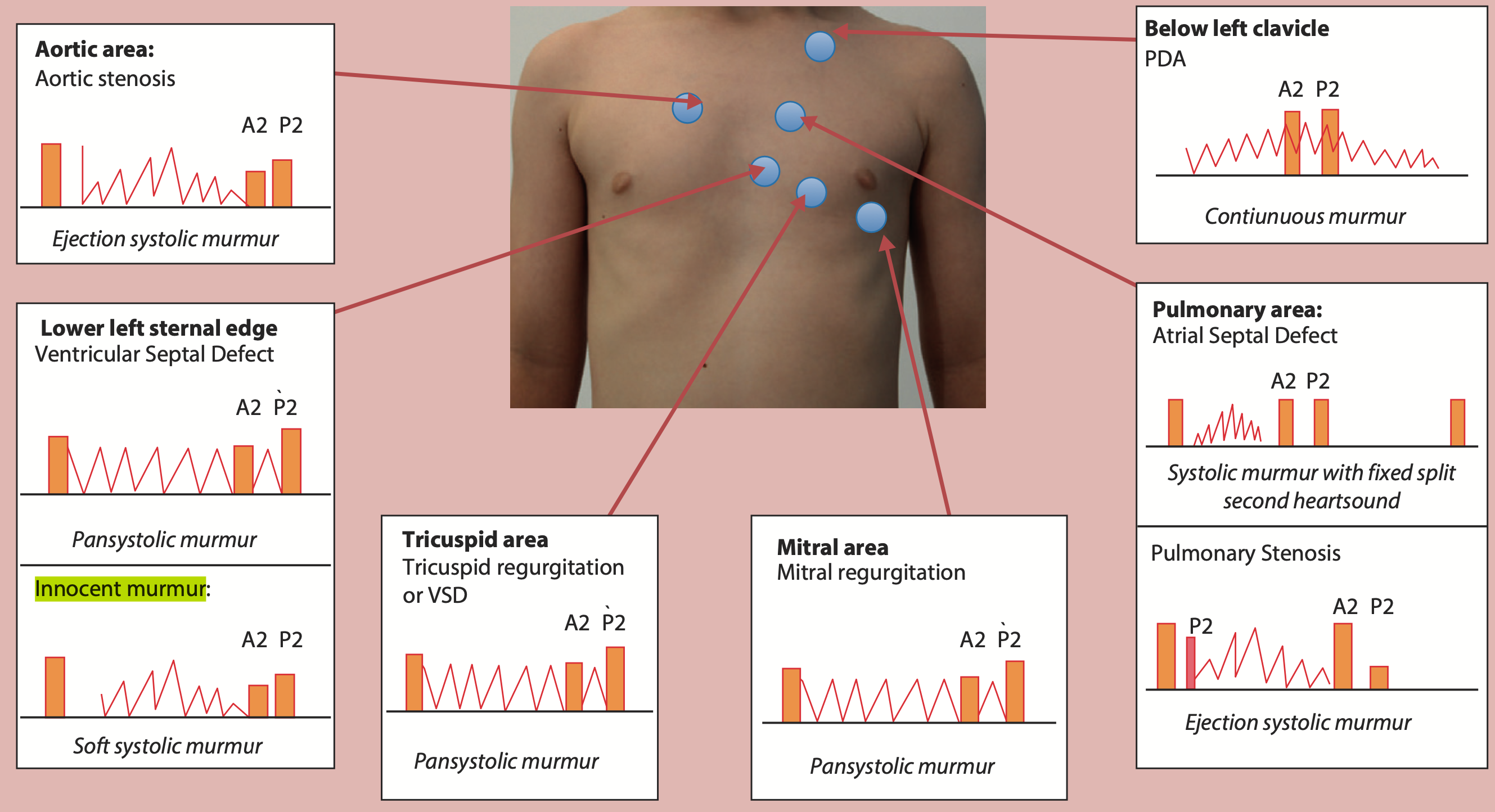
Memorize 4-5 differentials to all areas
Cardiac differential Based on murmur
Additional Checks
- Examine the back and mention the genital examination.
- Check for lower limb edema and mention sacral edema.
- Check lymph nodes (all neck and face groups, axilla, groin).
Investigations
- ECG
- X-ray
- VBG (acidosis)
- Cardiac CT/MRI
- Echocardiogram
Management
- Management depends on the severity of the case and diagnosis.
- For mild cases, follow-up is recommended.
- For heart failure, initiate medical treatment.
Specific Treatments
- Mitral Regurgitation: Start with medical treatment; valve replacement may be necessary.
- Pulmonary/Aortic Stenosis: Consider valvoplasty.
- Ventricular Septal Defect (VSD): Surgical closure may be required.
other notes
Do not forget to auscultate the anterior fontanelle for bruits when you examine a newborn with heart failure. (A-V malformation)
Types of Murmurs
-
Innocent/Physiological/Normal Murmur (Asymptomatic or Symptomatic):
- Soft, blowing sound
- Systolic only (maximum grade 2)
- Located at the left sternal edge
- Murmurs may change with movement in pediatrics
- Normal heart sounds
- No parasternal thrill
- No radiation
-
Pathological Murmur:
- Grade >3
- Harsh sound
- High intensity
- May change with position
Approach
- If the assessment investigation does not provide a diagnosis, consider 3-4 specific investigations.
- Treatment Plan:
- Provide 4 differential diagnoses (most probable, might be, etc.).
- Plan: “I will request CT, X-ray, lab investigations, and in some cases, surgical intervention or heart failure medications.”
other notes
| Condition | Description | Symptoms | Signs | Treatment |
|---|---|---|---|---|
| Ventricular Septal Defect (VSD) | - Most common CHD. - Defect in ventricular septum. - High Pressure in LV forces oxygenated blood back to RV. - Small defects often close spontaneously in the first 2 years of life while large defects require surgical repair within the 1st year. | - Asymptomatic - Rapid breathing - Excessive Sweating - Poor weight gain - Congestive Heart Failure, usually within 6 to 8 weeks of life if defect is large - Pulmonary Hypertension if defect is large - Eisenmenger’s syndrome | - Depend on the size of the defect - Loud harsh pansystolic heart murmur - Palpable thrill - Parasternal heave (RVH) - Signs of congestive heart failure: tachycardia, tachypnea, respiratory distress (retractions), grunting, difficulty with feeding, diaphoresis, displaced apex beat, and hepatomegaly | - Lasix and Captopril (ACE inhibitors) - Surgery is patching the defect by pericardium or Dacron (open heart surgery with cardiopulmonary bypass) - Pulmonary artery banding to reduce blood flow to lungs if not stable for surgery - Percutaneous Device closure |
| Atrioventricular Septal Defect (ASD) | - Defect in atrial septum - Pressure in LA is greater than RA (blood flows left to right) - Oxygen-rich blood leaks back to RA & RV and is then pumped back to lungs | - Asymptomatic - Large defect may cause symptoms of CHF: - Rapid breathing - Excessive Sweating - Poor feeding, failure to thrive - In adults: - Fatigue and dyspnea on exertion - Palpitations - Syncope - Stroke - Eisenmenger’s syndrome | - Heart murmur resulting from increased blood flow through pulmonary valve (systolic ejection murmur) - Wide and fixed splitting of second heart sound - Parasternal heave (RVH) - Signs of congestive heart failure | - Small defect (less than 5mm), may resolve spontaneously - Medical Management (Lasix, Captopril) for large defects with symptoms of heart failure - Transcatheter devices, such as a septal occluder may be used - Surgical closure is needed for large defects that cannot be closed by Transcatheter devices - Pulmonary artery banding to reduce blood flow to lungs if not stable for surgery |
| Patent Ductus Arteriosus | - Blood flows from aorta to the pulmonary artery, creating a left to right shunt, resulting in left atrium and ventricle overload - Increased pulmonary blood flow can result in pulmonary hypertension and reversal of the shunt, which is known as Eisenmenger’s Syndrome. This results in flow of desaturated blood to the lower extremities. | - Preterm neonate develop CHF and respiratory distress, Full term neonate may be asymptomatic - Infants with Large left to right shunts develop symptoms of congestive heart failure such as tachypnea, tachycardia, poor feeding, and slow growth - Children with small patent ductus are usually asymptomatic | - Continuous murmur heard best at the left sternal border, left subclavicular thrill - Widened pulse pressure and bounding peripheral pulses - Poor growth - Differential cyanosis | - Administration of Indomethacin / nsaids (prostaglandin inhibitor) to stimulate ductus to constrict - Surgical division or ligation of the PDA - Percutaneous device closure by PDA occluder device or coil |
| Coarctation of Aorta | - Constriction of the aorta at or near the insertion site of the ductus arteriosus - Reduces cardiac output - Aortic pressure is high proximal to the constriction and low distal to the constriction - Risk for CVA - Pink Blood - Higher pressure | - Often discovered 3-4 days after birth when the patent ductus arteriosus closes - Symptoms of shock develop very rapidly as no oxygenated blood flows to the lower extremities - Rapid breathing, sweating, and poor feeding often develop during the first week | - Most babies born at term with normal length and weight - Systolic murmur usually heard - Liver may be enlarged - Left arm/leg pulses may be diminished or absent - BP is about 20 mm/Hg higher in arms than in lower extremities - Upper extremity hypertension - Lower extremity cyanosis | - Medical Management (Dopamine, dobutamine, Lasix) - Oxygen - Administration of PGE1 (prostaglandin) infusions, to maintain ductal patency and improve perfusion to lower extremities - although will cause increased pulmonary flow - Surgical repair |
| Pulmonary Stenosis | - | - | - Systolic ejection murmur with a palpable thrill - Right ventricular hypertrophy - Cyanosis from reduced pulmonary blood flow and the right to left shunt of blood at foramen ovale due to high right ventricular pressure - Can lead to right ventricular failure, CHF | - Oxygen - Medical Management (Lasix) - Administration of PGE1 (prostaglandin) infusions, to maintain ductal patency in critical pulmonary stenosis - Pulmonary balloon valvuloplasty via cardiac cath - If unsuccessful, valvotomy |