Breastfeeding and Alternative to Breastfeeding
Dr. Salma Elgazzar
Learning Objectives
- Identify the major differences between human milk and commonly available formulas.
- Describe the advantages of breastfeeding and recognize common difficulties experienced by breastfeeding mothers.
Advantages of Breastfeeding
For the Baby
- Superior Nutrition: Perfectly balanced and nutritionally complete food for babies.
- Sterile and Fresh: Breast milk is always fresh, self-regulated, and at the proper temperature.
- Increased Resistance to Infections: Decreased risk of allergies (atopic eczema, allergic rhinitis, asthma, and allergic gastroenteropathy) and lactose intolerance.
- Less Nappy Rash and Thrush: Fewer stomach upsets and constipation.
- Dental Health: Breastfed infants tend to have fewer cavities.
- Jaw and Teeth Development: Promotes proper development.
- Higher IQs: Due to good brain development early in life.
- Emotional Benefits: Babies benefit emotionally because they are held more.
- Mother-Baby Bonding: Promotes bonding.
- Long-term Health: Decreased risk of malnutrition, obesity, and heart disease compared to formula-fed babies.
- Anti-inflammatory Properties: Contains anti-inflammatory properties.
For the Mother
- Uterine Contraction: Baby’s sucking causes the uterus to contract and reduces blood flow after delivery.
- Contraception: Menstruation ceases during lactation, offering a form of contraception.
- Weight Loss: Mothers tend to lose weight and achieve their pre-pregnancy figure more easily.
- Reduced Cancer Risk: Less likely to develop breast and ovary cancer later in life.
- Economical and Convenient: More economical and convenient than formula feeding.
- Less Medical Visits: Fewer trips to the doctor and less money spent on medications.
- Mother-Baby Bonding: Promotes bonding.
- Hormonal Benefits: Hormones released during breastfeeding create feelings of warmth and calm.
Stages of Lactation
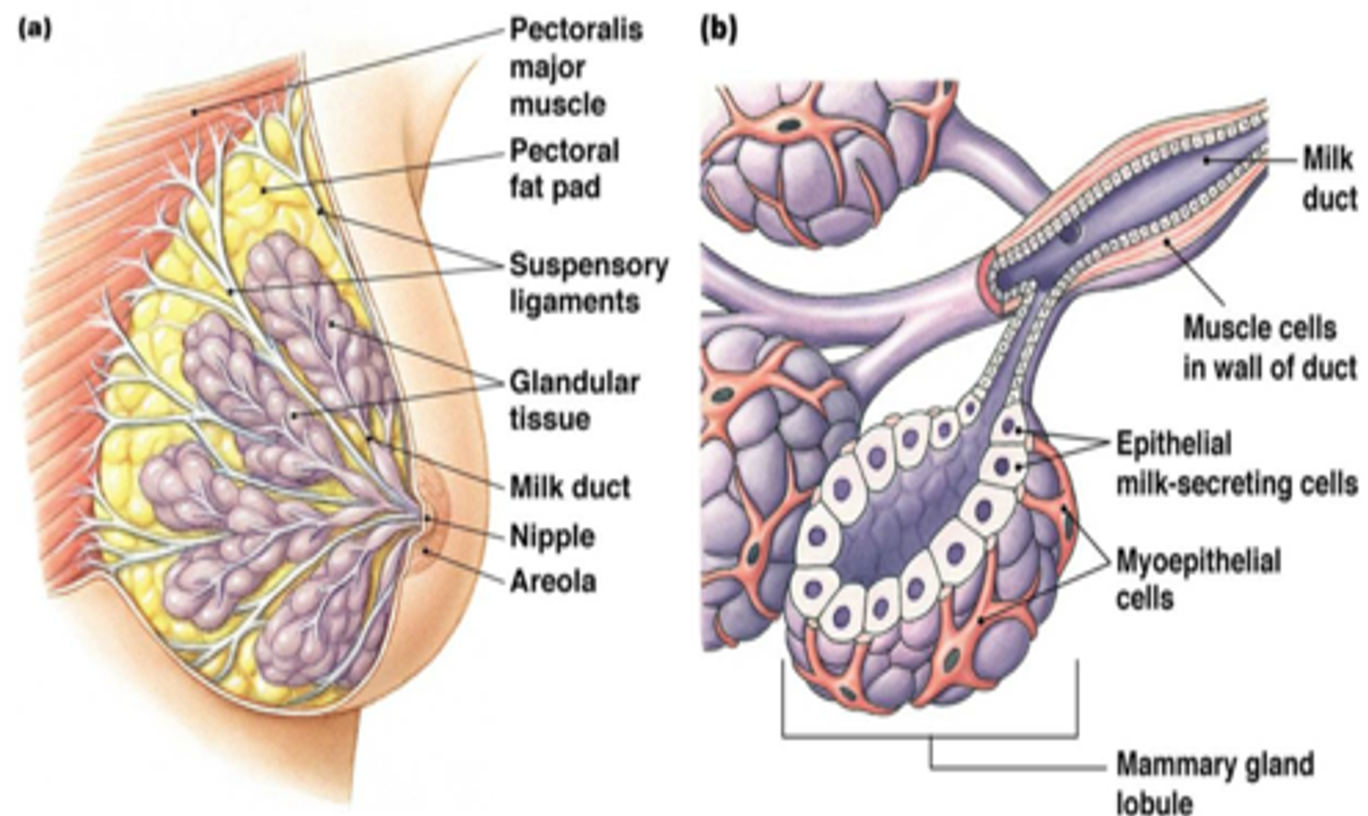
Mammogenesis
- Mammary (breast) growth occurs.
- The size and weight of the breast increase.
Lactogenesis
In lactogenesis, the mammary gland develops the capacity to secrete milk.
Stage 1
Occurs by mid-pregnancy. - The mammary gland becomes competent to secrete milk.
- Changes in glandular fluid: Increase in lactose, total protein, and immunoglobulin concentrations; decrease in sodium and chloride concentrations.
- Colostrum: Women often describe drops of colostrum on their nipples in the second or third trimester.
- Hormonal regulation: High circulating levels of progesterone and estrogen hold the secretion of milk in check.
Stage 2
Occurs around the time of delivery.
- Onset of copious milk secretion.
- Increased blood flow, oxygen, and glucose uptake.
- Increased citrate concentration: Considered a reliable marker for the second stage of lactogenesis.
Galactopoiesis
- Occurs later than 9 days after birth to the beginning of involution.
- Established secretion is maintained.
- Autocrine system control continues.
Involution
- Average 40 days after last breastfeeding.
- Milk secretion decreases from the buildup of inhibiting peptides.
Maternal Reflexes
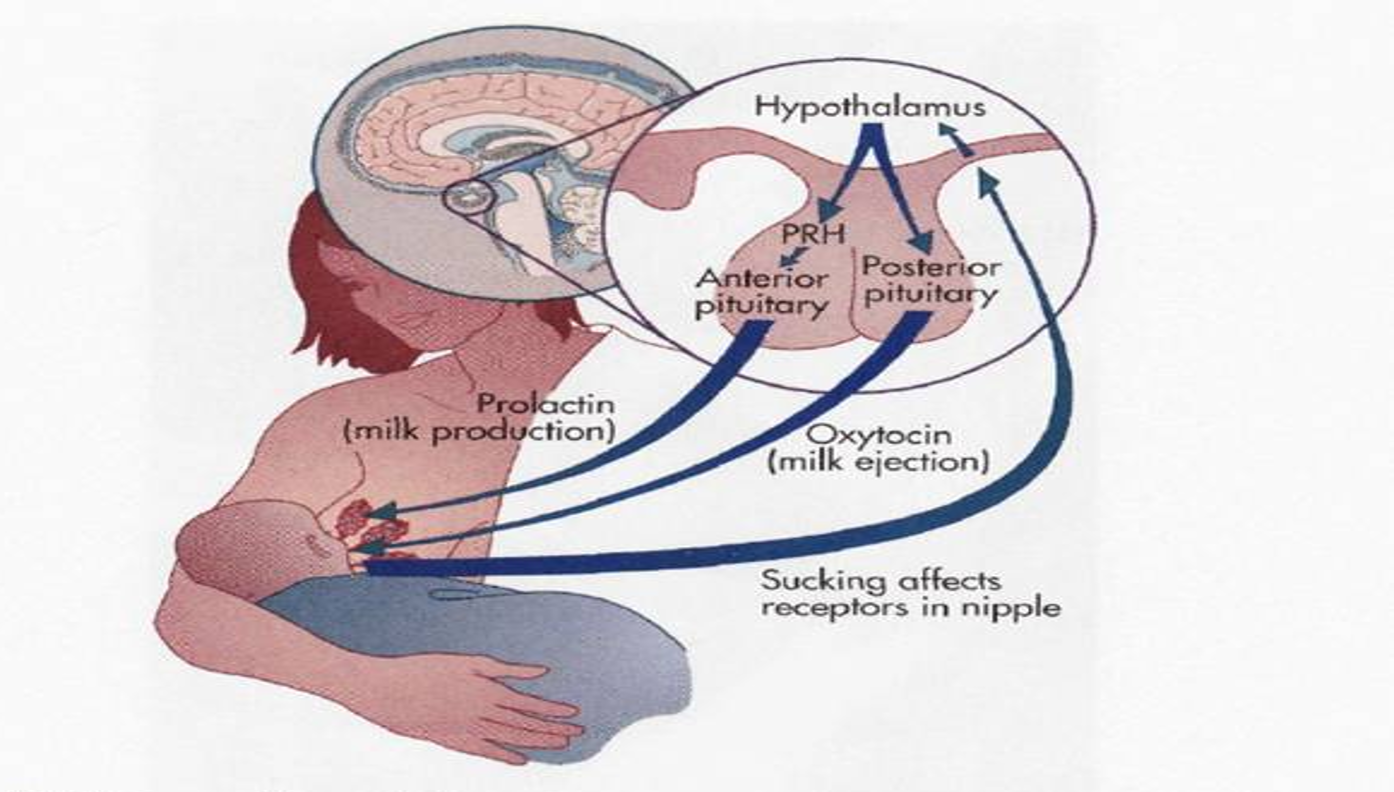
A. Maternal Reflexes
Initiated via suckling of the mother’s nipple by the baby
- Nipple erection reflex.
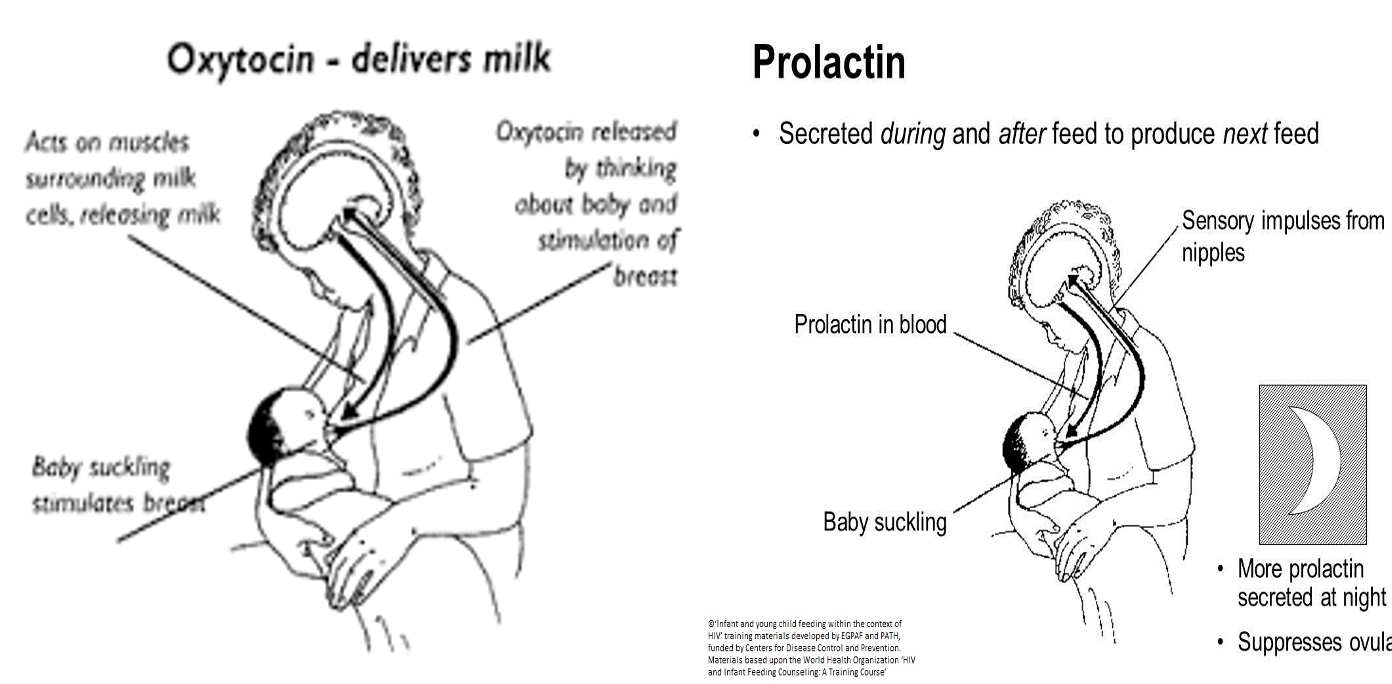
- Prolactin reflex: Sensory stimuli to the hypothalamus stimulate the anterior pituitary to secrete prolactin, which is transported by the bloodstream to the glandular cells of the breast alveoli where it stimulates the secretion of milk.
- Oxytocin reflex (let-down reflex or milk-ejection reflex): Oxytocin is reflexively secreted from the posterior pituitary and stimulates the contraction of the myoepithelial cells surrounding the alveoli, thus forcing milk into larger ducts.
B. Neonatal Feeding Reflexes
- Rooting reflexes: Touching of the cheek or circumoral area leads to turning the head to the side of the stimulus & opening the mouth as the baby is seeking the nipple.
- Sucking (or suckling) reflex: The tactile stimulus caused by the nipple and areolar tissue filling the mouth leads to a milking action by the tongue against the hard palate.
- Swallowing reflex: Follows suckling and allows interruption of breathing to prevent choking.

Control of Milk Secretion
- Endocrinal.
- Autocrine control: If the milk is not regularly removed from the breast, an inhibitory peptide will accumulate leading to the stoppage of milk secretion. After a few weeks, the amount of milk production becomes proportionate to the extent of breast evacuation.
- Psychological: No factor is more important than a happy relaxed state of mind. - Let-down reflex can be initiated by maternal emotional factors such as the sight or sound of the hungry baby or even the thought of nursing the baby. - Let-down reflex is suppressed by worry, fear, and unhappiness.
- Adequate balanced maternal nutrition.
- Sufficient rest.
Drugs & Smoking
- Chlorpromazine may enhance milk secretion.
- Estrogen-containing contraceptives, diuretics, and smoking may suppress lactation.
- Domperidone is the most effective medicine used to improve breast milk supply by stimulating the release of prolactin, which in turn stimulates breast milk production.
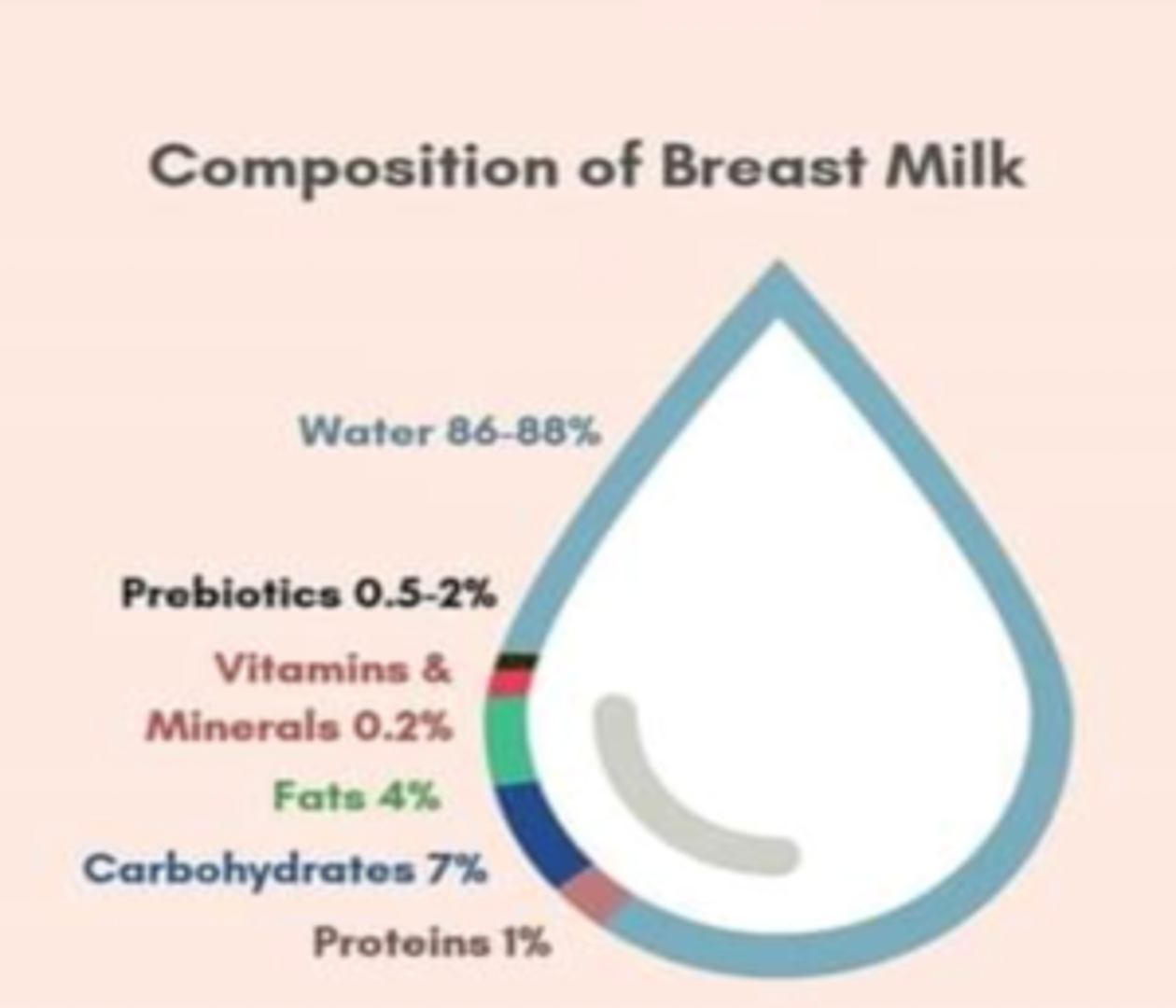
Composition of Breast Milk
- Breast milk contains complex proteins, lipids, carbohydrates, and other biologically active components. The composition changes over a single feed as well as over the period of lactation.
1- Variability According to Stage of Lactation
- Colostrum.
- Transitional milk: Follows the colostrum.
- Mature milk: Is secreted by the 10th-20th day after delivery.
2- Diurnal Variation
- Fat contents at midday is 2.5 fold that in early morning or night.
3- Variation Within Each Feed
- Fat content of the last amount of milk in each feed (hind-milk) is 3 fold that in first drops (fore-milk). This helps in achieving baby’s satiety, thus preventing overfeeding and obesity in breast-fed infants.

4- Variation According to Gestational Age In case of premature baby, the protein and mineral contents are increased.
Colostrum
- Secreted during the first few days (5 days) after delivery.
- Rich in protein & antibodies (especially secretory IgA) that provide passive immunity to the baby (the baby’s immune system is not fully developed at birth).
- More rich in cholesterol, macro-minerals (Na, K, …), microminerals, vit. A.
- Rich in leukocytes (macrophages and lymphocytes) and antibacterial factors (lactoferrin & lysozyme).
- Colostrum also helps the newborn’s digestive system to grow and function properly.

Composition of Breast MilkZ
- Human milk contains 0.8% to 0.9% protein, 4.5% fat, 7.1% carbohydrates, and 0.2% ash (minerals).
Carbohydrates
- Mainly lactose.
- Several lactose-based oligosaccharides have been identified (as minor components) which act as prebiotics to promote the growth of lactobacilli.
Carbohydrate (g/100 ml):Y
- Lactose: 7
- Oligosaccharides: 0.5
The Fat Fraction
- Contains specific triglycerides of palmitic and oleic acid (O-P-O triglycerides), and also lipids with trans bonds.
- The lipids are vaccenic acid, and Conjugated linoleic acid (CLA) accounting for up to 6% of the human milk fat.
- High contents of cholesterol help myelination of the nervous system and protect against atherosclerosis and coronary disease in later life.
- Breast milk is rich in lipase that can digest 90% of milk triglycerides in the bile in the intestine.
Fat (g/100 ml):Y
- Total: 4.2
- Fatty acids - length 8C: trace
- Polyunsaturated fatty acids: 0.6
- Cholesterol: 0.016
Proteins
- Most of the proteins (70%) are soluble easily digested whey protein.
- Whey: casein ratio is 60:40.
- The principal proteins are alpha-lactalbumin, lactoferrin (apo-lactoferrin), IgA, lysozyme, and serum albumin.
- In an acidic environment such as the stomach, alpha-lactalbumin unfolds into a different form and binds oleic acid to form a complex called HAMLET that kills tumor cells. This is thought to contribute to the protection of breastfed babies against cancer.
- Non-protein nitrogen-containing compounds, making up 25% of the milk’s nitrogen, include urea, uric acid, creatine, creatinine, amino acids, and nucleotides.
Protein (g/100 ml)Y
- Total: 1.1
- Casein: 0.4
- Alpha-lactalbumin: 0.3
- Lactoferrin (apo-lactoferrin): 0.2
- IgA: 0.1
- IgG: 0.001
- Lysozyme: 0.05
- Serum albumin: 0.05
- Beta-lactoglobulin: -
Vitamins and Minerals
- Low phosphate content prevents neonatal hypocalcemic convulsions.
- Low renal solute load (minerals content is ¼ that of cow’s milk).
- Low sodium content prevents hypernatremia & sudden infant death syndrome.
- Low risk of iron deficiency anemia during the first 6 months of life due to better iron absorption (acidic bowel medium and the presence of large amounts of vit.C, E & copper).
Minerals (g/100 ml):Y
- Calcium: 0.03
- Phosphorus: 0.014
- Sodium: 0.015
- Potassium: 0.055
- Chlorine: 0.043
Anti-Infective Properties - Humoral protection:
- Secretory IgA comprises 90% of immunoglobulin in human milk, provides mucosal protection.
- Bifidus factor promotes the growth of lactobacillus bifidus, which metabolizes lactose to lactic acid and acetic acids, the resulting low PH may inhibit the growth of gastrointestinal pathogens.
- Lysozyme bacteriolytic enzyme.
- Lactoferrin iron-binding protein inhibits the growth of Escherichia coli.
- Interferon antiviral agent.
- Cellular:
- Macrophages phagocytic synthesize lysozyme, lactoferrin, C3, C4.
- Lymphocytes T cells may transfer delayed hypersensitivity responses to infants.
- B cells synthesize IgA.
Breastfeeding Policy of the Department of Health
The Department of Health is committed to protecting, promoting, and supporting breastfeeding through advocacy; implementation of “Ten Steps to Successful Breastfeeding”.
Ten Steps to Successful Breastfeeding
- Have a written breastfeeding policy that is routinely communicated to all healthcare staff.
- Train all healthcare staff in skills necessary to implement this policy.
- Inform all pregnant women about the benefits and management of breastfeeding.
- Help mothers to initiate breastfeeding within a half-hour of birth.
- Show mothers how to breastfeed, and how to maintain lactation even if they are separated from their infants.
- Give newborn infants no food or drink other than breastmilk, unless medically indicated.
- Practice rooming-in, allow mothers and infants to remain together 24 hours a day.
- Encourage breastfeeding on demand.
- Give no artificial teats or pacifiers (also called dummies or soothers) to breastfeeding infants.
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic.
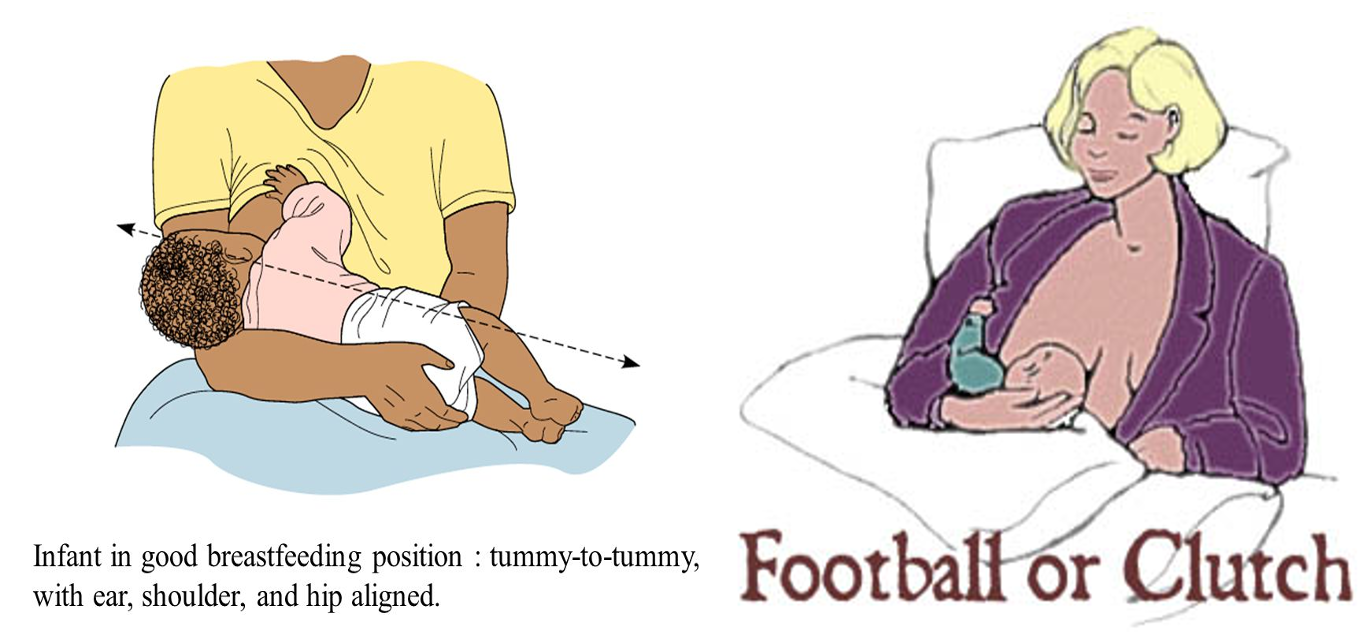
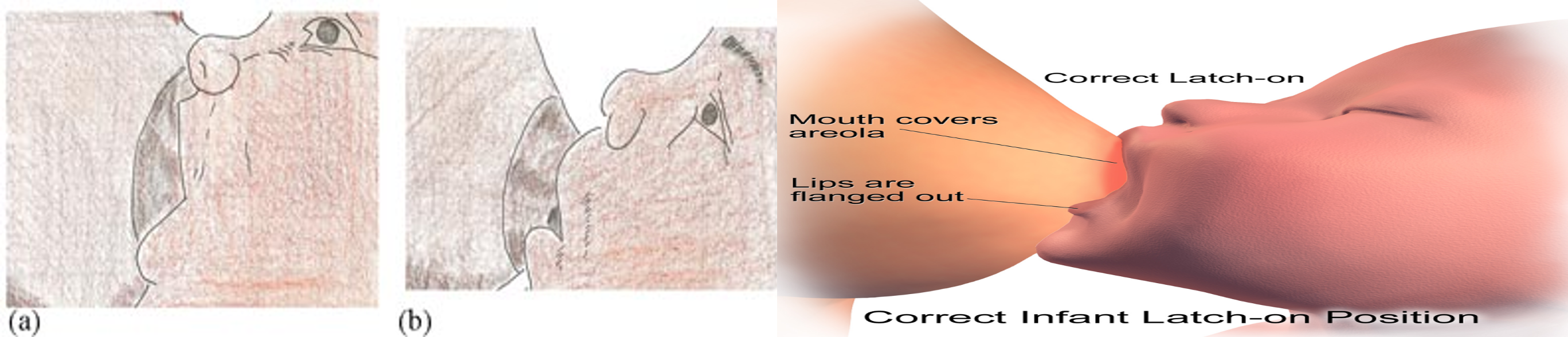
4 Criteria of good attachment:Z
- Baby’s chin is touching the breast
- Baby’s mouth is widely open
- Lower lip is turned outwards
- More areola tissue above than below the mouth
- No pain while breast feeding