How to Approach? 60 years old male, known case of diabetes mellitus, presented to Emergency Department complaining of fever and Foot discharge.
Common triggers for ulceration
- Poorly fitting footwear
- Unnoticed trauma from foreign body
- Burns (hot bath, hot water bottle, radiator)
- Heel friction in a patient confined to bed
- Nail infection
- Dry skin
- Self-treatment of callus with sharp instruments, or corn plasters
- Callus not effectively treated
Duration of the current symptoms (when & How noticed)
- What drew the patient attention? (discharges, bad smell, bleeding, …)
- Course of the ulcer since appearance (size, shape, discharge, if healed and broken down now)
- Associated Sx?(fever, sensation changes) Any other ulcers elsewhere?
- Hx of previous Trauma / burn / bare foot
- Any Tx had been suggested or administered?
- Previous Amputation / interventions
- DM controlled? (since? medication on? Following with endocrinology? Diet?)
Examination:

Remember:
- Wash your hand & Protective equipment (gloves, gown, face mask)
- Introduce your self & identify your Patient
- Assure Privacy
- Chaperon / nurse presence
- Explain the Procedure / what you will do
- Take the Permission / consent
- Check the surroundings of the patient
- Position the patient & Exposure
Then, start the focus examination
I- Look:
- Location
- shape
- Size (approximately)
- Floor (Color & Content)
- Discharges (pus, blood, quantity)
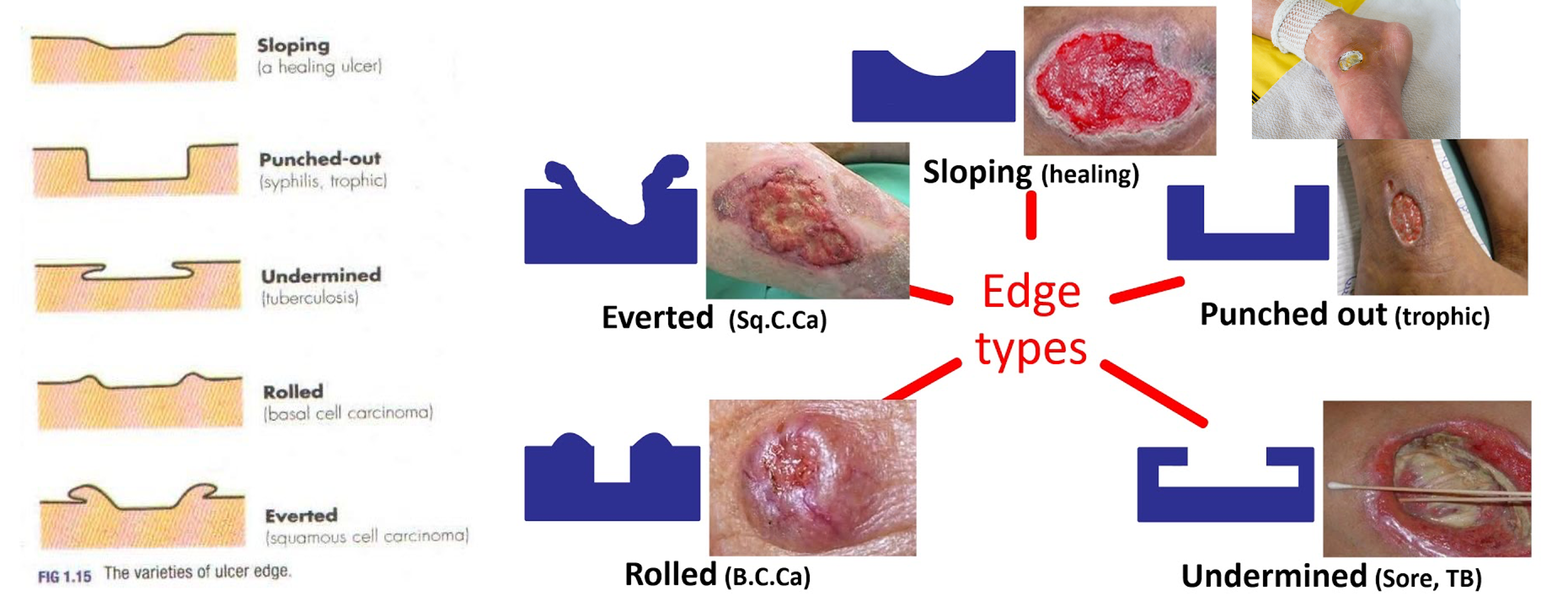
- Edge
II- The floor:
-
Granulation Tissue (Red Pink): Collagen, fibroblast, capillary, Inflammatory cells and bacteria
-
Eschar: (Black) Layer of dead tissue + DRIED
-
Scab: (yellow) Sloughed and dried small amount of discharges
III- Edge:
- Flat sloping ( healing / venous)
- Punched out (Syphilis / DM (more commonly) / Ischemic)
- Undermined (pressure necrosis, carbuncle, Tuberculous)
- Rolled (BCC)
- Everted (SCC / Ulcerated AdenoCA)
- Sloping edge: pale/pink consistent of new healthy epithelium growing over the base of the ulcer
Also in “Look” you can comment on the surrounding of the ulcer, like: dry skin, scars, hair loss, pigmentation, …
IV- Feel: TTB
- Tenderness
- Arterial Ulcer is painfull
- Venous ulcer less painfull
- Neuropathic usually not
- Temperature
- Base
Note
Sloping edge: pale/pink consistent of new healthy epithelium growing over the base of the ulcer
Also in “Look” you can comment on the surrounding of the ulcer, like: dry skin, scars, hair loss, pigmentation, …
V- Examine Surrounding Tissue:
- Induration (Infection, Trauma)
- Pigmentation (Venous ulcer mainly)
- Scaring
- Edema
-
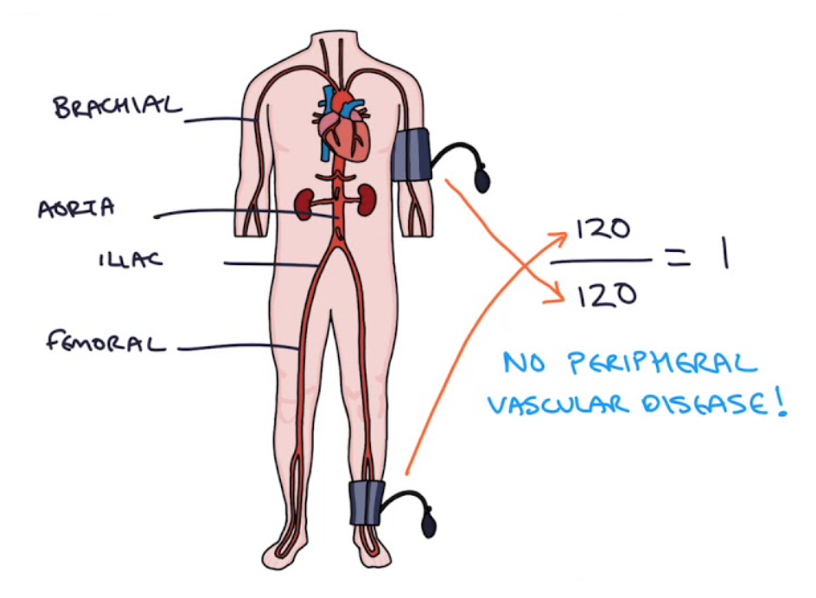
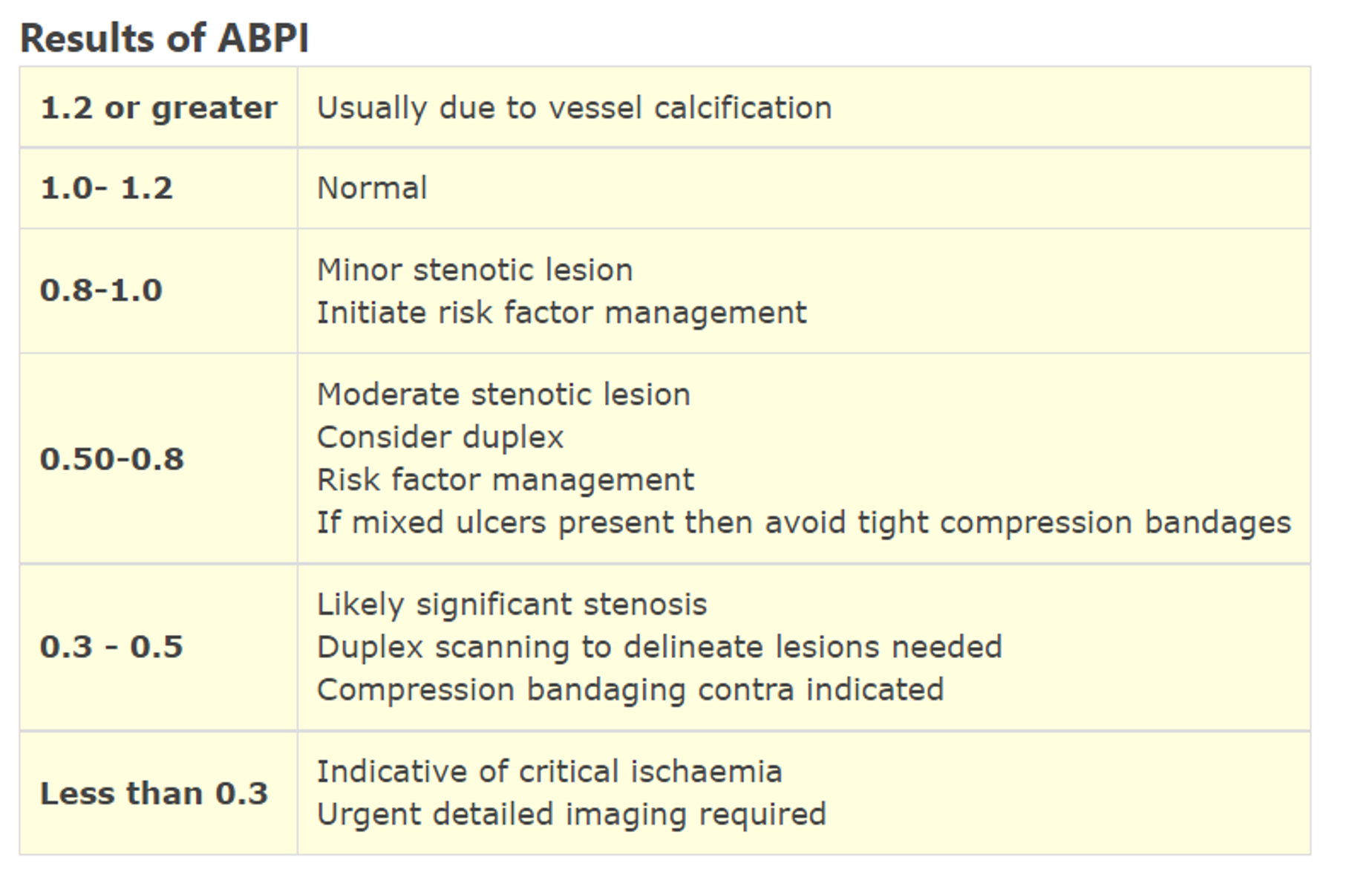
Vascular Assessment
- Skin examination (Atrophy, hair loss, nail changes)
- Capillary refill
- Peripheral pulses (femoral, popliteal, post. tibial, dorsalis pedis)
- Ankle-Brachial index ?
-
Neurosensory Assessment
- Light touch, pin prick, temperature, proprioception
-
Lymph nodes
- Local (lymphatic / venous obstruction)
- General (Liver, Cardiac, Renal, low Alb)
Neurological assessment for identification of loss of protective sensation (LOPS).
10‐g monofilament (plus at least 1 of the following 4):
- Pinprick sensation
- Vibration using 128‐Hz tuning fork
- Vibration perception threshold (VPT)
- Ankle reflexes
Examination of light touch (pressure perception)
Using the 10‐g monofilament. Filament, applied perpendicular to the skin surface of plantar surfaces of the big toe and the first, third and fifth metatarsal heads, bilaterally.
A normal protective sensation of pressure when the test is correct on at least two out of the four sites on each foot, and there should be at least one

Examination of superficial pain (pin‐prick sensation).
A disposable pin should be applied just proximal to the toenail on the dorsal surface of the hallux, with just enough pressure to deform the skin. The pin can have a sharp and a dull edge and the patient is asked to recognize if the sharp or the dull edge is touching him and at what site.
An inability to perceive the pinprick correctly over either hallux is regarded as an abnormal test result.
The pinprick should be performed starting from the toe and advancing toward the knee, on the anterior surface of both legs. Patients should not be allowed to watch during the examination.
Documentation of the level at which the sensation goes from dull to sharp is made for both sides.

Examination of vibration perception (using the 128‐Hz tuning fork):
This is tested on the dorsal side of the distal phalanx of the great toes, just proximal to the nail bed. It can also at the medial malleolus.
The tuning fork should be placed perpendicular to the foot at a constant pressure with the patient’s eyes closed.
The examination is repeated twice, and there should be at least one “sham” application in which the tuning fork is not vibrating.

Describe the following

-
ulcer - if not say discontinuity of skin breakdown representing ulcers involving the second dorsum middle toe, 1x1 cm, circular, granulated healing tissue, edge punched out… shiny skin surrounding edema, erythema
-
Skin disconutiy on left foot between fourth and fifth toe longitudinal 5x2 cm looks like ulcer, floor with dead tissue, undermined edges proximal, punched distal, surrounding looks edematous, hair loss.
-
Ulcer on medial left big toe, 4x4, irregular shape, floor with dead tissue and granulation tissue, with sloping and punched edge, with scar, nair changes, edematous, hair loss.