Allergic Contact Dermatitis
- ACD occurs when contact with a particular substance causes a delayed hypersensitivity reaction
- The sensitization process requires 10-14 days
- Upon re-exposure, dermatitis appears within 12-48 hours.
Substances causes ACD
- The most common cause is Rhus dermatitis (poison ivy, poison oak)
- Fragrances
- Nickel
- Formaldehyde
- Preservatives
- Topical antibiotics
- Benzocaine
- Vitamin E
- Rubber compounds
Poison Oak (البلوط السام) & Poison Ivy (اللبلاب السام)
Poison oak leaves Poison ivy leaves


ACD: Clinical Findings
-
The main symptom of ACD is pruritus.
-
Presents as eczematous, scaly edematous plaques with vesiculation distributed in areas of exposure
-
ACD is bilateral if the exposure is bilateral (shoes, gloves, ingredients in creams, etc.)
 lateral aspect of left arm, erythematous scaly, itchy, plaques, i’lldemarcated
eczema, but if theres cause contact dermatitis
lateral aspect of left arm, erythematous scaly, itchy, plaques, i’lldemarcated
eczema, but if theres cause contact dermatitis
Skin Exam

Rhus Allergy
- Lesions begin as erythematous macules that become papules or plaques
- Blisters often form over one to two days

 papule macule ⇒ bullae
papule macule ⇒ bullae
Examples of Severe Rhus Allergy
![[Allergic Contact Dermatitis ACD-1747637789183.webp]]
Skin Exam
This patient recently changed her eye shadow and moisturizer.

On Examination
- There is bilateral-symmetric, pruritic, erythematous, scaly, slightly lichenified plaques on her eyelids.
Eyelid Allergic Contact Dermatitis
- Intensely pruritic
- Scaling red plaques on upper > lower eyelids
- Allergic contact dermatitis of the eyelid is often caused by transfer from the hands
- Common causes:
- Nail adhesive/polish
- Fragrances and preservatives in cosmetics
- Nickel
Evaluation of Dermatitis
1- History
Important to take a comprehensive history
- Ask about the dermatitis-specific history (e.g., onset, location, temporal associations)
- Daily skin care routine
- All topical products
- Occupation/hobbies
- Regular and occasional exposures (e.g. lawn care products, animal shampoos)
2- Examination
- Complete dermatologic assessment of the patient.
- The shape, configuration, and location of the dermatitis are useful clues in identifying the culprit allergen.
3- Confirmation and investigation
- Elimination of a suspected trigger may be both diagnostic and therapeutic
- In chronic cases, patch testing is necessary to identify specific allergens
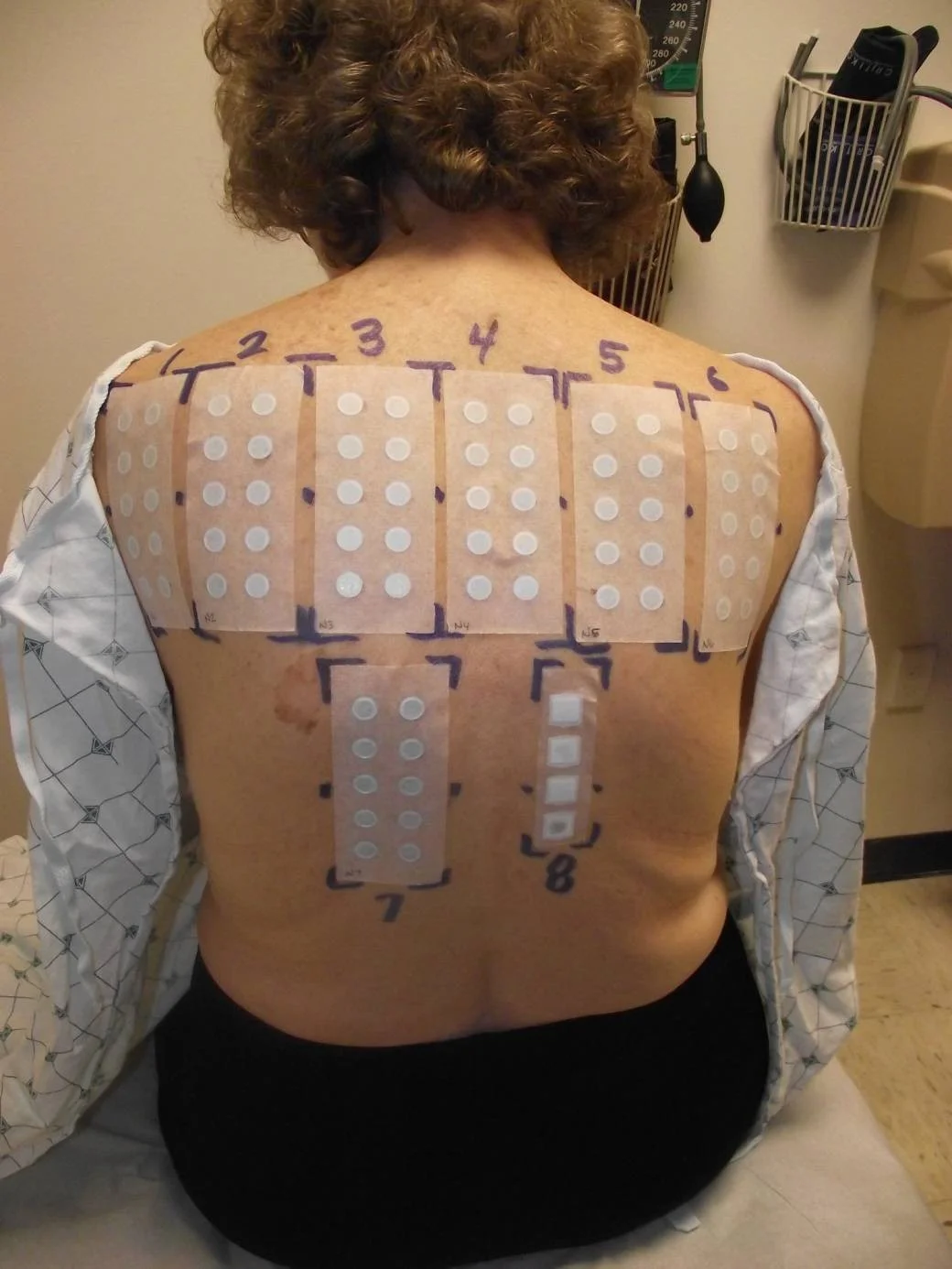
Patch Testing
-
Patch testing is used to determine which allergens a patient with allergic contact dermatitis reacts against
-
A series of allergens are applied to the back, and they are removed after 2 days
-
On day 4 or 5, the patient returns for the results
-
Positive reactions show erythema and papules or vesicles
-
Identification of specific allergens helps the patient find products free of those allergens
-
Example of a patient with patches (allergens) placed on the back
Positive Patch Test
- Positive patch test reactions at 96 hour reading
- This patient had three positive reactions
- Nickel, Balsam of Peru, and Fragrance
- Avoidance of these allergens should improve their rash

ACD Treatment
Avoid exposure to the offending substance
Treatment of the acute phase depends on the severity of the dermatitis
In mild to moderate:
- 1- Topical steroids of medium to strong potency for a limited course is successful.
- 2- Soothing lotions can provide further relief in mild cases
In severe cases:
- 1- A short course of systemic steroids may be required for acute flares and severe cases .
- 2- Topical steroid of medium to strong potency
- 3- Wet dressings are helpful when there is extensive oozing and crusting
Can you guess what the following patients are allergic to?
Medication Allergy Topical Antibiotic Cream
Patient calls 9 days after you performed a skin biopsy, reporting itching at the site

Nickel Dermatitis
This 11-year-old girl presents with 3 months of an itchy rash on the sides of her nose and ears



Latex Allergy
This respiratory therapist has an intermittent rash that clears when she goes on vacation


Case Four
Case Four: History
- HPI: B is a 32-year-old woman who presents with three months of severe itching, redness, and scaling on her eyelids. She has tried aloe vera and tea tree oil products, but they haven’t helped.
- PMH: no history of asthma, hay fever or childhood eczema
- Allergies: shellfish
- Medications: birth control pills
- Family history: noncontributory
- Social history: single; works as a bank teller
- ROS: negative
Case Four: Skin Exam

Case Four, Question 1
- Ms B has a bilaterally-symmetric, pruritic, eczematous eruption on her eyelids. What is the most likely diagnosis? a. Allergic contact dermatitis b. Rosacea (usually not itchy) c. Psoriasis (not usually limited to the eyelids) d. Seborrheic dermatitis (usually not itchy)
Allergic contact dermatitis
- Allergic contact dermatitis (ACD) is a delayed-type hypersensitivity reaction
- Poison ivy (rhus dermatitis) is the prototypic allergic contact dermatitis
- Susceptible patients become sensitized to an allergen in contact with their skin
- ACD is pruritic
- The distribution of the rash mirrors the area of exposure
Eyelid dermatitis
- May be adult atopic dermatitis if personal history of atopy and chronic
- If no atopic history and acute onset of pruritic eyelid dermatitis, think of ACD
- Allergic contact dermatitis of the eyelid is often caused by transfer from the hands
- Cosmetics, metals (nickel), topical medications, and artificial nails
Case Four, Question 2
-
On further questioning, Ms B recently changed her eye shadow and moisturizer. What treatment would you recommend other than avoidance?
a. Desonide cream b. Clobetasol ointment (too potent) c. Fluocinonide gel (too potent) d. Ketoconazole cream (not fungal)
Steroid strengths
- Topical steroids are classified by potency
- For the face, low-potency steroids (e.g., desonide) can safely be used intermittently for flares
- Potent steroids can be used in severe cases for a few days, but limit the amount given
Case Four, Question 3
-
Ms. B has an allergic contact dermatitis that responds to topical steroids. What is the best test to confirm the cause of her rash?
a. Allergen-specific IgE antibodies b. Indirect immunofluorescent antibody (IIF) test c. Patch testing d. Prick skin testing e. Radioallergosorbent test (RAST)
Case Four, Patch Test
- The patient underwent patch testing for ACD
- There were three positive reactions on day 4
- Nickel, Balsam of Peru, and Fragrance
- Avoidance of these allergens should improve her rash
- Refer patients to a dermatologist who performs patch testing when the allergen is unclear or the dermatitis is chronic
