Routine care and resuscitation of newborn
Dr Faten Zaidan
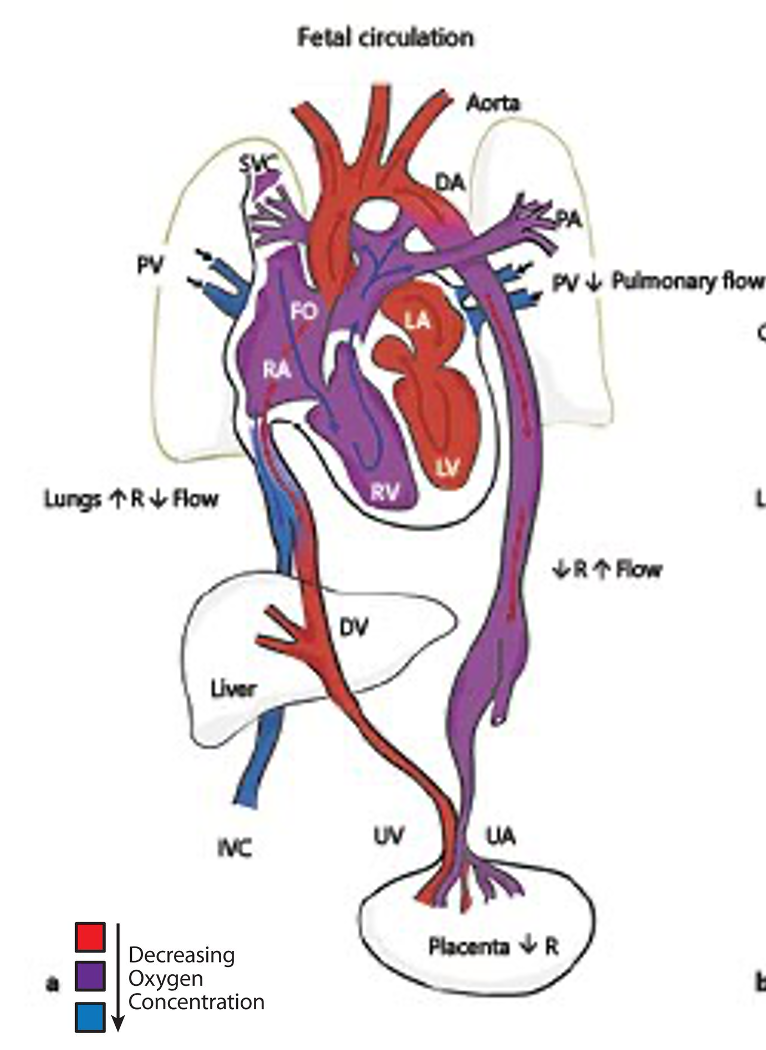
Fetal Physiology and the Transition to Extrauterine Life
Oxygenated Blood from the placenta
Oxygenated Blood from the placenta goes to the umbilical vein. Then UV in the liver splits into two branches, one for the liver and the other becomes ductus venosus. Blood goes then through the ductus venosus to inferior vena cava and gets mixed with deoxygenated blood.
Mixed Blood goes from IVC to right atrium. Also, Blood from SVC goes to right atrium. From the right atrium, blood goes to the right ventricle, then to pulmonary arteries to the lungs. Remember that pressure in Pulmonary vessels and lungs are very high due to fluid in alveoli.
Because of the very high pressure in the right side of the heart, some blood goes from the right atrium to left atrium through foramen ovale. Also, Blood from Pulmonary veins goes to the left atrium. From the left atrium to the left ventricle, blood goes to the aorta.
Also, Because of the high pressure in the pulmonary artery, blood passes to the aorta through a branch from pulmonary artery to the aorta, named Ductus Arteriosus. Blood goes from the aorta to umbilical artery then to the low-resistant placenta.
Intrauterine pulmonary blood flow is initially limited because of high pulmonary vascular resistance and the right-to-left shunting across the patent foramen ovale and patent ductus arteriosus.
- Blood supply from placenta is cut
- Ductus venosus closes due to unuse
- Pressure of the Right side of the heart falls
- Therefore, foramen ovale closes
- Pulmonary resistance falls because fluids are getting absorbed from the alveoli and replaced with air (infant started breathing)
- Blood goes from right ventricle to the pulmonary artery to get oxygenated in the lung
- Oxygenated Blood goes from pulmonary vein to the left atrium then left ventricle then aorta then IVC to the rest of the body
- Due to decrease pressure in pulmonary vessels, ductus arteriosus closes.
Important Physiologic Changes During Transition to Extrauterine Life
- Increased systemic vascular resistance with separation from the low-resistance placental vasculature
- Closure of right-to-left shunts
- Foramen ovale (closes when left atrial pressure greater than right atrial pressure)
- Ductus arteriosus (left-to-right flow within minutes of ventilation, then closure over days)
- Increased metabolic rate leading to higher glucose needs
- Increased catecholamine levels to support blood pressure
- Thyroid hormones surge after birth, possibly in response to the relatively cold extrauterine environment
Routine care of newborns
-
Umbilical cord should be cut within 30 sec after delivery
- Umbilical cord contains 2 arteries and one vein (Smiley face)
- Average length ~55cm
- 30% of congenital anomalies present with single umbilical artery
- Most common: Trisomy 18
- If Single umbilical artery is present, do renal US and echo to check for other anomalies

-
Place him/her under the radiant warmer to keep infant warm
- INFANT RADIANT WARMERS
Dry the infant thoroughly immediately after delivery with clean towel to prevent heat loss.
- Maintain a warm delivery room.
- Place the infant under a pre-warmed radiant warmer.
- Cover extremely preterm infants (<1500 g) with a plastic bag up to the neck, and place a portable warming pad under the layers of towel on the resuscitation table.

-
Stimulate the infant by rubbing the back and the feet to make him cry support spontaneous respiration
- Acceptable methods of stimulating a baby to breathe
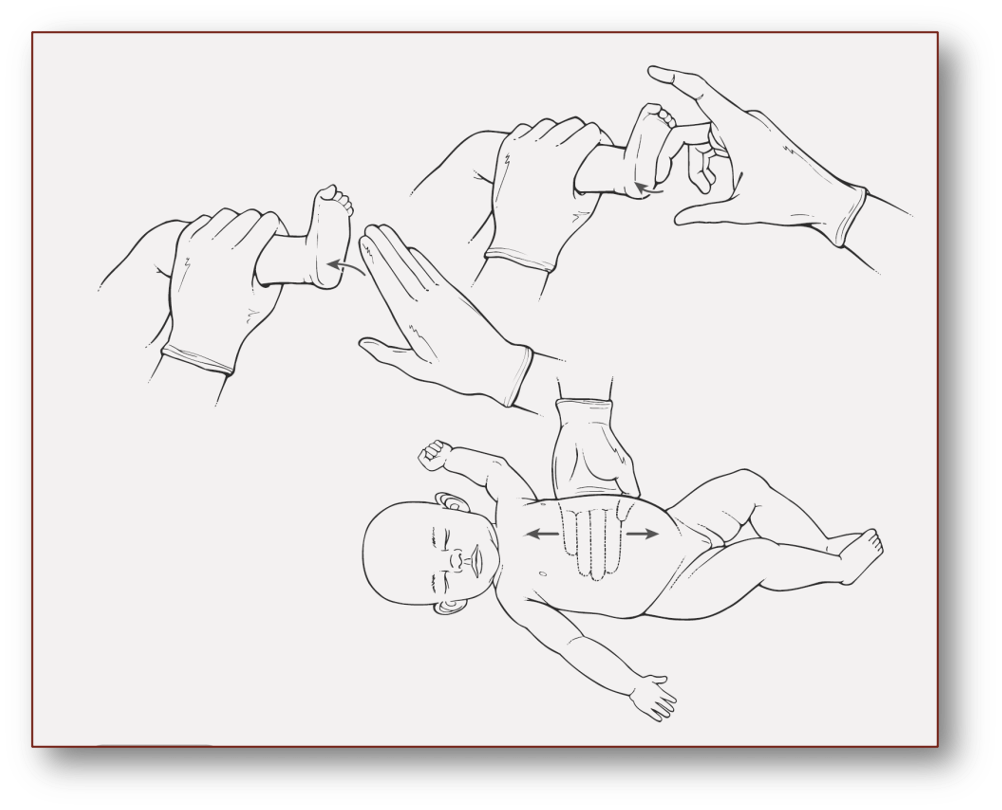
- Acceptable methods of stimulating a baby to breathe
-
Calculate APGAR score After delivery of infant, we check for Good muscle tone, Good crying effort, adequate Breathing, and Pink Central color. We also follow up oxygen saturation. Based on that we identify the APGAR SCORE.
The Apgar score is assigned at 1, 5, and 10 minutes of age.
It gives an objective retrospective idea of how much resuscitation is required at birth, and the infant’s response to resuscitative efforts.
During resuscitation, assessment of respiratory activity and heart rate provides the quickest and most accurate evaluation of the need for continuing resuscitation.
| APGAR Score | 0 (Points) | 1 | 2 |
|---|---|---|---|
| Appearance | Blue or pale all over | Blue extremities, but torso pink | Pink all over |
| Pulse | None | < 100 | ≥ 100 |
| Grimace | No response | Weak grimace when stimulated | Cries or pulls away when stimulated |
| Activity | None | Some flexion of arms | Active |
| Respirations | None | Weak, irregular or gasping | Strong cry |
Scoring Interpretation:
- 0-3 Critically Low
- 4-6 Fairly Low
- 7-10 Generally Normal
Acrocyanosis

-
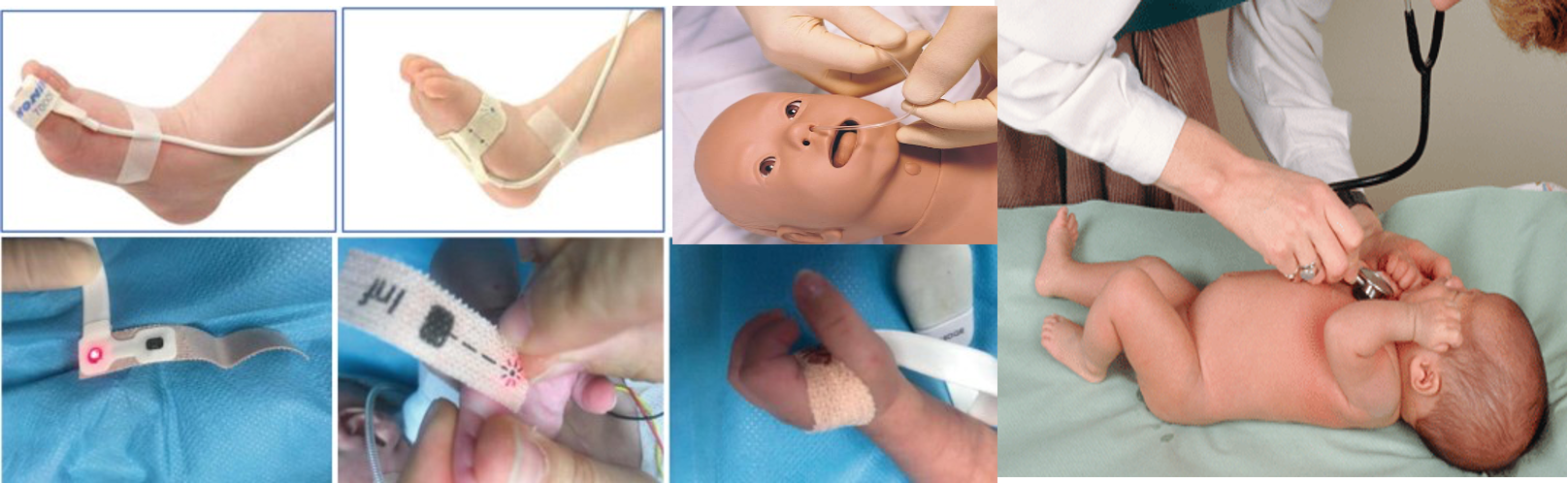
Position airway
-
Suction the oral cavity and the nostrils superficially
- Deep pharyngeal stimulation with a suction catheter may cause bradycardia and apnea that are probably of vagal nerve in origin, and this should be avoided.
-
Do full examination from head to toe
-
Skin-to-skin contact with the mother
Gestational Age
-
Gestational Age: the number of weeks in pregnancy since the 1st day of the last normal menstrual cycle - Preterm: ≤ 36 wk and 6 days - Term: 37 wk and 0 days to 41 wk and 6 days - Post-term: ≥ 42 wk
-
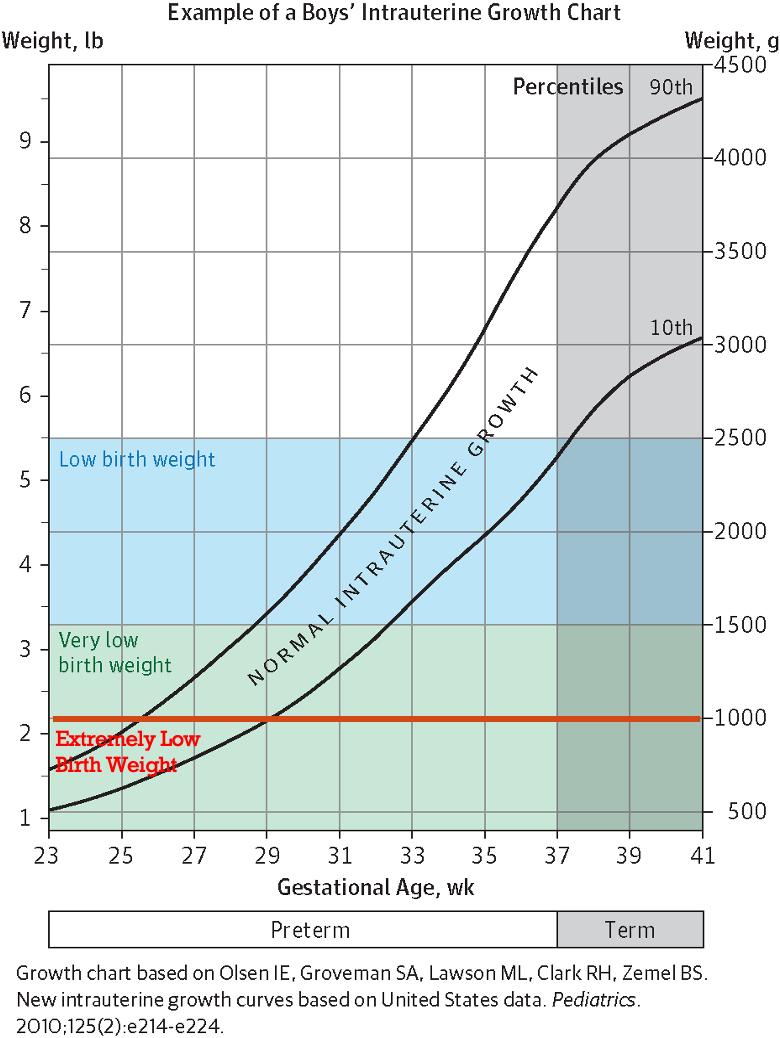
Appropriate for gestational age (AGA): infant with a birth weight between 10th and 90th percentile for the given gestational age
-
Small for Gestational age (SGA): infant with a birth weight < 10th percentile for the given gestational age
-
Large for Gestational age (LGA): infant with a birth weight >90th percentile for the given gestational age
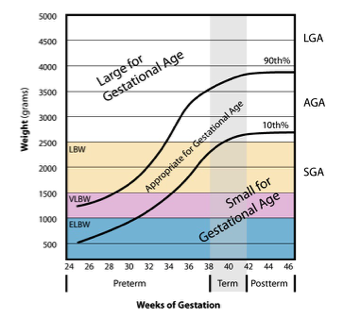
Birth Weight
| Category | Birth Weight |
|---|---|
| Normal | 2500 gr - 3500 gr |
| Low Birth Weight (LBW) | < 2500 g |
| Very Low Birth Weight (VLBW) | < 1500 g |
| Extremely Low Birth Weight (ELBW) | < 1000 g |
| Large Birth Weight | ≥ 4000 gr |
Intrauterine Growth Restriction
IUGR: Fetal weight < 10th percentile for gestational age
Risk Factors:
- Maternal Hypertension
- Smoking
- Malnutrition
- Ethanol ingestion
- Uterine and Placental Malformations causing decrease in uteroplacental flow
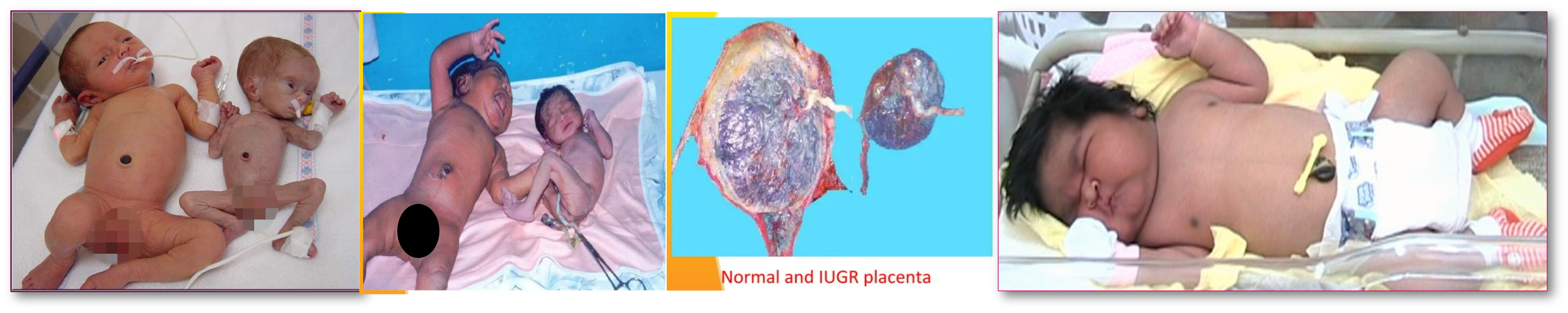
Symmetric vs Asymmetric
| Symmetric | Asymmetric |
|---|---|
| Occurs as a result of growth inhibition early in pregnancy | Occurs as a result of nutrient supply restriction in utero |
| Early onset | Late onset |
| Causes: TORCH, chromosomal disorders, congenital malformations | Causes: chronic hypoxia, malnutrition, chronic hypertension, renal disease |
| Growth of head and abdomen decreased equally | Head stays normal but abdominal growth slows down |
Appropriate & IUGR?
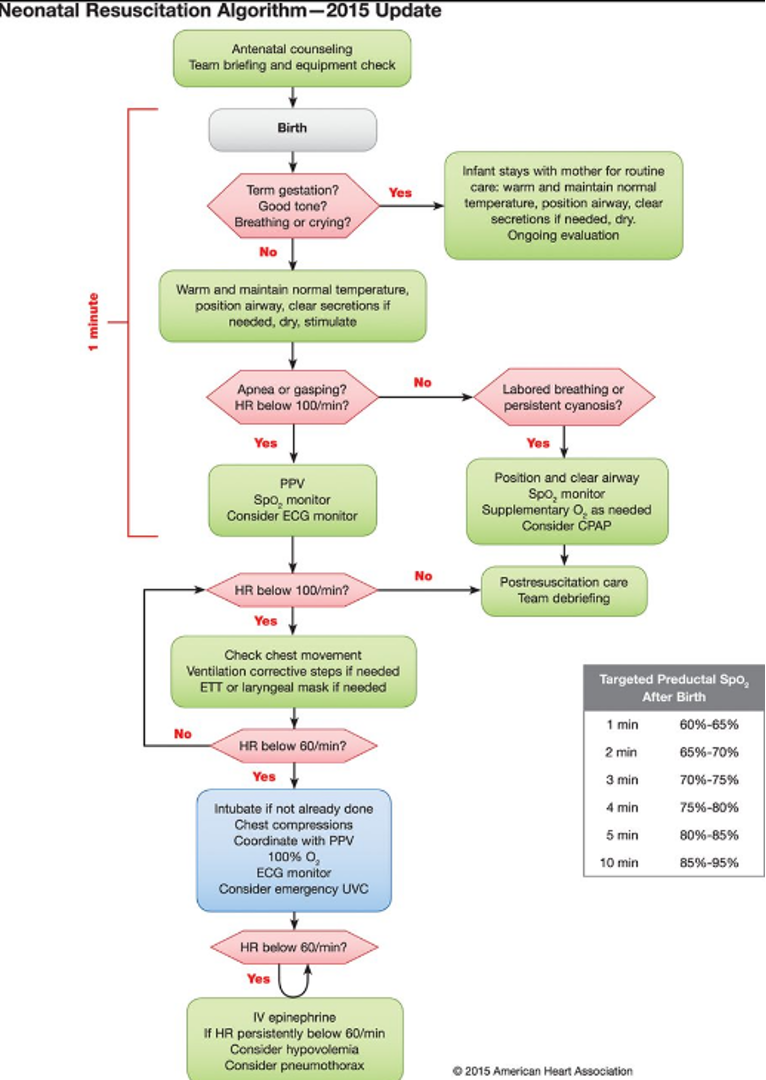
Neonatal Resuscitation
I- Positive pressure ventilation (PPV) is a noninvasive airway method that delivers oxygen continuously creating positive pressure during inspiration. Therefore bronchioles and alveoli are prevented from collapsing at the end of expiration.
! The stomach should be emptied during and after bag-and-mask ventilation by orogastric suctioning.
II- Endotracheal intubation is performed as indicated, and when PPV is not efficient.
III- If pulse is < 60 beats/min despite 30 seconds of positive-pressure ventilation, chest compression should be initiated.
A) Chest compressions Techniques:
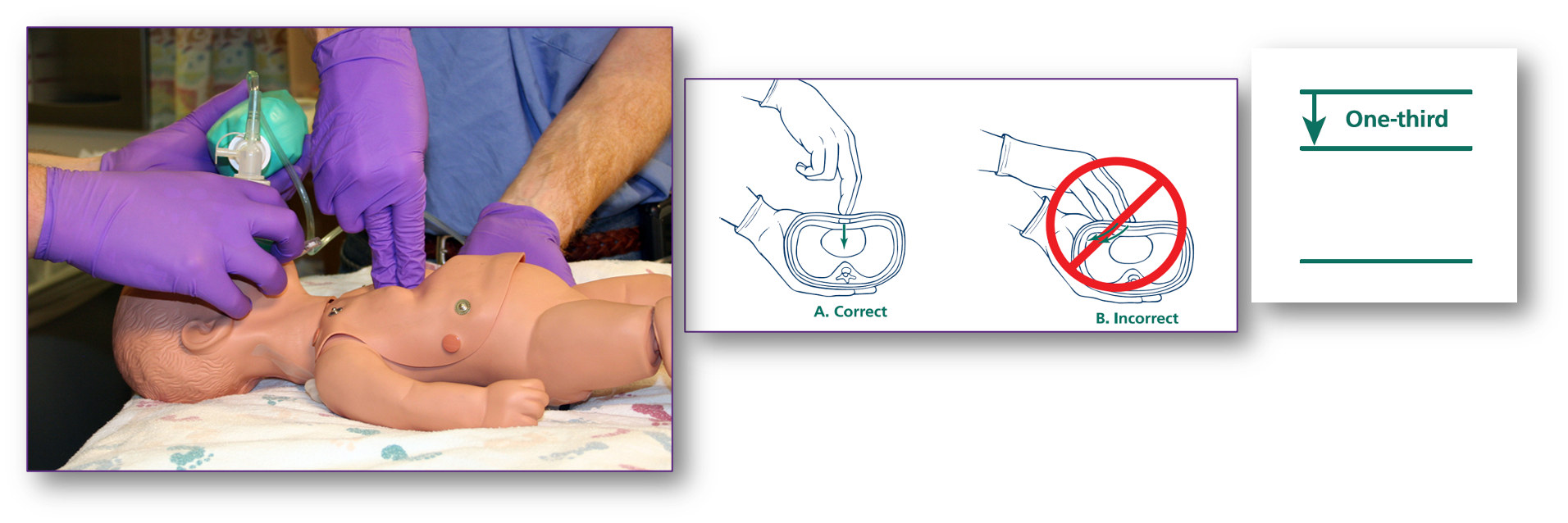
- Thumbs Technique
- 2-finger technique
B) Palpate for the central pulse in Brachial artery
C) The sternum is compressed ⅓ of the antero-posterior diameter (4 cm or 1.5 in) of the chest at a regular rate
D) If single rescuer, compression to breathing ratio is 30:2
E) If two rescuers, compression to breathing ratio is 15:2
IV- Epinephrine recommendations
- Route: Intravenous (preferred)/Intraosseous or Endotracheal every 3 to 5 minutes.
- Dose: 0.01mg/kg of 10,000 solution IV/IO (equal to 0.1 ml/kg) followed by 3 ml normal saline flush.Z
- Endotracheal tube dose is 0.1 mg/kg/dose (1ml/kg)
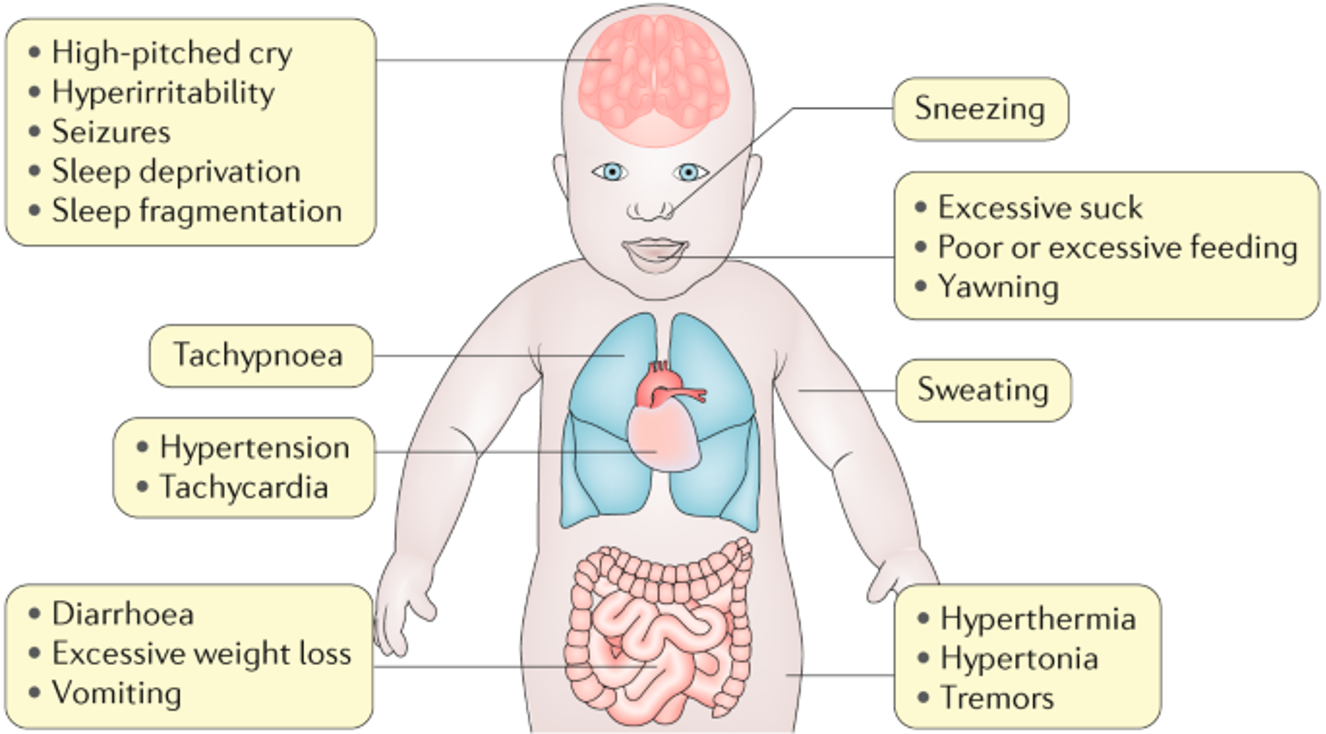
Other medications: Naloxone
- Naloxone is an opioid (narcotic antagonist) that is administered to an infant with neonatal Abstinence Syndrome secondary to mothers with opioid misuse (heroin/methadone). (sneezing, hypertension, high pitched cry most commonly presentation)
- The intravenous or intramuscular dosage for naloxone is 0.1 mg/kg to be repeated every 5 minutes, as necessary.
Bag-and-mask ventilation of the neonate.
- E and C hand positioning for good seal
- Baby in sniffing position

Thumbs Technique
- Thumbs are placed on the lower third of the sternum, between the xiphoid and the line drawn between the nipples, encircling the chest.
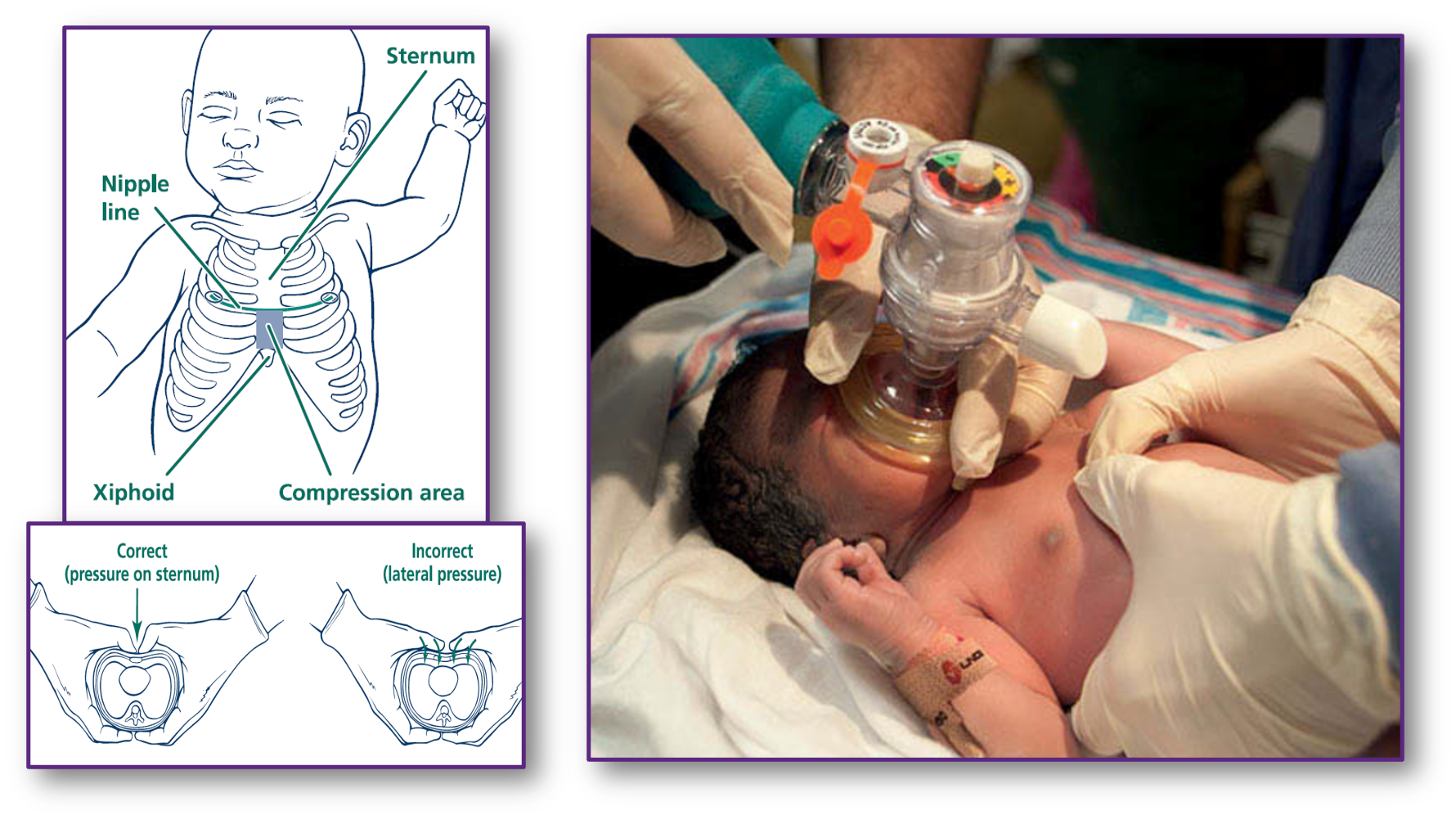
2-finger technique
- The middle and ring fingers of one hand can be placed on the sternum while the other hand supports the back.
In every CPR cycle
- Look for the reversible/treatable causes of cardiac arrest.
- The most common cause of bradycardia in children is hypoxia.
Reversible causes
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypoglycemia
- Hypo-/hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade, cardiac
- Toxins
- Thrombosis, pulmonary
- Thrombosis, coronary
Upon discharge
Three things are given to every neonate upon delivery:
- Potassium: single intramuscular dose or three oral doses to prevent hemorrhagic disease of newborn
- Hepatitis B vaccine: Hepatitis B immunoglobulin is added to babies whose mothers are hepatitis B positive
- Tetracycline/erythromycin ophthalmic drops to prevent gonorrheal conjunctivitis
Benign skin conditions in newborn
History
Perinatal history is divided into three stages:
-
Prenatal:
- Primi or no abortion
- Maternal blood group/RH status
- Maternal illnesses or infections (TORCH, HTN, DM)
- Antenatal screening test results (HAVsAg, blood group)
- Maternal medication or drug intake
-
Natal:
- Preterm or small for gestational age, post maturity, twins
- Mode of delivery and instrument use (e.g., birth trauma)
- Delayed cord clamping (possible polycythemia)
- Blood group of mother and baby
-
Postnatal:
- Admission to ICU, oxygen need, ventilator use, blood transfusion, fever, IV antibiotics, surgery, TPN
- Mother’s HBVsAg status and newborn test results (HBV vaccine, HBIG)
- Newborn screening test results (galactosemia, TSH)
Family History:
-
Consanguinity
-
Previous siblings with neonatal jaundice
-
Other family members with jaundice
-
Anemia or blood disorders
-
Splenectomy
-
Bile stones or gallbladder removal
-
Follow-up during pregnancy
-
Illnesses during pregnancy and their implications
-
Medications taken during pregnancy, such as Valproate and Phenytoin, and their potential risks
-
Effects of anabolic steroids
-
Radiation exposure during pregnancy
-
Fetal movement analysis to identify potential conditions
-
Conditions associated with Polyhydramnios and Oligohydramnios
-
Length of gestation
-
Mode of delivery
-
Measurements of birth weight, height, and head circumference
-
Apgar score evaluation
-
Neonatal disease or admission and its reasons
Nutritional History
- Breast fed or bottle fed
- For how long
- Which formula
- What volume does he take at each feed
- Frequency of feed
- Time of weaning and introducing solids and cereals