FERTILIZATION AND IMPLANTATION
By dr. Mona Ahmed
Introduction: Post-Ovulation Preparation
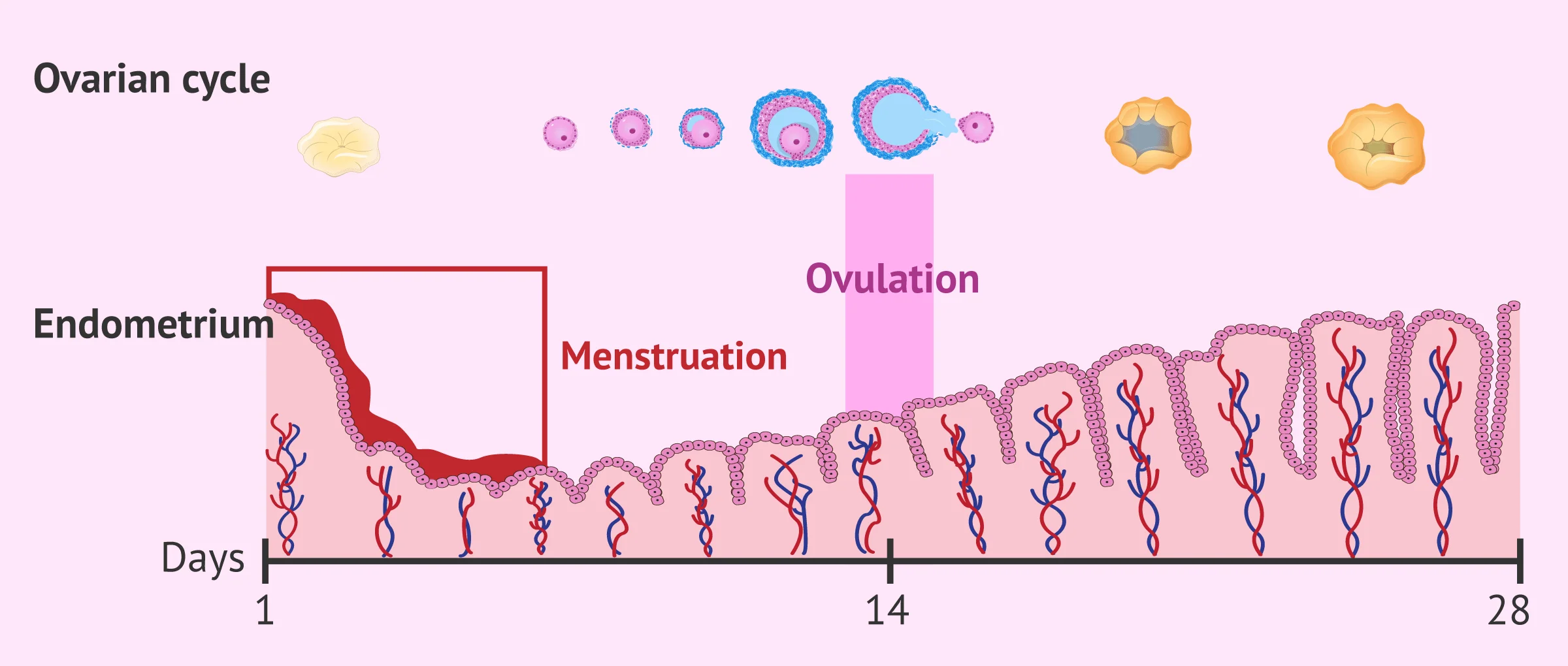
Endometrial Changes
After ovulation the cells of the dominant follicle & CL produces large amounts of progesterone which prepares the endometrium to support a pregnancy.
Fertilization Process
- Involves the fusion of two haploid gametes with 23 chromosomes each to produce a zygote that contains 46 chromosomes
- Fertilization generally occurs in the fallopian tube and generally within one day of ovulation.
- Both sperm and egg can show their vitality only to a limited period. Sperm is alive for 48-72 hours in a female reproductive system whereas the egg can be fertilized for 24 hours.
,,,,,,,,,,,,,,
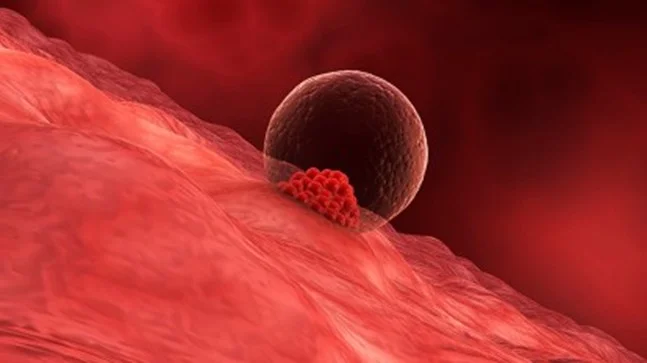
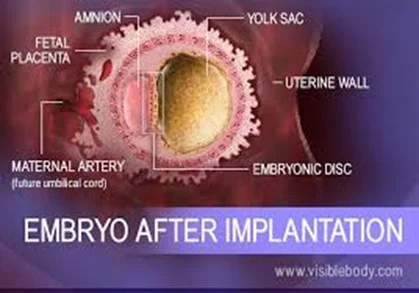
Implantation Process
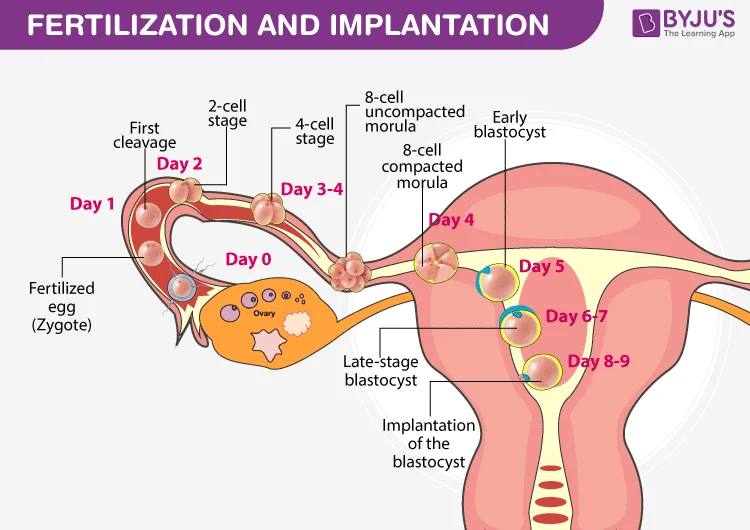
- After fertilization the zygote travels down the fallopian where it becomes a morula.
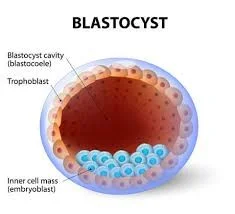
- Once it reaches the uterus, the morula becomes a blastocyst.
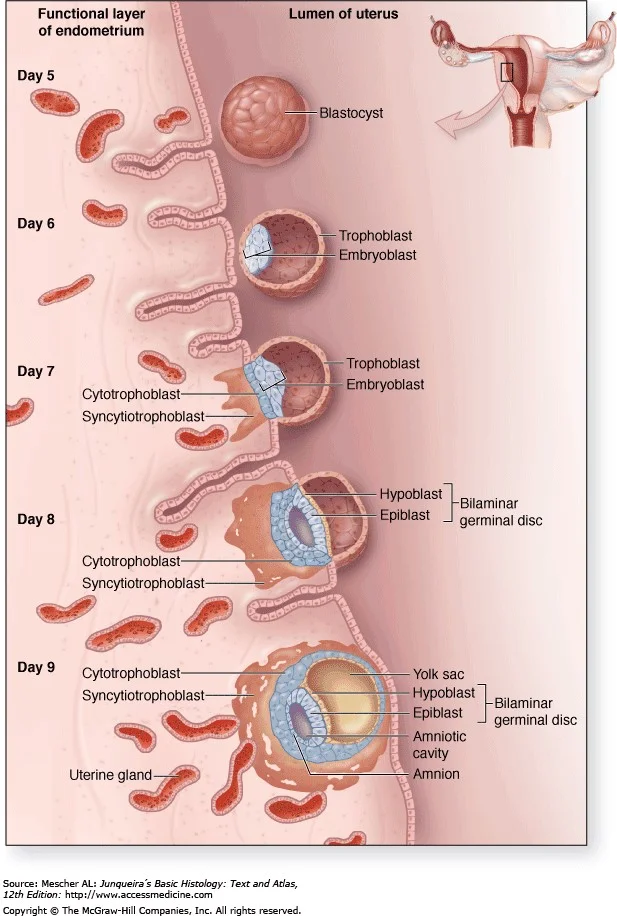
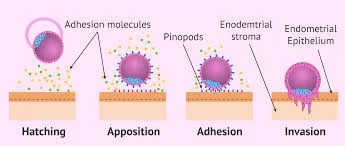
- The blastocyst then burrows into the uterine lining, a process called implantation.

Hormonal Regulation: Human Chorionic Gonadotrophin (hCG)
hCG Secretion and Physiological Role
The implanted blastocyst secretes human chorionic gonadotrophin (hCG):
- ‘rescue CL from luteolysis to maintain progesterone secretion.
- prevent menstruation.
- and support the early conceptus (for approximately 8 weeks).
- after which the early placental tissue becomes the main source of progesterone.
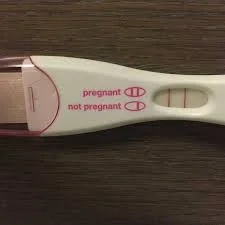
hCG Detection in Pregnancy
- hCG can be detected in the urine in sensitive pregnancy tests 1 or 2 days before the expected date of menstruation.
- Most women delay taking a pregnancy test until after a missed period.
Visualizing Early Pregnancy
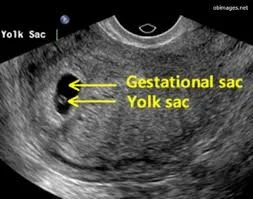
Ultrasound Detection of Gestational Sac and Embryo
-
A transvaginal ultrasound scan (TVUSS) can detect an early intrauterine gestational sac, the first sign of a normal pregnancy, at around 5 weeks’ gestation.
-
A few days later a circular yolk sac can be seen within the gestational sac, and the embryonic fetus can usually be identified after 5.5 weeks’ gestation.
-
The fetal heartbeat may be visible as early as 6 weeks’ gestation.

Ultrasound Imaging Parameters
 #CC VID
#CC VID
Embryonic Structure Post-Implantation
Clinical Manifestations of Implantation
Symptoms and Signs
- Gastrointestinal disorders
- Breast swelLLING
- Nausea
- Implantation bleeding
- Increased urge to urinate
hCG (human chorionic gonadotropin)
-
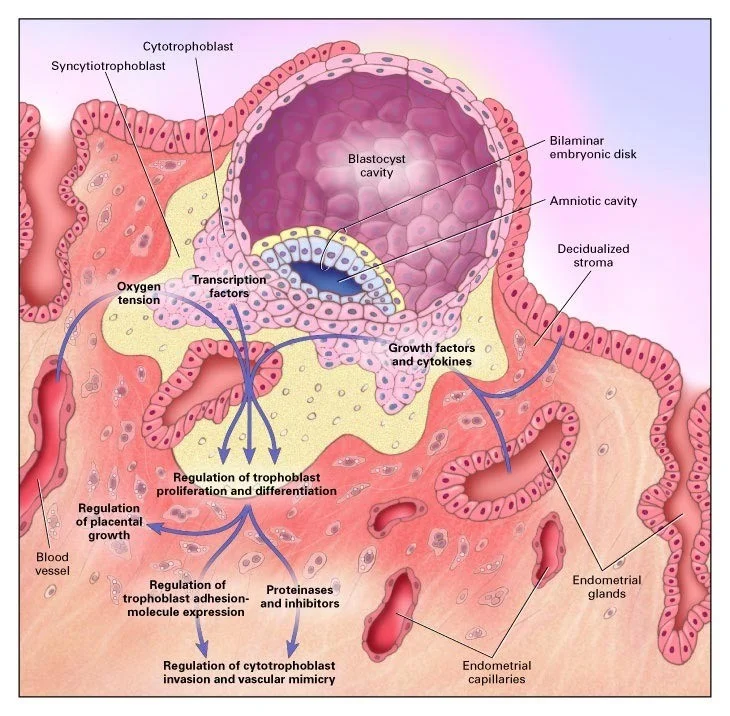
Primarily produced by syncytiotrophoblasts.
-
Detected from 6 days after fertilization; forms basis of modern pregnancy testing.
-
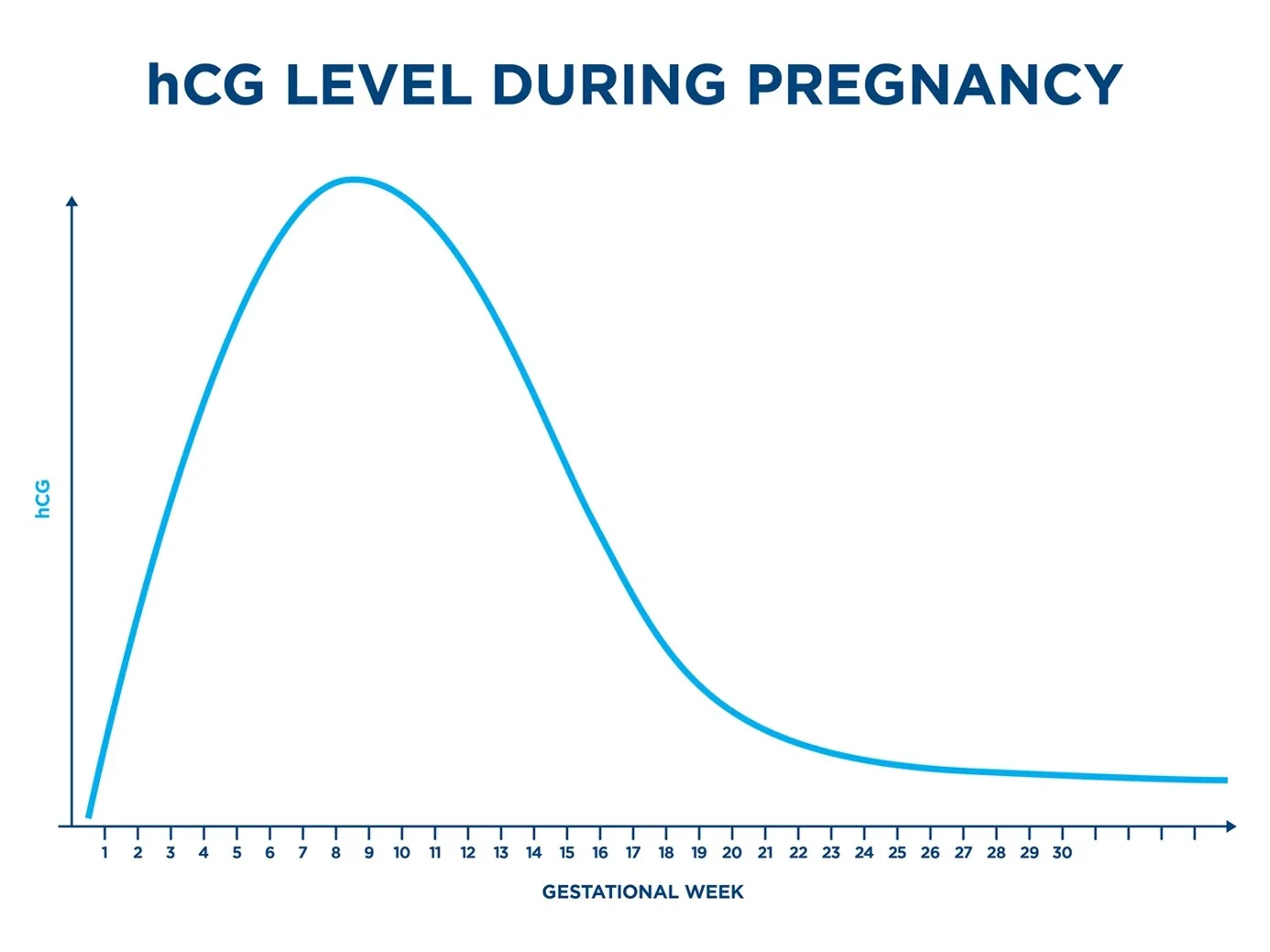
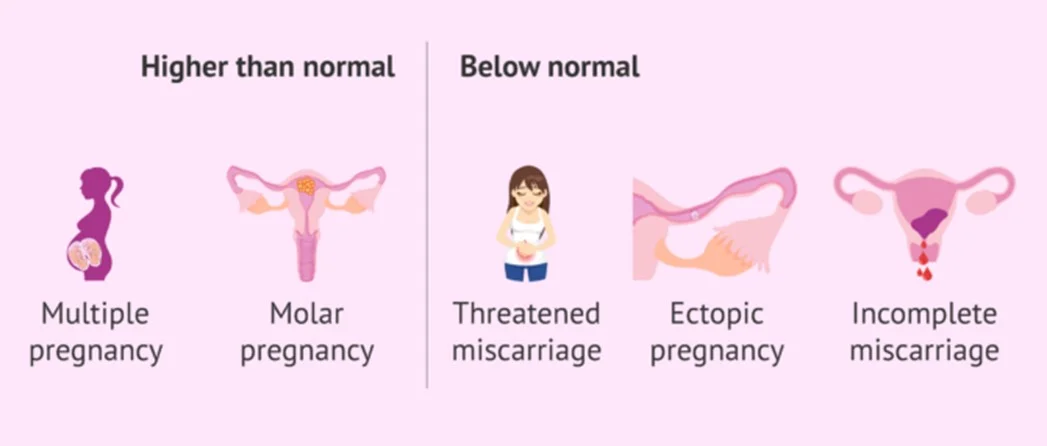
Concentrations reach a peak at 10–12wks gestation, then plateau only after 13 weeks until remainder of the pregnancy. - beyond 13 weeks is abnormal, may be due choriocarcinoma Molar pregnancy can produce very high hCG levels, which often result in nausea and vomiting—symptoms similar to those of a normal pregnancy.
Effect
- continuation of pregnancy
- Maintenance of the corpus luteum graviditatis
- Stimulation of progesterone and estrogen synthesis of the corpus luteum graviditatis
Detailed Characteristics and Effects of hCG
- ✓ Primarily produced by syncytiotrophoblasts.
- ✓ Detected from 6 days after fertilization; forms basis of modern pregnancy testing.
- ✓ Concentrations reach a peak at 10-12wks gestation, then plateau for remainder of the pregnancy.
- Effect
- ✓ continuation of pregnancy
- ✓ Maintenance of the corpus luteum graviditatis
- ✓ Stimulation of progesterone and estrogen synthesis of the corpus luteum graviditatis
Comparison Table: Maternal Complications
| Condition | Key Diagnostic Features | Critical Management | Unique Risks |
|---|---|---|---|
| Hyperemesis Gravidarum | >5% weight loss, dehydration, ketonuria, no other cause | IV fluids (RL/NS), thiamine first, then B6 + doxylamine | Wernicke encephalopathy, fetal growth restriction |
| Cervical Insufficiency | Painless dilation <24w, history of 2nd-trimester loss | Cerclage (McDonald/Shirodkar), vaginal progesterone | Preterm birth, PPROM |
| Chorioamnionitis | Maternal fever >38°C + fetal tachycardia/malodorous fluid | IV ampicillin + gentamicin (+ clindamycin if C-section) | Neonatal sepsis, maternal DIC |
| Pemphigoid Gestationis | Periumbilical blisters/itching, “herpetiform” lesions | Topical/systemic glucocorticoids | Preterm labor, fetal rash |
| Polymorphic Eruption (PEP) | Pruritic papules in striae, spares umbilicus | Low-potency steroids, antihistamines | None (benign) |
| Pregnancy Luteoma | Solid ovarian mass, maternal/fetal virilization | Expectant management (resolves postpartum) | Premature labor (if large) |
Essential Hyperemesis Takeaways:
- Emergency Protocol:
- Rule out moles/infection → Ultrasound, β-hCG, U/A.
- IV Fluid: LR/NS (not dextrose initially).
- Thiamine (100mg IV) → before any glucose to prevent Wernicke’s.
- Antiemetics: Pyridoxine (B6) + doxylamine (1st-line), then ondansetron.
- Diet: Small dry-carb meals; avoid triggers (strong smells, iron supplements).
- Discharge Criteria: Tolerating oral intake, ketonuria resolved, weight stable.