IM
A collection of air within the pleural cavity that can lead to partial or complete pulmonary collapse.
Classified as: Spontaneous pneumothorax:
- Primary SP: Without clinically apparent underlying lung disease.
- Secondary SP: A complication of underlying lung disease. * Recurrent pneumothorax: A second episode of SP either ipsilateral or contralateral.
Traumatic pneumothorax: Caused by trauma (e.g., penetrating injury, blunt, iatrogenic trauma: mechanical ventilation).
-
Iatrogenic pneumothorax: Complication of medical procedures (thoracentesis, CV placement, ventilation, including non-invasive ventilation or lung biopsy).
-
Tension pneumothorax: A life-threatening condition characterized by progressively increasing pressure within the chest and cardiorespiratory compromise. It can lead to severe respiratory distress and haemodynamic collapse.
Aetiology and Epidemiology of Pneumothorax
Primary pneumothorax: Caused by rupture of apical pleural bleb due to a congenital defect in the connective tissue of the alveolar wall.
Risk factors:
- Family history
- Male sex (M:F ratio 6:1)
- Young age
- Asthenic body habitus (slim, tall stature)
- Smoking (90% of cases): Up to 20-fold increase
- Homocystinuria
- Marfan Syndrome
Secondary pneumothorax: Commonest causes:
- COPD: Rupture of emphysema bullae
- Bronchial asthma
- Carcinoma
- Lung abscess - bronchopleural fistula
- Cystic fibrosis: Severe pulmonary fibrosis with cyst formation
- Infections: TB, Pneumocystis pneumonia
- Catamenial pneumothorax: Rare
Pneumothorax: Clinical Features
-
Asymptomatic
-
Sudden, severe, and/or stabbing, ipsilateral pleuritic chest pain and dyspnea.
-
Physical signs:
- Chest movement reduced on the affected side.
- Mediastinal shift: Trachea shifted to the opposite side.
- Percussion note - hyper-resonant
- Breath sound - reduced or absent
- Vocal resonance - reduced or absent
- Added sound - none
- Subcutaneous emphysema
-
Additional findings in tension pneumothorax:
- Valvular mechanism: When air is sucked into the pleural space during inspiration but not expelled during expiration, leading to ↑ pleural pressure, lung collapse, and mediastinum shift. This will ↓ venous return and ↑ respiratory difficulty.
- Clinically:
- Severe acute respiratory distress: Cyanosis, restlessness, sweating
- Distended neck veins
- Hemodynamic instability (tachycardia, hypotension, pulsus paradoxus)
- Secondary injuries (open or closed wounds).
P-THORAX: Pleuritic pain, Tracheal deviation, Hyperresonance, Onset sudden, Reduced breath sounds (and dyspnea), Absent fremitus, X-rays show collapse.
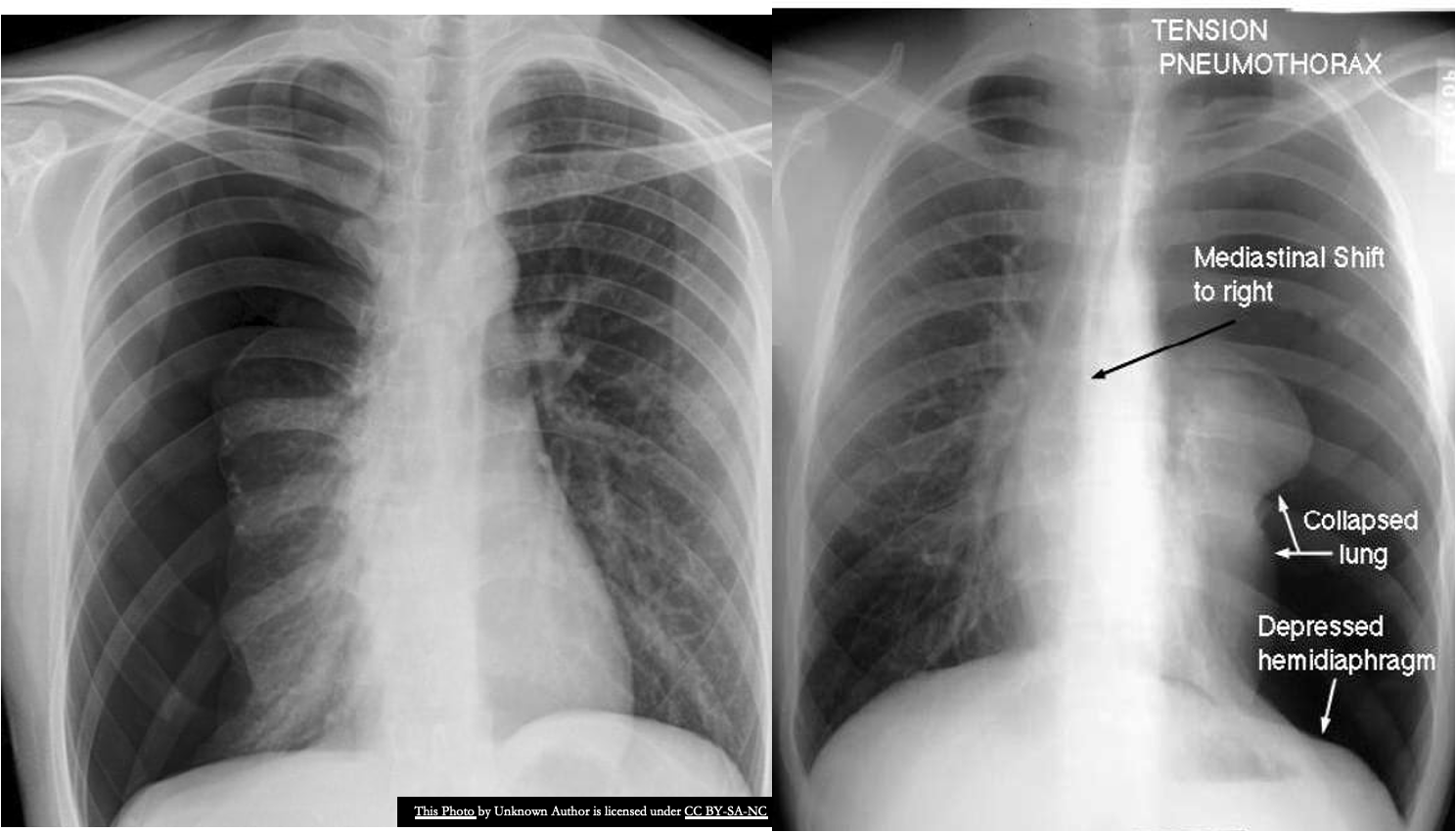
Tension Pneumothorax
- Normally intrapleural pressure is negative.
- In pneumothorax, it becomes positive leading to collapse of the lung.
- In cases of tension pneumothorax, immediate decompression is a priority and should not be delayed by imaging.
There are completely absent lung markings on the right, with the right lung collapsed and pushed across into the left hemithorax, along
with the mediastinal contents.
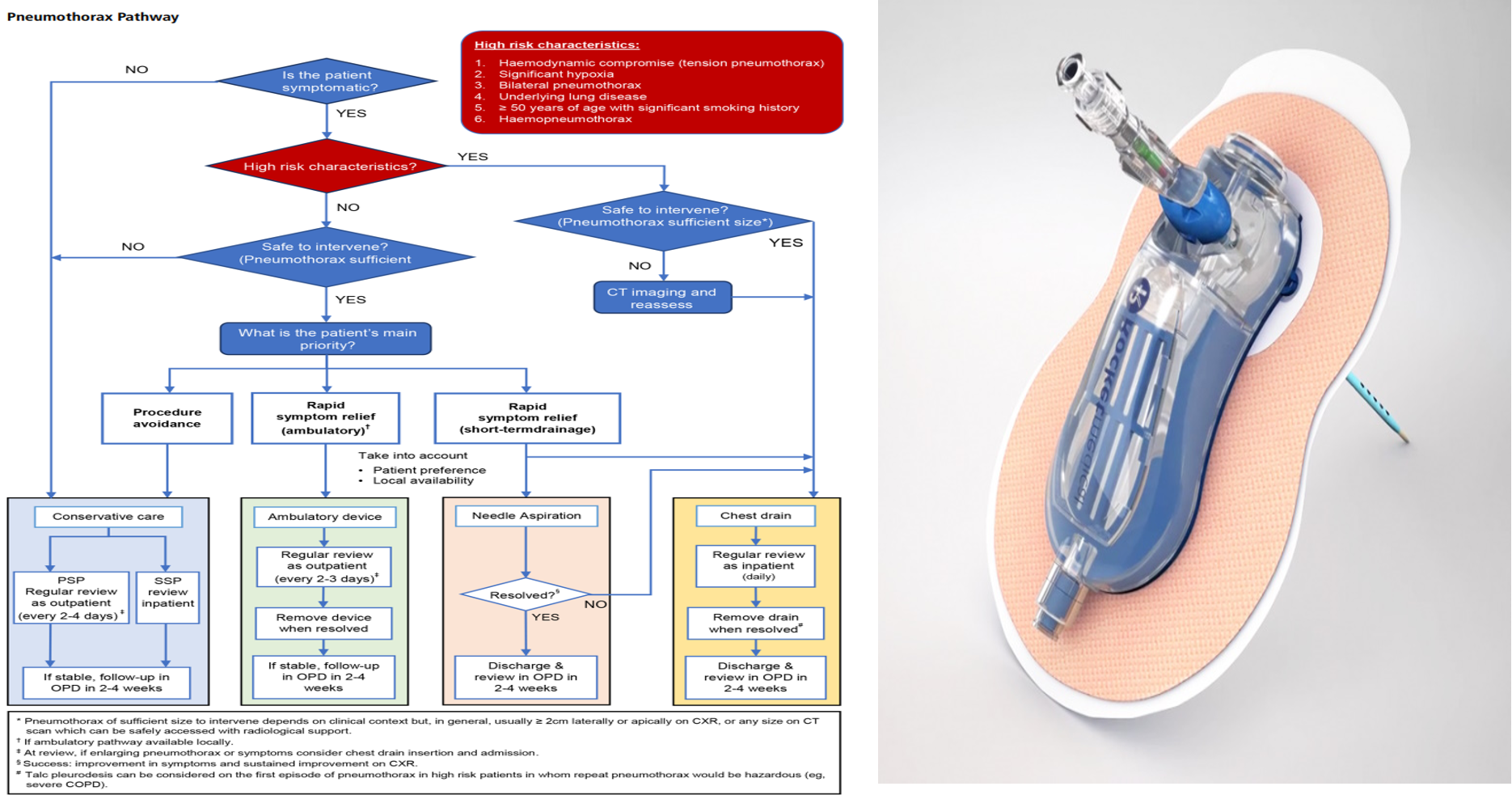
Pneumothorax: Management
Kumar : 974 Respiratory disease
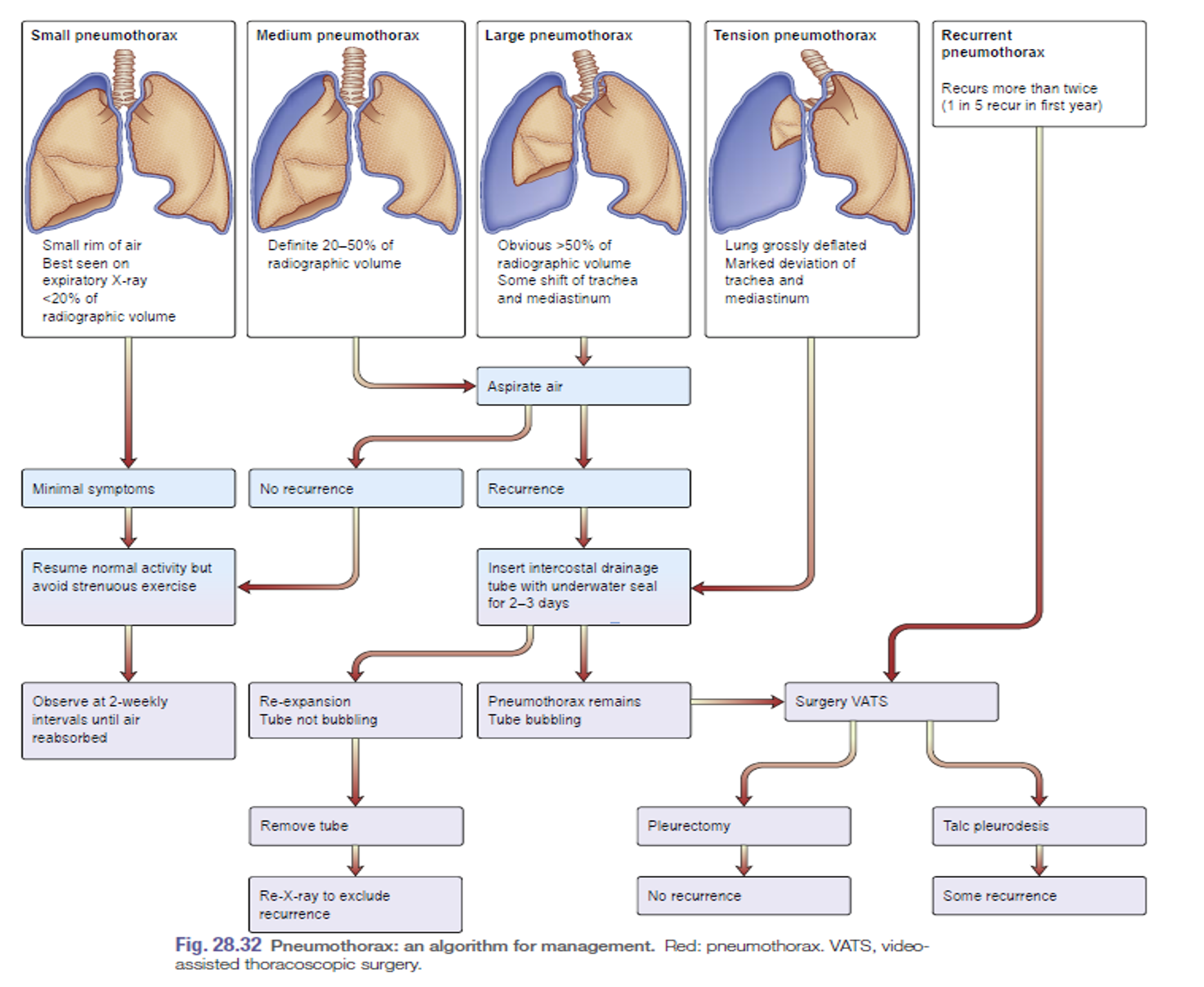 Small Pneumothorax:
< 20% of radiographic volume (best seen in expiratory film). Minimal symptoms.
Small Pneumothorax:
< 20% of radiographic volume (best seen in expiratory film). Minimal symptoms.
- Observe for 2 weeks until air is reabsorbed.
- Resume normal activity but avoid strenuous exercise.
Moderate Pneumothorax: When there is 20-50% of radiographic volume. Aspirate air.
Large Pneumothorax: When more than 50% of the radiographic volume and it causes shift of the trachea and mediastinum.
- Aspirate air.
- If reoccurrence, insert intercostal drainage tube with underwater seal for 2-3 days.
- Look for reexpansion (tube not bubbling) and remove the tube and do X-ray chest.
Management of Tension Pneumothorax: Causes collapse of the lung and shifting of the trachea and mediastinum to the opposite side.
- Aspirate air until preparing the drain.
- Insert intercostal drainage tube with underwater seal for 2-3 days.
- Look for reexpansion (tube not bubbling) and remove the tube and do X-ray chest.
Safe Triangle:
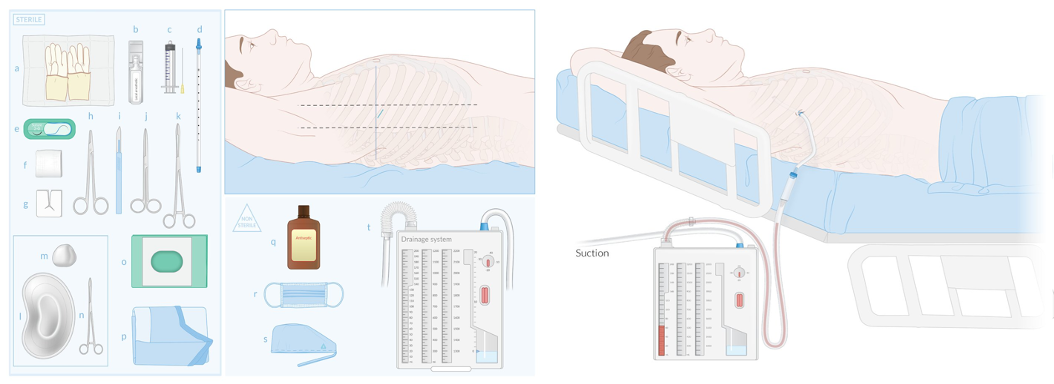
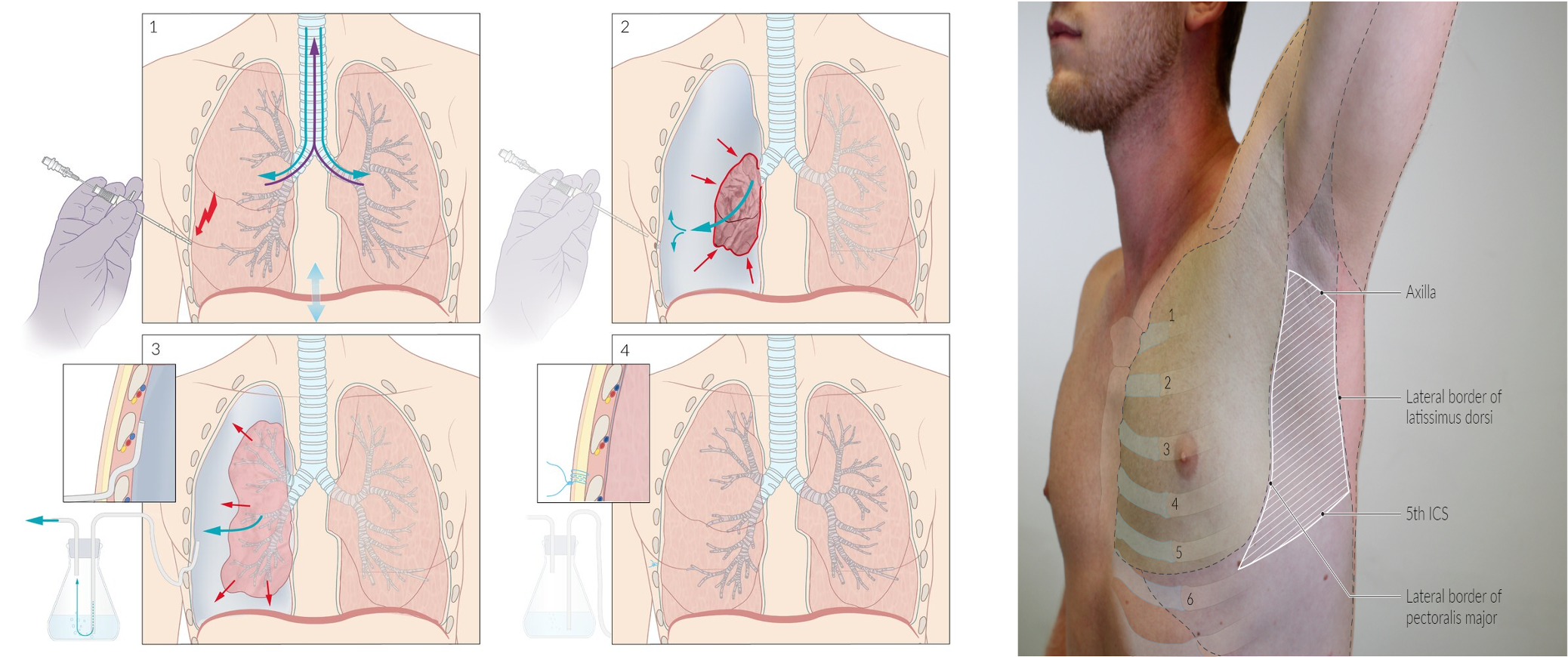
Rocket® Pleural Vent™:
- It includes an 8FG catheter mounted on an 18G needle and a pigtail catheter to minimize the risk of occlusion.
- Ambulatory devices typically have a one-way valve and vent to prevent air and fluid return to the pleural space while allowing for controlled escape of air and drainage of fluid.
- Many devices also have an indication diaphragm that signals when the catheter tip enters the pleural space and continues to fluctuate with respiration, aiding in the assessment of pneumothorax resolution.
Pneumothorax: Discharge Advice
- Smoking: Avoid smoking to reduce the risk of further episodes. The lifetime risk for smoking men is around 10% compared with around 0.1% in non-smoking men.
- Fitness to fly: 1 week post check X-ray.
- Scuba diving: The BTS guidelines state: ‘Diving should be permanently avoided unless the patient has undergone bilateral surgical pleurectomy and has normal lung function and chest CT scan postoperatively.‘
Imaging
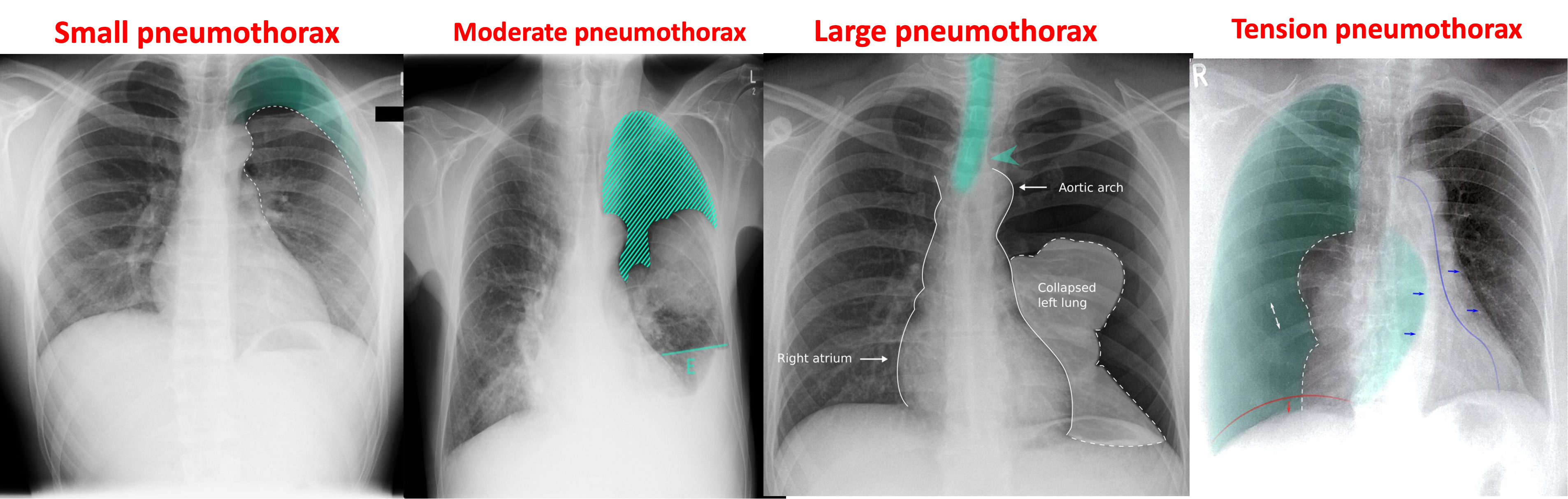
Patients with pneumothorax usually present with sudden-onset dyspnea, ipsilateral chest pain, diminished breath sounds, and hyper resonant percussion on the affected side.
Tension pneumothorax further manifests with distended neck veins, tracheal_deviation , and hemodynamic instability.
Unstable patients with tension pneumothorax (life-threatening) require immediate needle decompression.
-
The diagnosis of pneumothorax is usually confirmed by chest x-ray.
-
CT can provide information about the underlying cause (e.g., bullae in spontaneous pneumothorax).
-
*Tension pneumothorax is primarily a clinical diagnosis and prolonged diagnostic studies should be avoided *In cases of tension pneumothorax, immediate decompression is a priority and should not be delayed by imaging.
Signs of pneumothorax
A) Supportive findings of pneumothorax
- Ipsilateral pleural line with reduced/ absent lung markings (i.e., increased transparency)
- Abrupt change in radiolucency
B) Supportive findings of Tension pneumothorax
- Ipsilateral diaphragmatic flattening/inversion and widened intercostal spaces.
- Mediastinal_shift toward the contralateral side.
- Tracheal_deviation toward the contralateral side.
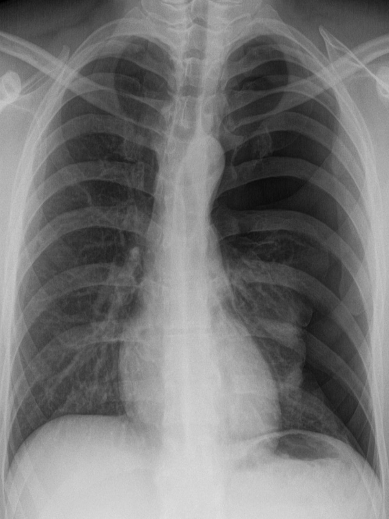
Spontaneous pneumothorax
Chest x-ray (PA view) Within the left lung, a thin convex line can be seen, beyond which there are no lung markings. Mediastinal structures are shifted to the contralateral side . Note the prominent tracheal deviation.
*As this patient has no history of trauma to the thoracic wall or lungs, these features are indicative of a spontaneous pneumothorax.
Right anterior pneumothorax
CT thorax (axial view; lung window)
There is a loss of bronchovascular markings over the anterior aspect of right lung.
These findings are pathognomonic of right anterior pneumothorax.
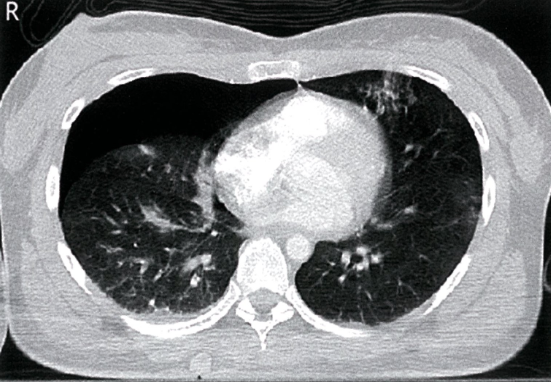
Hydropneumothorax
- Middle age patient with cough fever and weight loss since months.
- Air and fluid in the pleural cavity.
- Look at the air fluid level