Hx of a lump or an ulcer
Does the lump ever disappear? A lump may disappear on lying down, or during exercise, and yet be irreducible at the time of
Duration When was it first noticed?
First symptom What brought it to the patient’s notice?
Other symptoms What symptoms does it cause?
Progression How has it changed since it was first noticed?
Persistence Has it ever disappeared or healed? (diabetic foot)
Multiplicity Has (or had) the patient any other lumps or ulcers? (lymphonedapathy), (neurofibromatosis)
lipoma - benign (excision)
Multiple Painful Lipoma - Dorcum's disease
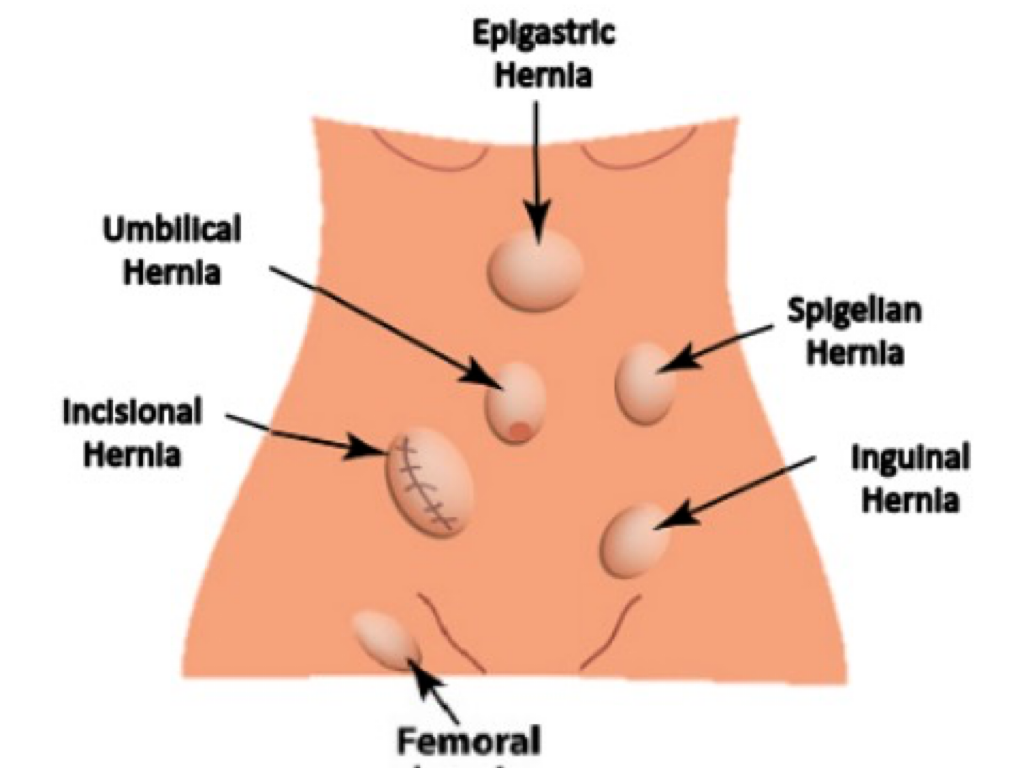
Hernia - (Repair/Suture or Excision)
I&D - Abscess drainage
Cause What does the patient think caused it?
Shape Remember that lumps have three dimensions. You cannot have a circular lump because that is a plane figure. Many lumps are not regular hemispheres, but have an asymmetrical shape. In these circumstances, it is permissible to use descriptive terms such as pear shaped or kidney shaped.
Size Once the shape is established, it is important to measure its various dimensions. Again, remember that all solid objects have at least three dimensions: width, length and height or depth. Some lumps will need more measurements to describe them accurately; sometimes a diagram may clarify your written description.
Surface The first feature of the lump that you will notice when you feel it will be its surface, whether smooth or irregular. An irregular surface may be covered with smooth bumps, rather like small stones, which can be called bosselated. It may be flat or rough.
There may be a mixture of surfaces if the lump is large.
Temperature Is the lump hot or of normal temperature? Assess the skin temperature with the palmar surfaces of your fingers, because they are sensitive (free of sweat) and cool.
HISTORY AND EXAMINATION OF A LUMP
History
Most patients with a lump feel it frequently and should be able to tell you about the history of its clinical features. Therefore you should seek answers to the following questions.
-
When was the lump first noticed?
It is important to be precise with dates and terminology. Do not write ‘the lump first
The presence or absence of pain is important, particularly if it is the presenting feature. In very general terms, pain is usually associated with inflammation, not neoplastic change. Most
Revision panel 1.11
The examination of a lump or ulcer
Local examination
- Site (right neck swelling)
- Size (0.2x0.8 Meters use ruler)
- Shape (Irregular, regular)
- Surface (feel surface Nodular or Smooth)
- Depth (Deep or superficial - check contraction after squeeze hand)
- Colour (strawberry, portwine?, purple, orange, chronic inflammation; hyperpigmentaiton, redness; active inflammation )
- Temperature ( Hot; Abscess, Malignancy , Cold, Normal; Lipoma)
- Tenderness (Painful or Painless)
- Edge (Ill-defined or well-defined) feel the edge?
Composition: Solid, fluid or gas
- consistency (Hard/Firm/Soft like?)
- fluctuation (Fluid; Cyst - Pseudocyst; without epithelium)
- fluid thrill ()
- translucence (Torch; hydrocele - any cyst vs hernia)
- resonance
vascular
-
pulsatility (Transmitted/True? - aneurysm, varicose) - Expansile vs transmission (two finger))
-
compressibility (Tumour/Hernia/)
-
bruit (Turbulence/Murmur - thrill if palpable)
- Reducibility (Renal Hernia, cough)
- Relations to surrounding structures – mobility/fixity
- Regional lymph glands (Malignancy/Infection — Primary / Secondary
State of local tissues:
- Arteries (examine arteries before & after the swelling (Parathesia, loss of pulse etc..))
-
nerves
-
Bones and joints
Superficial splemelanoma/Sprengeng??? most common type
Types of Ulcer
| Feature | Venous | Arterial | Neuropathic Diabetic | Pressure |
|---|---|---|---|---|
| Underlying condition | Varicose veins, previous deep-vein thrombosis, obesity, pregnancy, recurrent phlebitis | Diabetes, hypertension, smoking, previous vascular disease | Diabetes, trauma, prolonged pressure | Limited mobility |
| Ulcer location | Area between the lower calf and the medial malleolus | Pressure points, toes and feet, lateral malleolus and tibial area | Plantar aspect of foot, tip of the toe, lateral to fifth metatarsal | Bony prominences, heel |
| Ulcer characteristic | Shallow and flat margins, moderate-to-heavy exudate, slough at base with granulation tissue | Punched out and deep, irregular shape, unhealthy wound bed, presence of necrotic tissue, minimal exudate unless infected | Deep, surrounded by callus, insensate | Deep, often mace |
| Condition of Leg/Foot | Hemosiderin staining, thickening and fibrosis, skin, limb edema, normal capillary refill | Thin shiny skin, reduced hair growth, cool skin, pallor on leg elevation, absent or weak pulses, delayed capillary refill, gangrene | Dry, cracked, insensate, calluses | Atrophic skin, loss of muscle mass |
| Treatment | Compression therapy, leg elevation, surgical management | Revascularization, Anti-Platelet medications, Management of risk factors | off-loading of pressure, topical growth factors | Off-loading of pressure; Reduction of excessive moisture, shear, and friction; adequate nutrition |
 |
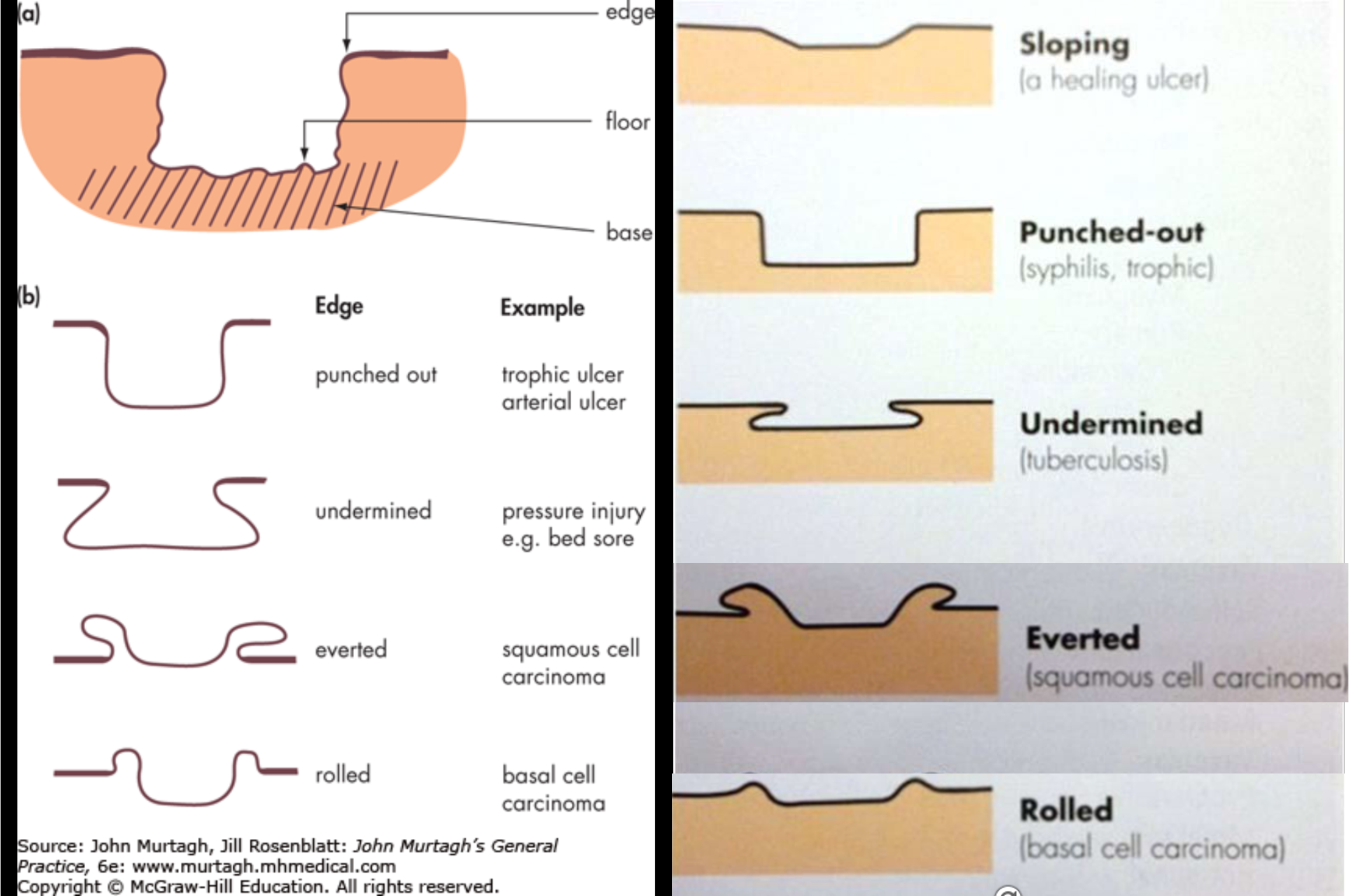
Inspection - Floor
- Red; clean granulation; fibronogen; loop of capilarry
- Black
Palpation - Base ()
Edge
- Sloping - healing ulcer
- Undermined - Bedsores (sacral, trochantric, scalp) - decubitus ulcer, pressure
- Punched-out
- Everted - SCC
- Rolled - BCC
Comparison of the three major types of leg ulcers
| Venous | Arterial | Neuropathic | |
|---|---|---|---|
| History | Prior deep venous thrombosis, stroke, miscarriages Obesity, multiple pregnancies Pain upon prolonged standing | Cigarette smoking Diabetes Dyslipidemia Intermittent claudication | Diabetes Other causes of peripheral neuropathy |
| Location | Gaiter distribution Malleolar regions (medial > lateral) | Pressure sites Distal points (toes) | Pressure sites |
| Pain | Mild to moderate | Severe | Painless |
| Morphology | Irregular borders Shallow | Necrotic eschar Punched out | Punched out |
| Surrounding skin | Pigmentation secondary to hemosiderin Lipodermatosclerosis | Shiny atrophic skin with hair loss | Thick callus surrounding ulcer |
| Other physical examination findings | Varicosities Peripheral edema Stasis dermatitis | Weak/absent peripheral pulses Prolonged capillary refilling time (>3 to 4 seconds) Pallor on leg elevation (45° for 1 min) | Peripheral neuropathy with decreased sensation |
| Relevant studies | Duplex ultrasonography | Ankle-brachial index Computed tomography angiography (CTA) Magnetic resonance angiography (MRA) |
Etiologies of leg ulcers
Common
| Category | |
|---|---|
| Venous | |
| Arterial | |
| Neuropathic |
Uncommon
| Category | |
|---|---|
| Physical | Thermal burns, cold injury, radiation, trauma, factitial |
| Bites | Spider |
| Infection | Bacterial, fungal, spirochete, protozoal |
| Vasculopathies | Livedoid vasculopathy, Buerger’s disease |
| Hypercoagulable states (inherited and acquired) | Factor V Leiden, antiphospholipid antibody syndrome, protein C and S deficiency, anti-thrombin III deficiency, prothrombin G20210A mutation, hyperhomocysteinemia and methylenetetrahydrofolate reductase (MTHFR) polymorphism |
| Vaso-occlusive disorders | Calciphylaxis, cholesterol emboli, type I cryoglobulinemia, cryofibrinogenemia, oxalosis |
| Vasculitis (small and medium-sized vessel) | Henoch-Schönlein purpura, rheumatoid vasculitis, mixed cryoglobulinemia, polyarteritis nodosa, granulomatosis with polyangiitis, lupus erythematosus |
| Pyoderma gangrenosum | IBD |
| Necrobiosis lipoidica | DM |
| Panniculitis | Alpha-1-antitrypsin deficiency, pancreatic fat necrosis, erythema induratum (nodular vasculitis) |
| Neoplastic conditions | Squamous cell carcinoma, basal cell carcinoma, cutaneous T and B cell lymphoma, Kaposi’s sarcoma |
| Systemic sclerosis | |
| Hematologic disease | Hemoglobinopathies, thrombocytosis |
| Drugs | Hydroxyurea, warfarin, heparin |
| Metabolic | Calcinosis cutis, gout, prolidase deficiency, leukocyte adhesion deficiency, Werner syndrome |

- Umbilicus hernia (crescent sign)
- Everted & swelling of Umbilicus, distended abdomen (put your hand for palpable hernia) (repair surgery) (para-hernia commonly in adults) ++ ascites/pregnancy
- Midline scar, multiple…
- Midline scar, RT inguinal swelling/mass/lump, LT inguinal scar. - diff?
- Inguinal scrotal mass - hernia - on foley’s catheter - place hand for cough - diff hydrocele, lipoma
- Midline scar, huge swelling irregular… Incisional hernia (cough test) - (strangulation of hernia - risk factor of repaired hernia) - diff of IBD, Cancer, Hernia, adhesive …
Groin Diff Diagnosis?

-
Lump RT Forearm around 4cm, regular, spherical, thrill, smooth, non tender, pulsatile, non compressible, diff… lipoma, subcutanous cyst, neurofibroma/
-
LT Infrascapular swelling on lumbar region, spherical 5x5cm, soft, normal overlying skin, no scar, cough (normal hernia), Diff.. Soft tisue sacrcoma? Hernia? lipoma?
-
Mass between RT thumb and index - rounded, 4x4cm, regular, reddish, dilated blood vessel, tender on palpitation diff. lipoma, neurofibroma, sacrcoma?
-
Punctum - Sebaceous cyst - Epidermal cyst - treatment excision

- Ulcer LT foot, medial malleolus, irregular, edema, pinkish, related tissue tendon, sloping (common in), base is muscle, varciosed venous, erythema. CVI (chronic venous insufficiency)
- two ulcer over head of metatarsal, callus thick skin, punched out, floor related to the tissue (neuropathy), Base … ,
- .
- .
- over heal necrotic tissue bed sore

- ..
- Healed ulcer,
- .
- .
- .
- .
- .
Other Presentations of Ulcer Z CC
Marjolin’s ulcer (scc) - chronic wound scar turning into Squamous cell carcinoma
Cushing Ulcer - Due brain injury? - prevent GI Ulcer given PPI
Curling Ulcer Burn victim - stress - vasoconstricion - ischemia -