 Allergic Contact Dermatitis (Henna dermatitis) Z
Allergic Contact Dermatitis (Henna dermatitis) Z
 very severe itchy Z
very severe itchy Z
 Eyelids Allergic Contact Dermatitis
Eyelids Allergic Contact Dermatitis
 Chronic Allergic Contact Eczema (Related to slippers)
Chronic Allergic Contact Eczema (Related to slippers)
 Contact dermatitis
This patient had a suture for his broken leg.
Contact dermatitis
This patient had a suture for his broken leg.
 Allergic contact dermatitis
Allergic contact dermatitis
 Allergic Contact dermatitis
Allergic Contact dermatitis
Contact Dermatitis CS-OSPE
Allergic Contact Dermatitis (ACD)
- Main Symptoms: Pruritus (itching) and redness are the main symptoms.
- Pathology: It is a delayed hypersensitivity reaction (type 4 immune reaction) which mediated by T cells and Langerhans cells (cell-mediated reaction). Even with long-time use, ACD can happen suddenly.
- Describe:
- Presents as eczematous, scaly edematous plaques with vesiculation distributed in areas of exposure, most of the times bilateral.
- The primary skin lesion in chronic contact dermatitis is a Plaque.
- Can be erythematous scaly bilateral plaques in palms.
- Ill-demarcated scaly plaques in dorsum of left foot (e.g., related to slippers).
- Possible Causes/Examples:
- Henna dermatitis: Girl made henna and developed itching.
- Ivy, Oak, Fragrance, Vitamin E.
- Slippers (leading to Chronic Allergic Contact Eczema).
- Reaction to suture for a broken leg.
- Recurrent itching erythema on hand and ear.
- How to diagnose / Investigation:
- Clinical: Full history and Examination.
- Specific Test: Patch test (positive result expected).
- Other investigations: Scrap and KOH (especially if fungal is a differential, e.g., with soil contamination). CBC, urine and stool analysis, thyroid function test.
- Differential Diagnosis: Irritant Contact Dermatitis (ICD), Eczema, Fungal infection.
- Management/Treatment (Tt):
Specific Clinical Examples:
- Eyelids Allergic Contact Dermatitis: Very itchy, bilateral erythematous scaly plaques in upper eyelids.
- Diaper Eczema: Type of contact dermatitis. Can’t be atopic because it will spare this area.
Irritant contact dermatitis (ICD).
- Main Symptoms: Pain and redness are the main symptoms.
- Pathology: Direct damage to the epidermis. Irritants affect people differently, and this effect depends on the strength of the material and the thickness of the skin.
- Describe: Erythema, chapped skin, dryness and fissuring after repeated exposures over time. Pain is a common symptom.
- Possible Causes: Mildly irritating substances (e.g., soaps, detergents) or strong substances (e.g., acids).
- How to diagnose / Investigation:
- Clinical: Full history and Examination.
- Specific Test: Patch Testing (negative result, used to exclude an allergic contact dermatitis).
- Other investigations: CBC, urine and stool analysis, thyroid test.
- Differential Diagnosis: Allergic Contact Dermatitis (ACD), Eczema.
- Management/Treatment:
- Avoidance: Identification and avoidance of the potential irritant.
- Topical Therapy: Topical therapy with steroids.
- Education: Educate the patient.
| ICD | ACD | |
|---|---|---|
| Common | ✓ | ✓ |
| Prev. Exposure | X | X |
| Duration | ~Days | ~1-3 weeks |
| Symptoms | Pain, Burning | X |

Diaper Contact Dermatitis
Type of contact dermatitis
- Can’t be atopic because it will spare this area


What is the most likely diagnosis?
- ACD; Allergic contact dermatitis
Case Description: A 35-year-old male from Bangladesh, working in building and ceramic works, complains of an itchy lesion.
A 46-year-old electrical technician man presented with chronic bilateral pruritic plaques on the dorsal feet (look to attached image) for 10 years throughout this period the condition waned and waved.
Clinical Findings: Bilateral lichinified plaques with fissures are observed in the dorsum of feet. (Note: The image in the exam was more clear and fissures were visible).
Differential Diagnosis:
- Allergic contact dermatitis
- Irritant contact dermatitis
- Contact dermatitis
- Psoriasis
Confirmation of Diagnosis (Patch Test): To confirm the diagnosis, a patch test is performed. Patches containing allergens are placed on the patient’s back for 2 days, then removed. Positive reactions show erythema and papules or vesicles.
Explain the underlying pathogenesis of the disease?
- It’s a type 4 HYPERSENSITIVITY reaction mediated by Langerhans cells that phagocyte the antigens and present it to the T-lymphocytes within regional lymphatic nodes.
Explain the above-mentioned test, how you will perform the test (procedure), mention the Important durations, interpretation of the possible test results?
- The test is performed by applying series of antigens on the back of the patient for 48 Hours, then the patient is appointed for a test reading after 96 - 120 hours from the first day.
- There are three possible results if the test is positive, which will be interpreted as follow:
- Erythema indicates a mild reaction
- Papules indicate moderate
- Vesicles indicate severe
Treatment:
- Avoidance of allergens
- Emollients
- Potent topical steroids

Patch Test
Interpretation is typically done after 4 days.
What is this?
- Patch test
- Skin allergic test
In which condition we use :
- Allergic contact dermatitis
Positive signs:
- Erythema
- Papule
- Vesicle
A patch test is a painless procedure to identify allergens.

 Irritant contact dermatitis Z
Irritant contact dermatitis Z


Irritant Contact Dermatitis
A 35 Y\O surgeon, complaining of itchy hands for the last months. The condition improves during vacations. Patch test was negative.
What is the diagnosis?
- Irritant contact dermatitis
What is the next appropriate step of the management to reach the diagnosis?
- Detailed history
How to confirm?
- Take history and physical examination.



Contact Dermatitis
Case Description: Itchy hand of a worker.
What is your diagnosis?
- Contact dermatitis.
Explain the underlying pathogenesis?
- First exposure: Antigen stimulates Langerhans cells, which then migrate to the lymph node and activate T-cells, leading to the production of antibodies and cytotoxic cells.
- Second exposure: The reaction will be faster due to prior sensitization.
What is the treatment?
- Avoid the trigger.
- Antihistamine.
- Topical steroid.
-
- Desonide Cream, - Topical Clobetasole 0.5% ointment
- Emollient.
Which cells are responsible for the pathogenesis of the disease?
- Langerhans cells


- Lesions begin as erythematous macules that become papules or plaque.
- Blisters often form over one to two days.
What is the diagnosis?
- Rhus allergic contact dermatitis.
Clinical Presentation
- Bullea.
- Cell distribution.
Pathology
- Exogenous eczema due to skin inflammatory condition created by reaction to an externally applied substance.
- Type IV: Cellular mediated hypersensitivity reaction.
Treatment
- admission.
- Systemic steroid: for short course may be required for acute flares and severe cases.
- Topical steroid of medium to strong potency:
- Fluocinonide 0.05% or
- Triamcinolone acetonide ointment, cream, lotion 0.1%
- Wet dressings are helpful when there is extensive oozing and crusting.
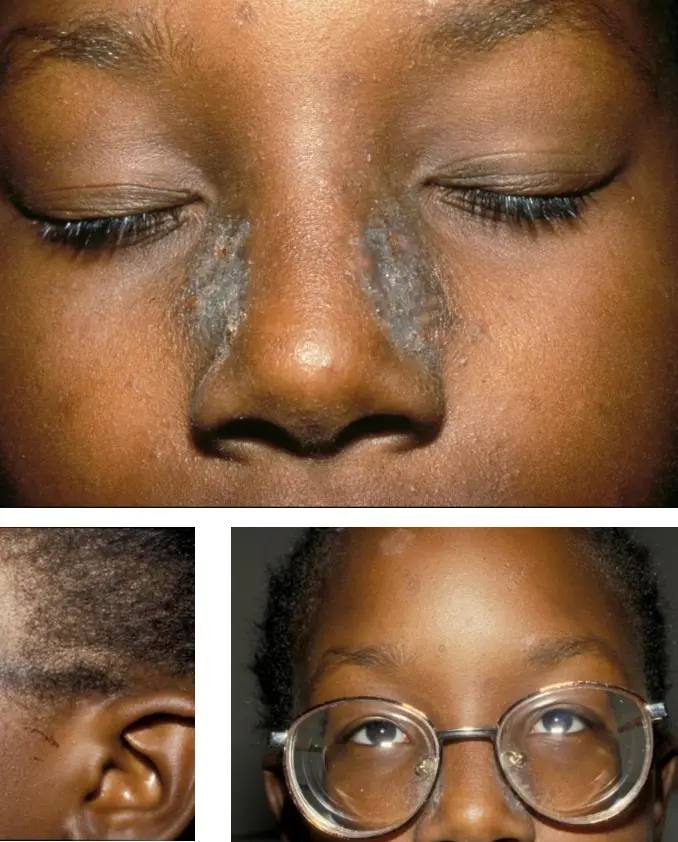
- This 11-year-old girl presents with 3 months of an itchy rash on the sides of her nose and ears.
Nickel Dermatitis/ Allergic Contact Dermatitis
Clinical Presentation:
- Pruritic
- Scale
- Plaques
Pathology:
- Exogenous eczema due to a skin inflammatory condition created by reaction to an externally applied substance.
- Type IV: Cellular mediated hypersensitivity reaction.
Treatment:
- Mild-Moderate case:
- Topical steroids of medium to strong potency for a limited course are successful.
- Fluocinonide 0.05% or
- Triamcinolone acetonide ointment, cream, lotion 0.1%
- Topical steroids of medium to strong potency for a limited course are successful.
- Soothing lotions can provide further relief in mild cases.