Surgery
Shock
Hypovolemic Shock
-
Most common type in surgical practice.
-
Reduction in intravascular volume.
- Blood loss: Trauma, GI bleeding, ruptured aneurysm
- Plasma loss: Burn
- Water & electrolytes loss: Diarrhoea, vomiting
-
Easily correctable.
Classes of haemorrhagic shock Based on estimated blood loss & patients’ initial presentation (ATLS)
| Class | Blood loss (ml) | Blood loss - % volume | Pulse / min | Systolic BP | Pulse pressure | Respiration rate | Urine (ml/hr.) | Mental status | Initial fluid |
|---|---|---|---|---|---|---|---|---|---|
| Class I | Up to 750 | Up to 15% | <100 | Normal | Normal/increased | 14-20 | >30 | Slightly anxious | Crystalloid |
| Class II | 750-1500 | 15-30% | 100-120 | Normal | Decreased | 20-30 | 0.5 to 1.5 cc/kg/hour | Mildly anxious | Crystalloid |
| Class III | 1500-2000 | 30-40% | 120-140 | Decreased | Decreased | 30-40 | 20-30 | Anxious, confused | Crystalloid & blood |
| Class IV | >2000 | >40% | >140 | Decreased | Decreased | >35 | 5-15 Negligible | Confused, lethargic | Crystalloid & blood |
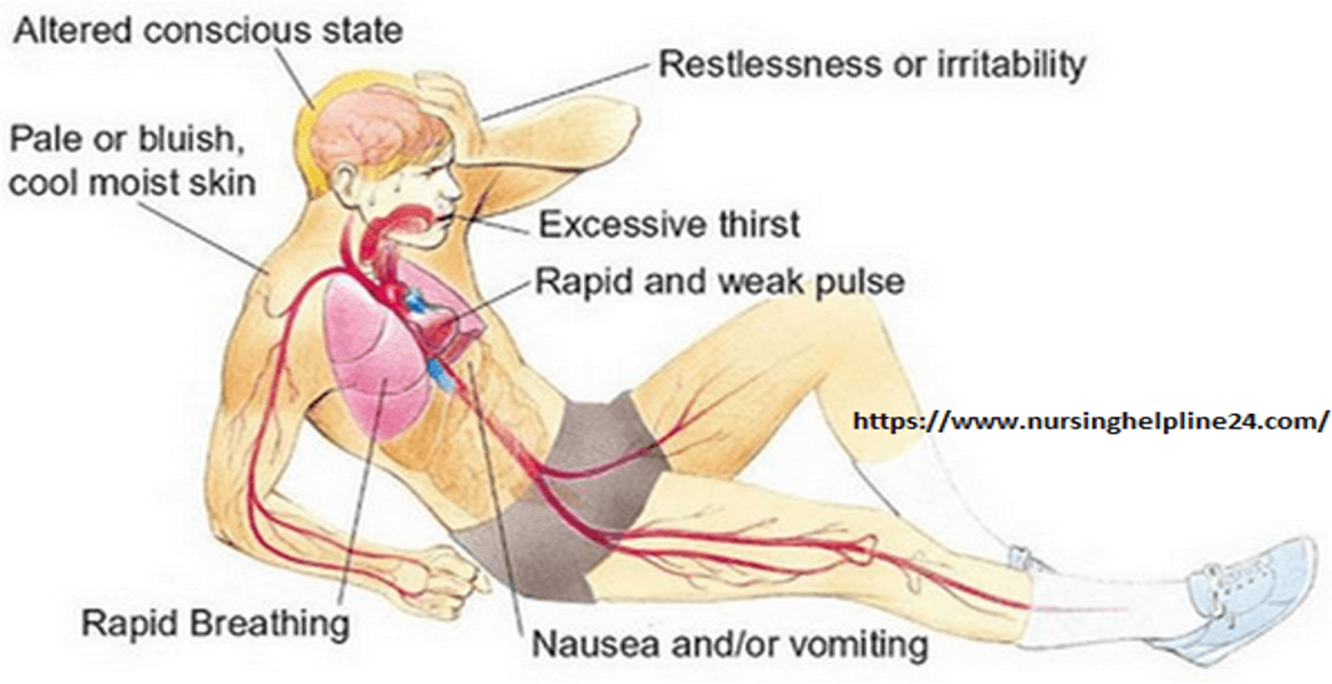
Signs and symptoms
- Anxiety, restlessness, altered mental state
- Distracted look in the eyes
- Thirst and dry mouth
- Cool, pale, clammy skin
- Hypothermia
- Rapid and shallow respirations
- Oliguria (Urine Output<30ml/hour)
- Hypotension
- A rapid, weak, thready pulse
Treatment:
Resuscitation
- a. To ensure clear airway, adequate breathing and circulation.
- b. Provision of 100 percent oxygen by a face mask. Deliver oxygen at a flow of 5-6 liters per minute
Hypovolemic shock
-
Position: The patient is kept in “head down position”.
-
Arrest external bleeding
-
Fluid resuscitation- Two wide bore (14-16 gauge) peripheral venous access.
-
PRBCs: Life threatening/ continued bleeding. Vasopressor & inotropes- little role
-
Invasive monitoring: CVP, PAWP, acid-base status, UOP
-
Fluid replacement—Crystalloid solution like Ringer lactate is ideal in situations where Na and H2O loss is predominant and will also serve as initial treatment in hemorrhagic shock.
-
Blood transfusion is advised in hemorrhagic shock and
-
Plasma transfusion in case of burns.
-
Colloids, e.g. Gelatin (Hemaccele), Hydroxyethyl starch (HES) and Dextran remain longer in the circulation and draw extracellular fluid (ECF) into the circulation by osmotic pressure.
Trauma
- Shock- secondary to hemorrhage in most trauma patients
- Patient can be in shock before developing hypotension
- Hypotension- a sign of decompensation (class III )
5 locations for major blood loss: - Chest - Abdomen - Pelvis and retroperitoneum - Multiple long bone fractures ( lower limb) - External hemorrhage
Pathophysiology of blood loss
Compensatory responses occur as: - Progressive vasoconstriction- skin pallor - Tachycardia to preserve cardiac output. - Increased peripheral resistance- catecholamines.
- Venous return- preserved in early stage, reduced later due to reduced blood volume in venous system.
- If Continued bleeding- shock develops.
- Inadequate tissue perfusion, metabolic acidosis.
Classes of hemorrhagic shock
| Class | Blood loss (ml) | Pulse | BP |
|---|---|---|---|
| Class I | Up to 750 | <100 | Normal |
| Class II | 750- 1500 | >100 | Normal |
| Class III | 1500- 2000 | >120 | Decreased |
| Class IV | > 2000 | >140 | Decreased |
Circulation Indicators of shock in trauma patients
- Tachycardia
- Agitation
- Tachypnea
- Sweating
- Cool extremities
- Weak peripheral pulse
- Decreased pulse pressure
- Hypotension
- Oliguria