Items of Pediatric History
-
Date of history.
-
Name of patient.
-
Informant: Mother, father, grandmother, school teacher, etc.
-
Reliability: Good, fair, poor.
-
History taken by: Your name and title.
-
Patient’s profile:
- Age (including date of birth)
- Sex
- Address (usually name of city, town, or village).
- Referred from…
- Significant medical conditions.
-
Chief complaints (Presenting Complaint):
- Who is concerned (patient, mother, school teacher…)?
- When did you notice that your child has changed?
- OR what is he complaining of?
- OR what do you think he is sick with?
- Use, when possible, patient’s or patient’s mother own words.
- Arrange complaints according to significance to child’s health.
- Onset / Course / Duration of each complaint.
- The main problem or complaints for which the child has been brought for medical attention: - Fever—5 days. - Vomiting—4 days. - Diarrhea. - Abdominal pain. - Cough. - Headache.
- History of present illness:
- Start with one of the following sentences:
- The patient was doing well until…
- The history of this child dates back to…
- The patient was in his usual state of health until…
- Analysis of symptoms respecting the chronological order of symptoms.
- Sequence of events.
- Other associated symptoms.
- Important negative symptoms related to the complaints.
- Start with one of the following sentences:
Items of Pediatric History
History of Present Illness
- Progress of disease; order and date of onset of new symptoms.
- Aggravating and alleviating factors.
- Significant medical attention and medications given and over what period.
- In acute infection, statement of type and degree of exposure and interval since exposure.
Outline of Specific Pediatric History Items
A. Antenatal
B. Perinatal
C. Neonatal
D. Growth, development, and behavior.
E. Nutrition
F. Past illnesses
G. Immunizations
H. Allergies and test reactions.
I. Accidents and injuries.
Antenatal
Antenatal care: booked/un-booked? Where? Frequency of visits.
- Prenatal exposure to illicit drugs, toxins, or infections; maternal diabetes; acute maternal illness; trauma; radiation exposure and fetal movements. (The prenatal period refers to the period of time from fertilization to birth.)
- Medications during pregnancy (timing/dose/duration).
- Maternal thyroid or seizure disorder.
- Polyhydramnios/Oligohydramnios.
- Maternal severe proteinuria or high blood pressure.
- Bleeding in the third trimester.
- Multiple gestation.
- Chorioamnionitis.
Perinatal History
Perinatal period: 22 completed weeks of gestation and ends 7 completed days after birth.
- Place of delivery.
- Presentation of the child (e.g., breech or face presentation).
- Mode of delivery: NSVD, assisted vaginal, C/S. Obstetrical complications.
- Gestational age.
- Birth weight and other birth measurements (Lt, HC).
- Resuscitation.
- Apgar Score or condition at birth in mother’s words.
- Maternal risk factors for sepsis (PROM, maternal UTI, maternal fever…).
- Baby & mother’s blood groups.
Neonatal
- When did the baby pass urine/meconium?
- Respiratory distress, anemia, jaundice, cyanosis, convulsions, infection, congenital anomalies.
- If he/she was admitted to the hospital:
- Length of hospital stay.
- Complications (e.g., intubation time, presence of intracranial hemorrhage ultrasonogram, feeding difficulties, apnea, bradycardia).
- If he/she was admitted to the hospital:
Developmental History
-
Growth is the increase in the size of the organ.
-
Development is the increase in the function of the organ.
-
Ask about physical growth (Wt., Ht, HC) especially if records are available.
-
Developmental milestones: - Gross Motor - Fine Motor - Social/Adaptive - Language/Speech
-
Age at attainment of important milestones (walking, talking, self-care).
-
Relationships with siblings, peers, adults.
-
School grade and performance.
-
Behavioral problems (Sleep disturbance, phobias, Pica, Abnormal bowel habits, stool holding, Bed wetting, and Unusual behavior).
Nutrition
- Breastfeeding or milk formula.
- Type and amount of semi-solid/solid foods, & when added.
- Any vitamin or iron supplementation.
- Difficulty encountered during feeding, e.g., NGT feeding.
- Any known food allergy.
- Type of diet.
- Change in feeding habits.
Past Medical History
- Infections: age, types, number, severity.
- Contagious diseases: age, complications.
- Past hospitalizations, operations age.
- Allergies: to drugs or food, type of reaction.
- Medications patient is currently taking (Names, dosages).
- Accidents and injuries.
Immunizations
- Place of vaccination.
- What schedule.
- Additional vaccines.
- Always ask for vaccination card (Up-to-date?!).
- Any vaccine side effects.
It is important to record the details of vaccines given to the child in chronological order.
Family History
- A. Father and mother (age and health)
- B. Marital relationship/consanguinity pattern
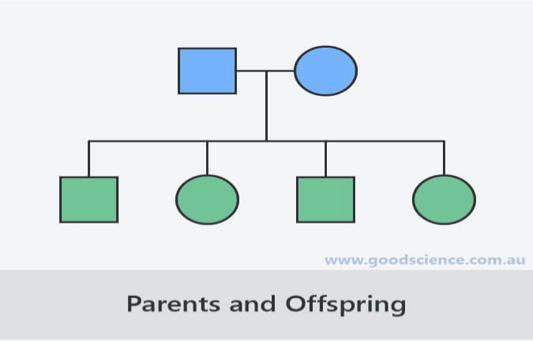
- C. Siblings: Age, health, significant illnesses (The pedigree chart).
- D. Birth of abnormal children (e.g., LBW, IUGR, Dysmorphic, with a motor deficit, mental retardation, or Congenital malformations).
- E. Stillbirth, miscarriages, age of death, and cause of death.
- F. TB, allergy, blood disorders, mental or CNS disorders, diabetes, cardiovascular, kidney disorders, etc.
- G. Health of contacts.
Social History
- Address, home condition (sunny, ventilation, rooms…).
- Health insurance.
- Parental education & occupation.
- Family income & socioeconomic status and allowances.
- Smoking at home, alcohol, and drugs.
- Who is taking care of the child in the home?
- Impact of the disease on the child, siblings, father, and mother.
- Safety: Child car seats, smoke detectors, bicycle helmets.
Adolescent History
[HEADS history]
- Home
- Education
- Activities
- Drugs
- Sexual activity.
Review of Systems
-
General:
- Overall health.
- Weight loss.
- Behavioral changes.
- Fever.
- Fatigue.
-
Skin:
- Rashes/bruising.
- Lumps/bumps.
- Nail/hair changes.
-
Eyes:
- Visual problems.
- Eye pain.
-
Ear, Nose, Throat:
- Frequency of colds.
- Sore throat.
- Earache.
-
Lungs:
- Cough.
- Shortness of breath.
- Wheezing.
-
Cardiovascular:
- Chest pain/Palpitation.
- Exercise intolerance.
- Syncope.
-
Gastrointestinal:
- Nausea/vomiting.
- Spitting up.
- Diarrhea.
- Recurrent abdominal pain.
- Constipation.
- Blood in stools.
-
Genitourinary:
- Dysuria.
- Hematuria.
- Polyuria.
- Vaginal discharge.
-
Musculoskeletal:
- Weakness.
- Joint pain.
- Gait abnormalities.
- Scoliosis.
-
Neurological:
- Headache.
- Seizures.
-
Endocrine:
- Growth delay.
- Polyphagia (Extreme, insatiable hunger).
- Polydipsia (Excessive thirst/fluid intake).
- Menses duration/Amount of flow.
Pediatric History Compared to Adult History
I. Content Differences: A. Prenatal and birth history. B. Developmental history. C. Social history of family – environmental risks. D. Immunization history.
II. Parent as Historian A. Parent’s interpretation of signs, symptoms. 1. Children above the age of 4 may be able to provide some of their own history. 2. Reliability of parent’s observations varies. 3. Adjust wording of questions varies (pain vs. limping).
B. Observation of parent-child interactions. 1. Distraction to parents may interfere with history taking. 2. Quality of relationship. C. Parental behaviors/emotions are important. 1. Parental guilt – nonjudgmental/reassurance. 2. The irate parent; causes.