CLO’s
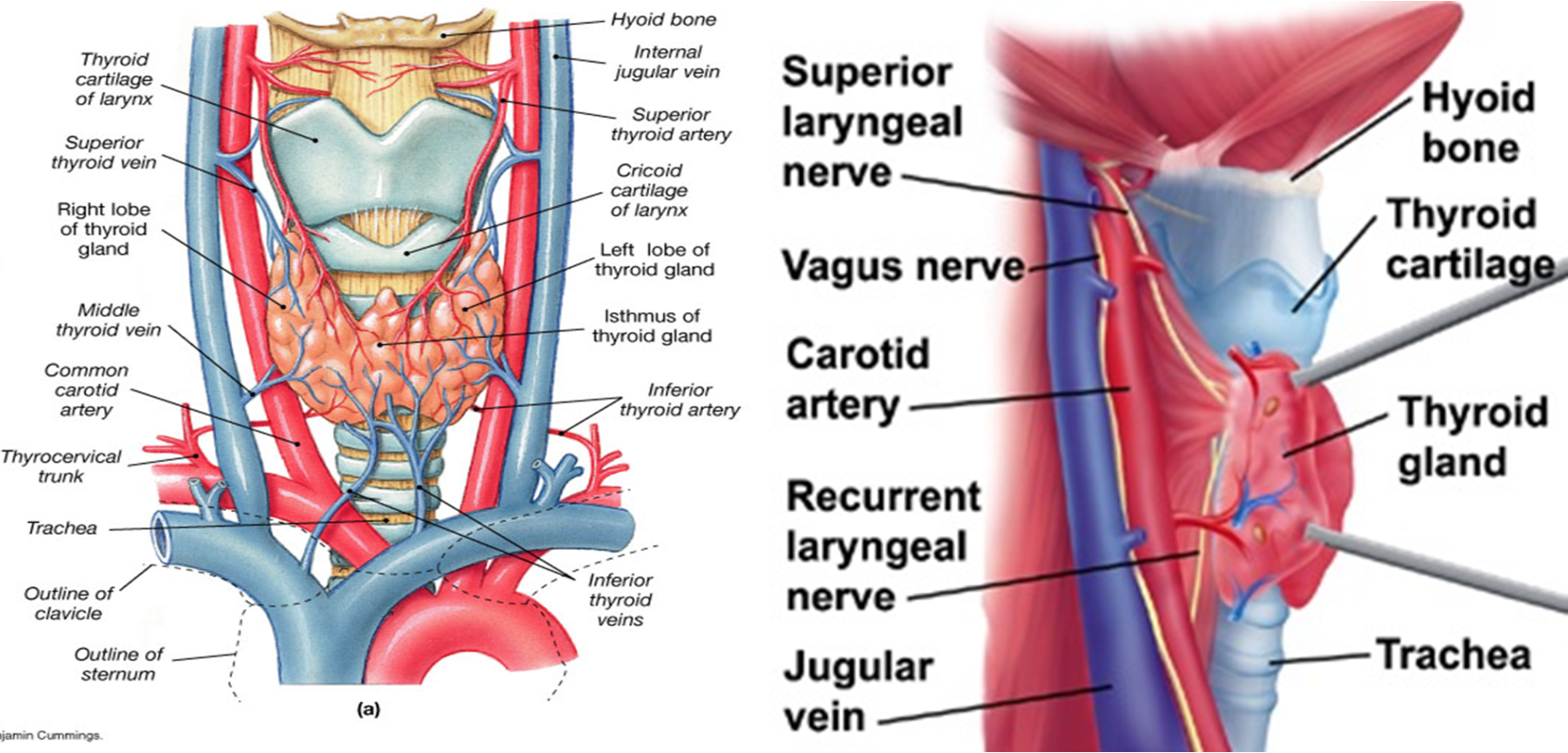
- Surgical anatomy, development & physiology
- Thyroid diseases- classification, aetiology, clinical presentations, investigations & treatment
- Complications of thyroid surgery
Classification- thyroid diseases
-
Congenital: Thyroglossal cyst, Lingual thyroid
-
Simple:
-
Non-toxic goitre,
-
MNG,
-
Solitary Thyroid Nodule (STN),
-
-
Functional disorders:
- Hypothyroidism
- Hyperthyroidism: Grave’s disease, Toxic adenoma, Toxic goiter (Toxic MNG), Thyrotoxicosis factitia
-
Thyroiditis:
-
- Benign: Follicular adenoma
- Malignant: Papillary, Follicular, MTC, Anaplastic, Lymphoma, Metastatic
Assessment of Thyroid Diseases
- FT4, T3,TSH (TSH low in hyper, high in hypo) TRH (hypothalamus)
- Serum Calcitonin (MTC)
- Antibodies: TSI-thyroid stimulating immunoglobulin, Anti-thyroglobulin antibody, anti-TPO- thyroid peroxidase
- Ultrasound
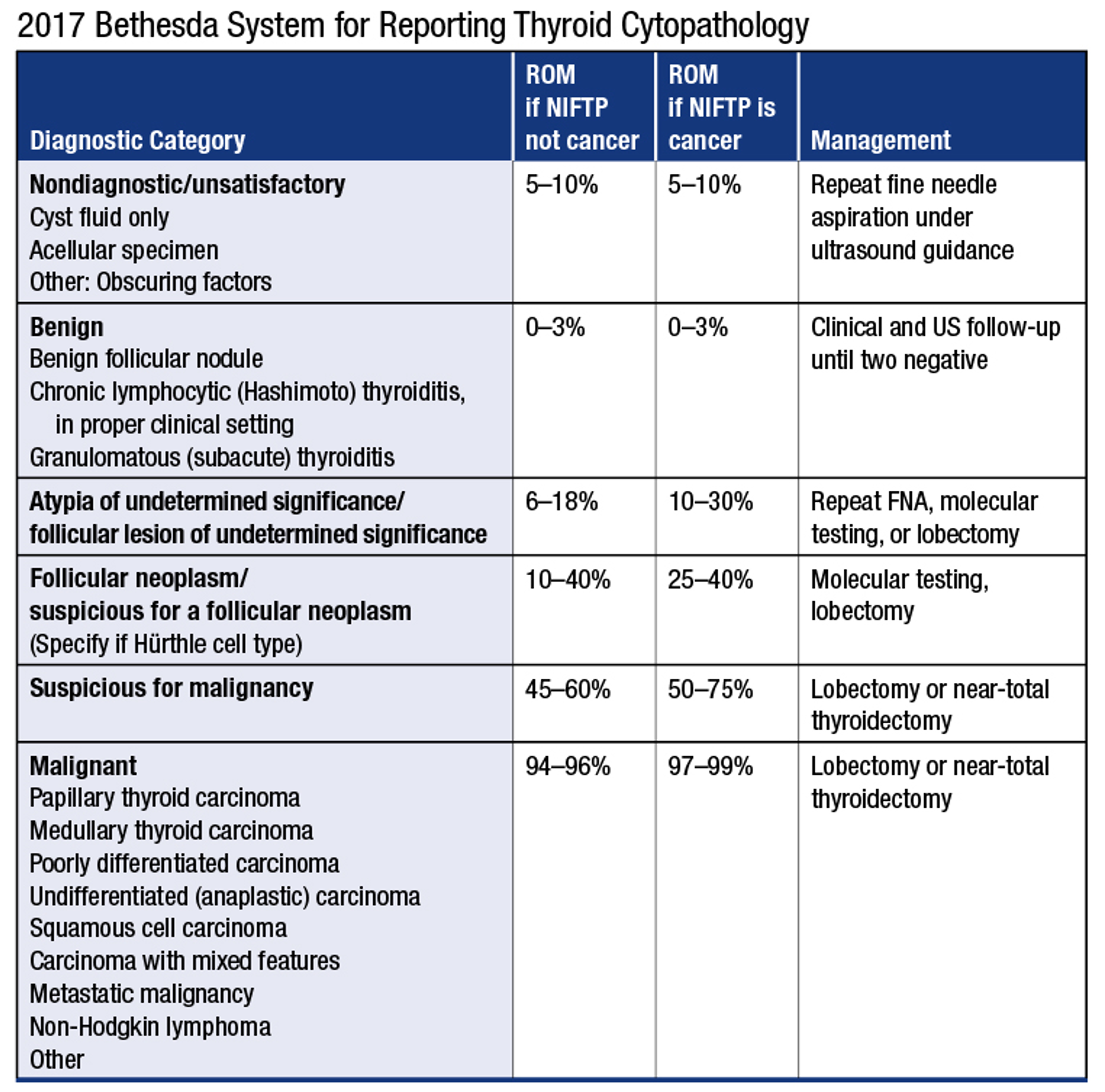
- FNA: accurate, palpation/US guided- non-diagnostic /benign/ undetermined / follicular neo./ suspicion of malignancy/ malignant- Bethesda system
- Radioisotope scanning (Tc99-Sodium pertechnetate)- toxic goitres
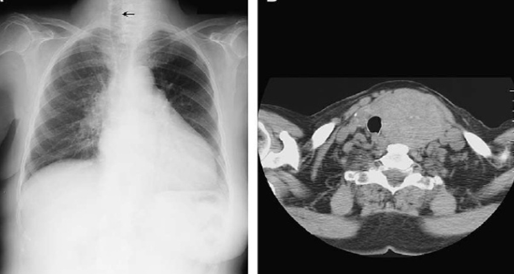
- CXR, CT, MRI ( retrosternal mass, staging malignancy, local invasion)
- PET scan
- Laryngoscopy- vocal cord assessment
OSPEZ
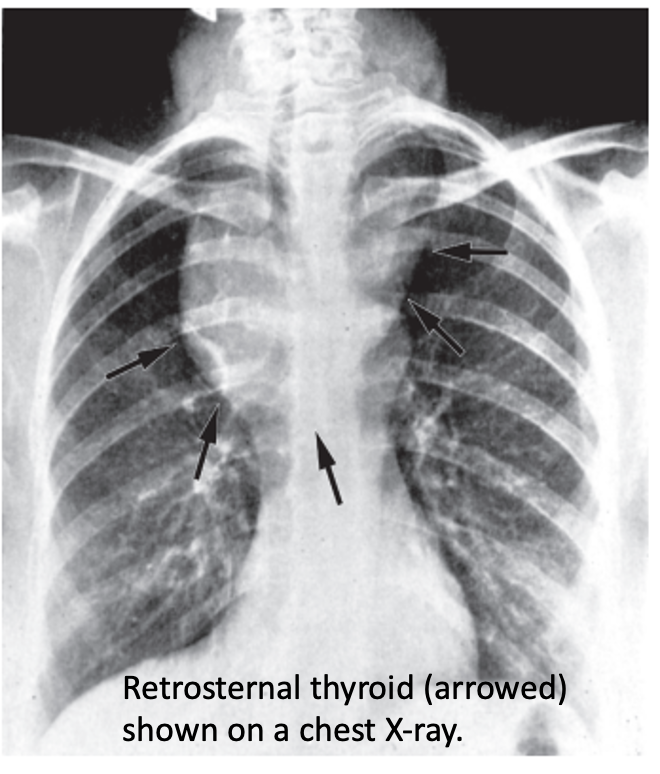
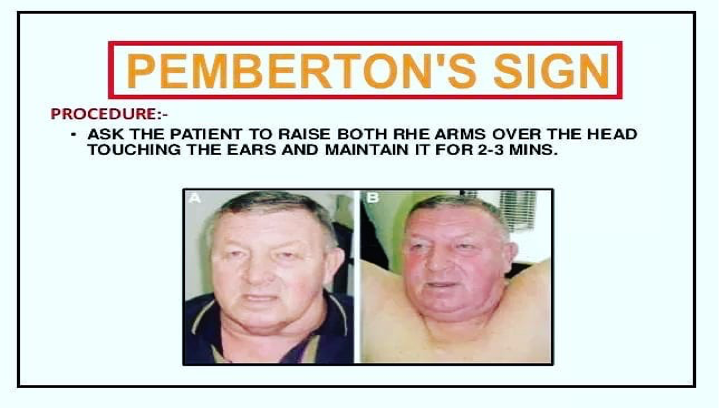 Pemberton’s sign is used to evaluate venous obstruction in patients with goiters. The sign is positive when bilateral arm elevation causes facial plethora. It has been attributed to a “cork effect” resulting from the thyroid obstructing the thoracic inlet, thereby increasing pressure on the venous system.
Pemberton’s sign is used to evaluate venous obstruction in patients with goiters. The sign is positive when bilateral arm elevation causes facial plethora. It has been attributed to a “cork effect” resulting from the thyroid obstructing the thoracic inlet, thereby increasing pressure on the venous system.
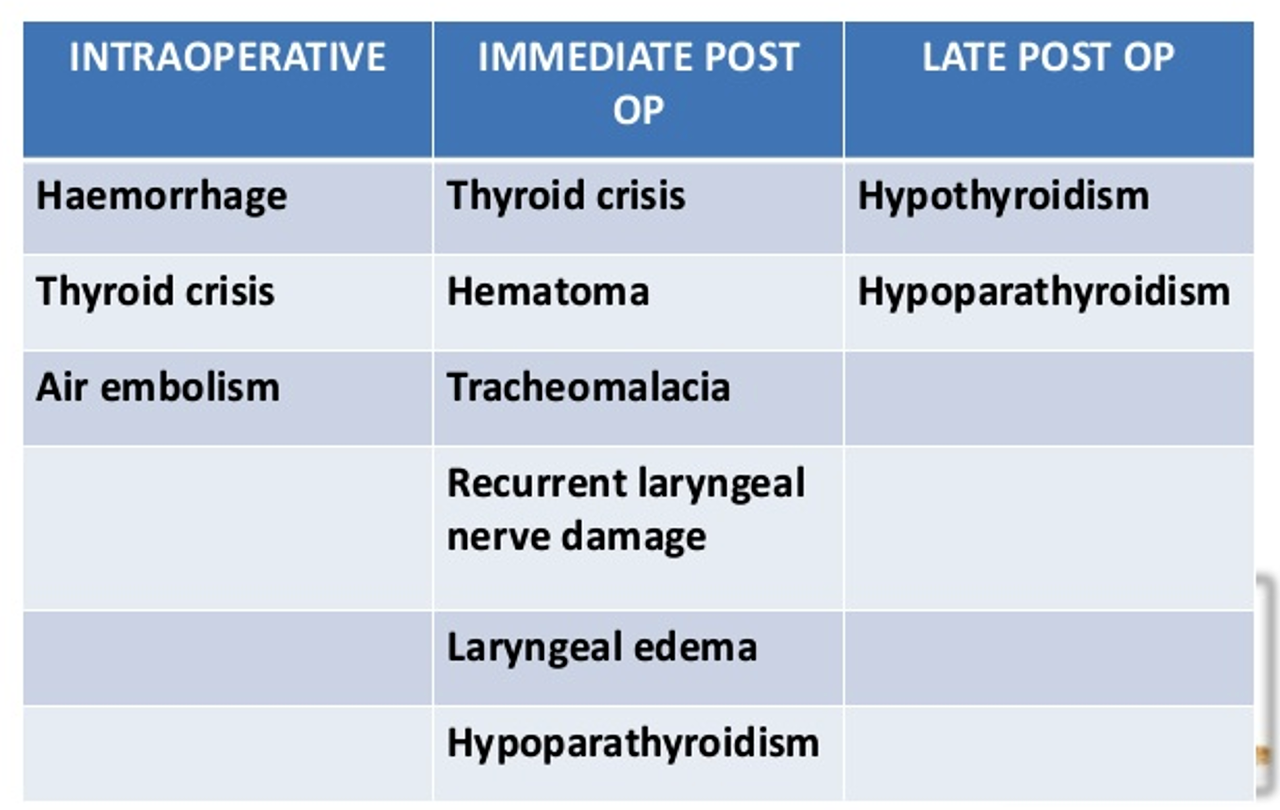
POST OP Complications of Thyroid Surgery
-
Tension Haematoma (1%): Usually within 6 hours of surgery. Management: immediate opening of the incision, airway control & return to OR- wound irrigation & control of bleeding
-
Recurrent laryngeal nerve injury (RLN): 1%
- Transient recovers in 1-6 weeks.
- Unilateral- hoarseness of voice.
- Bilateral- compromises airway, may need tracheostomy.
- The nerve provides the motor supply to the vocal cords (all intrinsic muscles of the larynx except cricothyroid) and sensory supply to the mucous membrane of the larynx inferior to the vocal folds.
-
The external branch of superior laryngeal nerve leading to a subtle disturbance in voice and in particular singing
-
Develops typically 24-72 hrs post operatively, but may manifest as early as as 1-3 hrs after surgery.
-
Laryngeal muscles are sensitive to hypocalcemia and inspiratory stridor progressing to laryngospasm, may be the first indication.
-
Circumoral tingling/ numbness , Chvostek’s/ Trousseau’s sign
-
Transient- Ca-carbonate 1 g x tds oral.
-
Severe: 10% Ca gluconate infusion. Permanent: parathyroid tissue auto transplant
Both completely = Aphonia Both Partial = Asphyxiation
Sup laryngeal n. voice become weak
-
Hypocalcaemia - Hypoparathyroidism
- Thyroid A.
- removed parathyroid
-
Tracheomalacia: tracheomalacia - longstanding chronic multinodular goiter - resulting in weak trachea after removal collapse of trachea = asphyxiation
-
It occurs after removal of long standing goiter, especially the thoracic inlet, that has compressed and weakened cartilaginous rings supporting the tracheal wall.
-
Immediate intubation or tracheostomy should be performed.
-
Later options include stenting, extrinsic tracheal support, tracheoplasty.