OBYGN-SKIM-MID
Female Anatomy
The Bladder
- The bladder wall is made of involuntary muscle.
- It is lined with transitional epithelium.
- Has an average capacity of 400 ml.
- The ureters open into the base of the bladder.
- The urethra leaves the bladder below the ureteric orifices.
- The base of the bladder is adjacent to the cervix & separated from the anterior vaginal wall by the pubocervical fascia.


The Urethra
- The female urethra is 3.5 cm long.
- and lined with transitional epithelium.
- The lower part occasionally become infected.
- The upper part of the urethra is mobile but the lower part is fixed.


The Ureter
- As the ureter crosses the pelvic brim
- it lies in front of the bifurcation of
- the common iliac artery.
- The ureter runs close to the lateral vaginal fornix to enter the bladder.
- Blood supply from the ovarian artery.
- Due to its close relationship to the cervix
- the vagina and the uterine artery.
- The ureter passes inferior to the uterine artery (“water under the bridge”) and is lateral to the cervix, making it susceptible to damage during hysterectomy (cut or tied). Ligation of the uterine artery is a common step in hysterectomy, and the ureter is at risk. If the ureter is injured, a stent may be placed to allow it to heal.

The Rectum
- The rectum extends from the level of the third sacral vertebra to the anal canal.
- The front and sides are covered by the peritoneum of the rectovaginal pouch.
- The middle third only the front is covered by peritoneum.
- Rectum is separated from the posterior wall of the vagina by the rectovaginal fascial.
- Lateral to the rectum, the uterosacral ligaments.



The Bony Pelvis
The bony pelvis provides support and protection for pelvic organs. Its function can be affected by metabolic diseases such as rickets.
The Pelvic Muscles, Ligaments and Fascia
The Pelvic Diaphragm
- The pelvic diaphragm is formed by the levator ani muscles, which are broad, flat muscles the fibres.
- The two muscles, one on either side, constitute the pelvic diaphragm.
- The muscles arise from:
- The body of the pubis.
- The pelvic fascia.
- The ischial spine.
- The levator ani muscle inserted into:
- The preanal raphe.
- The anal canal.
- The anococcygeal raphe.
- The coccyx.

Parts of Levator Ani Muscle
The muscle is described in two parts:
- The pubococcygeus.
- The iliococcygeus.
They have some sphincteric action. The nerve supply is from the third and fourth sacral nerves. The pubococcygeus muscles support: - the pelvic - abdominal viscera (including the bladder). Together with the fibres from the opposite muscle they form a loop that maintains the angle between the posterior aspect of the urethra and the bladder base. During micturition, this loop relaxes to allow the bladder neck and upper urethra to open and descend.


Urogenital Diaphragm
- Is made up of two layers of pelvic fascia.
- The deep transverse perineal muscles (compressor urethrae) lie between the two layers and the diaphragm is pierced by the urethra and vagina.
- The perineal body This is (a mass of muscular tissue) that lies between the anal canal and the lower third of the vagina.
- Its apex is where the rectum and posterior vaginal walls come into contact.

The Pelvic Peritoneum
The Broad Ligament
- peritoneum double reflection from the lateral borders of the uterus on either sides.
- Its not a ligament but a peritoneal fold and it does not support the uterus.
- The Fallopian tube runs in the upper free edge of the broad ligament.
- The lateral portion is called the ‘infundibulopelvic fold’ “suspensory” where ovarian vessels and lymphatics.


The Mesosalpinx
- the portion of the broad ligament that lies above the ovary.
The Mesovarium
- is a short mesentery that attached the ovary to the posterior layer of the broad ligament through which the ovarian vessels lies.
The Ovarian Ligament
- passes from the medial portion of the ovary to the uterus.
The Round Ligament
- continuation enter the inguinal canal, to end in the the labium major.

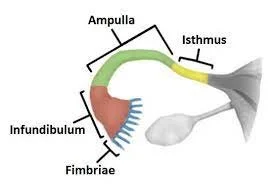
Parts of the Fallopian Tube
- Each tube is about 10 cm long and described in four parts. They are lined with ciliated epithelium:
- The interstitial portion (lies within the wall of the uterus).
- The isthmus (a narrow portion adjoining the uterus).
- The ampulla (the widest and longest portion).
- The infundibulum or fimbrial portion (where ampulla terminates).
Cervix Size & Uterus Direction
The cervix is approximately 2.5 cm in length. The uterus typically exhibits an ‘anteversion’ position, where its longitudinal axis is at right angles to the vagina and tilts forward. It also usually shows ‘anteflexion’, meaning it is flexed forward on itself at the isthmus. In some cases, the uterus may be tilted backwards (retroversion and retroflexion), which generally has no pathological significance unless fixed.
Vagina & Relationships
The vagina has no glands but is kept moist by uterine secretions, cervical gland secretions, and transudation from its epithelial lining. Physiological vaginal discharge may increase pre and post ovulation. Doderlein’s bacillus plays a protective role by breaking down glycogen to form lactic acid (maintaining a pH of ~4.5). Inflammation of the vagina is called vaginitis. Common causes include bacterial vaginosis, often characterized by the presence of clue cells on microscopy and caused by organisms like Gardnerella vaginalis. In diabetic women and children, vulvovaginitis is frequently caused by Candida species (fungal infection). The vagina has comprehensive relationships:
- posteriorly (pouch of Douglas, rectum, perineal body),
- anteriorly (bladder, urethra), and
- laterally (cardinal ligaments, levator ani muscles, ischiorectal fossae).
Vulva Components
The vulva comprises 8 components: Mons pubis, Labia majora (sebaceous and sweat glands and specialized apocrine glands.) , Labia minora (sebaceous glands but have no adipose tissue), Vaginal vestibule, Clitoris, Greater vestibular glands (Bartholin’s Glands), Hymen, and Vaginal opening.
Uterine Support
- ➤ The cardinal ligaments (transverse cervical ligaments)
- ➤ The uterosacral ligaments run from the cervix and vagina to the sacrum.
- ➤ Round ligament
- The bladder is supported by:
- ✓ pelvic fascia.
- ✓ pubocervical fascia.

The Blood Supply
The Ovarian Arteries
- supply the ovary and tube
- they anastomose with the terminal
- branches of the uterine artery.
The Internal Iliac (Hypogastric) Artery Branches
- supply the pelvic organs by the following branches:
- The uterine artery …supply to the uterus.
- The vaginal artery …supply the vagina.
- The vesical arteries … supply the bladder and terminal ureter.
- The pudendal artery… supplying the vestibular bulbs and clitoris.
- The superior rectal artery …supply the rectum.

The Pelvic Veins
- ✓ Around the bladder
- ✓ Uterus
- ✓ vagina
- ✓ rectum form… plexuses that drain into the internal iliac veins.
- ✓ The ovarian veins on each side begin in the pampiniform plexus in the broad ligament ending in the inferior vena cava.

Lymphatics
- The pelvic lymphatics draining:
- inguinal nodes.
- superficial femoral nodes.
- Pelvic nodes.
- para aortic nodes.

The Nerves
Nerve Supply (Somatic)
- The pudendal nerve.
- The perineal nerve.
- sacral nerves.
Autonomic Nerve Supply
- of the pelvic viscera:
- the preaortic plexus
- superior hypogastric plexus


Estimated Date of Delivery (EDD) from Last Menstrual Period (LMP)
The EDD is an estimation of the due date, most commonly calculated using Naegele’s Rule.
-
Naegele’s Rule Formula: LMP + 1 year + 7 days - 3 months.
-
Example:
- LMP: 4/9/2024
- EDD: 16/1/2025
-
Clinical Accuracy :
- It is an Estimate: Naegele’s Rule assumes a regular 28-day menstrual cycle with ovulation on day 14. This is not accurate for all women.
- Ultrasound is Gold Standard: A first-trimester ultrasound (before 14 weeks) is the most accurate method for dating a pregnancy and establishing the EDD. If there is a significant discrepancy between the LMP-based date and the ultrasound date, the ultrasound date is preferred.
- “Due Window”: Only a small percentage of babies are born on their exact EDD. It is more accurate to think of it as the midpoint of a “due window” (typically from 38 to 42 weeks).
Gestational Age (GA)
GA is the age of the pregnancy, calculated from the first day of the LMP and expressed in completed weeks and days.
-
How to Calculate: Count the number of completed weeks from the first day of the LMP to the current date.
-
Example: If LMP was 4/9/2024 and today’s date is 18/9/2024, the GA is 2 weeks and 0 days.
-
Clinical Accuracy: The accuracy of a GA calculation based on LMP is entirely dependent on the accuracy of the LMP itself. As with the EDD, a first-trimester ultrasound provides a more reliable determination of gestational age.
Gravida and Parity (G/P) & TPAL System
This system provides a shorthand summary of a woman’s obstetric history.
-
Gravida (G): The total number of times a woman has been pregnant, regardless of the outcome (includes current pregnancy).
-
Parity (P): The number of pregnancies carried to a viable gestational age.
- The threshold for “viability” can vary by institution (often 20 or 24 weeks). For maximum clarity, the TPAL system is preferred over a simple Parity count.
-
TPAL System: A detailed breakdown of parity.
-
T (Term): Number of term births (≥ 37 weeks).
-
P (Preterm): Number of preterm births (between 20-36 weeks).
-
A (Abortions): Number of pregnancies lost before 20 weeks (includes miscarriages and induced abortions).
-
L (Living): Number of living children.
-
A multiple birth (twins, triplets, etc.) counts as one gravidity and one parity event, but the number of living children (L) will reflect the number of babies.
-
History: A woman is currently pregnant. She previously had one miscarriage at 12 weeks and delivered twins at 38 weeks who are both living.
-
Accurate Notation: G3 T1 P0 A1 L2
-
Breakdown:
- G3: 3 total pregnancies (current pregnancy + twin pregnancy + miscarriage).
- T1: 1 term birth event (the twins delivered at 38 weeks).
- P0: 0 preterm births.
- A1: 1 miscarriage (at 12 weeks).
- L2: 2 living children (the twins).
-
Example
G 5 P 4 Means She is pregnant for 5 times : one is current pregnancy so she delivered 4 times .
G 5 P3 + 1 Means she is pregnant for 5 times : One is current pregnancy & she delivered 3 times & has one loss.
losses means: miscarriages , ectopic pregnancy & molar pregnancy (mention them in details).
Ex: A woman who has had six miscarriages with only one live baby born at 32 weeks and is pregnant again will be: gravida 8, para 1. (para 1+6.)(G viii P i+ iv)
OR to say ‘Mrs Wafaa is in her eighth pregnancy. She has had six miscarriages at gestations of 8–12 weeks and one spontaneous delivery of a live baby boy at 32 weeks. Baby Ahmed is now 2 years old and healthy.
-
Stillbirth: Stillbirth as ‘a baby delivered with no signs of life after 24 weeks of pregnancy’.
-
Intrauterine Fetal Death (IUFD): Babies with no signs of life in uter
INTRAUTERINE GROWTH RESTRICTION (IUGR): Infant with birth weight below the 10th percentile for a given gestational age.
- Intrauterine Fetal Death (IUFD): Babies with no signs of life in utero. The most accurate method for diagnosis is the absence of fetal heart activity by real-time ultrasound.
Amniotic Fluid
- Oligohydramnios: Reduced amniotic fluid volume. Can be seen in conditions like renal agenesis. A reversible complication that can be seen when indomethacin is used for tocolysis longer than 24 to 48 hours.
- Polyhydramnios: Excess amniotic fluid volume. Can be associated with conditions like cleft palate.
- Production: Amniotic fluid is mainly produced by the fetus.
- Intramembranous: This term, when applied to amniotic fluid, typically refers to the exchange of fluid across the fetal membranes (amnion and chorion), contributing to amniotic fluid volume regulation.
Third Trimester Bleeding
- Abruptio Placentae: Premature separation of the placenta from the uterine wall.
- Risk Factors: The most important risk factor is a previous abruption. Other factors include hypertension, trauma, and smoking.
- Couvelaire Uterus: In severe cases of abruptio placentae, extensive bleeding into the myometrium and beneath the uterine serosa can occur, leading to a bruised, purplish uterus known as a Couvelaire uterus.
Pregnancy
PPROM (Preterm premature rupture of membranes) is ROM prior to 37 weeks.
Embryology

Development of the Reproductive System
Development of the reproductive system begins with:
- Formation of undifferentiated gonads.
- and mesonephric and paramesonephric ducts.
- Further differentiation of the gonads:
- In male
- SRY gene on the Y chromosome ➡️ testes.
- Testosterone (by Leydig cells) ➡️ differentiation of the mesonephric ducts into male internal sex organs.
- Dihydrotestosterone ➡️ differentiation of male external genitalia.
- MIF (by Sertoli cells) ➡️ suppresses paramesonephric differentiation.
- In male

The male and female reproductive tracts are derived from the same embryonic/fetal tissue.
The gonads develop from three sources:
- Mesothelium (coelomic epithelium) lining the posterior abdominal wall
- Mesenchyme (intermediate mesoderm)
- Primordial germ cells

Up to the 7th week the internal genital organs in both sexes on both sides consist of two canal systems.
- The indifferent gonads consist of medulla and cortex.
- In XX: Ovary will originate from the cortex, and medulla will regress.
- In XY: Testes will develop from medulla and the cortex regress.
Cortex is the outermost.
Medulla is the innermost.


Primordial Germ Cells (PGC)
- Migrate from the allantois to the endoderm of the yolk sac.
- Then reach the genital ridge where they settle and lose their mobility.

Female Gonads
- By 12th week
- The ovary develops more slowly than the testes.
- The somatic cell will develop into follicle cells in the absence of SRY gene. As there are no Sertoli cells, there is no AMH.
- Stromal cells will surround the PGCs.
- The germ cells go on to differentiate into oogonia, proliferate, and enter the first meiotic division to form primary oocytes.
The maximum number of primordial follicles is reached at 20 weeks’ gestation when there are six to seven million primordial follicles present.
- The numbers of these reduce by atresia; they are 1-2 million at birth and 400,000 at puberty.

The fusion of the Mullerian ducts forms:
- the uterovaginal canal that gives rise to the
- ✓ Uterus
- ✓ Cervix.
- ✓ upper two thirds of the vagina.
- The lower third of the vagina urogenital sinus.
- The embryological origin of the hymen is controversial.
- The unfused, cranial portions of the paramesonephric ducts become the Fallopian tubes.
Many anomalies related to development of the uterus and vagina are attributable to abnormal fusion or regression of the caudal portion of the paramesonephric duct.

Overview of Sexual Differentiation
- Weeks 1–6: No sexual differentiation is apparent (no phenotypical differences).
- Week 6–7: Differentiation of the mesonephric and paramesonephric ducts begins.
- Week 12: Development of the external genitalia is complete.
- Week 20: Phenotypic differentiation is complete.
- Week 33: Descent of the gonads is complete.
Sexual Differentiation Pathways
Male: testosterone → dihydrotestosterone (via 5α-reductase) → differentiation of embryonic structures into male external genitalia.
Female:
estradiol and absence of DHT → differentiation of embryonic structures into female external genitalia (e.g., labioscrotal folds form the labia majora).

Fetal Skull Diameters
| Attitude | Well flexed | Less well flexed (partially extended) or deflexed | Extended ‘brow presentation’ | Hyperextended ‘face presentation’ |
|---|---|---|---|---|
| Diameter | Suboccipito-bregmatic | Occipito-frontal | Occipito-mental | Submento-bregmatic |
| Measurement | 9.5 cm | 11.5 cm | 13.0 cm | 9.5 cm Full extension |

-
Note on Longest Diameter: The Submentovertical diameter (11.5 cm) is considered the longest diameter of the fetal skull. The Occipito-mental diameter (13.0 cm) is also significant depending on presentation.
-
The fetal skull bones are connected by four main membranous sutures.
-
Suboccipito-bregmatic diameter (occipito-anterior position):
- The diameter is from the suboccipital region to the centre of the bregma.
- Diameter = 9.5 cm. Head well flexed.
-
Submento-bregmatic diameter:
- From the centre of the bregma to the angle of the mandible.
- Measuring 9.5 cm. This is the presenting diameter when the neck is hyperextended.
Fetal Presentation
- That part of the fetus entering the pelvis first. Types of presentation:
- Vertex (96.8%)
- Breech (2.5%) - (c/s or ECV, if fully dilated normal delivery)
- Face (0.2%)
- Shoulder (0.4%)
- Compound
- Brow (0.1%)
any presentation other than Vertex is grounds for C/S

Fetal Position
- Orientation of the presenting part in relation to the maternal public symphysis.
Types of position:
- Occipito-anterior (RT & LT).
- Occipitolateral (RT & LT).
- Occipito-posterior (RT & LT). in android pelvis - can be delivered vaginally but long labor and pain - w/ forceps and ventuse, and or C/S

**
Uterine Anomalies

- Normal Uterus
- Class I: Uterine Hypoplasia and/or Agenesis
- Class II: Unicornuate Uterus
- Class III: Uterus Didelphys
- Class IV: Bicornuate Uterus
- Class V: Septate Uterus
- Class VI: Arcuate Uterus
- Class VII: Diethylstilbestrol (DES) Drug Related
- Uterine anomalies like bicornuate uterus may be associated with urinary system anomalies.
Implantation and Fertilization

Introduction: Post-Ovulation Preparation
Endometrial Changes
After ovulation the cells of the dominant follicle & CL produces large amounts of progesterone which prepares the endometrium to support a pregnancy.

Fertilization Process
- Involves the fusion of two haploid gametes with 23 chromosomes each to produce a zygote that contains 46 chromosomes
- Fertilization generally occurs in the fallopian tube and generally within one day of ovulation.
- Both sperm and egg can show their vitality only to a limited period. Sperm is alive for 48-72 hours in a female reproductive system whereas the egg can be fertilized for 24 hours.

Implantation Process
- After fertilization the zygote travels down the fallopian where it becomes a morula.
- Once it reaches the uterus, the morula becomes a blastocyst.
- The blastocyst then burrows into the uterine lining, a process called implantation. Failure of placental delivery and profuse bleeding may indicate conditions like placenta accreta.






Hormonal Regulation: Human Chorionic Gonadotrophin (hCG)
hCG Secretion and Physiological Role
The implanted blastocyst secretes human chorionic gonadotrophin (hCG):
- ‘rescue CL from luteolysis to maintain progesterone secretion.
- prevent menstruation.
- and support the early conceptus (for approximately 8 weeks).
- after which the early placental tissue becomes the main source of progesterone.

hCG Detection in Pregnancy
- hCG can be detected in the urine in sensitive pregnancy tests 1 or 2 days before the expected date of menstruation.
- Most women delay taking a pregnancy test until after a missed period.

Visualizing Early Pregnancy
Ultrasound Detection of Gestational Sac and Embryo
-
A transvaginal ultrasound scan (TVUSS) can detect an early intrauterine gestational sac, the first sign of a normal pregnancy, at around 5 weeks’ gestation.
-
A few days later a circular yolk sac can be seen within the gestational sac, and the embryonic fetus can usually be identified after 5.5 weeks’ gestation.
-
The fetal heartbeat may be visible as early as 6 weeks’ gestation.


Ultrasound Imaging Parameters

Embryonic Structure Post-Implantation

Clinical Manifestations of Implantation
Symptoms and Signs
- Gastrointestinal disorders
- Breast swelLLING
- Nausea
- Implantation bleeding
- Increased urge to urinate

hCG: Characteristics and Effects
- ✓ Production: Primarily from syncytiotrophoblasts.
- ✓ Detection: Can be found in urine/serum as early as 6 days after fertilization, forming the basis of pregnancy tests.
- ✓ Peak Concentration: Reaches a peak at 10-12 weeks gestation, then plateaus.
- ✓ Clinical: Abnormally high levels can indicate a Molar Pregnancy or choriocarcinoma and often present with severe nausea and vomiting.
- ✓ Primary Effects:
- Rescues the corpus luteum to maintain progesterone secretion.
- Prevents menstruation and supports the early conceptus.
- Stimulates ongoing progesterone and estrogen synthesis in the corpus luteum.


Characteristics of the Human Placenta
The human placenta is best described as:
- Discoidal: Refers to its disc-like shape.
- Hemochorial: Characterized by maternal blood being in direct contact with fetal chorion.
- Deciduate: Involves the shedding of maternal decidua along with the fetal membranes at birth.
Antenatal Care
- 7 visit pregnancy on average.
- Booking visit (First visit) 0-13wk : Dating scan, basic investigations (memorize all), full history and examination. + folic
- Second Trimester: Anomaly scan best at 24th week for heart anomalies, generally 18-22 + iron supp. Gestational diabetes screening is typically done between 24-28 weeks via oral glucose tolerance/challenge test.
- Third Trimester: Regular check-ups for fetal growth and well-being.
Labor & Delivery
- Engagement: In primigravid women, engagement (descent of the widest diameter of the presenting part to below the pelvic inlet) may occur weeks before the onset of labor. In multiparous women, it often occurs during labor.
- Vasa Previa: Can cause fetal distress and blood loss, especially with abnormal cord insertion. This is a critical point for emergency management.
Postpartum Care
Puerperium
- The period of about six weeks after childbirth during which the mother’s reproductive organs return to their original non-pregnant condition. A delay in uterine involution without other signs is generally not significant.
Lactation
- Important points include precautions and proper techniques for breastfeeding to ensure infant health and prevent maternal complications like mastitis, abscess or otherwise. Breast milk predominantly contains IgA.
Contraception
Contraceptive counseling and use should be emphasized during the puerperium to avoid an undesired pregnancy.
Thromboembolism (DVT)
- Prevention:
- Mobility and rehydration are key.
- TED compression stockings can be used.
- Prophylaxis (e.g., heparin) may or may not be given, depending on individual risk factors.
Postpartum Infections
- Puerperal Sepsis (e.g., Endometritis): A serious infection occurring after childbirth, often presenting with fever, offensive vaginal bleeding, and abdominal pain. A common cause is retained products of conception, which can lead to septicemia.
Miscarriage


is a pregnancy that ends spontaneously before 24 weeks’ gestation or (or before viability).
- What is viability? More than 24 weeks of gestation or more than 500 gms.

Incidence:
15 - 20% of pregnancies.
Classification:
- Spontaneous miscarriage: occurs without medical or mechanical.
- induced abortion

Pathophysiology
Haemorrhage into the decidua basalis lead to:
A. Necrotic changes in the tissue adjacent to the bleeding. B. Detachment of the conceptus. C. The above will stimulate uterine contractions resulting In expulsion.


RISK FACTOR
- Maternal age - more than 35years.
- Increased gravidity.
- Previous history of miscarriage.
- Multiple pregnancy
Causes of miscarriage
Fetal causes & maternal causes
Fetal causes:
- Chromosomal (e.g. Trisomy, including Down’s syndrome due to non-disjunction).
- Structural e.g. Neural tube defect.
- Genetic e.g. X- Linked diseases



Maternal causes:
Immunological:
- Autoimmune diseases :APL.
uterine abnormality:
- septate uterus & cervical incompetence.
Endocrine :
- Poorly controlled diabetes (type 1/type 2).
- hypothyroidism and hyperthyroidism.
Infections (maternal/fetal):
- as TORCH infections.
- listeria
Environmental toxins:
- alcohol.
- Smoking.
- drug abuse.
- ionizing radiation.

Clinical presentation
- The most common sign of miscarriage is vaginal bleeding.
- Abdominal pain.
- Hypovolemic shock.
- Expulsion of products of conception.
- A symptomatic.
- Each type has its own symptoms
| Type of Miscarriage | Clinical Presentation & Key Features | Cervical Os | Ultrasound (US) Findings | Management |
|---|---|---|---|---|
| Threatened |
| Closed | Viable intrauterine fetus with a fetal heart (FH) present. |
|
| Inevitable |
| Open | Intrauterine pregnancy, often with no fetal heart (FH). |
|
| Incomplete |
| Open | Retained products of conception (RPOC) are visible. |
|
| Complete |
| Closed | Empty uterus. (hCG may be checked to exclude ectopic pregnancy if there was no previous scan). |
|
| Missed |
| Closed | Intrauterine pregnancy with no fetal heart pulsations. |
|
Investigations
- Transabdominal/TVUSS:
- a single ultrasound scan can diagnose a miscarriage if there is a pregnancy within the uterine cavity.
- Haemoglobin and ‘Group and Save’ (or cross-match if patient is severely compromised):
- Assess degree of vaginal loss and rhesus status.
Management
- expectant
- medical
- surgical
- approach depending on clinical presentation and patient choice
- Expectant management
- To avoid surgery
- urinary pregnancy test after 3 weeks and it is positive
- let pt come again She may need surgical treatment if she start to bleed heavily.
- Expectant management
Medical management
- Used in outpatient setting
- allow women to miscarry at home. It involves
- prostaglandin E analogue (misoprostol).
- progesterone antagonist (mifepristone)(if >9wks’).
The side-effects include:
- Pain.
- Vomiting
- Diarrhoea.
- women are routinely provided with pain relief and antiemetics). post-treatment pregnancy test is recommended
Women may need surgical treatment if medical treatment fail.

Surgical management
-
if there is:
- persistent excessive bleeding.
- haemodynamic instability.
- if women favour it.
-
It can be done by Surgical evacuation.
-
Evacuation risks:
- uterine perforation.
- postoperative pelvic infection.
- cervical trauma and subsequent cervical incompetence.
D. The head is grasped and crushed in order to remove it from the vaginal canal.
E. The placenta and remaining contents are suctioned from the uterus.
- Digital Removal: If clots or products of conception are visible at the cervix during an inevitable or incomplete miscarriage, they can sometimes be removed digitally or with forceps to control bleeding. Neurogenic shock is a risk in such procedures.

Recurrent miscarriage
Definition:
Loss of three or more consecutive pregnancies.
Incidence:
- 1% of pregnancies.
Risk factors:
- Advancing maternal and paternal age.
- Obesity.
- Balanced chromosomal translocations.
- Congenital abnormalities.
- Uterine structural anomalies and cervical incompetence.
- Antiphospholipid syndrome (APS).

Investigations
- testing for antiphospholipid antibodies
- imaging of the uterus.
- Products of conception should be sent for cytogenetic analysis to detect chromosomal abnormality.
- peripheral blood karyotyping of both partners should be performed.
Most couples have normal investigations


Diagnosis of cervical incompetence:
-
From history
- Three or more miscarriage es.
- Painless vaginal bleeding.
- decreased gestational age in subsequent pregnancy.
-
From investigations:
- Hagar dilator(No.8).
- HSG.
- During pregnancy: US Funnel shape, short cervix.
Management:
- Cervical cerclage.



SEPTIC MISCARRIAGE
- Following an incomplete miscarriage due to ascending infection.
- Or following criminal abortion.
- Clinical picture: -
- Symptoms:
- Offensive bloody vaginal discharge.
- Increased body temperature.
- Lower abdominal pain (pelvic peritonitis)
- generalized peritonitis.
- Signs:
- Increased pulse rate.
- Dehydration.
- toxicity.
- Symptoms:
- Clinical picture: -

Investigations:
- Blood.
- FBC.
- BHCG.
- Renal profile.(2ry to septic shock).
- Blood grouping & cross matching.
- ESR.
- High vaginal swab for C/S.
- Blood culture & sensitivity(if needed).
Treatment:
- Antibiotic.
- iv fluids.
- blood transfusion.
- Evacuation of retained product.

SEPTIC SHOCK
- Tachypnea Tachycardia
- Hypotension Hypothermia
- Oliguria
- Sepsis
- Multi organ failure
Anti-D administration
- All rhesus-negative women who have a surgical procedure to manage an EP or miscarriage should be offered anti-D immunoglobulin.
- Anti-D is not required for
- Threatened miscarriage.
- complete miscarriage.
- medical management of miscarriage or EP.
- but guidelines differ, and prophylaxis is often given

In all form of miscarriages: general clinical assessment should be made:
- vital signs.
- abdominal examination.
- vaginal examination.
- All needed investigations +/- ws:
- Send product for histopathology.
- Management should be according to clinical Type & gestational age.
Don’t Forget!!
- Pt emotionally distressed by her physical symptoms & loss of her baby. So
- Support her.
- Explain the causes & reassure her she is not guilty
Gynecology
Menstrual Cycle


Normal Menstrual Cycle Manifestation and Control
Manifestation of normal menstrual cycle Is: Presence of regular vaginal bleeding as a result of
- ➡️ shedding of the endometrial lining following
- ➡️ failure of fertilization.
The cycle depends on: Changes occurring in ovarian hormones
Which controlled by:
- Pituitary
- Hypothalamus
The hypothalamo–pituitary–ovarian axis (HPO). Hormonal abnormalities lead to menstruation abnormalities.
28 Days Menstrual phase (5 days)


The Hypothalamus
- Secretes gonadotrophin-releasing hormone (GnRH)
- which controls hormone secretion in the:
- anterior pituitary gland
- ✓ luteinizing hormone (LH)
- ✓ follicle-stimulating hormone (FSH)
- anterior pituitary gland
- ➤ GnRH released in a pulsatile pattern
- ➤ This process is modulated by the ovarian sex steroid hormones
- oestrogen and progesterone
- which controls hormone secretion in the:

Hypothalamus-Pituitary-Ovary-Uterus Feedback Loop

- N.B. the mechanism of action of the negative feedback of oestrogen is uncertain
Initial Stages of Follicular Development
Gonadotropin-Independent Growth
The initial stages of follicular development are independent of hormone stimulation.
- Follicular development will fail at the preantral stage and follicular atresia will ensue if pituitary hormones LH and FSH are absent.
- ➢FSH levels rise in the first days of the menstrual cycle, when oestrogen, progesterone and inhibin levels are low.
- • This stimulates a cohort of small antral follicles on the ovaries to grow.
Follicle Development Stages

Follicular and Luteal Phases Visual Overview



Cellular Interactions in Follicle Steroid Production
- Within the follicles, there are two cell types that are involved in the processing of steroids, including oestrogen and progesterone.
- These are the theca and the granulosa cells, which respond to LH and FSH stimulation, respectively.
- Theca cells ➡️ LH stimulates Progesterone.
- Granulosa cells ➡️ FSH stimulates Oestrogen.


Androgen and Estrogen Synthesis
LH stimulates production of androgens (from cholesterol) within theca cells. …These androgens are converted into oestrogen in granulosa cells, under the influence of FSH.
 FSH = follicle-stimulating hormone | LH = luteinising hormone
FSH = follicle-stimulating hormone | LH = luteinising hormone
Follicle Growth and Feedback
As the follicles grow, oestrogen secretion increases, leading to negative feedback (on the pituitary) which causes a decrease in FSH secretion. (This assists in selection of the dominant follicle while smaller follicles will undergo atresia).
Follicle Maturation and Hormonal Influence


Hormonal Interactions

Regulation of Ovarian Hormones
- Inhibin is secreted by granulosa cells, enhancing androgen synthesis.
- Activin is secreted by granulosa cells (is structurally similar to inhibin, but has an opposite action), increasing FSH binding on the follicles.
- Insulin-like growth factors (IGF-I, IGF-II): highest levels found in the dominant follicle fluid towards ovulation.
- Kisspeptins: proteins recently found to play a role in regulation of the HPO axis, mediated in metabolism of leptin.
- Leptin (affect hypothalamus) plays a role in energy production, weight and reproductive health.
- ” Mutations in the kisspeptin receptors associated with delayed or absent puberty”.

Summary of Hormone Feedback and Cellular Action



Ovulation
At the end of the follicular phase (which lasts an average of 14 days), the dominant follicle has grown to approximately 20 mm (mature follicle).
- ✓FSH induces LH receptors on the granulosa cells.
- ✓ Oestrogen increases until making a positive feedback effect on the pituitary.
- ✓LH surge (24–36 hours later).
- ✓ Progesterone from the mature follicle provides feedback for secretion, causing a small periovulatory rise in FSH.

Mechanism of Ovulation
Ovulation occurs after breakdown of the follicular wall. The LH surge is a predictor of ovulation. This process is under the influence of LH, FSH, and proteolytic enzymes (prostaglandins PGs). Inhibition of PG production may result in failure of ovulation. Thus, women wishing to become pregnant advised to avoid taking PG synthetase inhibitors, such as aspirin and ibuprofen.

Luteal Phase
- ✓After release of oocyte, the remaining granulosa and theca cells form the corpus luteum (CL) (due to accumulated yellow pigment).
- ✓Why? To supply granulosa cells with rich blood for steroidogenesis.
- ✓Progesterone stabilizes the endometrium in preparation for pregnancy.
- ✓High Progesterone levels suppress FSH and LH, which prevent another follicular growth.
- ✓The luteal phase lasts 14 days in most women; it is relatively constant in all women.
- ✓In the absence of βhCG (pregnancy), the CL will regress (luteolysis), leading to progesterone withdrawal, and shedding of the endometrium and menstruation.

Corpus Luteum Formation and Regression


Cycle Renewal and Hormone Feedback
- Reduction in levels of progesterone, oestrogen and inhibin feeding back to the pituitary cause increased secretion of gonadotrophic hormones.
- New preantral follicles begin to be stimulated and the cycle begins again.

Phases of the Woman’s Cycle


Menstruation
Menstruation (day 1) is the
- shedding of the ‘dead’ endometrium and ceases as the endometrium regenerates (which normally happens by day 5–6 of the cycle).
- Immediately prior to menstruation, three layers of endometrium can be seen.
- The basalis is the lower 25% of the endometrium, which will remain throughout menstruation and shows few changes during the menstrual cycle.
- The midportion is the stratum spongiosum with oedematous stroma and exhausted glands. The superficial portion (upper 25%) is the stratum compactum with prominent decidualized stromal cells.

Physiological Mechanism of Menstruation
A fall in circulating levels of oestrogen and progesterone 14 days after ovulation leads to loss of tissue fluid, vasoconstriction of spiral arterioles and distal ischaemia. This results in tissue breakdown and loss of the upper layers, along with bleeding from fragments of the remaining arterioles, seen as menstrual bleeding. Enhanced fibrinolysis reduces clotting. (This effect can be reproduced artificially, for example in patients taking the COCP).
Vaginal bleeding will cease after 5–10 days as arterioles vasoconstrict and the endometrium begins to regenerate.
- Haemostasis in the uterine endometrium is different from elsewhere in the body (no clot formation and no fibrosis).

Endometrial Repair
NOTE Endometrial repair involves:
- both glandular and stromal regeneration
- and angiogenesis
- to
- reconstitute the endometrial vasculature.

The Endometrium
Inflammation of the endometrium is called endometritis.
- The hormone changes effected by the HPO axis during the menstrual cycle will occur whether the uterus is present or not.
- The changes in the endometrium give the most obvious external sign of a regular cycle.
Puberty
Puberty is the process of physical changes by which a child’s body matures into an adult body capable of sexual reproduction.
- Thelarche: One of the first female physical sign of puberty, characterized by breast development.
- Adrenarche: The development of pubic hair, often occurring before gonadal maturation.
- Menarche: The onset of menstruation, typically the last physical sign of puberty.
- Timing of Menarche: Menarche typically occurs within 1-2 years after the onset of breast development (Tanner stage 2).
The Proliferative Phase
After menstruation, when glandular and stromal growth begin. The epithelium lining the endometrial glands cells increase by mitoses. Endometrial thickness increases from 0.5 mm to 3.5–5 mm at the end of the proliferative phase.

The Secretory Phase
- After ovulation (around day 14)
- there is a period of endometrial glandular secretory activity.
- Endometrial thickness does not increase any further.
- The glands will become more tortuous.
- Spiral arteries will grow.
- Fluid is secreted into uterine lumen.
- Later, formation of a temporary layer, known as the decidua, in the endometrial stroma.
Endometrial Receptivity
After day 21–22, a progesterone-dependent stage making the endometrium receptive for embryo implantation.

Endometrial Tissue Sections
- (A)proliferative phase.
- (B)secretory phases Of the menstrual cycle

Polycystic Ovary Syndrome (PCOS)
PCOS is a syndrome of :
- ovarian dysfunction
- with features of hyperandrogenism.
- and polycystic ovary morphology. It is also associated with altered metabolism of androgens and estrogens.
Clinical manifestations
- Menstrual irregularities.
- Signs of androgen excess (e.g. hirsutism).
- Obesity.
- Elevated serum LH levels.
- Insulin resistance .
- Increased risk of type 2 DM, CVD events, and endometrial cancer.
Affects around 5–10% of women of reproductive age.
The prevalence of PCOS on ultrasound is 25 %.

Aetiology
- Aetiology is not completely clear.
- There is often a family history (gene is important in its development).
Clinical features:
- Oligomenorrhoea/amenorrhoea up to 75% (due to chronic anovulation).
- Hirsutism.
- Subfertility (75 %).
- Obesity (40 %).
- Recurrent miscarriage in around (50–60 %).
- Acanthosis nigricans (areas of increased velvety skin pigmentation occur in the axillae and other flexures).
- May be symptomatic.



PCOS SYMPTOMS
- HAIR LOSS
- HIRSUTISM
- PELVIC PAIN
- INFERTILITY
- OVERWEIGHT
- IRREGULAR PERIODS
- FATIGUE
- HIGH TESTOSTERONE LEVELS
- ACNE

Diagnosis
Patients must have two out of the three features below:
- Amenorrhoea/oligomenorrhoea.
- Clinical or biochemical hyperandrogenism.
- Polycystic ovaries on ultrasound.
- The ultrasound criteria for the diagnosis of a polycystic ovary are:
- Eight or more subcapsular follicular cysts <10 mm in diameter.
- Increased ovarian stroma.
- The ultrasound criteria for the diagnosis of a polycystic ovary are:
While these findings support a diagnosis of PCOS, they are not by themselves sufficient to identify the syndrome.

Management
- Weight reduction.
- Lifestyle advice:
- Dietary modification and exercise because these patients are at an increased risk of developing DM and CVS.
- Medications:
- COCP:
- Regulate menstruation.
- Cyclical oral progesterone:
- Regulate menstruation.
- Metformin:
- In patients with PCOS with hyperinsulinemia and cardiovascular risk factors, often requiring glucose and lipid profile monitoring.
- Clomiphene:
- To induce ovulation where subfertility is a factor.
- COCP:

Hirsutism
PCOS is the most common cause of hirsutism.
- Medical treatment:
- Eflornithine cream topically.
- Cyproterone acetate.
- Dinetter anti-androgen contraceptive pill).
- Metformin:
- improves insulin resistance,
- Hyperandrogenaemia.
- anovulation.
- and acne .
- GnRH analogues with low-dose HRT: Reserved for women intolerant of other therapies.
- Surgical treatments, e.g. laser or electrolysis.
- Physical methods: shaving.

Gynecology Terminology
- Oligomenorrhea: Infrequent menstrual periods, typically defined as cycles longer than 35 days.
- Direct Maternal Mortality: Death resulting from obstetric complications of the pregnant state (pregnancy, labour, and puerperium), from interventions, omissions, incorrect treatment, or from a chain of events resulting from any of the above.
- Polyp (Cervical/Endocervical): The most common benign neoplasm of the cervix and endocervix.
Uterine Fibroids (Leiomyomas)
Uterine fibroids are benign tumors of the uterine smooth muscle.
- Management Options:
- Hysterectomy: Definitive surgical treatment, especially for women who have completed childbearing or have severe symptoms.
- Myomectomy: Surgical removal of fibroids while preserving the uterus, often preferred by women desiring future fertility or uterine preservation.
- Uterine Artery Embolization (UAE): A minimally invasive procedure that blocks blood flow to the fibroids, causing them to shrink. Suitable for women who have completed childbearing and wish to avoid surgery.
Ethics & Legal
Principles of Ethics
Four Pillars of Medical Ethics
- Autonomy الاستقلالية
- Beneficence الاحسان
- Non-Maleficence غير مؤذ
- Justice العدالة
Informed Consent
What is Informed Consent
- “Informed consent is a consent obtained freely, without threats or improper inducements, after appropriate disclosure to the patient of adequate and understandable information in a form and language understood by the patient on.
- The patient should be informed about:
- The expectation of benefit
- Other reasonable alternatives
- Possible risks that are known
- It can be given orally, by signing a form or a written statement or simply agreeing by a gesture.
- It must always be obtained in advance.
Requirements for Valid Consent
- Patient should be:
- Competent i.e., should have the capacity to make a decision. (free of a defect of mind or judgment, or not be a minor)
- Must do it freely and voluntarily (without threat)
- Doctor must give options to choose from and patient not to fear a rejection or neglect by the doctor in case he or she refuses to agree. (no threat)
- Doctor must also ensure that the information has been clearly understood. ( consequences & side effects )
PREPARED System
- There is general agreement that consent must be genuinely voluntary and made after adequate disclosure of information
- The PREPARED checklist is a useful tool to ensure covering all required aspects
THE PREPARED SYSTEM: A CHECKLIST TO ASSIST THE PATIENT AND PROVIDER IN THE PROCESS OF INFORMED CONSENT
| P | Plan | The course of action being considered |
|---|---|---|
| R | Reason | The indication or rationale |
| E | Expectation | The chances of benefit and failure |
| P | Preferences | Cultural and patient-centered priorities (utilities) affecting choice |
| A | Alternatives | Other reasonable options/plans |
| R | Risks | The potential harm from plans |
| E | Expenses | All direct and indirect costs |
| D | Decision | Fully informed collaborative choice |
Exceptions to the Rule of Informed Consent
-
Patients brought into emergency and accident departments (unconscious, alone & require life-saving measures)
-
Child under 16 years (in these cases, the parents may be given this right)
-
Impaired capacity to give consent (The guardian)
Confidentiality
How Much?
A doctor is expected to preserve absolute confidentiality on all that they know about their patient, not only during the treatment but also after it and even after the patient’s death.
Breaches of Confidentiality
- When a patient authorizes to do so in situations such as, while seeking employment.
- Medical report or opinion for the employer.
- Report prepared for a second opinion.
- Health care team.
- Disclosure is in the best interest of the patient.
- Public interest
- Holding back the information can cause harm to the members of the society.
- Legal requirement as in matters of Laws on Public Health control of diseases such as cholera, smallpox, plague, or venereal diseases.
- For research purposes but only as anonymous data after consent of the patient.
Modern Principles of Data Protection
- Data shall be accurate and up to date.
- Stored data should be adequate, relevant, not excessive
- Data is available to the patient to verify factual accuracy.
- Data is not stored for longer than will serve the interests of the patient.
- Data protection shall include security against improper access
Justice, Beneficence, Non-Maleficence
-
Justice: Race, sex, and religion are not considered morally legitimate criteria for the distribution of benefits
-
When resources are scarce, issues proper and clear distribution of care should follow clear guidelines that are fair and free of bias.
-
Beneficence: be nice, be better and kind.
-
Non-Maleficence: Do no Harm “first, do no harm,” originated from the Hippocratic school, and although few would dispute the basic concept, in day-to-day medical practice, physicians and their patients may need to accept some harm from treatment (such as necessary surgical trauma) in order to achieve a desired outcome.
How Ethics Interact with Clinical Decisions?
Appraise the Principles of Ethics
Clinical Reasoning
- Problem
- History
- Exam
- Data
- Differential Diagnosis, Clinical Assessment
- Further Diagnostic Evaluation
- Treatment Plan
Clinical Ethical Reasoning
- Problem
- Medical Facts
- Medical Goals
- Patient Goals
- Context
- Differential Diagnosis, Ethical Assessment
- Further Information & Dialogue
- Best Course of Action

Rationing
- Implicit (arbitrary)
- Based on access or ability to pay
- Irrational
- Explicit (planned)
- Based on measured value
- Rational

Remember
-
The interface of medicine and the law raises major ethical issues because legality and morality are not always synonymous.
-
If your are not sure , you can always consult the Ethical committee in your hospital
-
Do what is in the best interest of your patient and her wishes or goals and keep her informed